Published online Sep 18, 2024. doi: 10.5312/wjo.v15.i9.850
Revised: July 24, 2024
Accepted: August 13, 2024
Published online: September 18, 2024
Processing time: 136 Days and 3.3 Hours
Childhood obesity has emerged in the last decades as an important public health problem worldwide. Although relationships between obesity and flatfoot have been shown, no studies have investigated the influence of obesity on arthroereisis outcomes.
To evaluate correlations between childhood overweight/obesity and clinical and radiographic outcomes after subtalar arthroereisis with self-locking implants.
This retrospective study included one hundred and sixty-nine pediatric patients (10-14 years old) who underwent subtalar arthroereisis (PEEK PitStop® device) for severe flexible flatfoot. Exclusion criteria were additional procedures, revision of previous corrective surgeries, rigid flatfoot with severe deformity, and neurologi
EFAS and VAS scores improved post-operatively in the whole population. Only seven cases with complications were reported. Radiographic assessment revealed an improvement in all angles. Statistical analysis demonstrated that the impact of obesity was significant on arthroereisis outcomes: Relationships were reported between BMI and postoperative EFAS/VAS scores, postoperative calcaneal pitch angle, Kite angle, Meary angle and talo-first meta
Although arthroereisis represents a very effective and valid treatment for flatfoot both in normal weight and obese children, obesity significantly influences clinical and radiographic outcomes of arthroereisis, and obese children tend to perceive more pain and discomfort.
Core Tip: Childhood obesity has emerged in the last decades as an important public health problem worldwide. It has been demonstrated that pediatric flatfoot is also related to obesity, showing a two-fold higher risk compared to normal weight children. While the relationship between obesity and flatfoot has been well established, only a few studies have reported the relationships between childhood obesity and arthroereisis outcomes and no studies have assessed the outcomes of self-locking implants and obesity. The aim of the present study is to evaluate correlations between childhood overweight/obesity and clinical and radiographic outcomes after subtalar arthroereisis with self-locking implants.
- Citation: Monestier L, Riva G, Latiff M, Marciandi L, Bozzi E, Pelozzi A, Pautasso A, Pilato G, Surace MF, D'Angelo F. Pediatric flexible flatfoot: Does obesity influence the outcomes of arthroereisis? World J Orthop 2024; 15(9): 850-857
- URL: https://www.wjgnet.com/2218-5836/full/v15/i9/850.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i9.850
Childhood obesity has emerged in the last decades as an important public health problem worldwide. Recent data suggest that over 383 million individuals under 19 years of age may be affected in 2035, compared with over 175 million in 2020. The prevalence of obesity alone may increase from 14% to 24% of the population over the same period[1].
Childhood overweight/obesity is defined by body mass index (BMI) ≥ 25 kg/m² for overweight, and BMI ≥ 25 kg/m² for obesity, which is adjusted according to age and gender. While BMI between the 85th and 94th percentile is in the ‘overweight’ range, the BMI 95th percentile is in the ‘obese’ range[2].
Obesity is caused by excessive caloric intake; many factors may contribute including behavior, genetics, care and school environments, availability of affordable and healthy foods or beverages, and accessibility to places for physical activity[2,3].
As reported by the World Obesity Atlas in 2023, approximately 241 million children and adolescents (5-19 years old) are currently overweight or obese worldwide[1]. This scenario has been aggravated by the coronavirus disease 2019 pandemic; A recent study reported an 8.7% increase in childhood overweight and obesity during the pandemic[4]. The economic impact of childhood obesity is significant, including both the healthcare costs of treating obesity and its con
Literature has demonstrated that childhood overweight/obesity may lead to adulthood disorders such as chronic diseases, mental health problems, diabetes, cardiovascular disease, and some types of cancer[5,6]. Moreover, children with overweight/obesity may have a higher risk of musculoskeletal disorders such as slipped capital femoral epiphysis, Blount’s disease, and genu valgum, with an increased risk of fractures and musculoskeletal pain[7-11].
It has been demonstrated that pediatric flatfoot (pes planus) is also related to obesity, showing a two-fold higher risk compared to normal weight children[7,12-16]. Chen et al[14] found a significant difference in the prevalence of flatfoot between normal-weight (27%), overweight (31%) and obese (56%) children[14]. Cimolin et al[16] also reported a 70% rate of flatfoot in obese adolescents compared to 25% in the normal weight group[16].
The relationship between childhood obesity and flatfoot is still unknown. Mickle et al[17] asserted that higher rates of flatfoot in obese children may be explained by structural changes in the foot rather than the presence of thicker fat tissue under the midfoot region[17]. Moreover, Riddiford-Harland et al[18] showed that obese children have significantly gr
In the treatment of pediatric flatfoot, subtalar arthroereisis has been reported as a minimally invasive, effective, and low-risk procedure[20-22]. Described firstly by Chambers[23] in 1946 and then by Lelievrè[24] in 1970, subtalar arthroe
While the relationship between obesity and flatfoot has been well established, only a few studies have reported the relationship between childhood obesity and arthroereisis outcomes. Pavone et al[27] reported results following calcaneo-stop implants[27], but no studies have investigated the outcomes of self-locking implants and obesity.
The aim of the present study is to evaluate correlations between childhood overweight/obesity and clinical and ra
One hundred and sixty-nine pediatric patients (10-14 years old) underwent subtalar arthroereisis between February 2020 and April 2022 at the Pediatric Orthopedics Unit of the ASST Settelaghi in Varese, the only pediatric orthopedic depart
Surgery was indicated in patients presenting with flexible flatfoot, normal-aligned limbs and symptomatic flatfoot (foot pain during daily or sport activities, early muscle fatigue, disability in running or sport activity), severe grade (III-IV degree) or with critical malalignment of the hindfoot or a hindfoot valgus > 8°.
Exclusion criteria were introduced in order to reduce possible biases that may interfere with our purpose, which was to evaluate correlations between childhood obesity and outcomes after subtalar arthroereisis in flexible flatfoot in those aged < 10 years or > 14 years. Although there is no consensus on the age for surgery, performing subtalar arthroereisis before the age of ten may be too early, as nonsurgical management has been demonstrated to be efficient and should be pursued[28-30]; patients over 14 years were excluded because several authors have reported that the foot is defined ‘mature’ at the age of fourteen, with cessation of growth, closure of growth plates and stabilization of posture[31-33]. Patients under
Thirty-one (35.2%) females and fifty-seven (64.8%) males were included in the study. Mean follow-up was 17.03 months (range 8.9-34.7).
Bilateral subtalar arthroereisis was performed in all cases using an anatomical PEEK PitStop® endorthesis (In2Bones, Memphis, TN, United States) (Figure 1). At the end of the procedure, a boot plaster was placed, and the patient was invited to walk immediately with canes. The cast was removed after three weeks, and the patient was free to walk with comfortable footwear; an exercise protocol was given to the patients to help return-to-walk. Activities with a high risk of ankle sprain (i.e., running, jumping) were prohibited for the first two postoperative months: Only swimming and cycling were permitted.
Daily sport activities were allowed two months after surgery. Specific physiotherapy was indicated in the case of disability in walking or incomplete/unsatisfactory correction.
Patients were assessed preoperatively and postoperatively at 20 days, 60 days, and at the time of the study (mean 17.03 months, range 8.9-34.7). Preoperatively, the weight, height, and BMI of each patient were also determined.
Clinical evaluation included the following: Valgus position of the heel in orthostatism, gait analysis, functional tests (Silfverskiold test, the toe rising test, Jack test), and footprint on the podoscope. Moreover, the European Foot and Ankle Society (EFAS) and visual analogue scale (VAS) scores were obtained preoperatively and postoperatively: These scores were chosen as they are universally validated, also in the Italian language[34-36]. The EFAS score concerns six items relating to activities of daily living and four relating to the performance in sports. The VAS scale is an instrument for measuring pain experienced by the patient.
Weight-bearing foot X-rays were obtained, analyzed and compared preoperatively and postoperatively with Synapse® software (FUJIFILM Medical Systems United States).
In the antero-posterior view, Kite angle (between lines drawn down the axes of the talus and calcaneus) and first metatarsal-talus angle (between longitudinal axes of first metatarsal and talar neck) were calculated. In the lateral projection, Meary angle (between the longitudinal axes of the talus and the first metatarsal), calcaneal pitch angle (between the calcaneal inclination axis and the supporting horizontal surface) and lateral talo-calcaneal angle (between axes of the talus and calcaneus) were analyzed.
Data were analyzed using SPSS version 24.0 software (IBM, Armonk, NY, United States). The descriptive statistics were expressed by the use of means, SDs and frequencies. For the comparison of means, Student's t-tests were used with independent samples or with paired samples for the variables with normal distribution. In addition, statistical correlations between variables were identified by t-test; then, by means of linear regression, the trend of each parameter was analyzed as the other variables changed, obtaining R2. Statistical significance was set at P < 0.05.
Mean age at surgery was 12.20 years (range, 10.15-14.48): Seventeen 10-year-old children (19.40%), twenty-four 11-year-old children (24.10%), twenty-two 12-year-old children (33.90%), nineteen 13-year-old children (17.80%), and six 14-year-old children (4.80%).
Mean BMI at the time of surgery was 20.69 (range: 14.08-29.34, SD: 3.44). Forty-two patients had a BMI < 18 kg/m² (23.8%), one hundred and twelve were normal weight (63.6%) and twenty-two were obese (22.6%).
The following PitStop® PEEK endorthesis sizes were used: Size 10 in four cases (2.3%), size 11 in thirty-three cases (18.8%), size 12 in seventy-two cases (40.9%), size 13 in sixty-three cases (35.8%), and size 14 in four cases (2.3%).
EFAS and VAS scores are reported in Table 1. The mean preoperative EFAS score was 17.73 points (range, 2.00-40.00); postoperatively, the average score was 34.38 points (range, 18.00-40.00); as a result, the mean score increase was 16.65 points (range, 15.80-17.49, P = 0.001).
| Average | Min | Max | SD | SE | Sig (P < 0.05) | ||
| EFAS score | Pre | 17.73 | 2.00 | 40.00 | 5.74 | 0.433 | |
| Post | 34.38 | 18.00 | 40.00 | 4.08 | 0.308 | ||
| Δ EFAS | -16.65 | -16.00 | 0.00 | 5.69 | 0.429 | 0.001 | |
| VAS score | Pre | 6.38 | 0.00 | 10.00 | 2.48 | 0.187 | |
| Post | 1.98 | 0.00 | 6.00 | 1.23 | 0.117 | ||
| Δ VAS | -4.40 | 0.00 | -4.00 | 2.36 | 0.179 | 0.001 | |
The mean preoperative VAS score was 6.38 points (range, 0.00-10.00); postoperatively, the average score was 1.98 points (range, 0.00-6.00); as a result, the mean score increase was 4.4 points (range, 4.04-4.75, P = 0.001).
A few complications were reported: Six cases had superficial wound dehiscence (3.4%) and only one case required implant removal by surgery after three years due to ankle sprain during national gymnastics games (1.2%). Normal weight children reported four of six dehiscences and implant removal, without any significant differences to obese patients (P = 0.697). Physiotherapy was indicated in thirty patients (34.1%) due to disability in walking or sports.
Radiographic data are reported in Table 2. The mean preoperative Kite angle was 25.11° (range, 10.00-39.00); postoperatively, the mean angle was 20.78° (range, 11.00-33.00); as a result, the average reduction was 4.33° (SD 3.52; P = 0.001); the mean preoperative first metatarsal-talus angle was 7.86° (range, 1.00-31.00); postoperatively, the mean angle was 4.99° (range, 0.00-15.00); as a result, the average reduction was 2.86° (SD 4.19; P = 0.001).
| Average | Min | Max | SD | SE | Δ value | SD | SE | Sig (P < 0.05) | ||
| Calcaneal pitch angle | Pre | 15.52 | 8.00 | 27.00 | 3.18 | 0.240 | 3.31 | 2.38 | 0.179 | 0.001 |
| Post | 18.83 | 7.00 | 33.00 | 4.37 | 0.330 | |||||
| Talo-Calcaneal angle | Pre | 37.52 | 28.00 | 54.00 | 4.32 | 0.329 | -5.77 | 4.55 | 0.344 | 0.001 |
| Post | 31.75 | 22.00 | 42.00 | 3.64 | 0.275 | |||||
| Meary angle | Pre | 7.35 | 1.00 | 21.00 | 4.02 | 0.303 | -3.91 | 3.80 | 0.287 | 0.001 |
| Post | 3.44 | 0.00 | 18.00 | 2.85 | 0.215 | |||||
| Kite angle | Pre | 25.11 | 10.00 | 39.00 | 5.22 | 0.394 | -4.33 | 3.52 | 0.265 | 0.001 |
| Post | 20.78 | 11.00 | 33.00 | 4.37 | 0.330 | |||||
| Talo-M1 angle | Pre | 7.86 | 1.00 | 31.00 | 4.32 | 0.330 | -2.86 | 4.19 | 0.316 | 0.001 |
| Post | 4.99 | 0.00 | 15.00 | 3.01 | 0.227 |
The mean preoperative Meary angle was 7.35° (range, 1.00-21.00); postoperatively, the mean angle was 3.44° (range, 0.00-18.00); as a result, the average reduction was 3.91° (SD 3.80; P = 0.001); the mean preoperative calcaneal pitch angle was 15.52° (range, 8.00-27.00); postoperatively, the mean angle was 18.83° (range, 7.00-33.00); as a result, the average in
Statistical analysis demonstrated a significant correlation between BMI < 25 kg/m² and BMI > 25 kg/m² (P < 0.05), and postoperative VAS: Normal weight patients 1.88 points; obese patients 2.64 points (P = 0.001); postoperative EFAS: Normal weight patients 31.09 points; obese patients 34.84 points (P = 0.048); postoperative Kite angle: Normal weight patients 20.32°, obese patients 23.95° (P = 0.005).
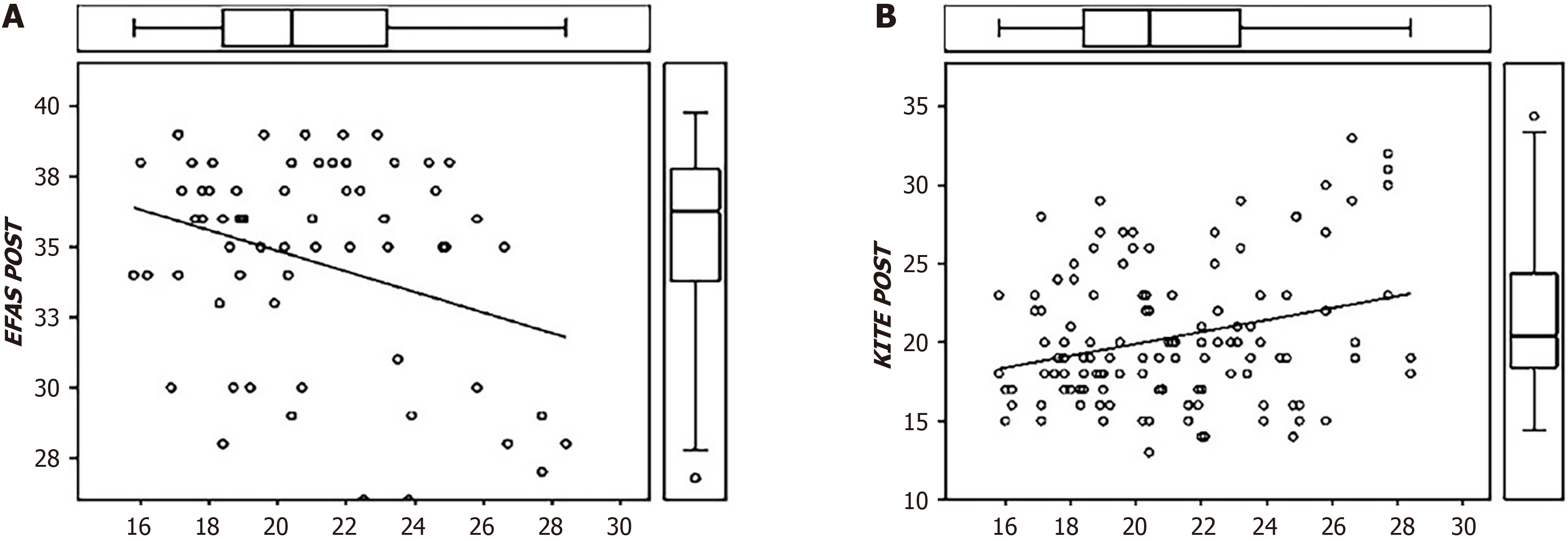
Relationships between BMI and postoperative EFAS score, postoperative VAS, postoperative calcaneal pitch angle, postoperative Kite angle, postoperative Meary angle and postoperative talo-first metatarsal angle were analyzed by linear regression: Postoperative EFAS score tended to decrease as BMI increased (P = 0.001; SE coefficient 2.081; R2 corrected 0.095) (Figure 2A). Postoperative VAS score did not appear to be affected by BMI trends.
Postoperative calcaneal pitch decreased as BMI increased (P = 0.001; SE coefficient 2.493; R2 corrected -0.007); the postoperative Kite angle also seemed to have a clinically agreeable behavior, as the angle tended to increase with increased BMI (P = 0.003; SE coefficient 1.802; R2 corrected 0.003) (Figure 2B). Finally, the postoperative Meary angle tended to increase as the patient's BMI increased (P = 0.001; SE coefficient 2.563; R2 corrected 0.067). No other statistically significant trends were detected.
Childhood obesity currently represents an important public health problem. Among other severe consequences, pediatric flatfoot has also been demonstrated to be related to obesity[7,12-15].
It has been shown that pediatric flatfoot (pes planus) is also related to obesity, with a two-fold higher risk compared to normal weight children[7,12-16]. The relationship between childhood obesity and flatfoot is still unknown. The structural and morphological changes reported in obese children with flatfeet are associated with compromised function in gait and activities[17,19].
In the treatment of pediatric flatfoot, subtalar arthroereisis has been reported as a minimally invasive, effective, and low-risk procedure[20-22].
Our study demonstrated that this surgical procedure is very effective in the treatment of symptomatic and flexible flatfoot: The EFAS score significantly increased and the VAS score significantly decreased after arthroereisis (P < 0.001), with general satisfaction in children and parents. Similarly, all angles measured significantly improved in the whole pediatric population (P = 0.0011). Our favorable results are similar to those reported in several other studies[37-44].
Regarding complications, we reported a rate of only 4.6%: The most common complication was superficial dehiscence treated with simple medications. Our results are in line with those from other studies, with complication rates ranging from 4.8% to 19.3%[20,45,46]. It is our opinion that superficial wound dehiscence is caused by the cast as sweating is fre
As demonstrated by the statistical analyses, obesity has a significant influence on both clinical and radiographic outcomes of subtalar arthroereisis: BMI over 25 kg/m² is significantly correlated with worse postoperative EFAS and VAS scores (P < 0.05). Also, postoperative angles show worse values in obese patients: Postoperatively, the calcaneal pitch, Kite angle, and Meary angle were significantly influenced (P < 0.05).
Few studies have reported the relationship between childhood obesity and the corrective potential of arthroereisis: Only Pavone reported results after calcaneo-stop implants[27], but no studies have reported the outcomes of self-locking implants.
As the goniometric improvements, with the exception of the Kite angle, were substantially similar in normal weight/overweight children, subtalar arthroereisis is effective in treating flexible flatfoot in both populations. However, the following question might arise: Is it worth performing this surgical procedure in overweight children? Based on our re
Nevertheless, our results allow us to assert that subtalar correction due to arthroereisis requires greater effort in over
Subtalar arthroereisis is effective in treating flexible flatfoot both in normal weight and obese populations. Nonetheless, obesity significantly influences clinical and radiographic outcomes and obese children tend to perceive more pain and discomfort.
| 1. | World Obesity Federation. World Obesity Atlas 2023. Mar 2023. [cited 3 August 2024]. Available from: https://s3-eu-west-1.amazonaws.com/wof-files/World_Obesity_Atlas_2023_Report.pdf. |
| 2. | Centers for Disease Control and Prevention. About Obesity. 2022. [cited 3 August 2024]. Available from: https://www.cdc.gov/obesity/php/about/index.html. |
| 3. | Kumar S, Kelly AS. Review of Childhood Obesity: From Epidemiology, Etiology, and Comorbidities to Clinical Assessment and Treatment. Mayo Clin Proc. 2017;92:251-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 678] [Cited by in RCA: 918] [Article Influence: 102.0] [Reference Citation Analysis (0)] |
| 4. | Woolford SJ, Sidell M, Li X, Else V, Young DR, Resnicow K, Koebnick C. Changes in Body Mass Index Among Children and Adolescents During the COVID-19 Pandemic. JAMA. 2021;326:1434-1436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 214] [Article Influence: 42.8] [Reference Citation Analysis (0)] |
| 5. | Jia P. Obesogenic environment and childhood obesity. Obes Rev. 2021;22 Suppl 1:e13158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 6. | Sadeghi-Demneh E, Azadinia F, Jafarian F, Shamsi F, Melvin JM, Jafarpishe M, Rezaeian Z. Flatfoot and obesity in school-age children: a cross-sectional study. Clin Obes. 2016;6:42-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Stolzman S, Irby MB, Callahan AB, Skelton JA. Pes planus and paediatric obesity: a systematic review of the literature. Clin Obes. 2015;5:52-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 47] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 8. | de Sá Pinto AL, de Barros Holanda PM, Radu AS, Villares SM, Lima FR. Musculoskeletal findings in obese children. J Paediatr Child Health. 2006;42:341-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 80] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 9. | Stovitz SD, Pardee PE, Vazquez G, Duval S, Schwimmer JB. Musculoskeletal pain in obese children and adolescents. Acta Paediatr. 2008;97:489-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 110] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 10. | Paulis WD, Silva S, Koes BW, van Middelkoop M. Overweight and obesity are associated with musculoskeletal complaints as early as childhood: a systematic review. Obes Rev. 2014;15:52-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 168] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 11. | Taylor ED, Theim KR, Mirch MC, Ghorbani S, Tanofsky-Kraff M, Adler-Wailes DC, Brady S, Reynolds JC, Calis KA, Yanovski JA. Orthopedic complications of overweight in children and adolescents. Pediatrics. 2006;117:2167-2174. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 304] [Cited by in RCA: 271] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 12. | Pfeiffer M, Kotz R, Ledl T, Hauser G, Sluga M. Prevalence of flat foot in preschool-aged children. Pediatrics. 2006;118:634-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 277] [Cited by in RCA: 278] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 13. | Tenenbaum S, Hershkovich O, Gordon B, Bruck N, Thein R, Derazne E, Tzur D, Shamiss A, Afek A. Flexible pes planus in adolescents: body mass index, body height, and gender--an epidemiological study. Foot Ankle Int. 2013;34:811-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 14. | Chen JP, Chung MJ, Wang MJ. Flatfoot prevalence and foot dimensions of 5- to 13-year-old children in Taiwan. Foot Ankle Int. 2009;30:326-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 69] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 15. | Butterworth PA, Landorf KB, Gilleard W, Urquhart DM, Menz HB. The association between body composition and foot structure and function: a systematic review. Obes Rev. 2014;15:348-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Cimolin V, Capodaglio P, Cau N, Galli M, Pau M, Patrizi A, Tringali G, Sartorio A. Foot-type analysis and plantar pressure differences between obese and nonobese adolescents during upright standing. Int J Rehabil Res. 2016;39:87-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Mickle KJ, Steele JR, Munro BJ. The feet of overweight and obese young children: are they flat or fat? Obesity (Silver Spring). 2006;14:1949-1953. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 121] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 18. | Riddiford-Harland DL, Steele JR, Baur LA. Medial midfoot fat pad thickness and plantar pressures: are these related in children? Int J Pediatr Obes. 2011;6:261-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 19. | Riddiford-Harland DL, Steele JR, Storlien LH. Does obesity influence foot structure in prepubescent children? Int J Obes Relat Metab Disord. 2000;24:541-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 96] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 20. | Bernasconi A, Lintz F, Sadile F. The role of arthroereisis of the subtalar joint for flatfoot in children and adults. EFORT Open Rev. 2017;2:438-446. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 74] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 21. | De Pellegrin M, Moharamzadeh D. Subtalar Arthroereisis for Surgical Treatment of Flexible Flatfoot. Foot Ankle Clin. 2021;26:765-805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 22. | Vulcano E, Maccario C, Myerson MS. How to approach the pediatric flatfoot. World J Orthop. 2016;7:1-7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (2)] |
| 23. | Chambers EF. An operation for the correction of flexible flat feet of adolescents. West J Surg Obstet Gynecol. 1946;54:77-86. [PubMed] |
| 24. | LeLièvre J. Current concepts and correction in the valgus foot. Clin Orthop Relat Res. 1970;70:43-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 25. | Subotnick SI. The subtalar joint lateral extra-articular arthroereisis: a preliminary report. J Am Podiatry Assoc. 1974;64:701-711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 26. | Vogler H. Subtalar joint blocking operations for pathological pronation syndromes. In: McGlamery ED, editor. Comprehensive textbook of foot surgery. Baltimore: Williams & Wilkins, 1987: 466-482. |
| 27. | Pavone V, Vescio A, Canavese F, Costa D, Sessa G, Testa G. Effects of body weight on the clinical and radiological outcomes of children with flexible flatfeet managed with the 'calcaneo-stop' procedure. J Pediatr Orthop B. 2019;28:228-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 28. | Ford SE, Scannell BP. Pediatric Flatfoot: Pearls and Pitfalls. Foot Ankle Clin. 2017;22:643-656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 29. | Dars S, Uden H, Banwell HA, Kumar S. The effectiveness of non-surgical intervention (Foot Orthoses) for paediatric flexible pes planus: A systematic review: Update. PLoS One. 2018;13:e0193060. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 57] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 30. | Rome K, Ashford RL, Evans A. Non-surgical interventions for paediatric pes planus. Cochrane Database Syst Rev. 2010;CD006311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 41] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 31. | Leung AK, Cheng JC, Mak AF. A cross-sectional study on the development of foot arch function of 2715 Chinese children. Prosthet Orthot Int. 2005;29:241-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 32. | Liu KM, Shinoda K, Akiyoshi T, Watanabe H. Longitudinal analysis of adolescent growth of foot length and stature of children living in Ogi area of Japan: a 12 years data. Z Morphol Anthropol. 1998;82:87-101. [PubMed] [DOI] [Full Text] |
| 33. | Onodera AN, Sacco IC, Morioka EH, Souza PS, de Sá MR, Amadio AC. What is the best method for child longitudinal plantar arch assessment and when does arch maturation occur? Foot (Edinb). 2008;18:142-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 46] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 34. | Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005;14:798-804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1542] [Cited by in RCA: 2011] [Article Influence: 95.8] [Reference Citation Analysis (0)] |
| 35. | Thong ISK, Jensen MP, Miró J, Tan G. The validity of pain intensity measures: what do the NRS, VAS, VRS, and FPS-R measure? Scand J Pain. 2018;18:99-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 419] [Article Influence: 59.9] [Reference Citation Analysis (0)] |
| 36. | Richter M, Agren PH, Besse JL, Cöster M, Kofoed H, Maffulli N, Rosenbaum D, Steultjens M, Alvarez F, Boszczyk A, Buedts K, Guelfi M, Liszka H, Louwerens JW, Repo JP, Samaila E, Stephens M, Witteveen AGH. EFAS Score - Multilingual development and validation of a patient-reported outcome measure (PROM) by the score committee of the European Foot and Ankle Society (EFAS). Foot Ankle Surg. 2018;24:185-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 85] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 37. | Giannini BS, Ceccarelli F, Benedetti MG, Catani F, Faldini C. Surgical treatment of flexible flatfoot in children a four-year follow-up study. J Bone Joint Surg Am. 2001;83-A Suppl 2 Pt 2:73-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 84] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 38. | Faldini C, Mazzotti A, Panciera A, Perna F, Stefanini N, Giannini S. Bioabsorbable implants for subtalar arthroereisis in pediatric flatfoot. Musculoskelet Surg. 2018;102:11-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 39. | Memeo A, Verdoni F, Rossi L, Ferrari E, Panuccio E, Pedretti L. Flexible Juvenile Flat Foot Surgical Correction: A Comparison Between Two Techniques After Ten Years' Experience. J Foot Ankle Surg. 2019;58:203-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 40. | Roth S, Sestan B, Tudor A, Ostojic Z, Sasso A, Durbesic A. Minimally invasive calcaneo-stop method for idiopathic, flexible pes planovalgus in children. Foot Ankle Int. 2007;28:991-995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 52] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 41. | Giannini S, Ceccarelli F, Vannini F, Baldi E. Operative treatment of flatfoot with talocalcaneal coalition. Clin Orthop Relat Res. 2003;178-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 59] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 42. | Husain ZS, Fallat LM. Biomechanical analysis of Maxwell-Brancheau arthroereisis implants. J Foot Ankle Surg. 2002;41:352-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 43. | Needleman RL. Current topic review: subtalar arthroereisis for the correction of flexible flatfoot. Foot Ankle Int. 2005;26:336-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 95] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 44. | Brancheau SP, Walker KM, Northcutt DR. An analysis of outcomes after use of the Maxwell-Brancheau Arthroereisis implant. J Foot Ankle Surg. 2012;51:3-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 45. | Metcalfe SA, Bowling FL, Reeves ND. Subtalar joint arthroereisis in the management of pediatric flexible flatfoot: a critical review of the literature. Foot Ankle Int. 2011;32:1127-1139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 75] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 46. | Indino C, Villafañe JH, D'Ambrosi R, Manzi L, Maccario C, Berjano P, Usuelli FG. Effectiveness of subtalar arthroereisis with endorthesis for pediatric flexible flat foot: a retrospective cross-sectional study with final follow up at skeletal maturity. Foot Ankle Surg. 2020;26:98-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |