Published online Nov 18, 2025. doi: 10.5312/wjo.v16.i11.111903
Revised: September 22, 2025
Accepted: October 23, 2025
Published online: November 18, 2025
Processing time: 125 Days and 12.5 Hours
The accuracy of blind intra-articular injections in the shoulder is rather low. Inaccurate injections tend to lead to poorer treatment outcomes. The “Delaware posterior bone touch technique” has shown higher accuracy in young, slender, healthy volunteers than the classical “Cyriax technique”.
To investigate whether the Delaware technique would also be more accurate in older patients with capsulitis.
We analyzed the files of 100 consecutive patients with capsulitis who were treated with an intra-articular injection containing a mixture of triamcinolone, lidocaine, and air. After the injection, the shoulder was moved to determine whether a squishing sound could be produced. The squishing sound was interpreted as an accurate injection. The scores with the new Delaware technique were compared against those with the Cyriax technique in a previous study.
Squishing was heard after 87% of the injections. This was 13% (10% points) more than the 77% in the previous study (P = 0.004).
The Delaware technique was significantly more accurate than the Cyriax tech
Core Tip: Some of the fluid injected with the intention of injecting into the shoulder joint appears to end up next to the joint. This is often attributed to leakage. It appears that in a part of the injections, the fluid doesn't leak out of the joint, but is deposited next to it if part of the needle opening is located outside the capsule. A different injection technique appears to have significantly reduced this risk. Based on this idea, a different injection technique was chosen: The Delaware method. This significantly increases the chance of accurate injection compared to the traditional method.
- Citation: Mens JMA, Van Kalmthout RTM. Improving accuracy for intra-articular injections for capsulitis of the shoulder by changing the injection technique. World J Orthop 2025; 16(11): 111903
- URL: https://www.wjgnet.com/2218-5836/full/v16/i11/111903.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i11.111903
Intra-articular injections with steroids are common in the management of capsulitis. Recent studies showed that efficacy is strongly related to accuracy[1,2]. However, accuracy of blind applied injections is very variable. In a review the accuracy varied between 42% and 100%[3]. Various techniques are investigated to improve accuracy: (1) Anterior; (2) Posterior; and (3) Cranial[4-6]. Most studies that compared injection techniques did not show large differences in accuracy[3,5,6]. A striking difference between two techniques was found in the study of Axe and Axe[7]. They introduced the “Delaware posterior bone touch technique”. This technique improved accuracy from 70% to 97%. The essential difference between the classical posterior technique (as introduced by Cyriax and Russel[8]) and the Delaware technique was a small lateral rotation of the arm by the patient once the tip of the needle had touched the humeral head[7]. One of the limitations of their study was that participants were young, slender and healthy[7]. The authors wondered whether their technique would also improve the accuracy in case of capsulitis in older patients regardless of body mass.
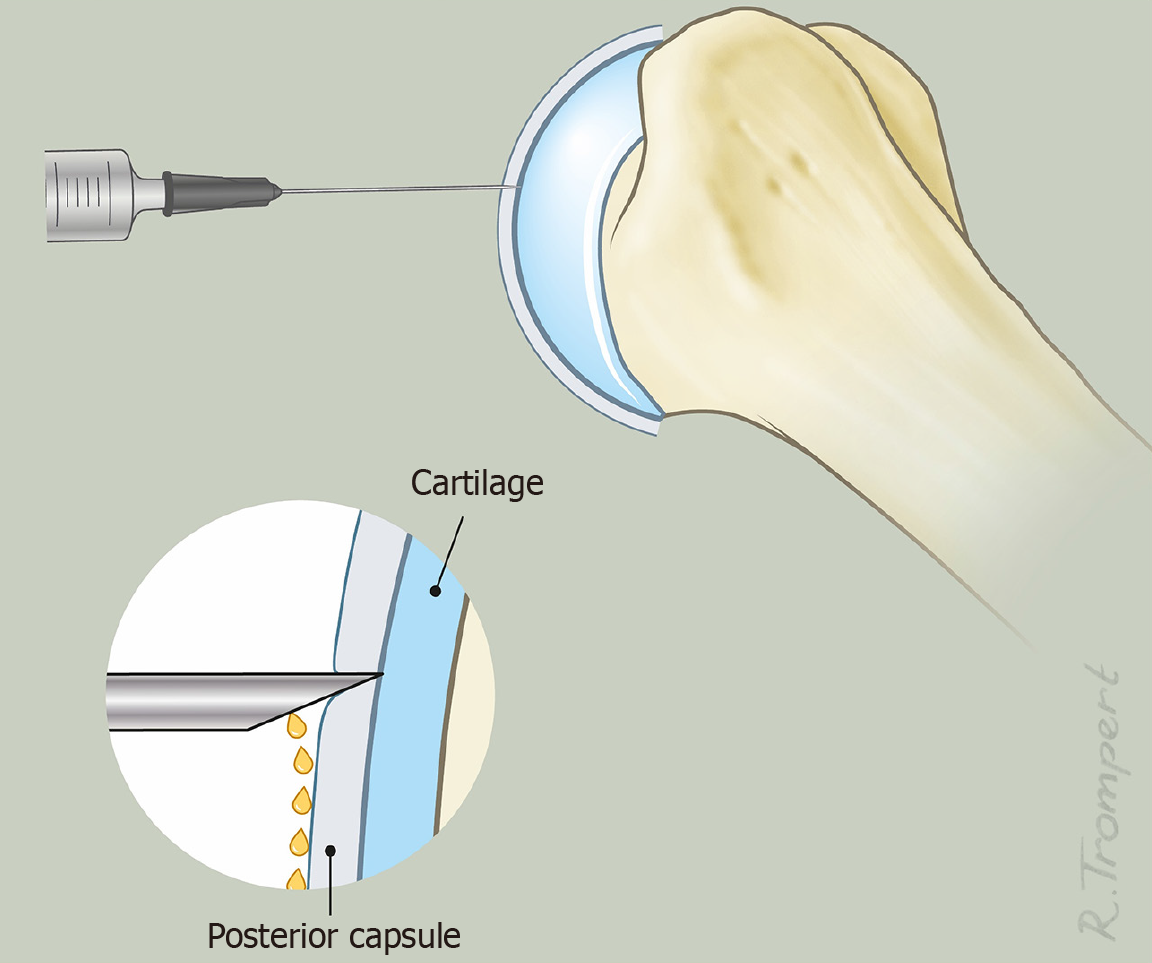
In most studies it has been assumed that the injection fluid is, partially or completely, placed outside the joint by two possible mechanisms: The opening of the needle is placed outside the joint or the injection was correct and the fluid leaks out of the joint after the procedure. As a third possibility we hypothesize that the fluid leaks out of the opening of the needle in case the tip of the needle has passed the capsule but a part of the opening is still outside the joint (Figure 1).
It seems that the Delaware technique lowers the risk that the opening of the needle is outside the joint. To enhance the result of their technique we adapted the technique by placing the opening of the needle in such a way that it faces laterally (Figure 2). The present study investigated whether, in patients with capsulitis, the accuracy of the adapted Delaware technique would be significantly higher than the 77% achieved in a previous study performed by the same investigators and with the classical posterior injection technique[2].
We retrospectively analyzed the files of 100 consecutive patients with freezing phase of capsulitis who were treated with the adapted Delaware injection technique. The patients were selected in the same outpatient clinic as in the previous study. The inclusion and exclusion criteria were the same as in our previous study[2]. Shortly this implicated: (1) Pain in the acromial region (with or without radiation into the arm); (2) Restriction of passive anteflexion, and active internal rotation; (3) At least a 20-degree restriction of passive lateral rotation and of glenohumeral abduction; (4) Pain at passive anteflexion as well as external and internal rotation; (5) No clinical signs of subacromial pain syndrome or osteoarthritis; and (6) No full-thickness rotator-cuff rupture and/or peri-articular calcifications larger than 3 mm on ultrasound examination. The research ethics committee of Erasmus University Rotterdam declared that, since the study was retrospective, no permission was needed.
All injections were applied by the same physician as in the previous study (Mens JMA). He had more than 30 years of clinical experience and performed roughly 200 intra-articular shoulder injections annually. He had been using the Delaware technique for approximately two years before the first patient was included in the current study. When using this technique, the patient sat with the arm in medial rotation by placing the lower arm on the trunk. Using a 50 mm 22 G needle, the skin was punctured 2 cm below the point where the acromion and the spine of the scapula meet. Care was taken to keep the bevel of the needle vertically, facing to the lateral side of the humeral head (see discussion). The needle was moved towards the tip of the coracoid process until the humeral head was clearly felt with the needle (Figure 3A). At that point, we asked the patient to move the arm slowly into slight lateral rotation (about 25-35 degrees) (Figure 3B). During this lateral rotation, care was taken to keep the needle firmly against the humeral head. In most cases, the needle advanced deeper into the body during this maneuver. With the arm in this position, a mixture of 0.5 mL of triamcinolone 40 mg/mL, 3.5 mL of lidocaine 1%, and 2 mL of air was injected.
After removing the needle, the physician moved the arm in medial rotation and lateral rotation and back in slight abduction to verify whether a squishing sound could be generated. The result, squishing or not, was recorded. The validity of the squishing sound as a check for accuracy was discussed in a previous study[2].
When calculating the sample size calculation, we assumed a significance level of α = 0.05 and a statistical power of 80%. However, considering a squishing rate (arbitrarily) 10% higher than the 77.05% reported in the previous study (i.e., 84.7%) as clinically meaningful, we estimated that a minimum of 4286 patients would be required to demonstrate a significant difference using a one-sided χ2 test. Consequently, a one-sample t-test was used. Relative risk (RR) and absolute risk reduction (ARR) were calculated and reported with 95%CI. Differences in patient characteristics compared to the previous study were calculated using an independent samples t-test (age), χ2 test (sex and diabetes) and Mann-Whitney U-test (non-normally distributed variables). Analyses were performed using Statistical Package for the Social Sciences version 27. A P < 0.05 was considered statistically significant.
The 100 patient files meeting the inclusion and exclusion criteria were gathered between January 1, 2019 and March 12, 2024. Information on squishing and patient characteristics was available for all 100 patients. There were no missing data. The patient characteristics where largely the same as those in our previous study (Table 1)[2]. Squishing was heard after 87% of injections. The percentage was 10% points more than the 77% recorded in our previous study (one-sample t-test two-sided P = 0.004). The RR for squishing was 1.13 (95%CI: 0.97-1.32). The ARR = 10.0% (95%CI: -2.5% to 22.4%).
| Variable | Present study | Previous study |
| Age in years, mean (SD) | 59 (10) | 60 (10) |
| Gender (women) (percentage) | 56 | 51 |
| Diabetes (percentage) | 7 | 8 |
| Duration of complaint in months, median (IQR) | 5 (4) | 5 (6) |
| Restriction of external rotation in degrees, median (IQR) | 40 (20) | 40 (20) |
| Restriction of abduction in degrees, median (IQR) | 40 (20) | 40 (15) |
The present study shows a statistically significant improvement in accuracy with the Delaware posterior bone touch technique over the classical Cyriax technique. Axe and Axe[7] compared the accuracy of these two injection techniques in young, slender, healthy volunteers. Their study found that the Delaware technique increased accuracy from 70% to 97% compared with the classical Cyriax technique[7]. The present study shows that improvement of accuracy is also achieved with this technique in middle-aged and older people with capsulitis regardless of body mass. The RR of 1.13 and the ARR of 10% were not statistically significant. However, a trend was found that the probability of a squishing sound was 13% higher and the probability of failure 10% lower with the Delaware technique compared to the Cyriax method.
We hypothesized that extra-articular fluid arises not necessarily from leakage out of the joint. We hypothesize that the fluid flows, at least partially, at the outside of the capsule when the opening of the bevel does not penetrate far enough through the shoulder capsule (Figure 1). A cadaveric study showed that the thickness of the place were posterior injections are given, the midportion of the posterior capsule, is the thinnest part of the whole capsule[9]. Ultrasound studies of healthy shoulders with the shoulder in a neutral position reported a mean thickness of the posterior capsule of 1.2 mm[10]. It may be assumed that the posterior capsule is even thinner when it is tensed and stretched by medial rotation. An ultrasound study among young healthy baseball players showed that thickness of the posterior capsule was 1.34 mm in throwing shoulders and 1.04 mm in non-throwing shoulders[11]. A study among patients with a frozen shoulder in the freezing stage showed a thickness of the posterior capsule of 1.3 mm; 0.4 mm thicker than at the healthy side[12].
The needles in the present study had a bevel opening that stretched 1.0-2.5 mm from the tip of the needle. So, if the needle penetrates the posterior capsule perpendicularly, a substantial part of the bevel opening may be outside the joint.
With a humeral head circumference of 15 cm, a 25-degree to 35-degree rotation displaces the tip of the needle by about 10-14 mm. This seems sufficient to drag the bevel opening completely into the joint (Figure 2). In our study, we made sure to orient the bevel opening laterally. This lateral orientation made the bevel opening face the cartilage, which leads theoretically to better injection placement than facing the capsule. After a small lateral rotation, the bevel of the needle is pulled under the joint capsule. Notice that the tip of the needle remains in contact with the cartilage during rotation.
In most studies inaccuracy is judged by the assessment of extra-articular contrast. It is striking to notice that the quality of the arthrogram is not necessarily compromised in case of extra-articular contrast[13]. This indicates that at least a part of the opening of the needle has entered the joint. The question is whether the presence of extra-articular fluid is the result of leakage out of the opening in the capsule, pierced by the removed needle, or by leakage out of the needle during the injection through a part of the opening of the needle outside of the capsule. Leakage through the opening in the capsule after removing of the needle is unlikely for several reasons. In the first place the capacity of the shoulder joint is large enough to store a small volume of injected fluid without increase of intra-articular pressure[14,15]. Secondly, magnetic resonance arthrography has shown that moving the arm after the injection does not influence the size or the appearance of extravasation[16,17]. Thirdly, extravasations in ultrasound guided posterior shoulder injections were much more frequent via perpendicular (out-of-plane) approach (47%) than via oblique (in-line) approach (13%)[18]. The size of the needles and the place where the capsule was pierced were similar. The authors assumed that the oblique route lowers the risk that a part of the opening of the needle is out of the capsule. The present study and the study of Axe and Axe[7] using the Delaware technique show that rotation of the arm after placing the needle enlarges the accuracy compared with the Cyriax method, while the needles and the places where the capsules are pierced are similar in both techniques. So, also the present study makes it unlikely to suppose that leakage of the fluid out of the capsule causes the difference. Leakage from the opening of the needle opening outside the joint seems more likely. It seems logical that leakages from the opening of the needle are not restricted to the shoulder. Leakage from the bevel may especially be expected if a needle with a large bevel is injected perpendicularly into a thin capsule.
Accuracy seems to be less dependent on the used technique than on the operator. A recent study on six publications showed that the average accuracy with the anterior approach was exactly the same as in studies using a posterior approach (87%). However, the wide variation between operators using the same technique, suggests that accuracy is substantially operator-dependent[6]. A study of three experienced and three inexperienced surgeons also found a large variation in accuracy between operators[5]. However, no correlation was found between accuracy and experience. For example, the average accuracy of anterior injections for three orthopedic surgeons with more than five years of ex
The strength of our study lies in its large sample size meeting strict inclusion criteria. The clinical setting, the physician administering the injections, the equipment, and the fluid used were the same as in the previous study. Therefore, the observed differences were not confounded by these factors. The limitations were that the investigator who assessed the squishing was not blinded to the injection technique and that the method of checking accuracy with the “squishing technique” is less validated than radiographic assessment. In the present sequential study, the patients had similar characteristics in both samples, however, a comparison in a prospective randomized trial would be more telling.
The present study indicates that a prospective randomized study should be performed to compare the injection techniques with radiographic control for correct placement. Besides accuracy it is important to investigate efficacy. A recent review showed that the anterior approach may be more beneficial in restoring shoulder range of motion at 12 weeks than the posterior approach[6].
The adapted Delaware posterior bone touch technique yielded a statistically significant improvement in intra-articular injection accuracy compared with the classical technique described by Cyriax and Russel[8]. The possible explanation is that leakage through the opening of the needle is prevented by dragging the bevel of the needle into the joint cavity by the small lateral rotation after the needle has passed through the capsule.
| 1. | Cheng X, Zhang Z, Wu M, Qiao L, Xu J, Lu M. A preliminary study of contrast-enhanced ultrasound guided capsule-preserving hydrodilatation in shoulder adhesive capsulitis. Quant Imaging Med Surg. 2024;14:4804-4814. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (1)] |
| 2. | Mens JMA, van Kalmthout RTM. Squishing sound heard following an intra-articular shoulder injection with fluid and air is associated with higher efficacy: A retrospective analysis. J Back Musculoskelet Rehabil. 2023;36:317-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 3. | Simoni P, Grumolato M, Malaise O, Preziosi M, Pasleau F, de Lemos Esteves F. Are blind injections of gleno-humeral joint (GHJ) really less accurate imaging-guided injections? A narrative systematic review considering multiple anatomical approaches. Radiol Med. 2017;122:656-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Rijs Z, de Groot PCJ, Zwitser EW, Visser CPJ. Is the Anterior Injection Approach Without Ultrasound Guidance Superior to the Posterior Approach for Adhesive Capsulitis of the Shoulder? A Sequential, Prospective Trial. Clin Orthop Relat Res. 2021;479:2483-2489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Tobola A, Cook C, Cassas KJ, Hawkins RJ, Wienke JR, Tolan S, Kissenberth MJ. Accuracy of glenohumeral joint injections: comparing approach and experience of provider. J Shoulder Elbow Surg. 2011;20:1147-1154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 46] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 6. | Rhim HC, Schon JM, Xu R, Schowalter S, Ha J, Hsu C, Andrew M, Robinson DM, Tenforde AS, Daneshvar DH. Targeting the Sweet Spot: A Systematic Review With Meta-Analysis of Anterior Versus Posterior Glenohumeral Joint Injections for Adhesive Capsulitis. Clin J Sport Med. 2025;35:1-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 7. | Axe JM, Axe MJ. 97% accuracy of intra-articular glenohumeral injection with a modified (Delaware) posterior bone touch technique. Del Med J. 2013;85:303-306; quiz 315. [PubMed] |
| 8. | Cyriax J, Russel G. Textbook of orthopaedic medicine volume 2: Treatment by manipulation massage and injection. 9th ed. London: Baillière Tindall, 1977: 164-166. |
| 9. | Ciccone WJ 2nd, Hunt TJ, Lieber R, Pedowitz R, Esch J, Tasto JP. Multiquadrant digital analysis of shoulder capsular thickness. Arthroscopy. 2000;16:457-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 31] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Tham ER, Briggs L, Murrell GA. Ultrasound changes after rotator cuff repair: is supraspinatus tendon thickness related to pain? J Shoulder Elbow Surg. 2013;22:e8-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Takenaga T, Sugimoto K, Goto H, Nozaki M, Fukuyoshi M, Tsuchiya A, Murase A, Ono T, Otsuka T. Posterior Shoulder Capsules Are Thicker and Stiffer in the Throwing Shoulders of Healthy College Baseball Players: A Quantitative Assessment Using Shear-Wave Ultrasound Elastography. Am J Sports Med. 2015;43:2935-2942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 82] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 12. | Wada T, Itoigawa Y, Yoshida K, Kawasaki T, Maruyama Y, Kaneko K. Increased Stiffness of Rotator Cuff Tendons in Frozen Shoulder on Shear Wave Elastography. J Ultrasound Med. 2020;39:89-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 13. | Rutten MJ, Collins JM, Maresch BJ, Smeets JH, Janssen CM, Kiemeney LA, Jager GJ. Glenohumeral joint injection: a comparative study of ultrasound and fluoroscopically guided techniques before MR arthrography. Eur Radiol. 2009;19:722-730. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 102] [Cited by in RCA: 86] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 14. | James-Belin E, Lasbleiz S, Haddad A, Morchoisne O, Ostertag A, Yelnik A, Laredo JD, Bardin T, Orcel P, Richette P, Beaudreuil J. Shoulder adhesive capsulitis: diagnostic value of active and passive range of motion with volume of gleno-humeral capsule as a reference. Eur J Phys Rehabil Med. 2020;56:438-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Ogul H, Tas N, Tuncer K, Polat G, Ogul Y, Pirimoglu B, Kantarci M. 3D volumetric MR arthrographic assessment of shoulder joint capacity in patients with primary adhesive capsulitis. Br J Radiol. 2019;92:20180496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Muylaert C, Boulet C, Buls N, Wuertzer S, Pouliart N, Machiels F, De Maeseneer M. Does Immobilization Post Injection Reduce Contrast Extravasation in MR Arthrography of the Shoulder? Can Assoc Radiol J. 2022;73:164-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 17. | Brenner ML, Morrison WB, Carrino JA, Nusser CA, Sanders TG, Howard RF, Meier P. Direct MR arthrography of the shoulder: is exercise prior to imaging beneficial or detrimental? Radiology. 2000;215:491-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Tsoi C, Tsai CSC, Law EKC, Lee RKL, Ng AWH, Griffith JF. A comparison of ultrasound-guided rotator interval and posterior glenohumeral injection techniques for MR shoulder arthrography. Clin Imaging. 2021;69:255-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/