Published online Dec 18, 2025. doi: 10.5312/wjo.v16.i12.111602
Revised: August 4, 2025
Accepted: October 29, 2025
Published online: December 18, 2025
Processing time: 166 Days and 17.5 Hours
Inferior intra-articular patella dislocation is rare and comprises horizontal (type 1) and the more common vertical (type 2) dislocations in young and elderly patients respectively. In this case report, we describe a case of an elderly patient who pre
A 75-year-old woman presented with a right knee fixed flexion deformity after a fall. Preoperative imaging confirmed a vertical intra-articular patella dislocation with a femoral trochlear osteochondral defect and lax though grossly intact patella tendon. Closed reduction was performed under general anaesthesia. Knee arthroscopy confirmed the presence of a femoral trochlear osteochondral defect whose edges were subsequently smoothed and there was debridement of scant debris with thorough irrigation of the joint. Postoperative imaging demonstrated anatomical alignment, however, there was a new nondisplaced medial femoral trochlear. The patient however was able to mobilise well in a range of motion brace set at 0-30 degrees and was discharged 1-day post operatively.
Inferior patella dislocation is rare and this article highlights its types and imaging features which determine the most appropriate management.
Core Tip: Assessment of inferior patella dislocation should focus on the patella position, any fractures and the condition of the extensor mechanism. Closed reduction is possible in type 2 injuries (vertical orientation from osteophyte locking), however, success is dependent on the depth and size of the osteochondral defect and degree of patella rotation. Open reduction is recommended for type 1 (horizontal type) due to associated soft tissue injury which can be repaired. In type 2 injuries open reduction is recommended with large osteochondral defects requiring smoothing and or debridement, large osteophytes requiring resection or removal of intra-articular loose bodies.
- Citation: Brooks JR, Pitman AG, Lucas P, Cawthorne DP, Wade SWT. Inferior patella dislocation in an elderly patient after a fall: A case report. World J Orthop 2025; 16(12): 111602
- URL: https://www.wjgnet.com/2218-5836/full/v16/i12/111602.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i12.111602
Patella dislocation is common with a mean annual incidence of 5.8 per 100000 people and more common in women[1]. Typically, 2/3 of presentations involve young patients under the age of 20 years, who often present with either medial or lateral dislocations[2,3]. We present an unusual case of an elderly woman presenting with a locked knee secondary to an inferior patella dislocation. In this case report, we review the types of inferior patella dislocation and discuss their mechanisms of injury, key imaging features and treatment options for this rare injury.
A 75-year-old female presented to the Emergency Department with right knee pain and a fixed flexion deformity after a fall.
The patient described a fall where her right knee folded beneath her while walking her dog and she was unable to recall if this was directly backwards or to the side. She was unable to extend or weight bear on the affected limb afterwards.
The patient denies any prior right knee injuries, hypermobility syndromes, known reduced bone mineral density or fragility fractures.
No prior relevant personal or family history.
On examination the right knee was diffusely tender and held in a fixed flexion deformity at 80 degrees. No open wound. The limb remained neurovascularly intact with strong dorsalis pedis and posterior tibial pulses.
Laboratory examination is not applicable.
A right knee X-ray demonstrated the knee flexed at 80 degrees with the patella inferiorly dislocated (Figure 1). On the subsequent computed tomography, the knee remained unchanged in position and the patella was perched in a small minimally depressed fracture of the femoral trochlear slightly lateral to the midline (Figure 1). The patella and quadriceps tendons appeared thin and there was a small joint effusion with incidental finding of a small popliteal cyst. Ultrasound of the right knee extensor mechanism revealed a lax patella tendon suspicious for a distal rupture and a small knee joint effusion. The quadriceps tendon and its insertion remained intact.
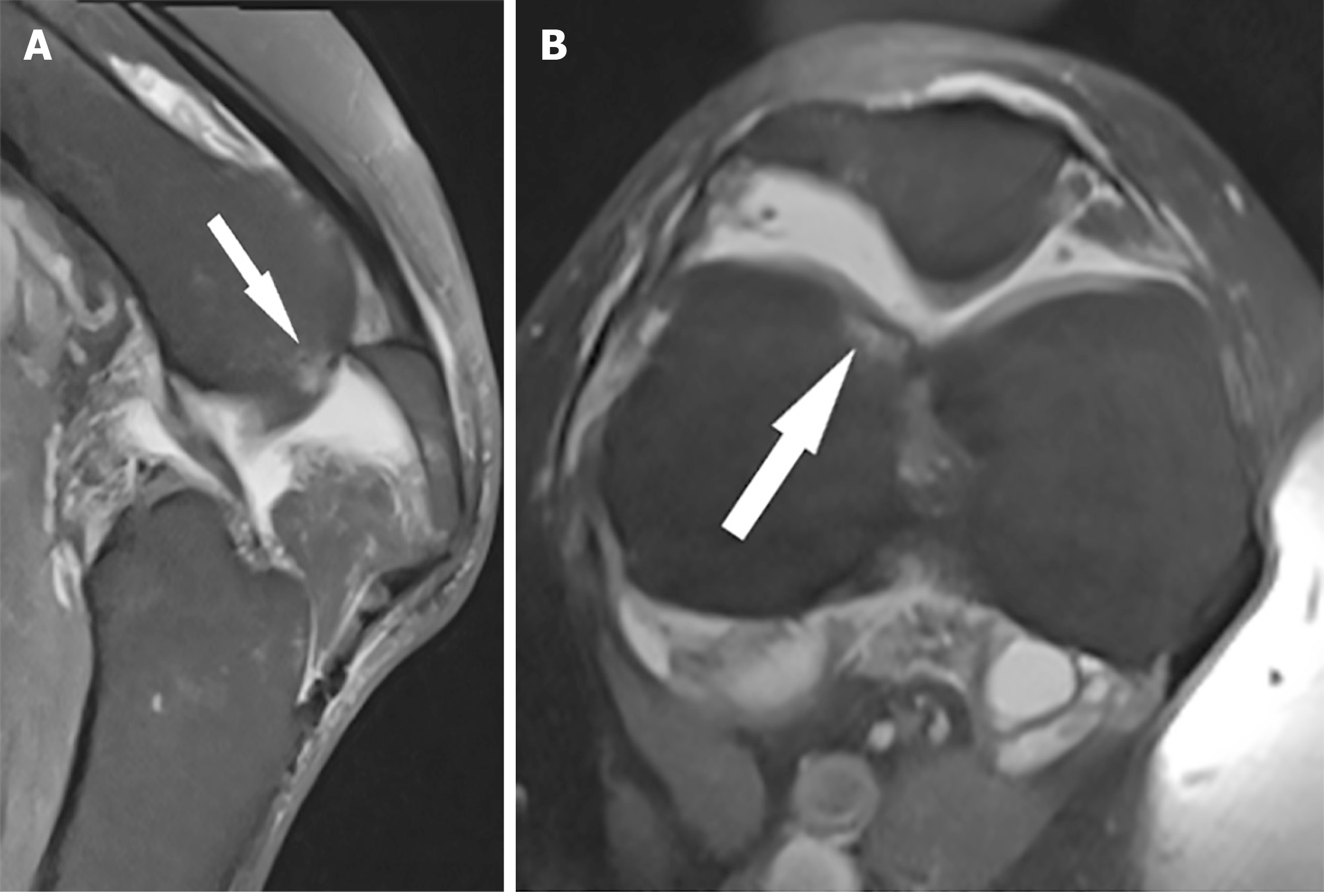
Preoperative magnetic resonance imaging (MRI) was undertaken on a 3T magnet to evaluate the condition of the extensor mechanism; however, this was challenging as the patients fixed flexion deformity prevented the use of the limb coil. MRI confirmed the presence of a small minimally depressed acute femoral trochlear fracture flanked by bone oedema (Figure 2). The quadriceps tendon and its patella attachment were intact; however, the patella tendon was concertinaed with heterogenous signal equivocal for a low-grade partial tear. There was no cruciate ligament or meniscal injury.
Inferior (type 2) intra-articular dislocation of the right patella.
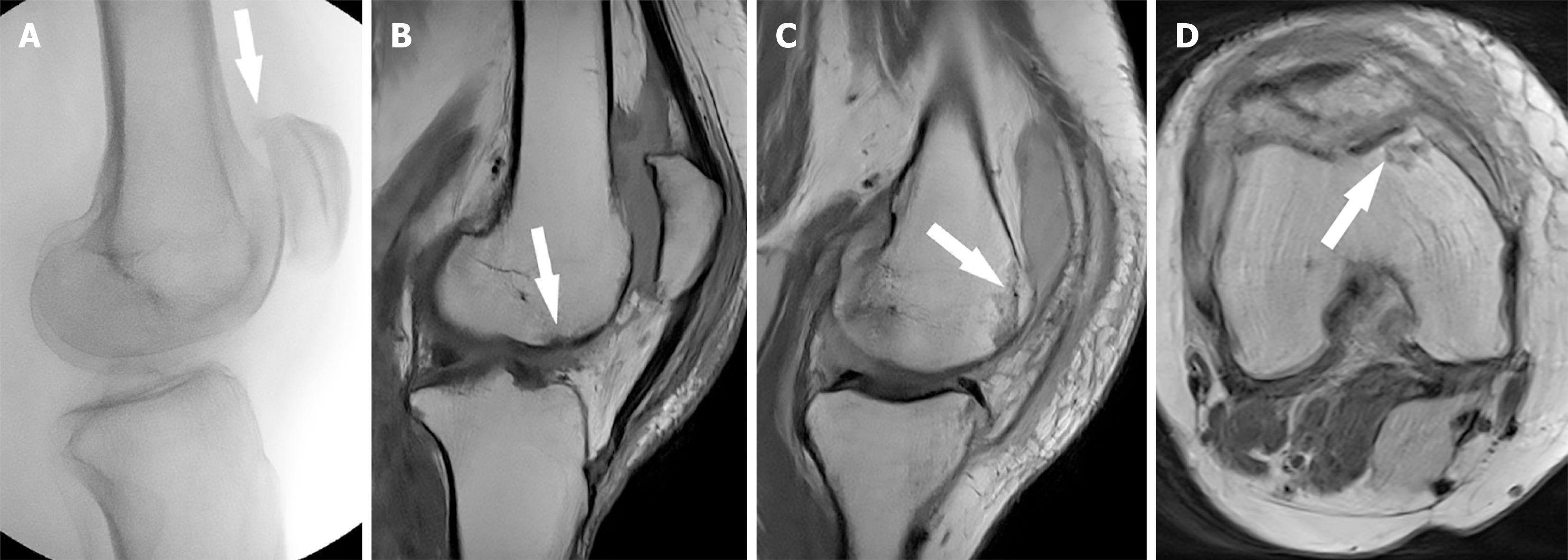
There was a single unsuccessful attempt at reduction in the Emergency Department. Subsequently closed reduction was performed under general anaesthesia and anatomical alignment was confirmed with fluoroscopy (Figure 3). Stability was assessed through range of motion (ROM) testing and clinically the patella and quadriceps tendon were intact. A diagnostic arthroscopy was conducted through medial and lateral portals. This confirmed the presence of a femoral trochlear osteochondral defect corresponding to the abnormality on the MRI. Other findings included blood-stained synovial fluid, full thickness patellofemoral chondral loss with exposed subchondral bone, and chondral fissuring and fragmentation in the medial and lateral compartments. The edges of the femoral trochlear defect were smoothed and scant debris and small loose bodies were debrided. The knee was thoroughly irrigated before closure.
Postoperative MRI of the right knee showed anatomical alignment of the patella with an intact extensor mechanism (Figure 3). However, there was a new small non-displaced osteochondral fracture of the medial femoral trochlear. Given the retro patellar osteochondral injury, she was mobilising weight bear as tolerated in a ROM brace 0°-30°. The patient went on to have an uneventful postoperative journey, discharging 1-day post operatively after physiotherapy clearance. She was followed up in the fracture clinic at 1 week and 6 weeks with graded return to full ROM under physiotherapy guidance. The patient had an uneventful recovery and had returned to baseline function by the 6 weeks follow up.
At 9 months, the patient was mobilising well; however, experienced anterior knee pain. On examination the patient had ROM 0°-120° and patellofemoral joint crepitus. She had otherwise returned to her baseline function. Follow up X-rays demonstrated interval healing of the medial femoral trochlear fracture where the fracture line was not visualised and alignment was anatomical (Figure 4). Advanced patellofemoral compartmental development change was present and likely accounted for the patient’s knee pain.
Inferior dislocation of the patella was first described in 1887[4] and since then a 2020 literature review by Despotidis et al[4] described 64 cases having been reported including in the presence of a knee prosthesis[5]. These dislocations are divided into 2 groups based on the axis of rotation as described by Bankes and Eastwood[6]. The more common horizontal (type 1) adolescent type typically involves males in their second decade[6-10]. The patella is forced into the intercondylar notch from a direct blow and quadriceps muscle spasm results in injury or rupture at its attachment to the upper anterior surface of the patella[6,7,9]. This rotates the patella in the horizontal plane so the articular surface is orientated inferiorly[6,7]. This injury can be associated with collateral ligament or patellofemoral ligament injury[10,11].
This case represents the less common vertical (type 2) degenerative type which is associated with patella superior pole osteophytes impacting the femoral trochlear via two mechanisms[3,6]. One mechanism involves sudden quadriceps contraction with the knee flexed, driving the superior patella osteophytes into the femoral trochlear; while the other mechanism consists of an upward blow to the inferior pole of the patella[7]. The mechanism in this case likely represented a combination of a blow to the patella, where the knee was flexed as the patient fell. In either mechanism, the patella rotates on its vertical axis, so the articular surface faces medially or laterally, and becomes perched in a small depressed femoral trochlear fracture due to osteophytes at the superior pole of the patella[4,7]. Typically, there is no quadriceps tendon avulsion injury[6]. A differential diagnosis for this injury is an extensor mechanism injury such as quadriceps tendon rupture; however, in this situation, the quadriceps tendon stump is often readily palpable. In this scenario, MRI confirmed an intact extensor mechanism.
Imaging assessment should focus on the location and lie of the patella, for any fractures and the condition of the extensor mechanism[3]. MRI is valuable to evaluate the extent of the osteochondral injury, for the presence of ligamentous, tendon or meniscal injuries and for any intra-articular loose bodies, which may require arthroscopy or open repair[7,11,12]. However, reduction should not be delayed by the MRI[3]. Urgent reduction is warranted to reduce the risk of articular damage, soft tissue compromise and symptomatic relief. To differentiate between the types of dislocation, the key features are the lie of the patella, the presence of marginal osteophytes (type 2 injury) and whether there is a quadriceps insertional avulsion injury (type 1 injury)[4,6,7].
Management options vary and to our knowledge there are no strict recommendations for treatment of inferior patella dislocation. Options include closed reduction under a peripheral nerve block with sedation or reduction (closed or open) under general anaesthetic[3,7,13,14]. Typically, in the first instance, these injuries are managed with closed reduction in the Emergency Department under procedural sedation with a low threshold proceeding to theatre if this fails. Closed reduction can be successful in type 2 injuries due to osteophyte locking rather than true impaction; however, the likelihood of success depends on the depth and size of the osteochondral defect, and the degree of rotation of the patella[3,4,15]. Where there is less than 90 degrees of rotation of the patella when viewed in sagittal as in this case report, closed reduction can be considered[15].
As demonstrated in this case report, the patella was perched in a minimally depressed femoral trochlear fracture and traction by the quadriceps tendon likely contributed to its fixed position. The role of quadriceps traction is highlighted in a case report by Al Khalifa and Syed[16], where there was spontaneous reduction of an intra-articular patella dislocation likely due to quadriceps muscle fatigue resulting in diminished patella traction. Considering this, to avoid extensor mechanism rupture or osteochondral injuries, repeated attempts at closed reduction without adequate anaesthesia should be avoided[3].
Knee arthroscopy is valuable to evaluate for suspected additional joint injuries such as chondral injury or small intra-articular lose bodies for debridement, resection of osteophytes and smoothing of the impression zone to prevent recurrence[3,17]. This is highlighted in a case report by Barlow et al[17], where, after a successful closed reduction of a type 2 inferior dislocation, there was recurrence requiring open arthroscopic reduction with smoothing of a deep lateral femoral condyle ridge and resection of a patella osteophyte. While the injury in this report is similar with an identical degree of flexion deformity (80°), closed reduction with sedation was unsuccessful in this report, requiring general anaesthesia and muscle relaxation. This is similar to a case report by Choudhary and Tice[8].
Open reduction is recommended in type 1 injuries, where soft tissue injury is more likely in young patients due to lax patellar attachments, and this allows direct inspection and repair if required[4,9]. It is also indicated where closed reduction has failed, where a potentially large force is required for reduction as with deep osteochondral defects or greater than 90° of patella rotation or concomitant fractures requiring open reduction[8,15,16,18-21]. Unlike in this case report, type 2 injuries often require open reduction, where a 2020 literature review by Despotidis et al[4] described 58% requiring open reduction (37/64 patients), 31% having closed reduction (20/64 patients) and 11% being unspecified. An example of this is a case report by McHugh et al[15], where attempts at closed reduction with sedation and under general anaesthesia were both unsuccessful. This required a midline longitudinal incision extending proximally over the quadriceps tendon and traction on the patella using a bone hook at the upper pole to achieve reduction[15]. In contrast to the current case report, the knee was held in less flexion (40° vs 80°); however, the femoral trochlear defect appeared deeper when directly comparing preoperative X-rays.
Post reduction treatment varies, where some authors advocate for initial mobilisation spanning from 1-4 weeks, followed by gradual return to mobilisation in a brace with physiotherapy[3,6,10]. Others such as our patient have successfully mobilized, patients within 1 week with good long-term outcomes[4,17]. Bankes and Eastwood[6] suggest immobilisation of the affected limb in extension for 3-4 weeks for type 1 injuries, where quadriceps avulsion has occurred, and early mobilisation in type 2 injuries, where there is no soft tissue injury.
Inferior patella dislocation is rare and must be suspected in patients who present with a fixed flexion deformity of the knee. Initial workup should include assessment of the extensor mechanism, degree of rotation of the patella, the size of the osteochondral defect and exclusion of a fracture or soft tissue pathology, which may require an open operative repair. Post reduction prognosis is good, and return to mobilisation is dictated by the presence of fractures, ligamentous injury, or tendon injury.
| 1. | Wang H, Yi Z, Zhan H, Teng Y, Zhang S, Wu M, Geng B, Xia Y. A Scientometric Analysis of Studies on Patellar Dislocation. Orthop J Sports Med. 2022;10:23259671221137051. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Duthon VB. Acute traumatic patellar dislocation. Orthop Traumatol Surg Res. 2015;101:S59-S67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 102] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 3. | Zimmermann J, Grüninger P, Babians A, Zingg U. Unusual total knee immobilization in an elderly patient due to inferior patella dislocation: Case report and review of the literature. Trauma Case Rep. 2021;33:100481. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 4. | Despotidis V, Weihs J, Joseph Z, Gousopoulos L. Intra-articular horizontal dislocation of the patella: a rare injury and review of the literature. BMJ Case Rep. 2020;13:e232249. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Holton CS, Cohen AP. Intra-Articular Dislocation of Patella Following Patellofemoral Arthroplasty. J Med Cases. 2013;4:284-287. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Bankes MJ, Eastwood DM. Inferior dislocation of the patella in the degenerate knee. Injury. 2002;33:528-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Yoshioka S, Arai Y, Ikoma K, Fujita S, Akai T, Sakuragi R, Muneyasu K, Kubo T. Two cases of inferior dislocation of the patella with impaction into the femoral trochlea of osteophytes on the superior pole of the patella. Case Rep Orthop. 2013;2013:691739. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Choudhary RK, Tice JW. Intra-articular dislocation of the patella with incomplete rotation--two case reports and a review of the literature. Knee. 2004;11:125-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Kramer DE, Simoni MK. Horizontal intra-articular patellar dislocation resulting in quadriceps avulsion and medial patellofemoral ligament tear: a case report. J Pediatr Orthop B. 2013;22:329-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Pagdal S, Lande O, Jadhav U. Intra-articular dislocation of patella reduced by closed method - A rare case report. J Clin Orthop Trauma. 2016;7:118-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Miranda SF, Kupczik F, Schiavon MEG, Sbrissia B, Suzuki GYK. Horizontal Intraarticular Dislocation of the Patella: Case Report. Rev Bras Ortop (Sao Paulo). 2020;55:800-803. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 12. | Venkatesh Gupta SK, H P P, Prathik R, Jeetesh L. Traumatic Intra-articular Intercondylar Dislocation of the Patella Reduced by the Closed Method with Open Quadriceps Repair in an Adolescent: A Rare Case Report. Cureus. 2018;10:e3705. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 13. | Wight L, James D. Intra-Articular Patellar Dislocation: A Technique for Closed Reduction: A Case Report and Review of the Literature. JBJS Case Connect. 2017;7:e94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Morin WD, Steadman JR. Case report of a successful closed reduction without anesthesia. Clin Orthop Relat Res. 1993;179-181. [PubMed] [DOI] [Full Text] |
| 15. | McHugh G, Ryan E, Cleary M, Kenny P, O'Flanagan S, Keogh P. Intra-articular dislocation of the patella. Case Rep Orthop. 2013;2013:535803. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Al Khalifa A, Syed K. Intra-articular dislocation of patella with femoral impaction-A case report and review of literature. Int J Surg Case Rep. 2019;59:176-179. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 17. | Barlow D, Foong KS, Rhee SJ, Sutcliffe W, Griffin SJ. Recurrent locked knee caused by an impaction fracture following inferior patellar dislocation: a case report. J Med Case Rep. 2011;5:347. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Colville J. An unusual case of intra-articular dislocation of the patella. Injury. 1978;9:321-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Garrison RT, McCabe JB. An unusual case of intra-articular dislocation of the patella. Ann Emerg Med. 1984;13:557-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Gidden DJ, Bell KM. An unusual case of irreducible intra-articular patellar dislocation with vertical axis rotation. Injury. 1995;26:643-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 21. | Sarkar SD. Central dislocations of the patella. J Trauma. 1981;21:409-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |