Published online Jul 18, 2024. doi: 10.5312/wjo.v15.i7.642
Revised: May 3, 2024
Accepted: June 11, 2024
Published online: July 18, 2024
Processing time: 121 Days and 19.1 Hours
Tibial avulsion fractures of the posterior cruciate ligament (PCL) are challenging to treat and compromise knee stability and function. Traditional open surgery often requires extensive soft tissue dissection, which may increase the risk of morbidity. In response to these concerns, arthroscopic techniques have been evolving. The aim of this study was to introduce a modified arthroscopic tech
To evaluate the effects of arthroscopic M-shaped suture fixation on treating tibia avulsion fractures of the PCL.
We developed a modified arthroscopic M-shaped suture fixation technique for tibia avulsion fractures of the PCL. This case series included 18 patients who underwent the procedure between January 2021 and December 2022. The patients were assessed for range of motion (ROM), Lysholm score and International knee documentation committee (IKDC) score. Postoperative complications were also recorded.
The patients were followed for a mean of 13.83 ± 2.33 months. All patients showed radiographic union. At the final follow-up, all patients had full ROM and a negative posterior drawer test. The mean Lysholm score significantly improved from 45.28 ± 8.92 preoperatively to 91.83 ± 4.18 at the final follow-up (P < 0.001), and the mean IKDC score improved from 41.98 ± 6.06 preoperatively to 90.89 ± 5.32 at the final follow-up (P < 0.001).
The modified arthroscopic M-shaped suture fixation technique is a reliable and effective treatment for tibia avulsion fractures of the PCL, with excellent fracture healing and functional recovery.
Core Tip: In this study, we describe a novel modification to the arthroscopic M-shaped suture fixation approach for tibial avulsion fractures of the posterior cruciate ligament (PCL), which emphasizes the creation of a suture fixation configuration resembling the letter "M", intended to achieve a more secure anatomical fixation of the avulsed bony fragment to the tibia. And we evaluate its outcomes through a case series. Our results showed that our modified arthroscopic treatment of PCL tibial avulsion fractures provides good clinical outcomes, radiologic healing, and knee stability. This fixation technique is worthy of widespread promotion.
- Citation: Zhang XH, Yu J, Zhao MY, Cao JH, Wu B, Xu DF. Arthroscopic M-shaped suture fixation for tibia avulsion fracture of posterior cruciate ligament: A modified technique and case series. World J Orthop 2024; 15(7): 642-649
- URL: https://www.wjgnet.com/2218-5836/full/v15/i7/642.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i7.642
The posterior cruciate ligament (PCL) is a critical stabilizer of the knee that maintains posterior and rotational stability during motion[1]. Injury to the PCL disrupts this normal kinetic functionality, leading to altered joint mechanics and increased joint instability, particularly in the anterior-posterior direction[2,3]. The PCL avulsion fracture is a rare form of PCL injury that is usually caused by high-energy events, such as motorcycle accidents, dashboard contact and hyper
While conservative management may be considered for nondisplaced avulsion fractures, surgical intervention is typically indicated for displaced fractures to re-establish joint stability and function[6,7]. Traditionally, open surgical techniques have been the mainstay for the fixation of tibial avulsion fractures. However, with advancements in arthroscopic technology, minimally invasive approaches have evolved[8]. Arthroscopy offers the benefits of minimal soft tissue dissection, lower infection risk, faster recovery, and the ability to assess and address intra-articular pathology concurrently.
Despite these advantages, arthroscopic fixation of tibial avulsion fractures has several challenges, including difficulty in reliably securing the avulsion fracture, as well as the high technical demands of the procedure. Various suture and fixation techniques have been described in the literature, and they have all been proven to be effective[9-13]. Nevertheless, the evolution of this technique continues as improvements are sought to optimize clinical outcomes and address technical limitations. Hence, we introduce a novel modification to the arthroscopic M-shaped suture fixation approach for tibial avulsion fractures of the PCL, which emphasizes the creation of a suture fixation configuration resembling the letter "M", intended to achieve more secure anatomical fixation of the avulsed bony fragment to the tibia.
In this study, we describe the modified technique, present a case series, delineate its surgical principles, and share our clinical outcomes with a focus on the safety, efficiency and stability imparted by this approach.
This case series included patients with tibia avulsion fractures of the PCL who underwent arthroscopic M-shaped suture fixation at our institution between January 2021 and December 2022. The inclusion criteria were as follows: (1) Tibia avulsion fracture of the PCL confirmed by X-ray, computed tomography (CT) scan, or magnetic resonance imaging (MRI); (2) Meyers-McKeever class II or III fracture[14]; (3) Waiting time from injury to operation less than 3 weeks; and (4) No preoperative joint dysfunction or history of knee injury. The exclusion criteria were as follows: (1) Anterior cruciate ligament (ACL) injuries, collateral ligament injuries, or severe multiple-ligament injuries; (2) Distal femoral or proximal tibial fractures; (3) Severe neurovascular injury; and (4) Follow-up periods < 12 months. Ethical approval was obtained from the Ethics Committee of our hospital, and informed consent was obtained from all patients.
All surgeries were performed by the same experienced orthopedic surgeon. The surgery was performed under general or spinal anesthesia with the patient in the supine position.
An anterolateral portal was established at the inferior level of the patella and slightly superior to the lateral aspect of the patellar tendon, and a conventional anteromedial portal (AM) was created. An arthroscope was used to inspect the joint space and to diagnose concomitant intra-articular ligament and meniscal lesions. The space between the ACL and PCL was opened carefully using a shaver, and then the arthroscope was passed through the anterior and PCL space to the posterior joint capsule. The affected limb was placed in the 4-font position. Afterward, two posterior medial incisions, upper and lower, were made under direct arthroscopic visualization. The posterior joint capsule was appropriately opened, and the gastrocnemius tendon was protected.
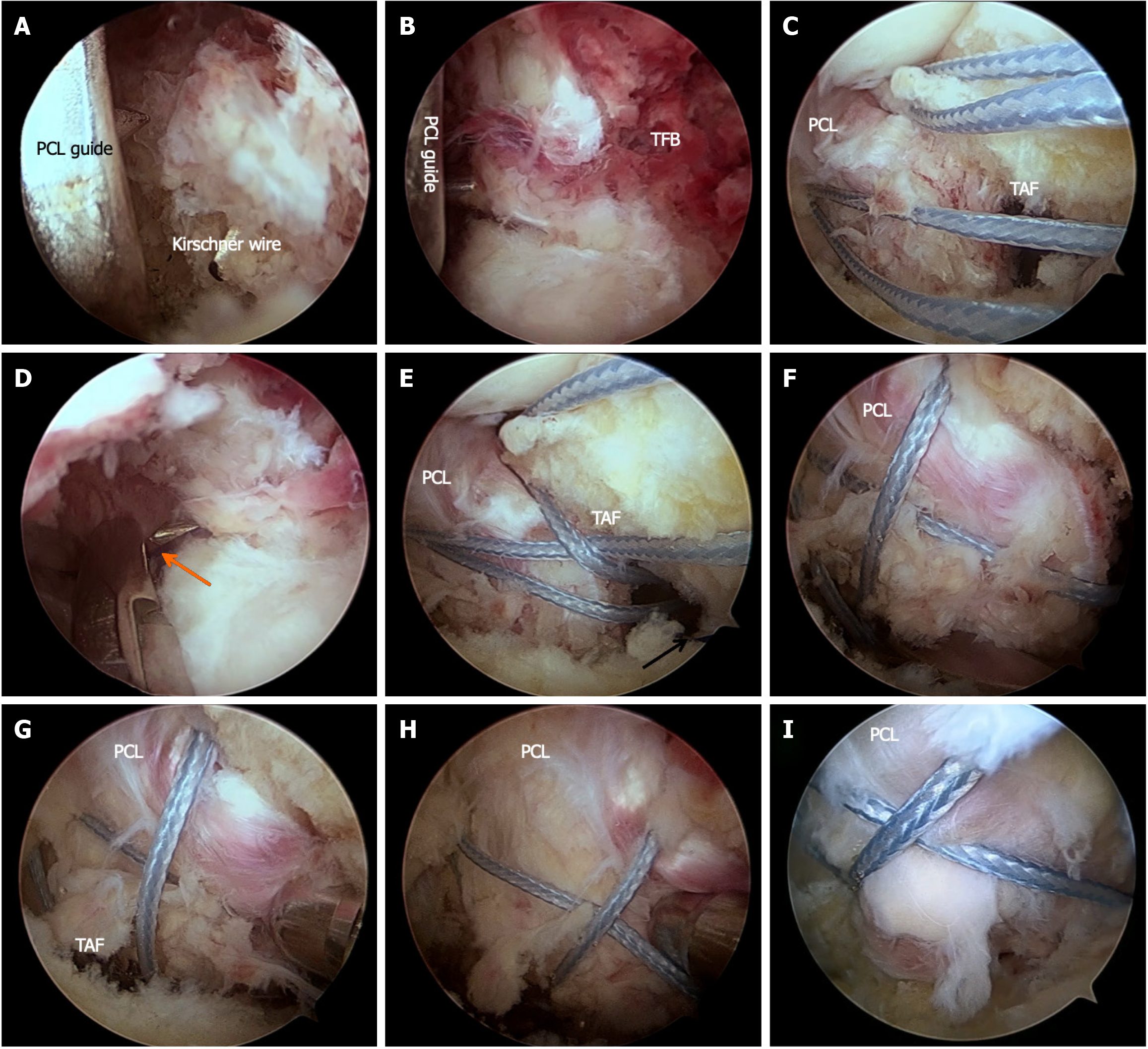
The arthroscope was inserted into the posterior joint cavity through the upper posteromedial portal, and both the upper and lower posteromedial portals were used to clean out the posterior joint cavity and expose the PCL avulsion bone fragment. After cleaning the bone bed, the PCL tibia guide was introduced into the posterior compartment through the AM portal. The tips of the guide were placed at the inferolateral or inferomedial corners of the tibial fracture bed. The tips were separated medially and laterally as much as possible and distributed on both sides of the distal bone bed. A 2.5 mm Kirschner guide wire was drilled into the anteromedial tibial cortex (Figure 1A and B). Two tibial tunnels were established.
A hollow catheter was used to pass polydioxanone (PDS) through the front of the PCL through the AM, which was subsequently removed through the posterior medial portal. This PDS suture was used to introduce two Ethicon MB66 sutures (Figure 1C). An epidural needle was used to introduce a PDS suture through one of the tibial tunnels (Figure 1D). This PDS suture was used to draw out both ends of one of the Ethicon MB66 sutures to the tibial tunnel opening (Figure 1E). In the same way, a PDS suture was introduced from another bone tunnel, and this PDS suture was utilized to draw out the two ends of another Ethicon MB66 suture to the tibial tunnel opening.
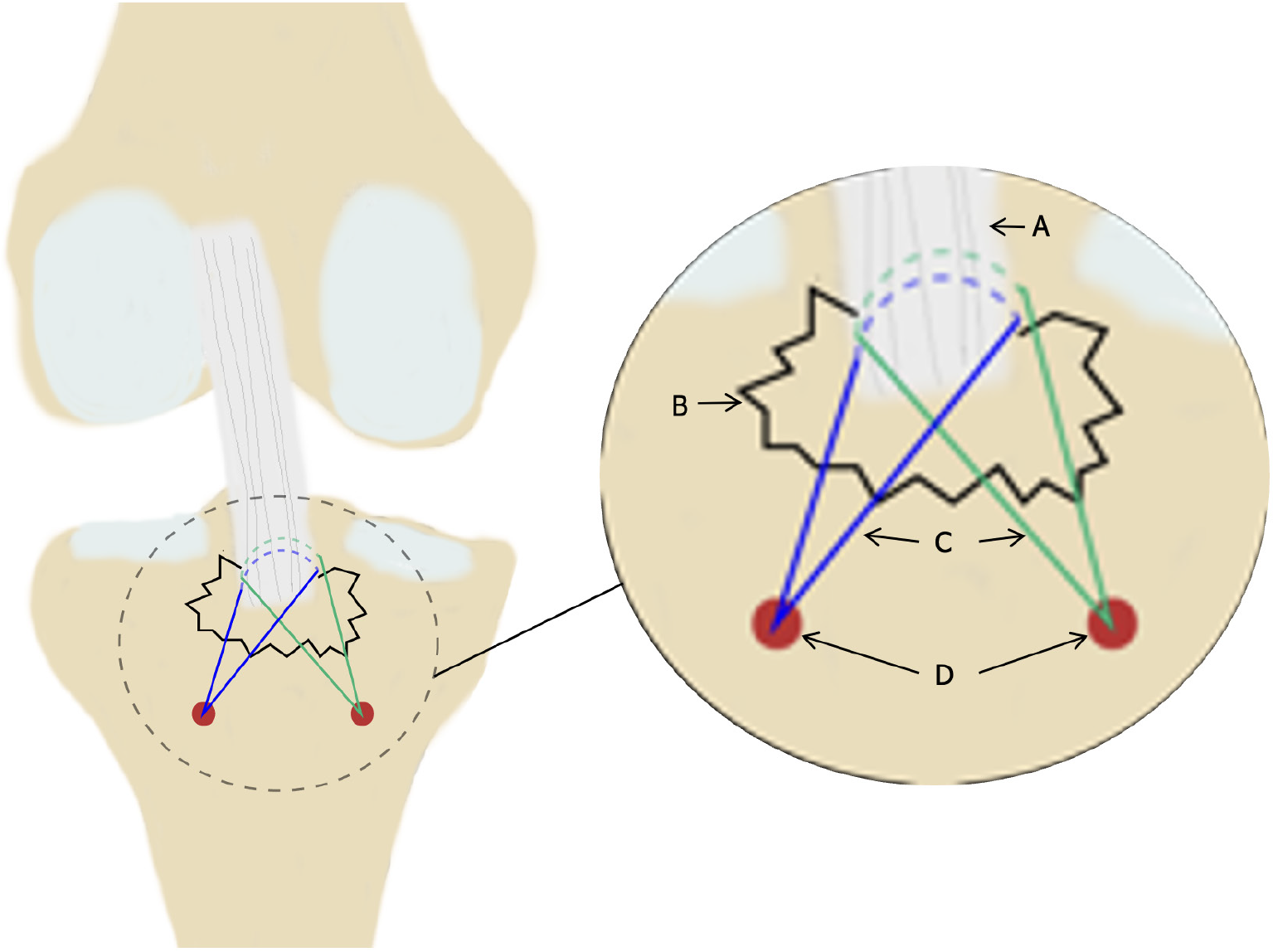
A suture grasper was used to adjust the position of the two Ethicon MB66 sutures so that the two sutures pressed on the fracture fragment in an "M" shape (Figure 1F). The bone fragments were reduced with the assistance of a probe (Figure 1G and H). The assistant performed the anterior tibial drawer test and tightened the two sutures. The avulsed bone fragment was observed and evaluated. After the fracture fragment was satisfactorily reduced (Figure 1I) and the PCL tension was restored, the sutures were knotted in pairs on the metal button. (The final fixation construct is shown in Figure 2).
The knee was immobilized in full extension for the first 3 weeks. Quadriceps exercises, straight leg raising, and ankle extension training were started immediately after surgery. After 3 weeks, protected passive flexion and extension with a knee brace were permitted. Partial weight bearing using crutches was allowed after 6 weeks. Full weight bearing was allowed after 8 weeks. Patients were encouraged to increase their activity gradually and resume normal life activities 3 months after surgery. Patients were allowed to resume sports activities 6 months after surgery.
Patients were followed up at regular intervals: 2 weeks, 4 weeks, 2 months, 3 months, 6 months, and 1 year postoperatively. Radiographic assessment (X-ray or CT) was performed immediately after surgery and at each follow-up visit to evaluate the reduction and healing of the fracture. MRI was performed on selected patients. The International knee documentation committee (IKDC) score[15], Lysholm score[16] and range of motion (ROM) were used to evaluate knee joint function. The posterior drawer test was performed to evaluate knee joint laxity.
Statistical analyses were performed using SPSS software. Continuous variables are expressed as the mean ± SD, and categorical variables are expressed as counts and percentages. Paired t tests were used to compare the preoperative and postoperative scores. Statistical significance was set at P < 0.05.
A total of 18 patients (9 males and 9 females) with tibial avulsion fractures of the PCL were included in this case series. The mean age of the patients was 49.72 ± 10.75 years. The injury mechanism was traffic accidents in 15 patients and falls from a height in 3 patients. Patient characteristics are summarized in Table 1.
| Characteristics | Summary data |
| Number of patients (n) | 18 |
| Age (years) | 49.72 ± 10.75 |
| Gender, n (%) | |
| Female | 9 (50.0) |
| Male | 9 (50.0) |
| Body mass index | 24.32 ± 2.8 |
| Side, n (%) | |
| Left | 13 (72.2) |
| Right | 5 (27.8) |
| Cause of injury, n (%) | |
| Traffic accident | 15 (83.3) |
| Falls from height | 3 (16.7) |
| Meyers-McKeever classification, n (%) | |
| Type II | 7 (38.9) |
| Type III | 11 (61.1) |
| Operation delay (day) | 6.56 ± 3.09 |
| Operation time (minute) | 55.28 ± 7.57 |
| Intraoperative blood loss (mL) | 11.94 ± 5.46 |
| Follow up (month) | 13.83 ± 2.33 |
All patients successfully underwent the modified M-shaped suture fixation technique without intraoperative complications. The average surgical time was 55.28 ± 7.57 minutes, and intraoperative blood loss was minimal, with an average of 11.94 ± 5.46 mL.
Radiographic examination revealed anatomical reduction (Figure 3) and solid union in all patients at the final follow-up. Three patients were selected for postoperative MRI. No displacement or nonunion of the fracture was found.
The mean IKDC score improved from 41.98 ± 6.06 preoperatively to 90.89 ± 5.32 at the final follow-up (P < 0.001). The mean Lysholm score also significantly improved from 45.28 ± 8.92 preoperatively to 91.83 ± 4.18 at the final follow-up (P < 0.001; Table 2).
| Preoperative | Final follow-up | P value | |
| Lysholm score | 45.28 ± 8.92 | 91.83 ± 4.18 | < 0.001 |
| IKDC score | 41.98 ± 6.06 | 90.89 ± 5.32 | < 0.001 |
| ROM (degree) | 59.17 ± 12.04 | 128.6 ± 4.79 | < 0.001 |
The mean ROM improved from 59.17 ± 12.04 degrees preoperatively to 128.6 ± 4.79 degrees at the final follow-up (P < 0.001; Table 2). All patients regained full ROM, comparable to that of the uninjured leg. All patients had a negative posterior drawer test at the final follow-up.
One patient developed mild transient knee effusion, which resolved with conservative management. During the follow-up period, no infections, neurovascular injuries, deep vein thrombosis, or recurrent instabilities were observed.
In our case series, we described a modified arthroscopic M-shaped suture fixation technique for the management of tibial avulsion fractures of the PCL. Our results showed that our modified arthroscopic treatment of PCL tibial avulsion fractures provides good clinical outcomes, radiologic healing, and knee stability. This fixation technique is simple, relatively fast, and easily reproducible in routine clinical practice.
The traditional management of displaced PCL tibial avulsion fractures often relies upon open reduction and internal fixation. Although it allows direct visualization and manipulation of the fracture site, it is associated with larger incisions, increased soft tissue damage, and a greater risk of infection, popliteal neurovascular structures, and postoperative stiffness. In contrast, patients who undergo arthroscopic techniques recover faster and have less postoperative pain due to reduced tissue trauma[17]. In our case series, patients showed a favorable recovery trajectory, with a return to preinjury levels of activity within the expected timeframe. This finding was in line with that of a prior study that underscored the benefits of arthroscopic approaches for treating PCL injuries[17].
Under arthroscopy, the clinical management of avulsion fractures commonly involves the use of screws[18], wires[19], or sutures[17,20,21]. These methods have all been proven to be effective. Several studies have assessed the outcomes of arthroscopic suture fixation for the treatment of PCL tibial avulsion. Sasaki et al[22] showed that there was no significant difference in biomechanical properties between fixations using screws and those using sutures. As the suture fixation technique is simple to perform and requires no secondary procedures, it has become the method of choice.
Various suture techniques for arthroscopic fixation, each with unique suture arrangements, have been documented. Xu et al[11] evaluated the outcome of arthroscopic treatment of PCL tibial avulsion fractures with the cinch knot technique. A total of 28 patients were followed up for a mean of 19 months. The mean Lysholm score was 96.96±3.62, and all patients had a normal ROM in the knee. Tao et al[23] treated PCL tibial avulsion using direct anterior-to-posterior suture suspension fixation. Compared with screw-suture fixation, anterior-to-posterior suture suspension fixation also showed satisfactory clinical results. Seifeldin et al[13] treated PCL tibial avulsion fractures with arthroscopic reduction and fixation by holding the PCL with two “cinch knots”. Fifteen patients were followed up for approximately 40 months. The results showed that the mean Lysholm score was 90.27 (range: 67-99), and the mean postoperative flexion was 134.7 degrees (range: 120-150). However, some of the configurations are complex and difficult to execute.
Our modified M-shaped suture technique is an extension of these foundational methods and addresses some limitations observed in prior studies. This technique offers several potential advantages. First, the configuration used in our fixation technique maximizes the contact area between the fracture fragment and the tibial bed, providing more stable fixation and hence promoting healing. It opposes the deforming forces of the natural tension of the PCL, resisting vertical and horizontal displacement. This stability is critical for early mobilization, which is a key factor in preventing joint stiffness and facilitating the return of function. Second, we relied on suture pressure on the fracture fragment and ligament tension to fix the PCL avulsion fracture fragment. The suture threads that are not passed through the fracture fragment or ligament prevent unnecessary damage to the PCL fibers and help maintain the integrity of the ligament. This approach simplified the operation process. The technical bottleneck of ligament sutures under arthroscopy is avoided. Third, the use of double bone channel fixation does not affect the contact area of the fracture fragment, and double suture arm compression fixation can effectively control rotation. The two bone channels should be spaced apart and away from the tibial fracture bed during the operation, which can reduce the number of sutures cutting bone channels and is more conducive to controlling rotation. Fourth, dual medial access simplifies the operation and eliminates the need to frequently switch accesses during the operation.
However, we acknowledge certain limitations within our study. First, this study included a small sample of patients and lacked a comparative group. Future studies with larger populations and longer follow-up durations are necessary to validate the long-term efficacy and safety of the M-shaped suture technique. Additionally, because of the rarity of PCL tibial avulsion fractures[4,5], multicenter studies or meta-analyses might be required to accumulate sufficient data to draw more generalized conclusions. Second, this study was deficient in associated biomechanical research. Future studies should be conducted to gather pertinent mechanical data to reinforce the validity of the findings.
In conclusion, the arthroscopic M-shaped suture fixation technique for tibial avulsion fractures of the PCL presented here is a reliable and effective treatment option that combines the benefits of both minimally invasive surgery and secure fixation. This fixation technique is simple, easily reproducible and worthy of widespread promotion.
| 1. | Griffith JF, Antonio GE, Tong CW, Ming CK. Cruciate ligament avulsion fractures. Arthroscopy. 2004;20:803-812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 57] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 2. | LaPrade CM, Civitarese DM, Rasmussen MT, LaPrade RF. Emerging Updates on the Posterior Cruciate Ligament: A Review of the Current Literature. Am J Sports Med. 2015;43:3077-3092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 167] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 3. | Wang D, Graziano J, Williams RJ 3rd, Jones KJ. Nonoperative Treatment of PCL Injuries: Goals of Rehabilitation and the Natural History of Conservative Care. Curr Rev Musculoskelet Med. 2018;11:290-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 4. | White EA, Patel DB, Matcuk GR, Forrester DM, Lundquist RB, Hatch GF 3rd, Vangsness CT, Gottsegen CJ. Cruciate ligament avulsion fractures: anatomy, biomechanics, injury patterns, and approach to management. Emerg Radiol. 2013;20:429-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 5. | Katsman A, Strauss EJ, Campbell KA, Alaia MJ. Posterior Cruciate Ligament Avulsion Fractures. Curr Rev Musculoskelet Med. 2018;11:503-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 65] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 6. | Gopinatth V, Mameri ES, Casanova FJ, Khan ZA, Jackson GR, McCormick JR, Brophy RH, Knapik DM, LaPrade RF, Chahla J. Systematic Review and Meta-analysis of Clinical Outcomes After Management of Posterior Cruciate Ligament Tibial Avulsion Fractures. Orthop J Sports Med. 2023;11:23259671231188383. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 7. | Hooper PO 3rd, Silko C, Malcolm TL, Farrow LD. Management of Posterior Cruciate Ligament Tibial Avulsion Injuries: A Systematic Review. Am J Sports Med. 2018;46:734-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 88] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 8. | Song JG, Nha KW, Lee SW. Open Posterior Approach versus Arthroscopic Suture Fixation for Displaced Posterior Cruciate Ligament Avulsion Fractures: Systematic Review. Knee Surg Relat Res. 2018;30:275-283. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 41] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 9. | Rhee SJ, Jang JH, Choi YY, Suh JT. Arthroscopic reduction of posterior cruciate ligament tibial avulsion fracture using two cross-linked pull-out sutures: A surgical technique and case series. Injury. 2019;50:804-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | Madi S S, Pandey V, Reddy B, Acharya K. Clinical and Radiological Outcomes Following Arthroscopic Dual Tibial Tunnel Double Sutures Knot-bump Fixation Technique for Acute Displaced Posterior Cruciate Ligament Avulsion Fractures. Arch Bone Jt Surg. 2021;9:50-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 11. | Xu Z, Dong Y, Feng YE, Xie P, Gu J, Kang K, Gao S, Zheng X. A simple arthroscopic technique for treatment of displaced "hinged" type of posterior cruciate ligament avulsion fractures. BMC Musculoskelet Disord. 2022;23:841. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 12. | Chen LB, Wang H, Tie K, Mohammed A, Qi YJ. Arthroscopic fixation of an avulsion fracture of the tibia involving the posterior cruciate ligament: a modified technique in a series of 22 cases. Bone Joint J. 2015;97-B:1220-1225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 13. | Seifeldin AF, Abdel-Kader KFM, Abdel Meguid KS, Wahsh M, Fekry AR. Arthroscopic management of avulsion fractures of the tibial attachment of the posterior cruciate ligament: A novel technique and mid-term outcomes. J Clin Orthop Trauma. 2023;42:102177. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Meyers MH, McKeever FM. Fracture of the intercondylar eminence of the tibia. J Bone Joint Surg Am. 1970;52:1677-1684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 363] [Cited by in RCA: 260] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 15. | Hefti F, Müller W, Jakob RP, Stäubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1:226-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1062] [Cited by in RCA: 1192] [Article Influence: 36.1] [Reference Citation Analysis (0)] |
| 16. | Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10:150-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1767] [Cited by in RCA: 1906] [Article Influence: 43.3] [Reference Citation Analysis (0)] |
| 17. | Chen SY, Cheng CY, Chang SS, Tsai MC, Chiu CH, Chen AC, Chan YS. Arthroscopic suture fixation for avulsion fractures in the tibial attachment of the posterior cruciate ligament. Arthroscopy. 2012;28:1454-1463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 18. | Martinez-Moreno JL, Blanco-Blanco E. Avulsion fractures of the posterior cruciate ligament of the knee. An experimental percutaneous rigid fixation technique under arthroscopic control. Clin Orthop Relat Res. 1988;204-208. [PubMed] [DOI] [Full Text] |
| 19. | Kim SJ, Shin SJ, Choi NH, Cho SK. Arthroscopically assisted treatment of avulsion fractures of the posterior cruciate ligament from the tibia. J Bone Joint Surg Am. 2001;83:698-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 66] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 20. | Wu L, Xu H, Li B, Xu B. Improved arthroscopic high-strength suture fixation for the treatment of posterior cruciate ligament avulsion fracture. J Orthop Surg (Hong Kong). 2022;30:10225536221101701. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 21. | Gui J, Wang L, Jiang Y, Wang Q, Yu Z, Gu Q. Single-tunnel suture fixation of posterior cruciate ligament avulsion fracture. Arthroscopy. 2009;25:78-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 42] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 22. | Sasaki SU, da Mota e Albuquerque RF, Amatuzzi MM, Pereira CA. Open screw fixation versus arthroscopic suture fixation of tibial posterior cruciate ligament avulsion injuries: a mechanical comparison. Arthroscopy. 2007;23:1226-1230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 53] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 23. | Tao T, Yang W, Tao X, Li Y, Zhang K, Jiang Y, Gui J. Arthroscopic Direct Anterior-to-Posterior Suture Suspension Fixation for the Treatment of Posterior Cruciate Ligament Tibial Avulsion Fracture. Orthop Surg. 2022;14:2031-2041. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/