Published online Apr 18, 2024. doi: 10.5312/wjo.v15.i4.337
Peer-review started: October 18, 2023
First decision: January 17, 2024
Revised: January 27, 2024
Accepted: March 15, 2024
Article in press: March 15, 2024
Published online: April 18, 2024
Processing time: 180 Days and 23.5 Hours
Excellent hip joint function facilitates limb recovery and improves the quality of survival. This study aimed to investigate the potential risk factors affecting postoperative joint functional activity and outcomes in elderly hip fractures patients and to provide evidence for patient rehabilitation and clinical mana
To explore the relationship between inflammatory factors and hip function and the interaction between inflammation and health after hip fracture in elderly patients.
The elderly patients who had hip fracture surgery at our hospital between January 1, 2021, and December 31, 2022 were chosen for this retrospective clinical investigation. Patients with excellent and fair postoperative hip function had their clinical information and characteristics gathered and compared. Age, gender, fracture site, surgical technique, laboratory indices, and other variables that could have an impact on postoperative joint function were all included in a univariate study. To further identify independent risk factors affecting postoperative joint function in hip fractures, risk factors that showed statistical significance in the univariate analysis were then included in a multiple logistic regression analysis. In addition to this, we also compared other outcome variables such as visual analogue scale and length of hospital stay between the two groups.
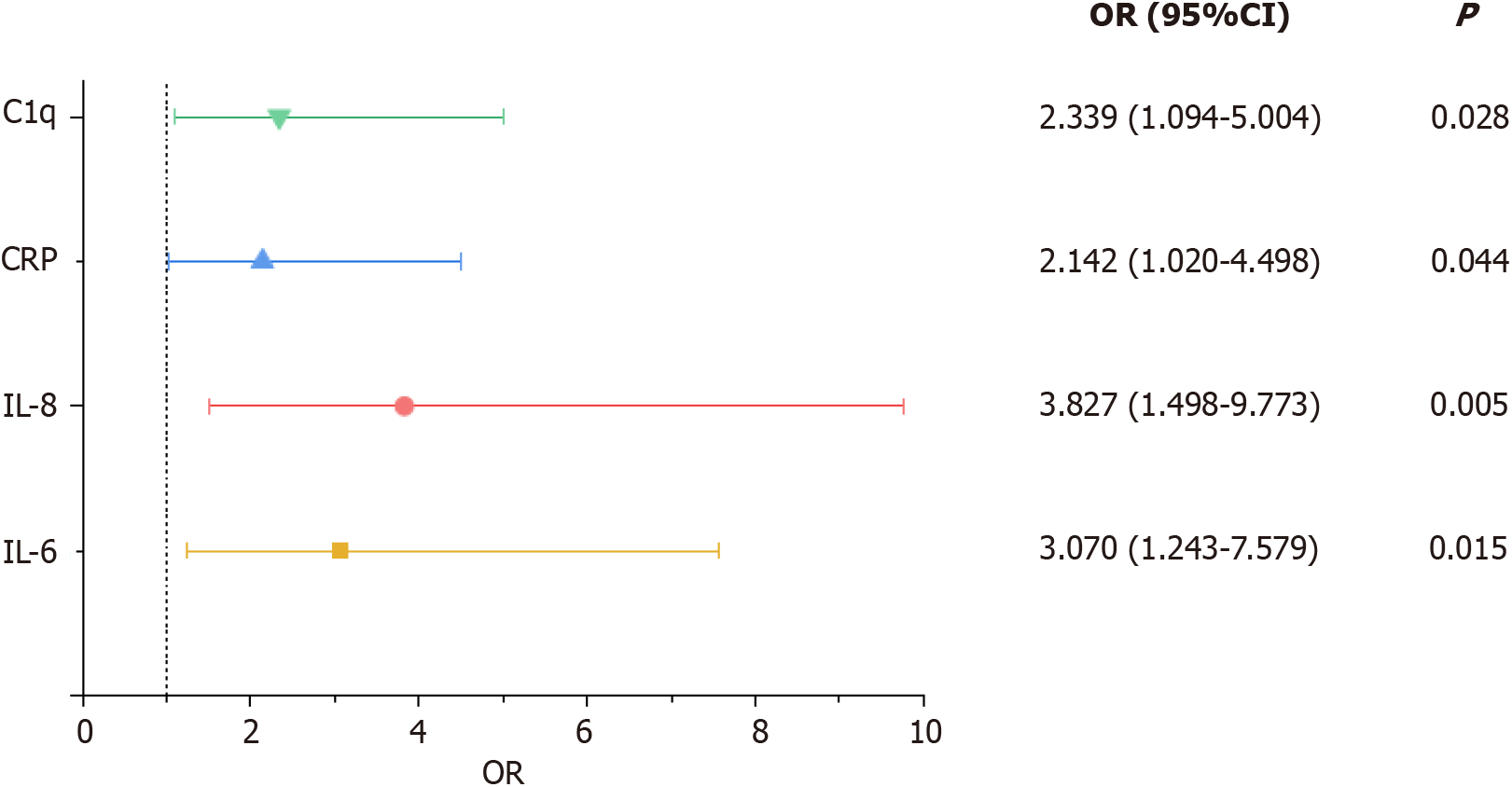
A total of 119 elderly patients with hip fractures were included in this study, of whom 37 were male and 82 were female. The results of univariate logistic regression analysis after excluding the interaction of various factors showed that there was a statistically significant difference in interleukin (IL)-6, IL-8, IL-10, C-reactive protein (CRP), and complement C1q (C1q) between the fair and excellent joint function groups (P < 0.05). The results of multiple logistic regression analysis showed that IL-6 > 20 pg/mL [(Odds ratio (OR) 3.070, 95%CI: 1.243-7.579], IL-8 > 21.4 pg/ mL (OR 3.827, 95%CI: 1.498-9.773), CRP > 10 mg/L (OR 2.142, 95%CI: 1.020-4.498) and C1q > 233 mg/L (OR 2.339, 95%CI: 1.094-5.004) were independent risk factors for poor joint function after hip fracture surgery (all P < 0.05).
After hip fractures in older patients, inflammatory variables are risk factors for fair joint function; therefore, early intervention to address these markers is essential to enhance joint function and avoid consequences.
Core Tip: Interleukin (IL)-6 > 20 pg/mL, IL-8 > 21.4 pg/mL, C-reactive protein > 10 mg/L, and complement C1q (C1q) > 233 mg/L may be independent risk factors for fair postoperative joint function in patients with hip fracture. In addition, C1q represented a specific risk factor for fair joint function after hip fracture surgery in elderly patients, these predictors may provide a new strategy for the treatment of hip fracture.
- Citation: Wang JM, Pan YT, Yang CS, Liu MC, Ji SC, Han N, Liu F, Sun GX. Effect of inflammatory response on joint function after hip fracture in elderly patients: A clinical study. World J Orthop 2024; 15(4): 337-345
- URL: https://www.wjgnet.com/2218-5836/full/v15/i4/337.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i4.337
Hip fractures are a serious and prevalent public health issue[1,2]. The high rates of sickness, mortality, and disability that are associated with ageing populations in particular pose a serious concern[3,4]. Also, as an osteoporotic fracture, it is highly susceptible to re-fracture[5], which will affect the patient’s mobility and quality of life[6,7]. The number of hip fractures is expected to increase to 4.5 million worldwide by 2050 as the population ages[8], and China will account for a significant proportion[9,10], thus the resulting physical and psychological problems, increased hospitalization costs and the social burden will pose a huge challenge in the future[11,12].
There are many risk factors for hip fracture, such as age, gender, smoking, osteoporosis, nutrition and medication[12,13]. However, few studies have explored the relevance of inflammatory factors to the prognosis of surgery in elderly hip fracture patients. Immunoinflammatory responses and oxidative stress have been shown to affect post-operative hip fracture outcomes[14]. There are several inflammatory factors associated with fracture trauma and bone healing, for example, interleukin (IL)-6 is increased in osteoporotic human bone and promotes the development and persistence of the inflammatory response that affects fracture healing[15]; elevated concentrations of IL-8 and IL-10 in the synovial fluid of patients with acute tibial plateau fractures[16]; C-reactive protein (CRP) is associated with mortality at one year after hip fracture surgery[17]; complement C1q (C1q) is also involved in the process of innate and acquired immunity and is important in maintaining the balance of the immune response[18].
The establishment and modification of patients’ rehabilitation exercises and treatment programmes depends in large part on the post-operative joint function, degree of pain perception, and duration of hospital stay following the hip fracture. The choices made about useful serum markers, prompt adjustments to treatment plans for better prognosis, and more efficient use of medical resources have a significant impact on families and society as a whole. Therefore, it is particularly necessary to explore the risk factors associated with older individuals after hip fracture surgery. This study aimed to analyze which inflammatory factors might be associated with joint mobility and prognostic outcomes after hip fracture surgery, and to establish direction for further study.
This study was a retrospective design. All procedures and methods of our study were carried out under the procedures and regulations of Shanghai East Hospital. Meanwhile, our hospital ethics committee reviewed and approved this research under the approval number: [2022] Research Audit No. 278. Written informed consent was obtained from all participants in this study, and all data related to the patients were complete and detailed and handled confidentially.
A total of 119 patients diagnosed with hip fractures were selected from the electronic case database of Shanghai East Hospital from January 1, 2021 to December 31, 2022, who met the diagnostic criteria for hip fracture and had completed elective surgery in our hospital. Then, all patients were divided into a postoperative fair hip function group (Score < 80) and a postoperative excellent hip function group (Score ≥ 90) according to the Harris hip function scale[19], with 37 males and 82 females, aged 56-100 years, with a mean age of (76.4 ± 12.29) years (Table 1). All included hip fracture patients in this study underwent proximal femoral nail antirotation (PFNA) and total hip arthroplasty (THA), including 61 patients who underwent PFNA and 58 patients who underwent THA (Table 1).
| Fair hip function after surgery (n = 67) | Excellent hip function after surgery (n = 52) | Total (n = 119) | t/χ2 | P value | |
| Age (yr) | 76.88 ± 12.54 | 75.79 ± 12.05 | 76.4 ± 12.29 | 0.538 | 0.660 |
| Sex | 0.005 | 0.946 | |||
| Female | 46 (68.7) | 36 (69.2) | 82 (68.9) | ||
| Male | 21 (31.3) | 16 (30.8) | 37 (31.1) | ||
| Hypertension | 0.149 | 0.699 | |||
| Yes | 41 (61.2) | 30 (57.7) | 71 (59.7) | ||
| No | 26 (38.8) | 22 (42.3) | 48 (40.3) | ||
| Diabetes | 0.008 | 0.929 | |||
| Yes | 15 (22.4) | 12 (23.1) | 27 (22.7) | ||
| No | 52 (77.6) | 40 (76.9) | 92 (77.3) | ||
| Types | 0.030 | 0.862 | |||
| Femoral neck | 32 (47.8) | 24 (46.2) | 56 (47.1) | ||
| Trochanteric | 35 (52.2) | 28 (53.8) | 63 (52.9) | ||
| Surgical method | 0.016 | 0.899 | |||
| PFNA | 34 (50.7) | 27 (51.9) | 61 (51.3) | ||
| THA | 33 (49.3) | 25 (48.1) | 58 (48.7) | ||
| Time from injury to | |||||
| Surgery | 4.69 ± 2.85 | 5.15 ± 2.82 | 4.89 ± 2.84 | 0.876 | 0.425 |
| Neut | 6.09 ± 2.38 | 6.49 ± 2.36 | 6.29 ± 2.36 | 0.643 | 0.806 |
| Lymph | 1.20 ± 0.61 | 1.14 ± 0.44 | 1.17 ± 0.53 | 0.455 | 0.152 |
| IL-6 | 53.08 ± 28.24 | 24.58 ± 9.57 | 37.03 ± 24.43 | 2.54 | 0.012 |
| IL-8 | 47.99 ± 23.39 | 24.06 ± 10.48 | 34.52 ± 20.98 | 7.47 | < 0.01 |
| IL-10 | 11.43 ± 4.83 | 9.44 ± 3.89 | 10.31 ± 4.42 | 2.49 | 0.014 |
| CRP | 21.76 ± 18.12 | 10.00 ± 5.55 | 15.14 ± 13.91 | 5.022 | < 0.01 |
| C1q | 207.44 ± 49.24 | 174.84 ± 66.86 | 189.08 ± 61.75 | 2.949 | 0.004 |
The inclusion criteria for our study were: (1) Age ≥ 50 years; (2) Diagnosis of disease met the criteria for hip fracture; and (3) Patients received surgical treatment in our hospital. Exclusion criteria: (1) No surgical treatment; (2) Hip fracture due to high energy injury; (3) Open fracture; (4) Fracture occurred with excessive blood loss; (5) Associated with bone metabolic or inflammatory diseases; (6) Received medications affecting bone metabolism and inflammatory factors such as glucocorticoids, antibiotics, calcitonin, bisphosphonates, etc. prior to admission to the hospital; (7) Pathological fracture; and (8) Patients with severe liver and kidney disease and malignancy.
The hip function is classified according to the Harris hip function scale, which is used to assess the outcome of various hip disorders, including: (1) Pain; (2) Function; (3) Deformity; and (4) Joint mobility. The score greater than or equal to 80 was classified as excellent group, and the score less than 80 was classified as fair group. The visual analogue scale (VAS)[20], is a visual analogue of the severity of pain. The scale is divided into 10 equal parts using a ruler, starting at 0 for no pain, 1-3 for mild pain, 4-6 for moderate pain, and 7-10 for severe pain, allowing the patient to subjectively state where they are on the scale and thus express the level of pain.
The following clinical characteristics were collected and reviewed by two experts: Age, sex, hypertension, diabetes, fracture laterality, type of fracture site, surgical approach, time from injury to surgery, VAS score, and length of hospital stay.
In addition, laboratory tests that may affect the prognosis of patients with hip fractures were also collected and analyzed, specifically. Neutrophil count, lymphocyte count, IL-6, IL-8, IL-10, CRP, serum C1q. Finally, all clinical information collected was independently reviewed and confirmed by another specialist.
The measurement data were expressed as mean ± SD, and the count data were expressed as the number of cases and percentage; the t-test for independent samples was used for measurement data between groups, and the chi-square test was used for count data. The covariates that were statistically significant after one-way logistic analysis were further analyzed using multiple logistic regression to determine the risk factors affecting functional limitation of the hip joint after hip fracture surgery, with P < 0.05 being considered statistically significant. IBM SPSS Statistics 25 software was used for statistical analysis of the relevant data and GraphPad Prism 9 software was used for the graphical interpretation of the findings.
A total of 119 elderly patients with hip fractures from Shanghai East Hospital affiliated with Tongji University were included in this study. 67 patients had fair hip function after surgery and 52 patients had excellent hip function after surgery. As shown in Table 1, there were significant differences in IL-6, IL-8, IL-10, CRP, and C1q (P < 0.05). However, there were no significant differences in age, gender, hypertensive disease, diabetes, fracture location, surgical approach, time from injury to surgery, serum neutrophil count, and lymphocyte count (P > 0.05).
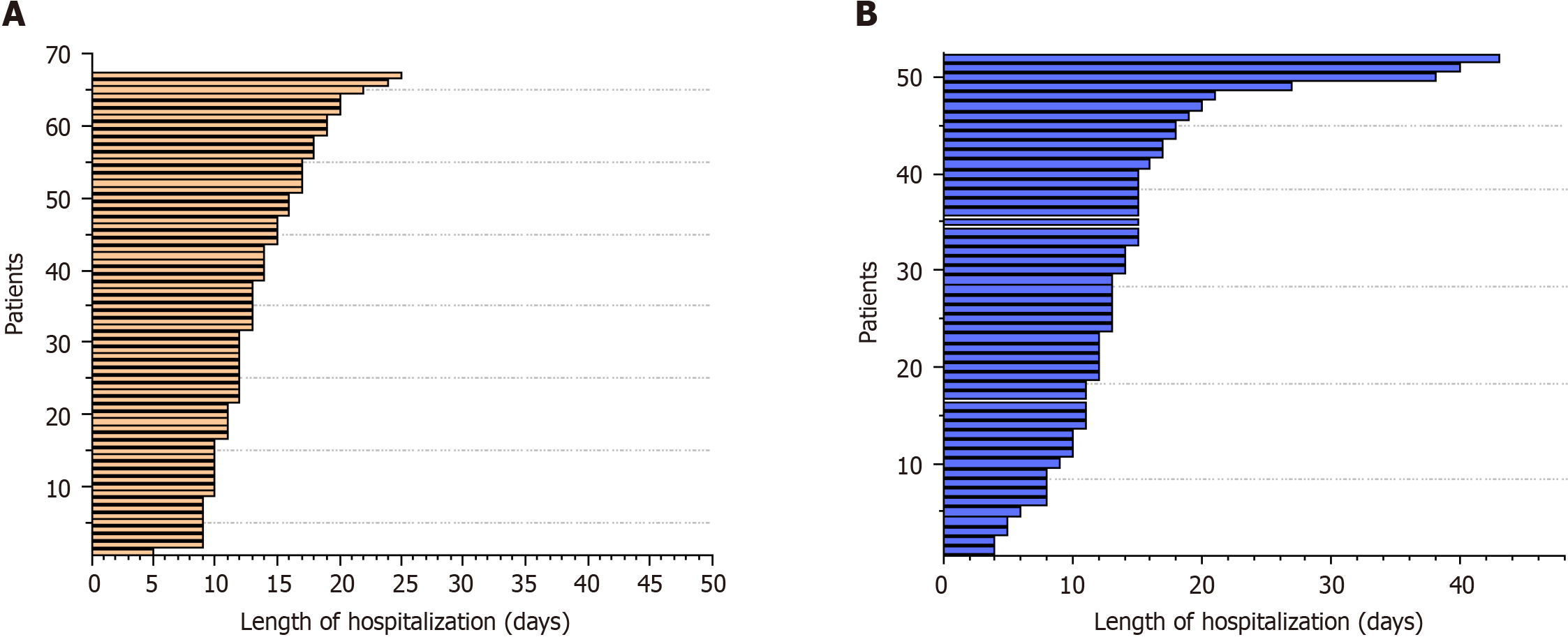
The differences between the two groups were statistically significant (P < 0.05) in terms of length of hospital stay (Figure 1), while the differences in VAS scores were not statistically significant (P > 0.05). Table 2 shows outcomes for both groups of patients during the observation period
| Fair hip function after surgery (n = 67) | Excellent hip function after surgery (n = 52) | F. group vs E. group | ||
| Outcome | mean ± SD | mean ± SD | Mean diff. (95%CI) | P value |
| VAS | 2.03 ± 0.82 | 1.85 ± 0.78 | 0.18 (-0.11-0.48) | 0.827 |
| Length of hospitalization | 14.31 ± 7.85 | 13.72 ± 3.98 | 0.59 (1.60-2.78) | 0.036 |
The risk factors from the univariate regression analysis were included in the multivariate logistic regression analysis, and as shown in Table 3 and Figure 2, IL-6 > 20 pg/mL [(Odds ratio (OR) 3.070, 95%CI: 1.243-7.579], IL-8 > 21.4 pg/ mL (OR 3.827, 95%CI: 1.498-9.773), CRP > 10 mg/L (OR 2.142, 95%CI: 1.020-4.498) and C1q > 233 mg/L (OR 2.339, 95%CI: 1.094-5.004) were independent risk factors for limited hip mobility after hip fracture surgery (all P < 0.05).
| Items | β | SE | OR | 95%CI | P |
| IL-6 > 20 pg/mL | 1.122 | 0.461 | 3.070 | 1.243-7.579 | 0.015 |
| IL-8 > 21.4 pg/mL | 1.342 | 0.478 | 3.827 | 1.498-9.773 | 0.005 |
| IL-10 > 5.90 pg/mL | 0.719 | 0.438 | 2.053 | 0.871-4.841 | 0.10 |
| CRP > 10 mg/L | 0.762 | 0.379 | 2.142 | 1.020-4.498 | 0.044 |
| C1q > 233 mg/L | 0.850 | 0.388 | 2.339 | 1.094-5.004 | 0.028 |
The years 2020 to 2030 are known as the decade of healthy ageing[21]. As the population ages, hip fractures are becoming more common in the elderly population, and in those over 65 years of age, hip fractures can lead to serious complications and reduce life expectancy[22,23]. The current treatment is still mainly surgical, but due to advanced age, weak organ function, and already existing comorbidities, often patients undergo surgery with a high mortality rate and multiple complication outcomes[3,12], therefore the identification of risk factors, as well as stratification of inpatients and precise and personalized treatment, is beneficial to improve the prognosis of elderly hip fracture patients. However, there is a lack of accurate clinical indicators for prognosticating hip function after hip fracture surgery in the elderly. This study focuses on analysing the possible association between inflammatory factor levels and hip function after hip fracture surgery in the elderly. Our findings suggest that IL-6 > 20 pg/mL, IL-8 > 21.4 pg/mL, CRP > 10 mg/L, and C1q > 233 mg/L are independent risk factors for poorer postoperative joint function in hip fracture patients, and that there are significant differences in length of hospital stay in these study subjects (P < 0.05). Thus, these suggest that physicians may need to take clinical measures to address these risk factors to prevent the occurrence and development of postoperative complications.
Numerous investigations have examined the evaluation of patients’ mortality, morbidity, and voluntary mobility following hip fractures. According to Xu et al[24] elderly hip fracture patients’ grip strength and weakness may be predictive of unfavorable outcomes. Thomas et al[25] compared the effects of the various surgical schedules on health outcomes in hip fracture patients and showed that delaying the timing of surgery in patients with poor health status did not have a beneficial effect. Furthermore, there is some disagreement over the risk factors reported in various nations and areas. For instance, one study found that women are more likely than men to suffer hip fractures that result in poor outcomes[26], while another study found that male patients are more likely to experience complications from hip fractures[27]. This could be due to their coexistence with multiple underlying conditions and poor habits. The development of databases and predictive indicators is essential to improving poor patient outcomes and boosting public health efficiency and well-being due to the world’s and China’s growing aging populations. Our study was based on a Shanghai population with a mean age of 76.4 ± 12.29 years, with the highest age of patients being 100 years. In addition to normal blood tests and CRP, our study focused more on lymphokines and complement, which have received less research attention, as we believe these factors play an irreplaceable role in fracture occurrence and bone healing throughout.
When a hip fracture occurs, immune cells around the fracture site secrete cytokines such as pro-inflammatory IL-6, IL-8, and anti-inflammatory IL-10[28,29], which stimulate mesenchymal stem cells (MSCs) to migrate to the fracture site and promote fracture repair, these lymphokines and CRP were also found to be significantly elevated in the serum of elderly hip fracture patients with coexisting complications[30]. Some studies have reported CRP as a major risk factor for death after hip fracture[17,31], this is consistent with our study that CRP is a risk factor for poor joint function. In addition, our finding that gender and fracture type did not correlate with hip fracture was also consistent with the finding of Yu et al[32].
We also looked at cytokines and complements, which are less common in other Chinese hospitals, in addition to CRP. Furthermore, although the Harris score is frequently employed to measure hip function in patients both before and after surgery, it is important to investigate how it correlates with other variables because there aren’t many studies emphasizing the importance of inflammatory factors on joint function. C1q levels are associated with inflammation-related and metabolic diseases[33], and hip fracture in the elderly as a fragility fracture, therefore C1q was also included in the study protocol, and the results showed that C1q is an independent risk factor for fair joint function after hip fracture surgery. In contrast, IL-10 was not found to be a risk factor for fair hip function in this study, probably because the timing of the appearance of each cytokine after trauma varies and IL-10 as an anti-inflammatory factor was not elevated to the concentration level it should be during the hospital stay.
There are some limitations to this study. Firstly, this is a single-center retrospective study with small sample size, potential confounding factors that may affect the clarity of the results, and the ability to detect differences between groups may be inadequate. However, from the beginning of the study, we set uniform standards, with two specialist physicians independently collecting data and checking by a senior physician to reduce study bias, although we would need multi-center institutions and hospitals and larger sample sizes to eliminate bias. Secondly, we only observed and analyzed functional activity and tests during hospitalization in elderly hip fracture patients. To better reflect the prognosis of the patients, we also added additional outcome factors like VAS and length of stay. However, because the patients’ circumstances varied and their privacy was protected, we did not investigate complications or mortality after discharge. It is planned that additional prospective research would be carried out in the future to examine the risk variables influencing hip function following surgery.
In conclusion, this study indicates several risk factors for less favourable prognosis of joint function in hip fracture patients, and these predictors may help alert physicians to develop rehabilitation protocols and early intervention.
The incidence of hip fractures and postoperative complications in the elderly is increasing. With the advent of the aging society, addressing this public health problem is becoming a non-negligible issue. At present, while the risk factors of hip function recovery after hip fracture in elderly patients are subjects of recent investigation, their specific impact on populations with hip fractures remains relatively not investigated.
In elderly people with hip fractures, the relationship between various inflammatory markers and joint function remains to be further studied.
This study aims to reveal the potential impact of inflammation on joint function in elderly patients with hip fractures, which may provide new approaches for the treatment and rehabilitation of hip fractures.
Of 119 patients with hip fractures who underwent elective surgery at Shanghai East Hospital between January 1, 2021, and December 31, 2022 were included in this retrospective analysis. Participants’ comprehensive clinical data, including: Age, sex, hypertension, diabetes, type of fracture site, surgical approach, time from injury to surgery, visual analogue scale score, and length of hospital stay, were collected and analyzed using statistical software. For the measurement data between groups, the independent samples t-test was employed, and for the count data, the chi-square test was utilised. To ascertain the risk factors influencing the functional limitation of the hip joint following a hip fracture, additional multivariate logistic regression analyses were carried out on the covariates that were statistically significant by one-way logistic analysis, with P < 0.05 being deemed statistically significant.
In this study involving 119 participants with an average age ≥ 75 years, there were no significant differences in age, sex, hypertensive disease, diabetes, fracture types, surgical approach, injury to surgery time, serum neutrophil count, and lymphocyte count. There were significant differences in interleukin (IL)-6, IL-8, IL-10, C-reactive protein (CRP), and complement C1q (C1q) between the two groups. Notably, we also looked at cytokines and complement, which have received relatively less attention in other hospitals in China, and these findings suggest several inflammation-related risk factors for fair joint function in patients with hip fractures.
To sum up, CRP, IL-6, IL-8 and C1q in patients with fair hip function after surgery were significantly higher than those in patients with excellent hip function in our study.
These results suggest that there is a certain correlation between inflammatory factors and the postoperative function of hip fracture, and provide a fresh approach for future research of the relationship between inflammation and joint function.
| 1. | Zhang C, Feng J, Wang S, Gao P, Xu L, Zhu J, Jia J, Liu L, Liu G, Wang J, Zhan S, Song C. Incidence of and trends in hip fracture among adults in urban China: A nationwide retrospective cohort study. PLoS Med. 2020;17:e1003180. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 213] [Cited by in RCA: 233] [Article Influence: 38.8] [Reference Citation Analysis (1)] |
| 2. | Dhanwal DK, Dennison EM, Harvey NC, Cooper C. Epidemiology of hip fracture: Worldwide geographic variation. Indian J Orthop. 2011;45:15-22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 474] [Cited by in RCA: 426] [Article Influence: 28.4] [Reference Citation Analysis (2)] |
| 3. | Leibson CL, Tosteson AN, Gabriel SE, Ransom JE, Melton LJ. Mortality, disability, and nursing home use for persons with and without hip fracture: a population-based study. J Am Geriatr Soc. 2002;50:1644-1650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 461] [Cited by in RCA: 499] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 4. | Abraham DS, Barr E, Ostir GV, Hebel JR, Golden J, Gruber-Baldini AL, Guralnik JM, Hochberg MC, Orwig DL, Resnick B, Magaziner JS. Residual Disability, Mortality, and Nursing Home Placement After Hip Fracture Over 2 Decades. Arch Phys Med Rehabil. 2019;100:874-882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 5. | Chen M, Du Y, Tang W, Yu W, Li H, Zheng S, Cheng Q. Risk factors of mortality and second fracture after elderly hip fracture surgery in Shanghai, China. J Bone Miner Metab. 2022;40:951-959. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 6. | Schemitsch EH, Sprague S, Heetveld MJ, Bzovsky S, Heels-Ansdell D, Zhou Q, Swiontkowski M, Bhandari M; FAITH Investigators. Loss of Independence After Operative Management of Femoral Neck Fractures. J Orthop Trauma. 2019;33:292-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 7. | Meng D, Bai X, Wu H, Yao S, Ren P, Lu C, Song Z. Patient and Perioperative Factors Influencing the Functional Outcomes and Mortality in Elderly Hip Fractures. J Invest Surg. 2021;34:262-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 8. | Cooper C, Cole ZA, Holroyd CR, Earl SC, Harvey NC, Dennison EM, Melton LJ, Cummings SR, Kanis JA; IOF CSA Working Group on Fracture Epidemiology. Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int. 2011;22:1277-1288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 729] [Cited by in RCA: 703] [Article Influence: 46.9] [Reference Citation Analysis (0)] |
| 9. | Cheung CL, Ang SB, Chadha M, Chow ES, Chung YS, Hew FL, Jaisamrarn U, Ng H, Takeuchi Y, Wu CH, Xia W, Yu J, Fujiwara S. An updated hip fracture projection in Asia: The Asian Federation of Osteoporosis Societies study. Osteoporos Sarcopenia. 2018;4:16-21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 227] [Cited by in RCA: 256] [Article Influence: 32.0] [Reference Citation Analysis (0)] |
| 10. | Cauley JA, Chalhoub D, Kassem AM, Fuleihan Gel-H. Geographic and ethnic disparities in osteoporotic fractures. Nat Rev Endocrinol. 2014;10:338-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 277] [Article Influence: 23.1] [Reference Citation Analysis (0)] |
| 11. | Leal J, Gray AM, Prieto-Alhambra D, Arden NK, Cooper C, Javaid MK, Judge A; REFReSH study group. Impact of hip fracture on hospital care costs: a population-based study. Osteoporos Int. 2016;27:549-558. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 196] [Cited by in RCA: 279] [Article Influence: 27.9] [Reference Citation Analysis (0)] |
| 12. | Hu F, Jiang C, Shen J, Tang P, Wang Y. Preoperative predictors for mortality following hip fracture surgery: a systematic review and meta-analysis. Injury. 2012;43:676-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 499] [Cited by in RCA: 488] [Article Influence: 34.9] [Reference Citation Analysis (0)] |
| 13. | Bian S, Hu J, Zhang K, Wang Y, Yu M, Ma J. Dairy product consumption and risk of hip fracture: a systematic review and meta-analysis. BMC Public Health. 2018;18:165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 67] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 14. | Thisayakorn P, Tangwongchai S, Tantavisut S, Thipakorn Y, Sukhanonsawat S, Wongwarawipat T, Sirivichayakul S, Maes M. Immune, Blood Cell, and Blood Gas Biomarkers of Delirium in Elderly Individuals with Hip Fracture Surgery. Dement Geriatr Cogn Disord. 2021;50:161-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 15. | Fischer V, Haffner-Luntzer M. Interaction between bone and immune cells: Implications for postmenopausal osteoporosis. Semin Cell Dev Biol. 2022;123:14-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 466] [Article Influence: 93.2] [Reference Citation Analysis (0)] |
| 16. | Haller JM, Marchand L, Rothberg DL, Kubiak EN, Higgins TF. Inflammatory cytokine response is greater in acute tibial plafond fractures than acute tibial plateau fractures. J Orthop Res. 2017;35:2613-2619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Kim BG, Lee YK, Park HP, Sohn HM, Oh AY, Jeon YT, Koo KH. C-reactive protein is an independent predictor for 1-year mortality in elderly patients undergoing hip fracture surgery: A retrospective analysis. Medicine (Baltimore). 2016;95:e5152. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 45] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 18. | Son M. Understanding the contextual functions of C1q and LAIR-1 and their applications. Exp Mol Med. 2022;54:567-572. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 19. | Chumchuen S, Apivatgaroon A, Phanichwong P, Kanokvaleewong C, Pinsornsak P, Pongcharoen B. Validity and Reliability of the Thai Version of the Modified Harris Hip Score for Patients With Hip Abnormalities. Orthop J Sports Med. 2022;10:23259671221141095. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 20. | Bielewicz J, Daniluk B, Kamieniak P. VAS and NRS, Same or Different? Pain Res Manag. 2022;2022:5337483. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 67] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 21. | Amuthavalli Thiyagarajan J, Mikton C, Harwood RH, Gichu M, Gaigbe-Togbe V, Jhamba T, Pokorna D, Stoevska V, Hada R, Steffan GS, Liena A, Rocard E, Diaz T. The UN Decade of healthy ageing: strengthening measurement for monitoring health and wellbeing of older people. Age Ageing. 2022;51. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 106] [Article Influence: 26.5] [Reference Citation Analysis (0)] |
| 22. | Kannus P, Niemi S, Parkkari J, Palvanen M, Vuori I, Järvinen M. Hip fractures in Finland between 1970 and 1997 and predictions for the future. Lancet. 1999;353:802-805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 226] [Cited by in RCA: 222] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 23. | Kristensen MT, Foss NB, Ekdahl C, Kehlet H. Prefracture functional level evaluated by the New Mobility Score predicts in-hospital outcome after hip fracture surgery. Acta Orthop. 2010;81:296-302. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 98] [Cited by in RCA: 128] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 24. | Xu BY, Yan S, Low LL, Vasanwala FF, Low SG. Predictors of poor functional outcomes and mortality in patients with hip fracture: a systematic review. BMC Musculoskelet Disord. 2019;20:568. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 217] [Article Influence: 31.0] [Reference Citation Analysis (0)] |
| 25. | Klestil T, Röder C, Stotter C, Winkler B, Nehrer S, Lutz M, Klerings I, Wagner G, Gartlehner G, Nussbaumer-Streit B. Immediate vs delayed surgery for hip fractures in the elderly patients: a protocol for a systematic review and meta-analysis. Syst Rev. 2017;6:164. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 26. | Veronese N, Maggi S. Epidemiology and social costs of hip fracture. Injury. 2018;49:1458-1460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 307] [Cited by in RCA: 635] [Article Influence: 79.4] [Reference Citation Analysis (0)] |
| 27. | Tian Y, Zhu Y, Zhang K, Tian M, Qin S, Li X, Zhang Y. Incidence and risk factors for postoperative pneumonia following surgically treated hip fracture in geriatric patients: a retrospective cohort study. J Orthop Surg Res. 2022;17:179. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 28. | Mountziaris PM, Mikos AG. Modulation of the inflammatory response for enhanced bone tissue regeneration. Tissue Eng Part B Rev. 2008;14:179-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 321] [Cited by in RCA: 352] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 29. | Kon T, Cho TJ, Aizawa T, Yamazaki M, Nooh N, Graves D, Gerstenfeld LC, Einhorn TA. Expression of osteoprotegerin, receptor activator of NF-kappaB ligand (osteoprotegerin ligand) and related proinflammatory cytokines during fracture healing. J Bone Miner Res. 2001;16:1004-1014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 418] [Cited by in RCA: 410] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 30. | Beloosesky Y, Grinblat J, Pirotsky A, Weiss A, Hendel D. Different C-reactive protein kinetics in post-operative hip-fractured geriatric patients with and without complications. Gerontology. 2004;50:216-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 67] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 31. | Sedlár M, Kudrnová Z, Erhart D, Trca S, Kvasnicka J, Krska Z, Mazoch J, Malíková I, Zeman M, Linhart A. Older age and type of surgery predict the early inflammatory response to hip trauma mediated by interleukin-6 (IL-6). Arch Gerontol Geriatr. 2010;51:e1-e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 32. | Yu S, Li C, Zhong Y, Zang J, Zhou Z, Wang S, Zhang Y. Risk factors for contralateral hip refractures in patients aged over 80 years with intertrochanteric femoral fractures. Front Surg. 2022;9:924585. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 33. | Veerhuis R, Nielsen HM, Tenner AJ. Complement in the brain. Mol Immunol. 2011;48:1592-1603. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 353] [Cited by in RCA: 334] [Article Influence: 22.3] [Reference Citation Analysis (10)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Buckley RE, Canada S-Editor: Liu H L-Editor: A P-Editor: Zhao YQ