Published online Nov 18, 2025. doi: 10.5312/wjo.v16.i11.112307
Revised: August 19, 2025
Accepted: October 10, 2025
Published online: November 18, 2025
Processing time: 113 Days and 16.7 Hours
The current method of cleaning and changing dressings for non-healing lumbar incisions post-radiotherapy is time-consuming and laborious, with very poor re
The patient was a 76-year-old female with lung cancer, positron emission tomo
Vacuum sealing drainage therapy has shown efficacy in treating nonhealing wounds after radiotherapy, promoting wound healing and reducing infection risk.
Core Tip: Treating non-healing lumbar incision post-radiotherapy is challenging, especially for midline incisions after lumbar spine surgery, which are difficult to heal. The current approach involves repeated wound cleaning and dressing changes, with unsatisfactory results. We used vacuum sealing drainage in a patient with radiation dermatitis who developed a non-healing wound after lumbar spinal surgery. The method is not only simple to perform but also shows clinical effectiveness. This is the first case of non-healing lumbar incision post-radiotherapy successfully treated using closed negative pressure drainage.
- Citation: Pan JL, Xing H, Li Y, Chang ZQ. Successful treatment of a non-healing lumbar incision post-radiotherapy using vacuum sealing drainage: A case report. World J Orthop 2025; 16(11): 112307
- URL: https://www.wjgnet.com/2218-5836/full/v16/i11/112307.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i11.112307
The incidence of poor wound healing after lumbar spinal surgery is high, which is a challenge for doctors. The incidence rate of poor wound healing after posterior lumbar surgery is reported to be 3.4%-24.4%. In a study of 1269 patients, the postoperative wound infection rate was 3.4%[1]. Another study showed that the rate of delayed wound healing after surgery was 24.4% in 954 patients[2]. Factors such as age, obesity, diabetes, hypertension, malnutrition, smoking, and alcohol consumption are also risk factors, and the midline incision during surgery is a major contributing factor due to poor blood supply and lack of muscle coverage in the subcutaneous tissue, leading to the formation of dead spaces.
In the aforementioned circumstances, wound nonhealing is more common after radiotherapy, making treatment more challenging. This results from tissue ischemia and fibrosis induced by radiotherapy. Radiation may also reduce regenerative capacity. The incidence rate of radiation dermatitis is high, with statistics showing that 87%-95% of patients receiving radiotherapy experience varying degrees of radiation dermatitis[3]. Clinical manifestations of radiation dermatitis range from mild erythema and dry desquamation to severe moist desquamation and ulcer formation. Severe radiation dermatitis affects the treatment and may lead to treatment interruption, affecting treatment outcomes[4]. Chronic radiation dermatitis is characterized by epidermal atrophy, thinning, loss of epidermal papillae, superficial dermal fibrosis, cellular necrosis, and is prone to causing nonhealing of postoperative wounds.
Surgery on the skin of patients with radiation dermatitis presents a formidable challenge, as tissue hypoxia, vascular damage, and reduced healing capacity resulting from radiation damage can lead to a significantly increased incidence of nonhealing surgical incisions[5]. The rate of poor wound healing following skin surgery post-radiotherapy can be as high as 30%-60%, surpassing that of regular surgeries[6]. Below, we present a case of a patient with a non-healing wound of approximately 15 cm at the lumbar spine incision site after radiotherapy. The wound successfully healed following treatment with vacuum sealing drainage (VSD).
A 76-year-old female presented to the spine clinic with unexplained lower back pain and bilateral leg pain while uri
Without any clear precipitating factors, the patient began to experience back pain and bilateral leg pain two months ago, which had been worsening over time. Local radiotherapy was administered at a different hospital, considering the possibility of a metastatic tumor.
The patient was diagnosed with lung cancer 6 years ago and underwent lung radiotherapy for 5 years. However, two months ago, she started experiencing back pain and a positron emission tomography/computed tomography scan revealed a high suspicion of metastasis to the L2/L3 vertebral bodies.
The patient denied any family history of malignant tumors.
Upon examination, severe lumbar spinal movement restriction was noted, along with tenderness and radiating pain at L2/L3, particularly on the left side. Muscle strength in both legs was decreased, and a positive straight leg raise test was observed on the left side.
Laboratory tests revealed an erythrocyte sedimentation rate of 54 mm/hour and a C-reactive protein of 32 mg/dL, with the rest of the examination results being essentially normal.
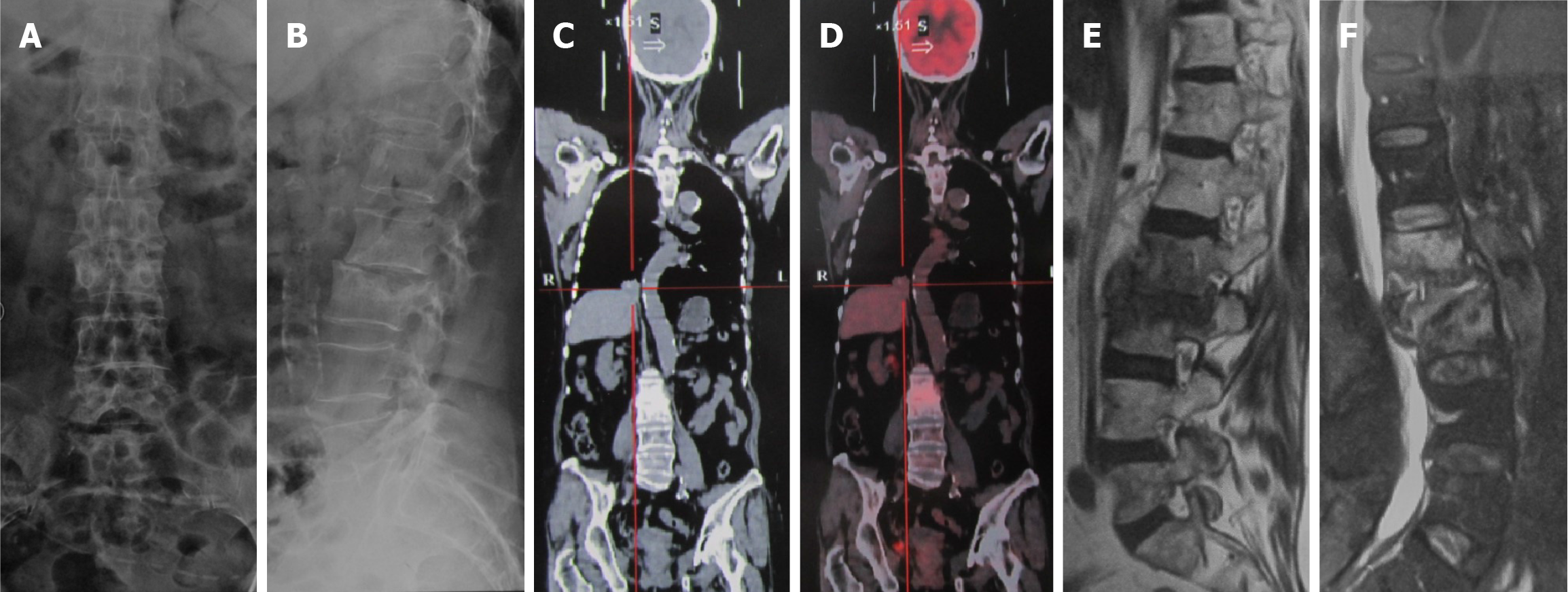
Lumbar spine lateral X-ray revealed visible destruction of L2 and L3 vertebral bodies with narrowing of the L2/L3 space (Figure 1A and B). Positron emission tomography/computed tomography suggested bone metastasis from lung cancer to L2 and L3 vertebrae (Figure 1C and D). Magnetic resonance imaging showed increased signals in L2 and L3 vertebral bodies and intervertebral space (Figure 1E and F).
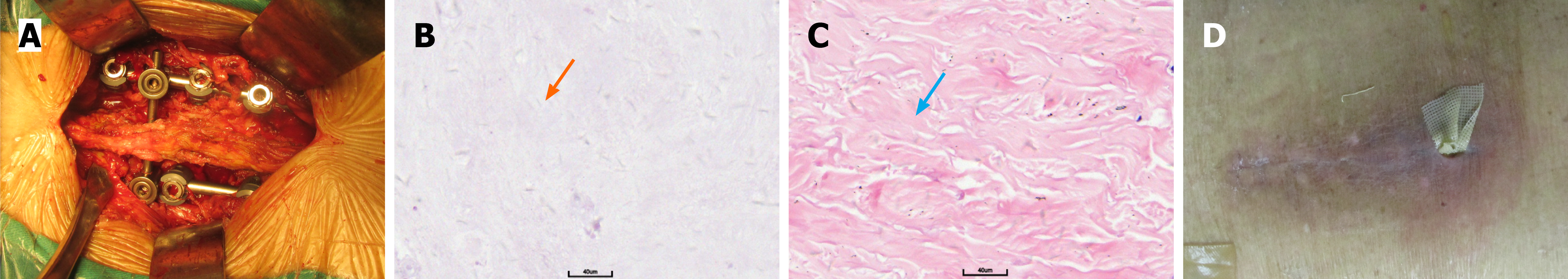
After completing preoperative examinations, the patient underwent lumbar decompression and internal fixation surgery. During the procedure, a window was opened on the left side of the L2/L3 vertebral body, revealing necrotic tissue in the dural sac and nerve root canal (Figure 2A). The intervertebral disc tissue was removed, the upper and lower cartilaginous endplates were scraped, and autologous bone grafts were implanted. Rapid pathology results showed bone, fibrous, and unstructured tissue. Postoperative pathology revealed significant proliferation of dermal sclerotic fibrous scar tissue with necrosis (Figure 2B and C). Multiple cultures of wound secretions and intraoperative tissues were negative for bacteria.
Based on the patient’s pathology findings and clinical presentation, the postoperative diagnosis was: Infection of the lumbar spine (L2/L3), and radiation dermatitis.
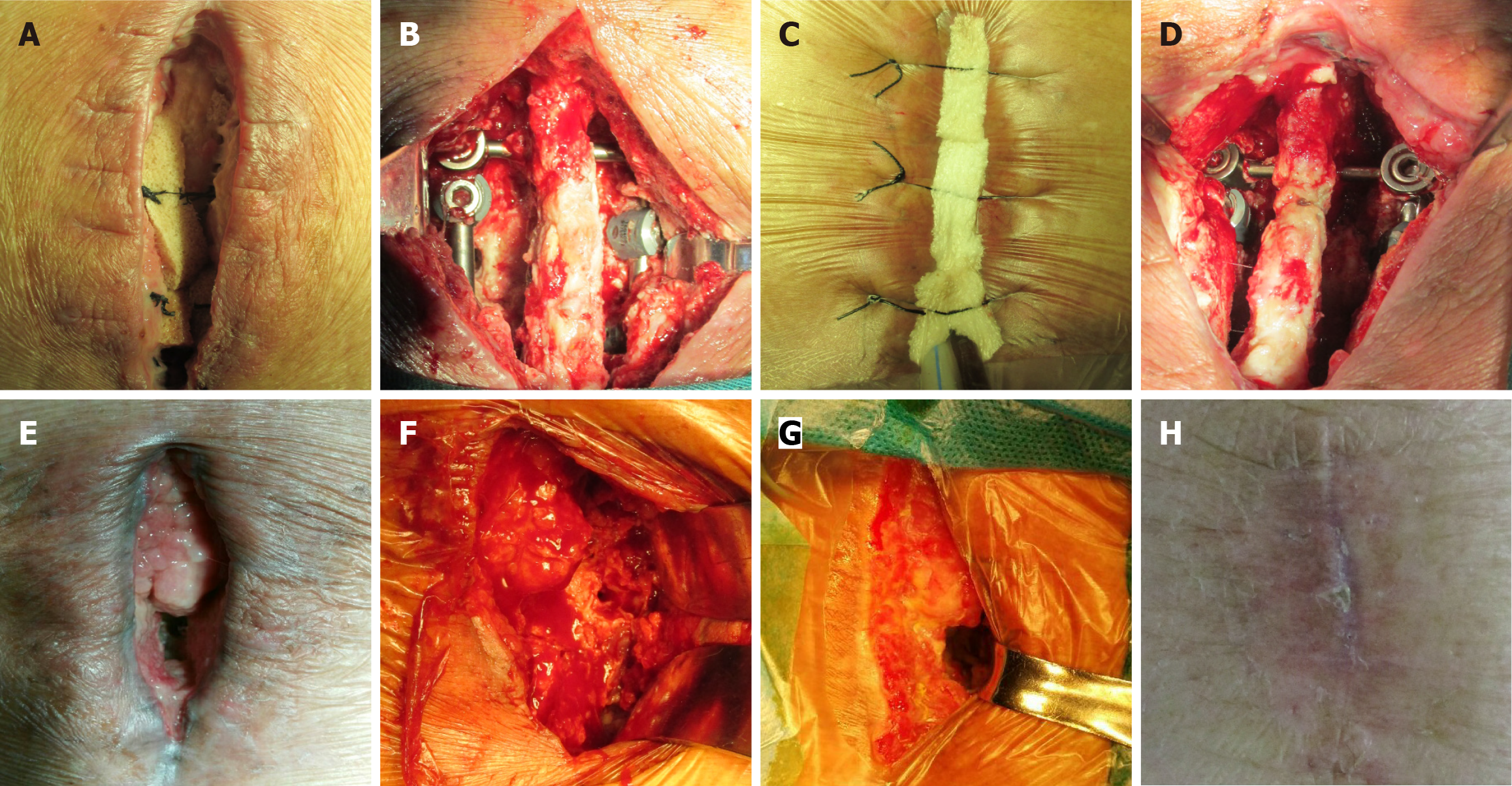
Two weeks after the operation, the incision showed signs of redness, swelling, and discharge, with exacerbation of local tissue necrosis. The lower end of the incision was not healing, accompanied by inflammatory exudate (Figure 2D). Immediate debridement was carried out, with the incision measuring 15 cm. The tissue inside the wound was necrotic and there was no active bleeding, accompanied by secretions. It is considered that hindrance of the healing process was due to the patient’s previous exposure to radiotherapy (total dose of 50 Gray in 25 fractions), resulting in inadequate local blood flow, coupled with postoperative infection. A sealed negative pressure drainage system (VSD) was placed at the incision site, and regular debridement and VSD replacement were performed every 5-7 days. VSD was connected to the hospital’s central negative pressure, maintaining a pressure of -125 mmHg and allowing for fluctuations. The outside was covered with a transparent occlusive membrane, without any additional dressings. The negative pressure compression status of the sponge was monitored in real time. The patient had no obvious pain, and the negative pressure drainage tube was 4-5 m long, which ensured that the patient could move around the bed. Following VSD treatment, the patient’s incision healed 78 days after surgery (Figure 3).
During the six months of follow-up, the patient’s wound continued to heal. After two years, there has been no breakdown or recurrence of the wound.
Non-healing of the lumbar incision after radiotherapy is a clinical challenge, especially in patients undergoing lumbar surgery, where tissue damage and poor blood supply caused by radiotherapy are important factors leading to poor incision healing. In addition, poor blood flow in the midline incision can lead to dead spaces[7]. Our patient had post-radiotherapy lumbar infection clearance, with increased wound secretion and local redness leading to non-healing of the wound. After initial assessment, the patient had a midline incision in the lumbar spine, and intraoperative pathology suggested chronic radiation dermatitis. It was decided to use VSD therapy. After 12 debridements and VSD therapy with a suction pressure set at -125 mmHg, the wound eventually healed after 78 days. The healing time was longer and the process was more difficult, highlighting the challenges of wound healing in radiation dermatitis.
Tissue damage following radiotherapy can affect wound healing[8]. Radiotherapy can lead to enhanced local tissue inflammation, impaired angiogenesis, and dysfunction of fibroblasts[9]. Prevention and treatment of radiation dermatitis have been a focus of clinical research. Various prevention and treatment strategies have been developed, including topical preparations, biological dressings, and various physical therapy methods[10]. However, once wound healing is compromised, treatment often becomes complex and challenging. Early intervention and personalized treatment plans have been shown to be crucial for improving outcomes[11]. There is currently no standardized approach for the treatment of non-healing wounds post-radiotherapy. Traditional treatment methods include local dressings and hyperbaric oxygen therapy, but the results are often unsatisfactory[12]. Compared to traditional methods, VSD demonstrates significant advantages. Clinically, negative pressure wound therapy promotes faster healing and superior granulation tissue formation through active fluid removal and improved microcirculation. Economically, while the initial setup cost is higher, it reduces the need for frequent dressing changes and can shorten hospital stays, leading to potential overall cost savings. Regarding patient comfort, negative pressure wound therapy provides a sealed, moist environment, resulting in less pain during dressing changes and greater mobility compared to conventional treatments.
VSD is an innovative wound treatment method that has developed in recent years. It uses continuous negative pressure to remove wound exudate, reduce local edema, eliminate infection factors and necrotic tissue, promote granulation tissue growth, improve local blood supply, and accelerate wound healing[13,14]. Multiple studies have confirmed that VSD has unique advantages in treating complex and difficult-to-heal wounds[15]. Recent research suggests that VSD may provide a new treatment option for these types of challenging wounds. VSD not only effectively controls infection and promotes wound healing, but also reduces patient discomfort and shortens hospital stay[8]. It is reported that continuous negative pressure can remove exudate, maintain wound cleanliness, promote local blood circulation, and improve tissue ischemia, mechanical stress stimulation can promote granulation tissue growth, and the closed environment can reduce the risk of infection[13]. VSD can promote the healing of surgical incisions after radiotherapy. This technology, through continuous negative pressure suction, can reduce wound exudate, promote vascular reconstruction, and accelerate granulation tissue growth[5].
This case suggests that surgery should be avoided on skin with radiation dermatitis, and if surgery is necessary, a midline incision should be avoided postoperatively. Based on the successful healing of the wound in this case, VSD treatment for nonhealing incisions after radiotherapy has been shown to be a simple and effective solution.
| 1. | Pei H, Wang H, Chen M, Ma L, Liu G, Ding W. Surgical site infection after posterior lumbar interbody fusion and instrumentation in patients with lumbar degenerative disease. Int Wound J. 2021;18:608-615. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 2. | An Y, Jiang J, Peng T, Zhao J, Xu H, Zhang X, Sun M, Zhao X. A New Predictive Nomogram for the Risk of Delayed Incision Healing After Open Posterior Lumbar Surgery: A Retrospective Study. Clin Spine Surg. 2023;36:E402-E409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 3. | Fang KC, Lee CH, Chuang HC, Huang TL, Chien CY, Tsai WL, Fang FM. Acute radiation dermatitis among patients with nasopharyngeal carcinoma treated with proton beam therapy: Prognostic factors and treatment outcomes. Int Wound J. 2023;20:499-507. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 4. | Guangmei D, Weishan H, Wenya L, Fasheng W, Jibing C. Evolution of radiation-induced dermatitis treatment. Clin Transl Oncol. 2024;26:2142-2155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 5. | Mohan A, Singh S. Use of fat transfer to treat a chronic, non-healing, post-radiation ulcer: a case study. J Wound Care. 2017;26:272-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 6. | Chung YL, Pui NN. Dynamics of wound healing signaling as a potential therapeutic target for radiation-induced tissue damage. Wound Repair Regen. 2015;23:278-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Wang J, Yang Y, Xing W, Xing H, Bai Y, Chang Z. Safety and efficacy of negative pressure wound therapy in treating deep surgical site infection after lumbar surgery. Int Orthop. 2022;46:2629-2635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 8. | Luu Y, Han J, Owji S, Kamat S, Luu C, Ungar J, Gulati N. Accelerated Healing from Severe Radiation Dermatitis Using Noncontact, Low-frequency Ultrasound-assisted Saline Wash Therapy. Adv Skin Wound Care. 2023;36:41-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 9. | Schäffer M, Weimer W, Wider S, Stülten C, Bongartz M, Budach W, Becker HD. Differential expression of inflammatory mediators in radiation-impaired wound healing. J Surg Res. 2002;107:93-100. [PubMed] |
| 10. | Rosenthal A, Israilevich R, Moy R. Management of acute radiation dermatitis: A review of the literature and proposal for treatment algorithm. J Am Acad Dermatol. 2019;81:558-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 120] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 11. | Hegedus F, Mathew LM, Schwartz RA. Radiation dermatitis: an overview. Int J Dermatol. 2017;56:909-914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 113] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 12. | Korpinar S, Cimsit M, Cimsit B, Bugra D, Buyukbabani N. Adjunctive hyperbaric oxygen therapy in radiation-induced non-healing wound. J Dermatol. 2006;33:496-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Liu J, Hu F, Tang J, Tang S, Xia K, Wu S, Yin C, Wang S, He Q, Xie H, Zhou J. Homemade-device-induced negative pressure promotes wound healing more efficiently than VSD-induced positive pressure by regulating inflammation, proliferation and remodeling. Int J Mol Med. 2017;39:879-888. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Xing H, Meng QF, Chang ZQ. [Mechanism of negative pressure wound therapy in the auxiliary treatment of bone and soft tissue infection]. Zhongguo Zuzhi Gongcheng Yanjiu. 2024;28:621-626. [DOI] [Full Text] |
| 15. | Kang SI, Kim S. The effectiveness of negative-pressure wound therapy for wound healing after stoma reversal: a randomized control study. Ann Surg Treat Res. 2023;105:126-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/