Published online Jun 18, 2024. doi: 10.5312/wjo.v15.i6.539
Revised: May 7, 2024
Accepted: May 27, 2024
Published online: June 18, 2024
Processing time: 138 Days and 11.5 Hours
Open long bone fractures are a major concern for pediatric patients due to the risk of surgical site infection (SSI). Early studies have recommended irrigation and debridement of open fractures within 6 hours-8 hours for the prevention of SSI. According to the American College of Surgeons (ACS) Best Practice Guidelines, in 2015, irrigation and debridement should be done within 24 hours.
To identify whether early irrigation and debridement, within 8 hours, vs late, between 8 hours and 24 hours, for pediatric open long bone fractures impacts rate of SSI.
Using retrospective data review from the National Trauma Data Bank, Trauma Quality Improvement Project (TQIP) of 2019. TQIP database is own by the ACS and it is the largest database for trauma quality program in the world. Propensity matching analysis was performed for the study.
There were 390 pediatric patients with open long bone fractures who were incl
Our findings support the recommendation for managing open long bone fractures from the ACS: Complete surgical irrigation and debridement within 24 hours.
Core Tip: Using the National Trauma Quality Improvement Project of 2019, data from 390 pediatric patients with open long bone fractures showed no significant difference in the rate of surgical site infection when irrigation and debridement was done within 8 hours vs between 8 hours and 24 hours.
- Citation: Savla R, Kuo YH, Ahmed N. Outcomes of early versus late irrigation and debridement of pediatric open long bone fractures. World J Orthop 2024; 15(6): 539-546
- URL: https://www.wjgnet.com/2218-5836/full/v15/i6/539.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i6.539
Open long bone fractures are a major concern for pediatric patients due to the risk of surgical site infection (SSI). The most widely used classification system of open fractures is Gustilo-Anderson's classification, which is categorized from minor grade I injuries to severe grade III injuries, and grade III is further classified into three subcategories[1,2]. The higher the grade of the open fracture, the higher the risk of infection. The infection rate for open fractures in children was reported at around 8%[3]. The consequences of infections after open tibial fractures in adults included a longer time for union, non-union of the fracture, the risk for sepsis, and even amputation[4]. Early administration of antibiotics and timely irrigation and debridement of an open fracture resulted in a reduction in the incidence of SSI[5,6].
Studies and guidelines are consistent with the early administration of antibiotics in open long bone fractures to min
The TQIP database of the calendar year of 2019 data was accessed for the study. All pediatric patients < 18 years of age who sustained blunt mechanism of injury and open tibial fractures who were admitted to the hospital and underwent irrigation and debridement within 24 hours were included in the study. Race, sex, injury severity score (ISS), glasgow coma scale (GCS) score, other regions' abbreviated injury scale (AIS) scores, the timing of antibiotic administration and comorbidities were included in the study. Patients with penetrating mechanisms of injury were excluded from the study. The primary outcome was SSI. The secondary outcomes were hospital length of stay and discharge disposition.
The data was summarized using summary statistics. The continuous variables were presented as a median and inte
The total of 390 patients who qualified for the study, 207 (53.1%) patients underwent irrigation and debridement within 8 hours of the patient’s arrival and the remaining 183 (46.9%) patients underwent irrigation and debridement between (8 hours-24 hours). There were no significant differences between the characteristics of these two groups, late vs early, including median age [IQR: 15 years (12-16) vs 14 years (10-16), P = 0.063], median GCS score [IQR: 15 (15-15) vs 15 (15-15), P = 0.732], the median timing (in hours) of antibiotic therapy administration [median IQR: 0.2 (0-0.88) vs 0.3 (0-0.86), P = 0.278]. The only significant difference between the groups was that a higher proportion of black race patients underwent late irrigation and debridement compared to non-black patients (21.9% vs 13%, P = 0.03). No significant differences were found between the groups regarding the comorbidities and an AIS score (Table 1).
| Irrigation and debridement within 8 hours | Irrigation and debridement after 8 hours | P value | |
| Age (years): Median (Q1, Q3) | 14 (10, 16) | 15 (12, 16) | 0.063 |
| Race | |||
| American indian | 1 (0.5) | 0 (0) | 1 |
| Asian | 4 (1.9) | 1 (0.5) | 0.377 |
| Black | 27 (13) | 40 (21.9) | 0.03 |
| Pacific islander | 2 (1) | 0 (0) | 0.501 |
| White | 151 (72.9) | 121 (66.1) | 0.176 |
| Other | 19 (9.2) | 19 (10.4) | 0.819 |
| Sex | |||
| Female | 64 (30.9) | 55 (30.1) | 0.941 |
| Male | 143 (69.1) | 128 (69.9) | |
| Injury severity score | 10 | 9 | 0.224 |
| Glasgow coma scale | 15 | 15 | 0.732 |
| Mechanism of Injury | |||
| Fall | 35 (16.9) | 41 (22.4) | 0.503 |
| Machinery | 1 (0.5) | 1 (0.5) | |
| MVT occupant | 42 (20.3) | 35 (19.1) | |
| MVT motorcyclist | 8 (3.9) | 7 (3.8) | |
| MVT pedal cyclist | 4 (1.9) | 5 (2.7) | |
| MVT pedestrian | 35 (16.9) | 41 (22.4) | |
| MVT other | 9 (4.3) | 6 (3.3) | |
| Pedal cyclist, other | 5 (2.4) | 3 (1.6) | |
| Pedestrian, other | 4 (1.9) | 3 (1.6) | |
| Transport, other | 41 (19.8) | 20 (10.9) | |
| Natural/ environment, other | 0 (0) | 1 (0.5) | |
| Overexertion | 4 (1.9) | 7 (3.8) | |
| Struck by, against | 16 (7.7) | 11 (6) | |
| Other specified and classifiable | 3 (1.4) | 2 (1.1) | |
| Antibiotic therapy (hours) | 0.3 (0-0.86) | 0.2 (0-0.88) | 0.278 |
| Comorbidities | |||
| Congenital abnormalities | 1 (0.5) | 3 (1.6) | 0.345 |
| Mental health disorder | 4 (1.9) | 4 (2.2) | 1 |
| Substance abuse | 2 (1) | 1 (0.5) | 1 |
| Bleeding | 0 (0) | 1 (0.5) | 0.469 |
| Abbreviated injury score of 3-5 | |||
| Brain | 7 (3.4) | 9 (4.9) | 0.612 |
| Spine | 4 (1.9) | 0 (0) | 0.126 |
| Chest | 12 (5.8) | 12 (6.6) | 0.92 |
| Abdomen | 8 (3.9) | 4 (2.2) | 0.506 |
| Upper extremity | 0 (0) | 1 (0.5) | 0.469 |
| Lower extremity | 193 (93.2) | 156 (85.2) | 0.016 |
Propensity score matching created 176 pairs of patients. After propensity score matching, there was an improvement in all the matching variables. There were no significant differences found between the groups, late vs early, regarding median age [IQR: 15 years (12-16) vs 14 years (11-16), P = 0.418], median GCS score [IQR: 15 (15-15) vs 15 (15-15), P > 0.99), the median timing ( in hours) of antibiotic therapy administration (median IQR: 0.2 (0-0.88) vs 0.3 (0-0.87), P = 0.428]. There was no significant difference between the groups regarding the black race patients who underwent late irrigation and debridement compared to non-black patients (21% vs 14.8%, P = 0.153) (Table 2).
| Irrigation and debridement within 8 hours | Irrigation and debridement after 8 hours | P value | |
| Age (years): Median (Q1, Q3) | 14 (11, 16) | 15 (12, 16) | 0.063 |
| Race | |||
| American Indian | 1 (0.6) | 0 (0) | |
| Asian | 4 (2.3) | 1 (0.6) | 0.371 |
| Black | 26 (14.8) | 37 (21) | 0.153 |
| Pacific islander | 2 (1.1) | 0 (0) | |
| White | 121 (68.8) | 120 (68.2) | 1 |
| Other | 19 (10.8) | 16 (9.1) | 0.71 |
| Sex | |||
| Female | 54 (30.7) | 54 (30.7) | 1 |
| Male | 122 (69.3) | 122 (69.3) | |
| Injury severity score | 9.5 | 9 | 0.748 |
| Glasgow coma scale | 15 | 15 | 1 |
| Mechanism of injury | |||
| Fall | 33 (18.8) | 40 (22.7) | |
| Machinery | 0 (0) | 0 (0) | |
| MVT occupant | 35 (19.9) | 33 (18.8) | |
| MVT motorcyclist | 8 (4.5) | 7 (4) | |
| MVT pedal cyclist | 4 (2.3) | 5 (2.8) | |
| MVT pedestrian | 29 (16.5) | 40 (22.7) | |
| MVT other | 8 (4.5) | 6 (3.4) | |
| Pedal cyclist, other | 3 (1.7) | 3 (1.7) | |
| Pedestrian, other | 2 (1.1) | 3 (1.7) | |
| Transport, other | 33 (18.8) | 20 (11.4) | |
| Natural/ environment, other | 0 (0) | 1 (0.6) | |
| Overexertion | 4 (2.3) | 5 (2.8) | |
| Struck by, against | 15 (8.5) | 11 (6.2) | |
| Other specified and classifiable | 2 (1.1) | 2 (1.1) | |
| Antibiotic therapy (hours) | 0.3 (0-0.87) | 0.2 (0-0.88) | 0.428 |
| Comorbidities | |||
| Congenital abnormalities | 0 (0) | 3 (1.7) | |
| Mental health disorder | 3 (1.7) | 3 (1.7) | 1 |
| Substance abuse | 1 (0.6) | 1 (0.6) | 1 |
| Bleeding | 0 (0) | 1 (0.6) | |
| Abbreviated injury score of 3-5 | |||
| Brain | 4 (2.3) | 8 (4.5) | 0.386 |
| Spine | 2 (1.1) | 0 (0) | |
| Chest | 7 (4) | 11 (6.2) | 0.48 |
| Abdomen | 4 (2.3) | 4 (2.3) | 1 |
| Upper extremity | 0 (0) | 1 (0.6) | |
| Lower extremity | 164 (93.2) | 152 (86.4) | 0.067 |
The rate of deep SSI was 0.6% for patients who received surgical irrigation and debridement within 8 hours and 1.1% for those who received it after 8 hours (AOR: 0.5, 95%CI: 0.268-30.909, P > 0.99) (Table 3).
| Irrigation and debridement within 8 hours | Irrigation and debridement after 8 hours | P value | Odds ratio | Absolute risk difference | |
| Deep surgical site Infection | 1 (0.6) | 2 (1.1) | 1 | 0.5 (0.268- 30.909) | -0.006 (-0.031 to 0.019) |
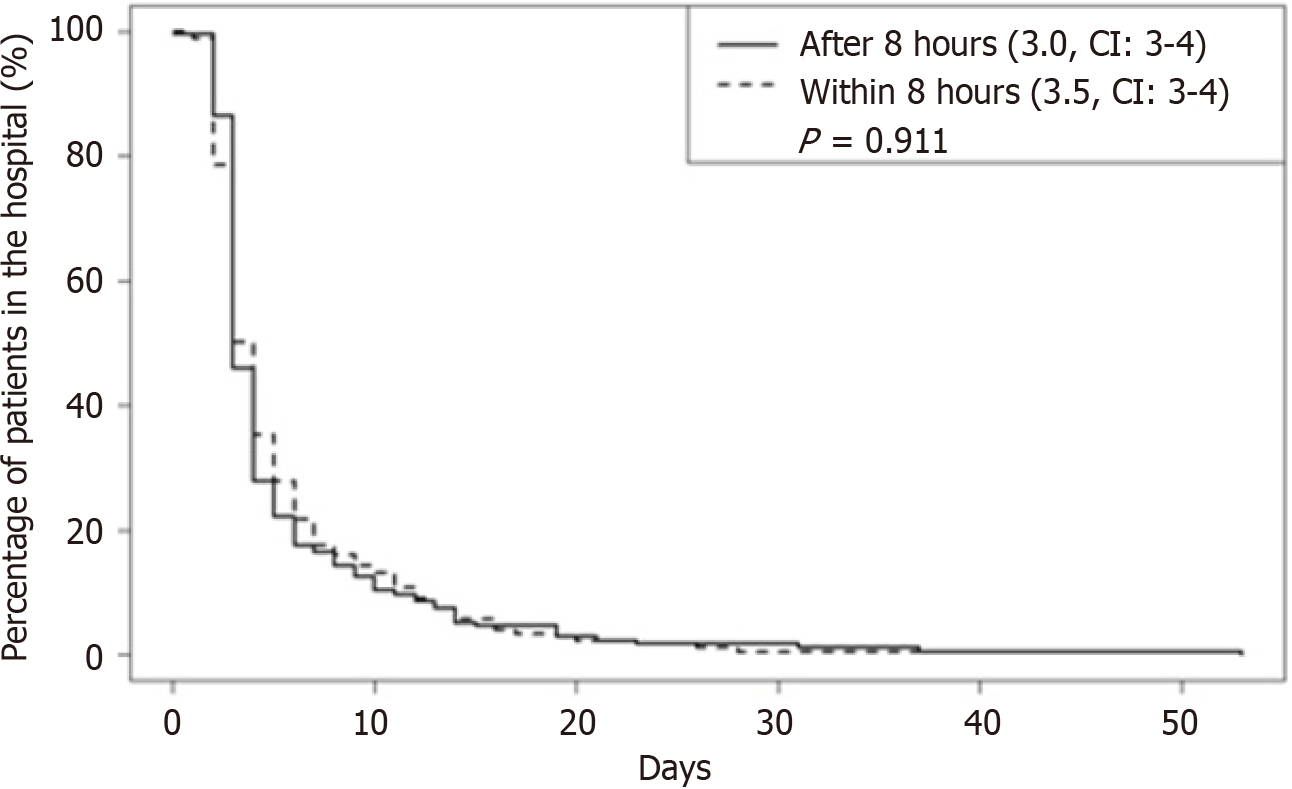
| Length of stay in hospital (days) | 3.5 (3,4) | 3 (3,4) | 0.911 | ||
| Discharge dispositions | |||||
| Home with care | 12 (6.8) | 10 (5.7) | 0.534 | ||
| Home without care | 145 (82.4) | 152 (86.4) | |||
| Rehabilitation | 12 (6.8) | 11 (6.2) | |||
| Short-term through long-term care facility | 5 (2.8) | 1 (0.6) | |||
| Skilled nursing facility | 1 (0.6) | 2 (1.1) | |||
| Other | 1 (0.6) | 0 (0) |
Patients who received irrigation and debridement within 8 hours stayed for an average of 3.5 days, and those who received it after 8 hours stayed for an average of 3 days, with no significant difference found (Figure 1).
Analysis of the discharge dispositions of the patients amongst the options of home with care, home without care, rehabilitation, short-term stay at a long-term care facility, skilled nursing facility, or other, there was no significant difference found between the two groups regarding discharge dispositions (Table 3).
Comparing pediatric patients with open tibial fracture injuries who received surgical irrigation and debridement within 8 hours vs after 8 hours-24 hours, we found no significant difference in the occurrence of deep SSI. The length of stay in the hospital and discharge dispositions were similar between the groups.
The literature regarding pediatric open long bone fracture management is relatively limited regarding the occurrence of infections; however, our results are concordant with the available data. Kuhn et al[3] conducted a retrospective study at a level 1 trauma center at Vanderbilt University Medical Center looking at open long bone fractures in 303 pediatric patients and found that infection rates were unrelated to the timing of operative debridement when patients were divided into two groups, within 6 hours and after 6 hours[3]. Additionally, Kelly et al[16] also conducted a retrospective study of 288 open fractures in pediatric patients at a level 1 trauma center in tennessee and found no significant association between the development of infection and time to surgical debridement; however, this data was not specific to long bone fractures. Another study by Skaggs et al[17] analyzed data from 536 pediatric patients who sustained open fractures across six tertiary pediatric referral centers in North America. They also found no significant difference between infection rates for patients treated within 6 hours vs after 6 hours, but this data was also not specific to long bone fractures. Our data on pediatric open long bone fractures, tibial fractures, concordant with these studies' conclusions; the timing of operative debridement within 24 hours is not directly predictive of SSI risk for pediatric open long bone fracture management.
Kuhn et al[3] studied several factors within pediatric open long bone fractures associated with the risk for deep infection, including the type of long bone, the Gustilo-Anderson type, the time of presentation to the hospital after the injury occurred, the number of operative debridement and the number of operative procedures. The only statistically significant variable in terms of increasing the risk of deep infection was the time between the injury and presentation to the hospital[3]. Wang et al[18] studied the management of Gustilo-Anderson type II and IIa pediatric open long bone fractures comparing early primary wound closure, which was closure during the initial operation, vs delayed wound closure, on subsequent return to the operating room, and found no significant associations between the rates of complications including infection, delayed compartment syndrome, nonunion, growth arrest, and the length of stay at the hospital. Chan et al[13] studied 60 patients with pediatric open tibial fractures at a level 1 trauma center in the United Kingdom. They found no significant association with outcomes of infection rate, time to union, problems with the union, and any additional unplanned surgery when comparing independent variables of time at which antibiotics were given, time to index surgery, type of skeletal fixation, and time to definitive cover[13]. Our study establishes that there were no significant differences in deep SSI, length of stay in the hospital, and discharge disposition when comparing pediatric open long bone fractures specifically tibial fractures patients who received surgical irrigation and debridement within 8 hours vs after 8 hours.
The main limitation of our study was its retrospective nature. Additionally, since the data is obtained from the TQIP, we could not account for differences between the hospitals regarding protocol and how each one specifically manages pediatric open long bone fractures. The surgical irrigation and debridement methodology at these different hospitals was unknown in terms of how they conducted the procedure, how much fluid was used during the irrigation, when the antibiotics were administered, and which antibiotics were administered. Unfortunately, TQIP data set does not provide information about the Gustilo-Anderson’s classification of the fractures but provides information about the severity of the fracture on AIS scores. Propensity score matching balanced the higher severity (AIS 3-5) of the fractures between the two groups (Table 2). These variables could have impacted our results in ways we cannot currently analyze. Nonetheless, the TQIP database is extremely beneficial in analyzing larger trends across the country. Future research with prospective studies can address these limitations.
Our study showed more than half of the open long bone fractures underwent irrigation and debridement within 8 hours of the patient’s arrival at the hospital. Performing the irrigation and debridement within 8 hours or between 8 hours-24 hours showed no significant differences in deep SSI, hospital length of stay or discharge to home. Our data supports the recommendation for managing open long bone fractures from the ACS: Complete surgical irrigation and debridement within 24 hours.
| 1. | Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58:453-458. [PubMed] |
| 2. | Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma. 1984;24:742-746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1593] [Cited by in RCA: 1462] [Article Influence: 34.8] [Reference Citation Analysis (0)] |
| 3. | Kuhn AW, Troyer SC, Martus JE. Pediatric Open Long-Bone Fracture and Subsequent Deep Infection Risk: The Importance of Early Hospital Care. Children (Basel). 2022;9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Johnson EN, Burns TC, Hayda RA, Hospenthal DR, Murray CK. Infectious complications of open type III tibial fractures among combat casualties. Clin Infect Dis. 2007;45:409-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 199] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 5. | Zuelzer DA, Hayes CB, Hautala GS, Akbar A, Mayer RR, Jacobs CA, Wright RD, Moghadamian ES, Matuszewski PE. Early Antibiotic Administration Is Associated with a Reduced Infection Risk When Combined with Primary Wound Closure in Patients with Open Tibia Fractures. Clin Orthop Relat Res. 2021;479:613-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 6. | Brown KV, Walker JA, Cortez DS, Murray CK, Wenke JC. Earlier debridement and antibiotic administration decrease infection. J Surg Orthop Adv. 2010;19:18-22. [PubMed] |
| 7. | Hoff WS, Bonadies JA, Cachecho R, Dorlac WC. East Practice Management Guidelines Work Group: update to practice management guidelines for prophylactic antibiotic use in open fractures. J Trauma. 2011;70:751-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 114] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 8. | Rodriguez L, Jung HS, Goulet JA, Cicalo A, Machado-Aranda DA, Napolitano LM. Evidence-based protocol for prophylactic antibiotics in open fractures: improved antibiotic stewardship with no increase in infection rates. J Trauma Acute Care Surg. 2014;77:400-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 88] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 9. | A report by the British Orthopaedic Association/British Association of Plastic Surgeons Working Party on the management of open tibial fractures. September 1997. Br J Plast Surg. 1997;50:570-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 57] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Crowley DJ, Kanakaris NK, Giannoudis PV. Debridement and wound closure of open fractures: the impact of the time factor on infection rates. Injury. 2007;38:879-889. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 93] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 11. | Pollak AN, Jones AL, Castillo RC, Bosse MJ, MacKenzie EJ; LEAP Study Group. The relationship between time to surgical debridement and incidence of infection after open high-energy lower extremity trauma. J Bone Joint Surg Am. 2010;92:7-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 199] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 12. | Orthopedic Trauma Association. ACS TQIP Best Practices in the Management of Orthopedic Trauma. 2015; 7. Available from: https://www.facs.org/media/mkbnhqtw/ortho_guidelines. |
| 13. | Chan Y, Selvaratnam V, James L, Nayagam S. Paediatric open tibial fractures. Do children require a modified approach to that advised by the British Orthopaedic Association and British Association of Plastic Reconstructive and Aesthetic Surgeons in the UK? J Pediatr Orthop B. 2021;30:19-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Ho DE, Imai K, King G, Stuart EA. MatchIt: Nonparametric Preprocessing for Parametric Causal Inference. J Statistic Software. 2011;42:1-28. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1461] [Cited by in RCA: 1462] [Article Influence: 97.5] [Reference Citation Analysis (0)] |
| 15. | R Core Team. R: A language and environment for statistical computing. 2023. Available from: https://www.R-project.org/. |
| 16. | Kelly D, Sheffer B, Elrod R, Piana L, Pattisapu N, Nolan V, Spence D, Sawyer J. Infections After Open Fractures in Pediatric Patients: A Review of 288 Open Fractures. J Surg Orthop Adv. 2022;31:73-75. [PubMed] |
| 17. | Skaggs DL, Friend L, Alman B, Chambers HG, Schmitz M, Leake B, Kay RM, Flynn JM. The effect of surgical delay on acute infection following 554 open fractures in children. J Bone Joint Surg Am. 2005;87:8-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 74] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 18. | Wang KK, Rademacher ES, Miller PE, Lins L, Jordan E, May C, Glotzbecker MP, Hedequist DJ, Shore BJ. Management of Gustilo-Anderson Type II and IIIA Open Long Bone Fractures in Children: Which Wounds Require a Second Washout? J Pediatr Orthop. 2020;40:288-293. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/