Published online Feb 18, 2025. doi: 10.5312/wjo.v16.i2.103817
Revised: January 4, 2025
Accepted: January 15, 2025
Published online: February 18, 2025
Processing time: 72 Days and 16.9 Hours
Return to work (RTW) and resumption of driving (ROD) are critical factors that influence postoperative quality of life in patients undergoing total hip arthroplasty (THA). However, few studies have focused on the minimally invasive (MIS) approach and its effect on these outcomes.
To investigate RTW and ROD's timelines and influencing factors following an
A retrospective analysis was conducted on 124 patients who underwent anterior MIS-THA. Data on the demographics, occupational physical demands, and RTW/ROD timelines were also collected. Clinical outcomes were measured using standardised scoring systems. Statistical analyses were performed to evaluate the differences between the groups based on employment status and physical work
Among employed patients, the RTW rate was 94.7%, with an average return time of five weeks. The average ROD time was 3.5 weeks across all patients. Despite similar postoperative clinical scores, RTW time was significantly influenced by occupations' physical workload, with heavier physical demands associated with delayed RTW.
Anterior MIS-THA facilitates early RTW and ROD, particularly in occupations with lower physical demands. These findings highlight the importance of considering occupational and physical workload in postoperative care planning to optimize recovery outcomes.
Core Tip: This study investigates the outcomes of anterior minimally invasive total hip arthroplasty (MIS-THA), focusing on return to work (RTW) and resumption of driving (ROD). Among 124 patients, 94.7% returned to work within an average of 5 weeks. All patients who drove preoperatively resumed driving postoperatively, with an average ROD time of 3.5 weeks. Patients with heavier physical workloads required more time to RTW compared to those with lighter workloads. The findings highlight the advantages of MIS-THA, including reduced recovery times and tailored postoperative care to support occupational demands, contributing to improved quality of life and productivity.
- Citation: Ishikura H, Masuyama Y, Fujita S, Tanaka T, Tanaka S, Nishiwaki T. Return to work and resumption of driving after anterior minimally invasive total hip arthroplasty. World J Orthop 2025; 16(2): 103817
- URL: https://www.wjgnet.com/2218-5836/full/v16/i2/103817.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i2.103817
Studies on the return to work (RTW) and resumption of driving (ROD) have attracted significant attention across all types of orthopaedic surgeries, including joint arthroplasty[1–5].
Total hip arthroplasty (THA) has undergone significant advancements, making it a standard procedure not only for elderly patients but also for relatively younger individuals, including those actively engaged in work and daily driving[6]. As THA techniques improve, long-term outcomes have become more favourable, raising critical questions regarding the timing and feasibility of returning to work and resuming driving postoperatively. These aspects are vital for workers and daily drivers whose ability to return to routine activities significantly affects their quality of life and economic stability.
Minimally invasive (MIS) surgery has gained prominence in orthopaedic procedures because of its potential benefits, including reduced recovery times and postoperative pain. As for the THA, the anterior MIS-THA refers to an anterior approach THA that uses a leg positioner to minimize the detachment of the iliofemoral ligament and short external rotators, reducing extra-articular invasion to the minimum. This intertissue-sparing technique is believed to be advan
The existing literature on post-THA recovery has predominantly focused on traditional surgical approaches or presented a combination of various methods. These studies provide valuable insights into the general outcomes of THA; however, they often lack detailed analyses of the specific approaches to occupational and driving activities. Few studies have classified occupations based on physical demands or examined the RTW period for each occupation, despite reports in the field of spine surgery indicating that the timing of RTW varies depending on physical workload[9].
This study investigated the outcomes of MIS-THA at our institution, focusing on the timelines and factors influencing RTW and ROD.
We retrospectively analysed 158 consecutive THA procedures performed at our institution between November 2022 and February 2024. The patients in this study underwent MIS-THA, and their employment and driving statuses were documented in their medical records. The exclusion criteria were incomplete records (n = 17) and inability to ascertain follow-up data (n = 15). Patients with early postoperative periprosthetic femoral fractures (n = 1) and those requiring revision due to stem subsidence (n = 1) were also excluded. Thus, 124 patients were included in this study. Written informed consent was obtained from all participants.
All surgeries were performed using a MIS anterior approach, with the assistance of a leg positioner[10]. This technique involves a small incision at the anterior aspect of the hip to preserve the intermuscular and neurovascular structures. The leg positioner allows a person outside the surgical field to control various movements such as internal and external rotation, abduction and adduction, extension, elevation, and traction of the lower limbs. This reduces the number of assistants required for THA. Because femur manipulation becomes easier, short external rotators such as the conjoined tendon can be easily managed without detachment, ultimately preserving soft tissue.
Postoperative rehabilitation commenced the day after surgery, with full weight-bearing ambulation permitted as soon as possible. During hospitalisation, the patients underwent training in activities of daily living, including stair climbing, and were discharged approximately 7–10 days postoperatively. Rehabilitation guidance was provided at discharge, and only a few patients required outpatient rehabilitation. After discharge, patients were informed that they could decide when to RTW or resume driving at their discretion.
Data on patient demographics (age, sex, height, and weight), employment status, physical job demands, and timing of RTW and ROD were collected. Patients were followed up in outpatient clinics at 1 month, 3 months, and 6 months postoperatively and were interviewed regarding the timing of RTW and ROD. The RTW and ROD rates were assessed based on the resumption rates at the 6-month follow-up. Based on previous reports, jobs were classified into three categories according to their physical demands: (1) Light work (e.g., desk jobs and executives); (2) Medium work (e.g., drivers and standing jobs that did not involve lifting heavy objects); and (3) Heavy work (e.g., factory workers and farmers)[11]. The clinical outcomes measured included pain, function, and overall patient satisfaction.
Student’s t-test was used to compare the mean values between two groups. Differences in categorical variables were evaluated using the χ2 test. The Kruskal-Wallis test was used to analyze continuous variables in the three groups. Suppose a significant difference was found among the three groups (P < 0.05), the Steel-Dwass tests were used to evaluate the differences between each pair of groups. Analyses were performed using Bell Curve for Excel ver. 4.04 (Social Survey Research Information Co. Ltd. Tokyo, Japan). All statistical analyses were performed at a significance level of P < 0.05.
Among the study’s 124 patients, 67 patients were not employed preoperatively (unemployed group), and 57 patients were (employed group). All patients underwent a postoperative follow-up period of at least 12 weeks, with an average follow-up period of 35 weeks. The preoperative patient backgrounds were compared based on employment status (Table 1). The unemployed group was generally older, had a higher proportion of female patients, and had a lower average height and weight than the employed group. The driving rate was significantly higher in the employed group. The preoperative Harris hip score (HHS), Western Ontario and Mcmaster Universities Osteoarthritis Index (WOMAC), Centre for Epidemiologic Studies Depression Scale, and University of California, Los Angeles (UCLA) activity scores were not significantly different between the two groups.
| Unemployed | Employed | P value | |
| Number of patients | 67 | 57 | - |
| Age (years) | 71.4 ± 8.9 | 64.6 ± 10.0 | < 0.001 |
| Number of females | 65 (97.0) | 47 (82.4) | 0.006 |
| Height (cm) | 152.5 ± 6.7 | 156.2 ± 8.5 | 0.010 |
| Weight (kg) | 54.9 ± 11.7 | 61.5 ± 12.7 | 0.007 |
| Preop Harris hip score | 54.9 ± 13.8 | 55.4 ± 10.6 | 0.60 |
| Preop Western Ontario and Mcmaster Universities Osteoarthritis Index | 39.2 ± 16.4 | 40.9 ± 18.2 | 0.81 |
| Preop Centre for Epidemiologic Studies Depression Scale | 13.5 ± 7.0 | 13.3 ± 548 | 0.84 |
| Preop University of California, Los Angeles | 2.3 ± 0.5 | 2.3 ± 0.5 | 0.93 |
| Rate of RTW | - | 54 (94.7) | - |
| Time to RTW (week) | - | 5.0 ± 4.1 | - |
| Number of drivers | 41 (61.2) | 48 (84.2) | 0.005 |
| Time to resumption of driving (week) | 3.5 ± 2.5 | 3.5 ± 2.5 | 0.92 |
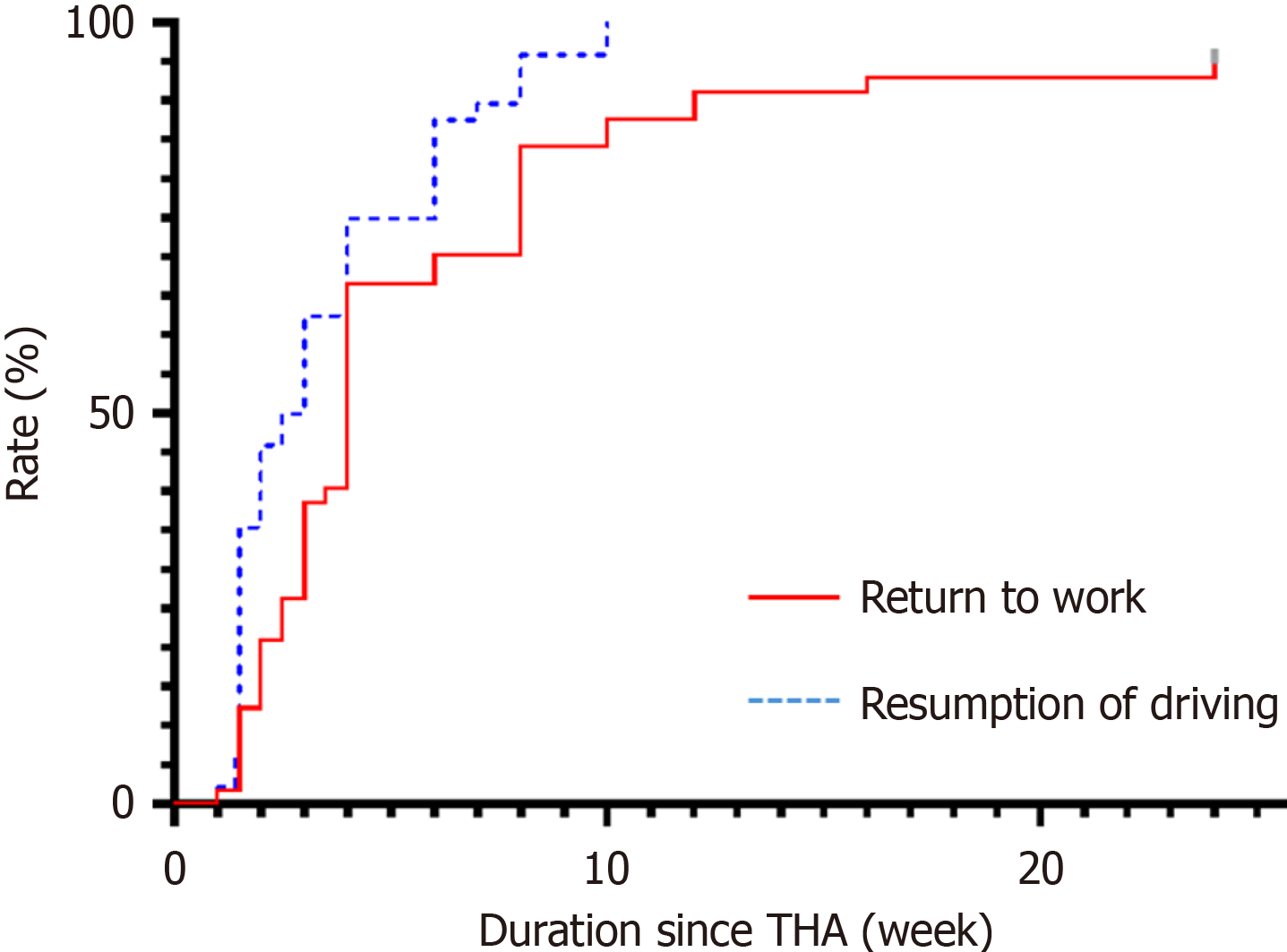
In the employed group, 94.7% of the patients returned to work postoperatively, with an average return time of five weeks after THA. The average time to ROD was approximately three weeks in both groups, with no significant difference. Both RTW and ROD rates gradually increased with time after surgery (Figure 1).
The relationship between the physical demands of work and the time to RTW was analysed. Despite no significant differences in HHS, WOMAC, and UCLA scores at three months postoperatively among the three groups, patients with heavier physical workloads tended to RTW later (Table 2). The Kruskal-Wallis test showed significant differences in RTW times among the three groups (P = 0.019). Further comparisons using the Steel-Dwass test revealed that the RTW time in the heavy work group was significantly longer than that in the light group (P = 0.028).
| 1 (light) | 2 (medium) | 3 (hard) | P value | |
| Number of patients | 20 | 22 | 12 | |
| Time to return to work (week) | 3.6 ± 2.3 | 5.3 ± 5.0 | 7.0 ± 4.2 | 0.019 |
| Postop Harris hip score | 92.5 ± 7.3 | 95.6 ± 1.5 | 95.4 ± 0.8 | 0.58 |
| Postop Western Ontario and Mcmaster Universities Osteoarthritis Index | 12.8 ± 12.1 | 9.6 ± 6.7 | 10.9 ± 10.1 | 0.8 |
| Postop University of California, Los Angeles | 3.6 ± 0.6 | 3.8 ± 0.6 | 4.0 ± 0.5 | 0.28 |
In this study, 46% (57/124) of patients who underwent THA were employed, and 72% (89/124) were regular drivers, reflecting the increasing prevalence of THA among individuals engaged in work and driving activities.
This study provides new insights into the RTW and ROD after MIS-THA. The primary findings included a remarkably high RTW rate of 94.7%, with an average postoperative return time of five weeks, and an average ROD time of approximately 3.5 weeks.
Previous reports on RTW and ROD after THA showed significant variability in the rate and timeline. According to a meta-analysis by Soleimani et al[12], the average return-to-work rate after THA among patients employed before surgery was 87.9% (95%CI: 0.793–0.933). The time to RTW varied among reports: 24 days[13], 5 weeks[14], 6.4 weeks[15], 69 days[16], 10 weeks[17], 85 days[18], 12.5 weeks[19], 13.6 weeks[20], and 13.8 weeks[21], with most studies indicating a return period of approximately 1.5–3 months. In our study, the rate of RTW was relatively high, and the timing of RTW tended to be earlier than reported in other studies.
Regarding the ROD, previous studies reported resumption rates of 77%[22] and 88%[23] at six weeks postoperatively. This study's resumption rates were 87.5% at six weeks and 100% at 10 weeks, demonstrating relatively favourable outcomes.
The variability in RTW and ROD outcomes across studies can be attributed to several factors, including preoperative hip conditions, surgical techniques, implant types, patient environments (including economic circumstances and workplaces), hospital environments (private, public, or acute care hospitals), and differing medical opinions regarding postsurgical recovery. Therefore, a study conducted at a single facility, where these conditions, including the surgical approach, are standardised, is highly valuable.
A detailed analysis of our results revealed that the physical demands of patients' occupations significantly influenced the time to RTW. Specifically, patients engaged in jobs classified as having heavy physical demands took an average of 7.0 weeks to resume work, compared to 3.8 weeks for those in light or moderate physical demand jobs. This disparity underscores the importance of considering the nature of the patient’s occupation when planning postoperative care and advising on expected recovery times. In the present study, the proportion of individuals engaged in work with heavy physical demands was relatively high, exceeding 20% of the workforce. Approximately 40% of these individuals are tea farmers, reflecting their regional characteristics. Tea cultivation involves tasks that require a fully seated posture similar to a squatting position and advanced hip joint function. This was identified as contributing to the prolonged time needed for RTW.
The earlier ROD compared with RTW aligns with the general understanding that driving typically imposes less physical strain than many occupational tasks. Our findings did not show significant differences in the driving resumption time based on the operated side or employment status, suggesting a uniform recovery in this aspect of daily activities.
The early RTW and driving observed in our study cohort is promising and highlights the potential advantages of MIS-THA. MIS-THA uses a leg positioner to facilitate femoral manipulation, minimising soft-tissue detachment. Minimising invasiveness outside the joint capsule may reduce postoperative pain and accelerate recovery, allowing patients to resume normal activities sooner. This has profound implications for the patients’ quality of life and economic pro
This study has several limitations. Because this was a retrospective study conducted at a single institution, the generalisability of the results is limited. The lack of long-term follow-up data renders the sustainability of RTW and ROD unclear. Because RTW is influenced by each country's healthcare insurance and social security systems[24], it is not easy to make direct comparisons between countries.
Future studies should include prospective cohort studies conducted to gather more generalisable data. Comparative studies of different surgical approaches and implants are necessary. Developing postoperative rehabilitation programmes tailored to individual patient needs could enhance recovery outcomes.
In conclusion, MIS-THA at our institution resulted in favourable early RTW and ROD outcomes for patients. The data contribute to the growing body of evidence supporting the benefits of MIS surgical techniques in orthopaedic practice. Future studies should continue exploring the factors influencing recovery time and optimize postoperative care protocols to enhance patient outcomes.
We would like to express our gratitude to all the administrative staff in Shizuoka Red Cross Hospital who assisted with data collection for this study.
| 1. | McDonald EL, Shakked R, Nicholson K, Daniel JN, Pedowitz DI, Winters BS, Rogero R, Raikin SM. Return to Driving After Foot and Ankle Surgery: A Novel Survey to Predict Passing Brake Reaction Time. Foot Ankle Spec. 2021;14:32-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Lalehzarian SP, Agarwalla A, Liu JN. Return to work following shoulder arthroplasty: A systematic review. World J Orthop. 2022;13:837-852. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 3. | Kalejman IP, Pasqualini I, Larrague C, Gallego F, Tanoira I, Ranalletta M, Rossi LA. Factors affecting return to work following arthroscopic rotator cuff repair. Shoulder Elbow. 2024;17585732241255947. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 4. | Peters MCWM, Pronk Y, Brinkman JM. Eight of ten patients return to daily activities, work, and sports after total knee arthroplasty. World J Orthop. 2024;15:608-617. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (6)] |
| 5. | van Zaanen Y, Hoozemans MJM, Kievit AJ, Kuijer PPFM; Expect TO work Consortium. Predictive Validity of the Work, Osteoarthritis, or Joint Replacement Questionnaire for Return to Work After Total Knee Arthroplasty: A 12-Month Multicenter Prospective Cohort Study. J Arthroplasty. 2024;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 6. | Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007;370:1508-1519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1477] [Cited by in RCA: 1909] [Article Influence: 100.5] [Reference Citation Analysis (0)] |
| 7. | Matta JM, Shahrdar C, Ferguson T. Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clin Orthop Relat Res. 2005;441:115-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 463] [Cited by in RCA: 451] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 8. | Berger RA, Jacobs JJ, Meneghini RM, Della Valle C, Paprosky W, Rosenberg AG. Rapid rehabilitation and recovery with minimally invasive total hip arthroplasty. Clin Orthop Relat Res. 2004;239-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 270] [Cited by in RCA: 239] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 9. | Singh S, McIntosh G, Dea N, Hall H, Paquet J, Abraham E, Bailey CS, Weber MH, Johnson MG, Nataraj A, Glennie RA, Attabib N, Kelly A, Rampersaud YR, Manson N, Phan P, Rachevitz M, Thomas K, Fisher C, Charest-Morin R. Effects of Workload on Return to Work After Elective Lumbar Spine Surgery. Global Spine J. 2024;14:420-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 10. | Goldberg TD, Kreuzer S, Randelli F, Macheras GA. Erratum to: Direct anterior approach total hip arthroplasty with an orthopedic traction table. Oper Orthop Traumatol. 2021;33:556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 11. | Wang M, Zhao R, Hao Y, Xu P, Lu C. Return to work status of patients under 65 years of age with osteonecrosis of the femoral head after total hip arthroplasty. J Orthop Surg Res. 2023;18:783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 12. | Soleimani M, Babagoli M, Baghdadi S, Mirghaderi P, Fallah Y, Sheikhvatan M, Shafiei SH. Return to work following primary total hip arthroplasty: a systematic review and meta-analysis. J Orthop Surg Res. 2023;18:95. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 13. | Batra A, Gogos S, Nizam I. When do patients drive after minimally invasive anterior hip replacements? A single surgeon experience of 212 hip arthroplasties. SICOT J. 2018;4:51. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Tanavalee A, Jaruwannapong S, Yuktanandana P, Itiravivong P. Early outcomes following minimally invasive total hip arthroplasty using a two-incision approach versus a mini-posterior approach. Hip Int. 2006;16 Suppl 4:17-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | McGonagle L, Convery-Chan L, DeCruz P, Haebich S, Fick DP, Khan RJK. Factors influencing return to work after hip and knee arthroplasty. J Orthop Traumatol. 2019;20:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 16. | Kangas P, Soini S, Pamilo K, Kervinen V, Kinnunen ML. Return to Work Following Hip or Knee Arthroplasty: A One-Year Prospective Cohort Study in Participants with Direct Referral from Hospital to Occupational Health Care Services. J Occup Rehabil. 2024;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 17. | Hauer G, Smolle M, Zaussinger S, Friesenbichler J, Leithner A, Maurer-Ertl W. Short-stem total hip arthroplasty is not associated with an earlier return to work compared to a straight-stem design. Sci Rep. 2021;11:4968. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 18. | Boersma AR, Brouwer S, Koolhaas W, Brouwer RW, Zijlstra WP, van Beveren J, Stevens M. No association between preoperative physical activity level and time to return to work in patients after total hip or knee arthroplasty: A prospective cohort study. PLoS One. 2019;14:e0221932. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 19. | Tilbury C, Leichtenberg CS, Tordoir RL, Holtslag MJ, Verdegaal SH, Kroon HM, Nelissen RG, Vliet Vlieland TP. Return to work after total hip and knee arthroplasty: results from a clinical study. Rheumatol Int. 2015;35:2059-2067. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 20. | Al-Hourani K, MacDonald DJ, Turnbull GS, Breusch SJ, Scott CEH. Return to Work Following Total Knee and Hip Arthroplasty: The Effect of Patient Intent and Preoperative Work Status. J Arthroplasty. 2021;36:434-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 21. | Oken FO, Yildirim OA, Asilturk M. Factors affecting the return to work of total hip arthroplasty due to of developmental hip dysplasia in in young patients. J Orthop. 2018;15:450-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Coxe FR, Kahlenberg CA, Garvey M, Cororaton A, Jerabek SA, Mayman DJ, Figgie MP, Sculco PK. Early Recovery Outcomes in Patients Undergoing Contemporary Posterior Approach Total Hip Arthroplasty: Each Week Shows Progress. HSS J. 2024;20:245-253. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 23. | Dugdale EM, Siljander MP, Trousdale RT. Factors Associated With Early Return to Driving Following Total Joint Arthroplasty. J Arthroplasty. 2021;36:3392-3400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | Kamp T, Brouwer S, Seeber GH, Overgaard S, Gademan MGJ, Stevens M. Return to work policies and practices after total hip or knee arthroplasty in Denmark, Germany, and the Netherlands: an exploratory study. Disabil Rehabil. 2024;46:5313-5322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/