Published online Mar 18, 2024. doi: 10.5312/wjo.v15.i3.215
Peer-review started: December 3, 2023
First decision: January 6, 2024
Revised: January 11, 2024
Accepted: February 2, 2024
Article in press: February 2, 2024
Published online: March 18, 2024
Processing time: 103 Days and 4.2 Hours
In recent years, the use of Magnesium alloy implants have gained renewed popularity, especially after the first commercially available Conformité Européenne approved Magnesium implant became available (MAGNEZIX® CS, Syntellix) in 2013.
To document our clinical and radiographical outcomes using magnesium implants in treating peri-articular elbow fractures.
Our paper was based on a retrospective case series design. Intra-operatively, a standardized surgical technique was utilized for insertion of the magnesium implants. Post – operatively, clinic visits were standardized and physical exam findings, functional scores, and radiographs were obtained at each visit. All complications were recorded.
Five patients with 6 fractures were recruited (2 coronoid, 3 radial head and 1 capitellum). The mean patient age and length of follow up was 54.6 years and 11 months respectively. All fractures healed, and none exhibited loss of reduction or complications requiring revision surgery. No patient developed synovitis of the elbow joint or suffered electrolytic reactions when titanium implants were used concurrently.
Although there is still a paucity of literature available on the subject and further studies are required, magnesium implants appear to be a feasible tool for fixation of peri-articular elbow fractures with promising results in our series.
Core Tip: Magnesium implants can be a useful tool in fixation of peri-articular elbow fractures with promising results.
- Citation: Fang C, Premchand AXR, Park DH, Toon DH. Peri-articular elbow fracture fixations with magnesium implants and a review of current literature: A case series. World J Orthop 2024; 15(3): 215-229
- URL: https://www.wjgnet.com/2218-5836/full/v15/i3/215.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i3.215
In recent years, the use of Magnesium alloy implants in orthopaedic surgeries have gained renewed popularity. Apart from being bioabsorbable, negating the need for implant removal, magnesium also has good osteoconductive properties[1-4]. Biomechanically, it exhibits greater biomechanical strength than any pre-existing polymers, and reduces the stress-shielding effect associated with titanium and steel implants as it has a Young’s modulus closer to bone[4].
Currently, the main utility of magnesium implants in the orthopaedic community is within the foot and ankle community where satisfactory results have been reported with its utility in forefoot osteotomies[5-7]. However, its utility in the setting of orthopaedic trauma has been steadily increasing[8].
Our study aims to document our clinical and radiographical outcomes using magnesium implants to treat peri-articular elbow fractures. To our knowledge, our study is the first study analyzing outcomes in radial head and coronoid fractures in the English literature.
This study is a retrospective case series analyzing the clinical and radiographical outcomes of patients with peri-articular fractures of the upper limb, specifically the radial head, coronoid and capitellum, that were surgically treated with bioabsorbable magnesium screws (MAGNEZIX®, Syntellix AG, Hanover, Germany).
Domain specific review board approval was obtained prior to initiation of the study. Patients were recruited over the duration of 8 months from May 2019 to December 2019. All patients recruited were adult aged 21 years old and above, with isolated, closed peri-articular fractures of the elbow and no neurovascular compromise presenting to our institution. Pre-operatively, all patients were counselled regarding the usage of the magnesium implants and the risks and benefits of surgical fixation were extensively explained.
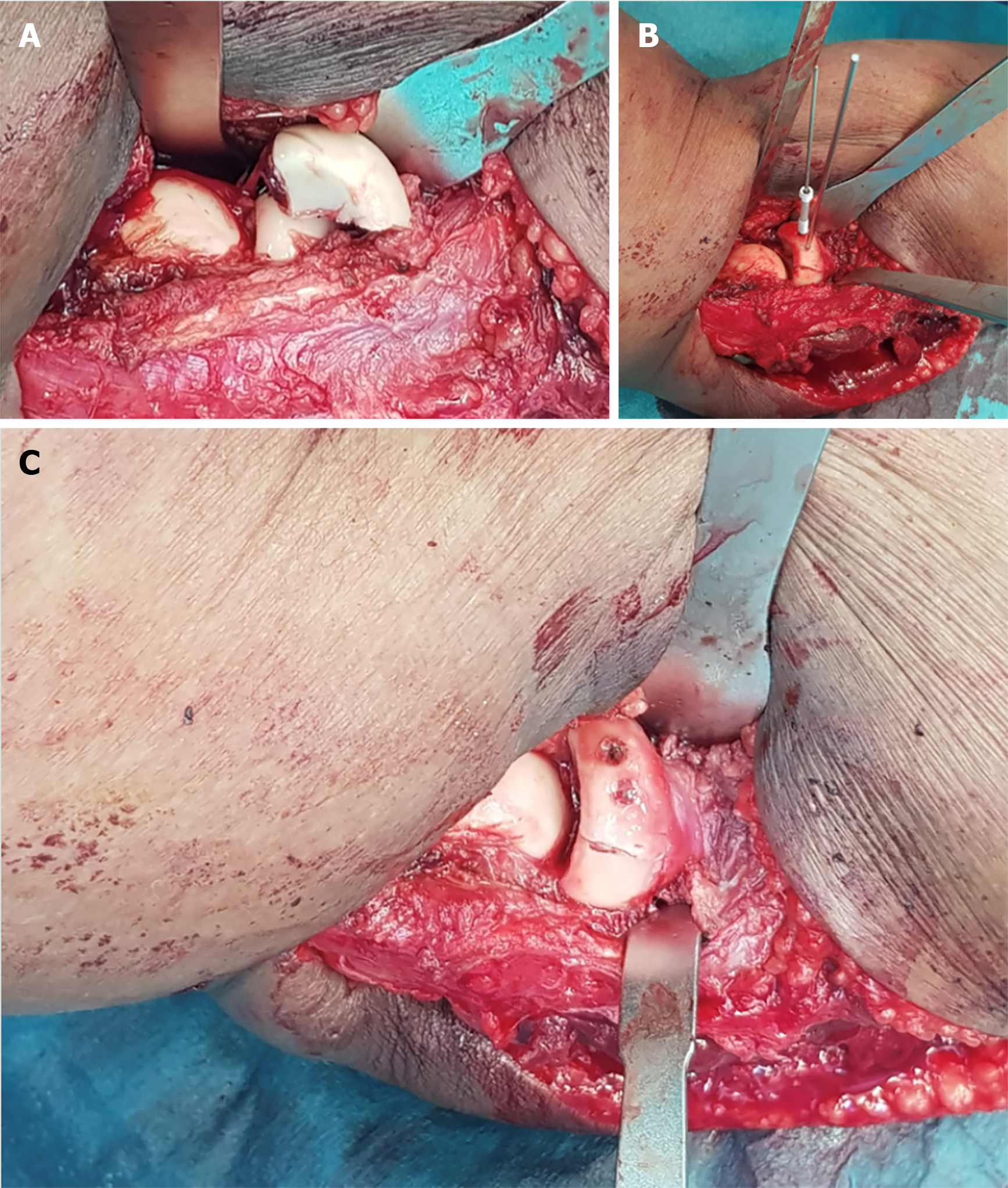
All patients recruited underwent surgery performed by one of the senior authors of this study with a standardised surgical technique for implantation of the magnesium compression screws in accordance with the manufacturers recommendation. Intra-operatively, after temporary reduction with Kirschner-wires, a cannulated drill was utilised to create a pilot hole before the main hole is drilled and the screw inserted over the Kirschner-wire. Care was taken not to apply excessive torque during screw insertion.
Post-operatively, all patients were started immediately on a progressive occupational therapy regime. Passive range of motion was allowed immediately post operatively followed by graduated progression to active range of motion within 2-3 wk. All patients had regular therapy visits post-operatively for supervised sessions. Patients underwent a standardised follow up regime with the primary surgeon at 2 wk, 4 wk, 6 wk, 3 months, 6 months and 1 year post-operatively. During each visit, clinical notes were taken for each patient documenting relevant history and physical exam findings. Two functional scores, namely the Mayo elbow performance score (MEPS) and disabilities of the arm, shoulder and hand (DASH) score was also recorded at each visit. All complications were recorded.
Our study studied a total of 5 patients with 6 fractures, 2 of the coronoid, 3 of the radial head and 1 of the capitellum. The mean age at the time of surgery was 54.6 years of age ranging from 34 to 76 years old, and the mean length of follow up was 11 months, ranging from 7 to 13 months.
All 5 patients exhibited good short to medium term clinical outcomes with a mean MEPS of 100 points and a mean DASH score of 2.72 points (0.8–10.3 points) at final follow up. No fractures exhibited any loss of reduction at the point of final follow up, and there were no complications or revision surgeries required for all 5 patients. Notably, none of our patients developed any clinical signs or symptoms of synovitis of the elbow joint (Table 1).
| Fracture sustained | Follow up | Clinical outcomes scores (At latest follow up) | ROM (Latest follow up) | Clinical outcomes | ||
| Mayo score | DASH score | |||||
| 67/F | Bryan & Morrey Type 3 capitellum fracture | 7 months | 100 points | 0.8 points | 25-130 degrees; Full prono/supination | Pain free; Went back to work as a cleaner without issues |
| 34/M | Coronoid #: Regan and Morrey type 2 | 11 months | 100 points | 0.8 points | 10–130 degrees; Full prono/supination | Pain free; Went back to recreational exercise (football) |
| 58/M | Comminuted olecranon #; Radial head #: Mason type 2 | 13 months | 100 points | 0.9 points | 0-150 degrees; 80 degrees prono/supination | Went back to work as a machine operator |
| 38/M | Radial head #: Mason type 2 | 13 months | 100 points | 0.8 points | 0–150 degrees; Full prono/supination | Pain free; Back to Gym work including weights |
| 76/M | Terrible triad injury; Coronoid #: Regan and Morrey type 3; Radial head #: Mason type 4 | 11 months | 100 points | 10.3 points | 10–130 degrees; Full prono/supination | Posterior elbow pain (Olecranon bursitis) – Resolved; Pain free from six months onwards |
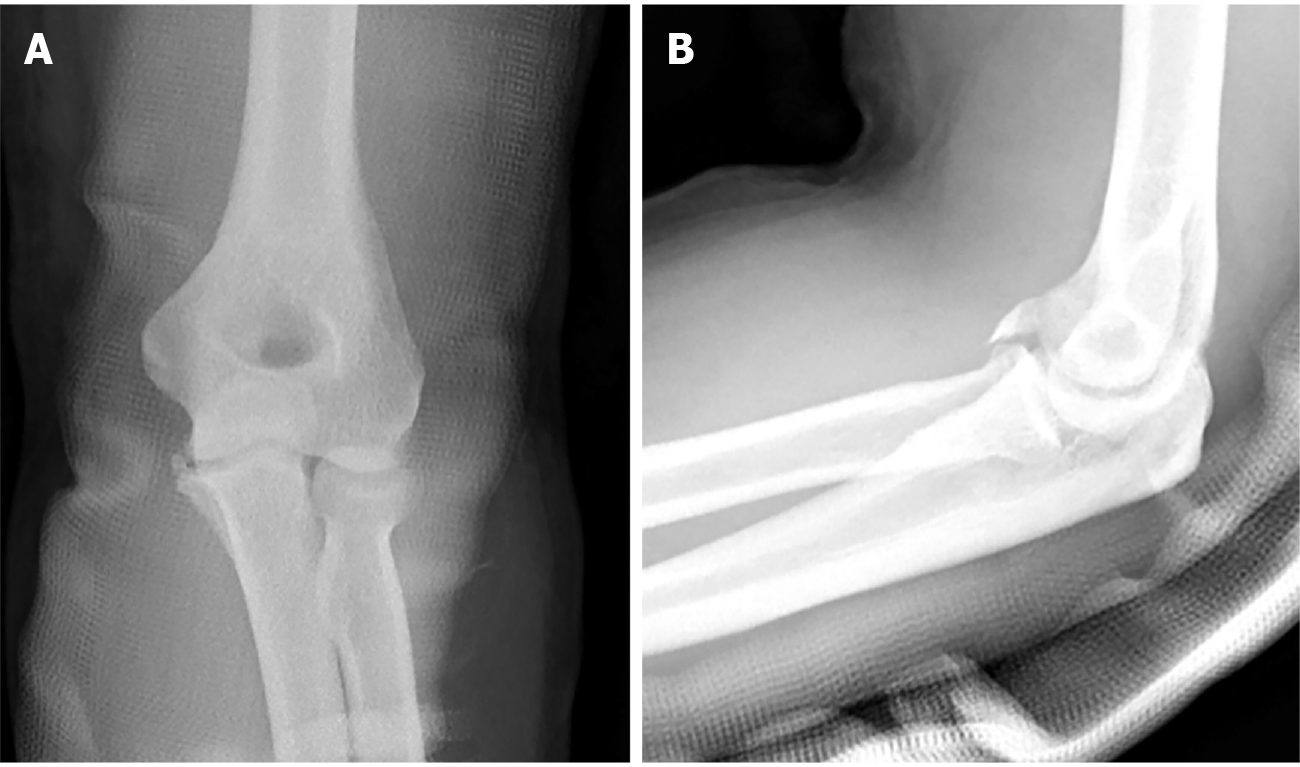
Patient one is a 67 year old, functionally active chinese lady with no past medical history who sustained a closed left Bryan and Morrey type 3 capitellar fracture after a mechanical fall from standing height (Figure 1).
Access to the elbow was obtained via a mid-axial approach after which fracture reduction was achieved under direct visualization and held with Kirschner wires. Four magnesium screws were then used to compress the fracture site before a 4 hole 1/3 tubular plate was cut and applied in a buttress fashion. Clinically, the patient was pain free by 2 wk and had obtained 25 to 130 degrees of elbow flexion and full prono/supination by the 6 months. At the point of latest follow up, she reported good functional outcomes scores, with a MEPS of 100 points and a DASH score of 0.8. She had also returned to her full time work as a cleaner without any difficulties.
One magnesium screw was noted to have broken at the 6 wk radiograph. However, there was no loss of fracture reduction and the fracture was noted to have united at 6 months post-op (Figure 2).
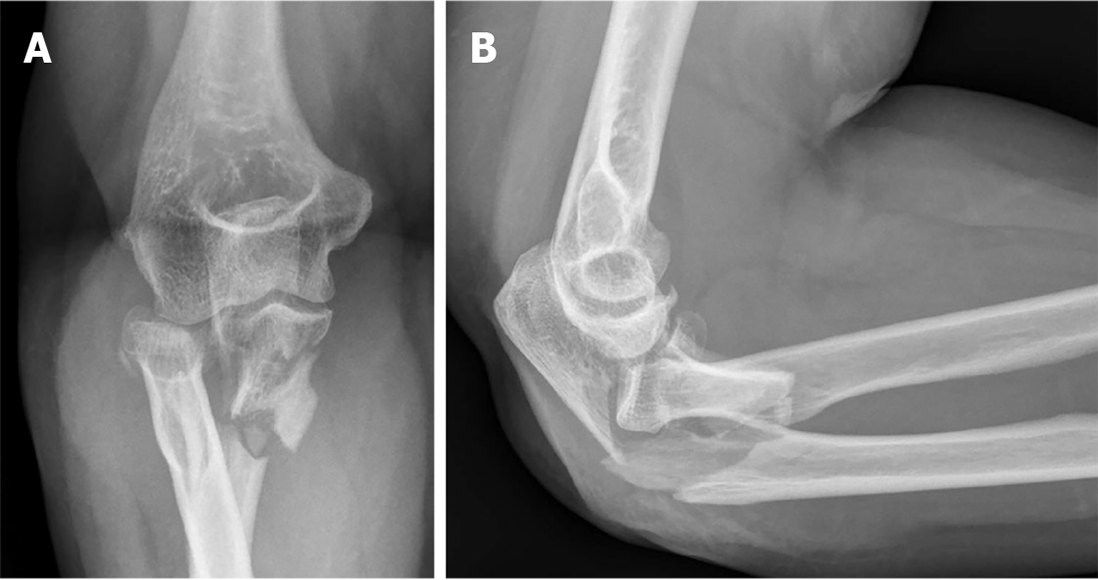
Patient two is a 34 year old male with no significant past medical history who sustained an isolated closed Regan and Morrey type 2 coronoid fracture. Intra-operatively the coronoid fracture was fixed using a Zimmer ALPS Coronoid plate applied in a buttress fashion and a Magnezix CS 2.7 mm compression screw for compression (Figure 3).
Fracture union was noted at 6 wk post-op, and by 6 months, he had obtained 10-130 degrees of elbow flexion, and managed to return to full work duties as well as recreational football. At the point of final follow up, he reported satisfactory functional outcome scores with a MEPS of 100 and a DASH score of 0.8 points (Figure 4).
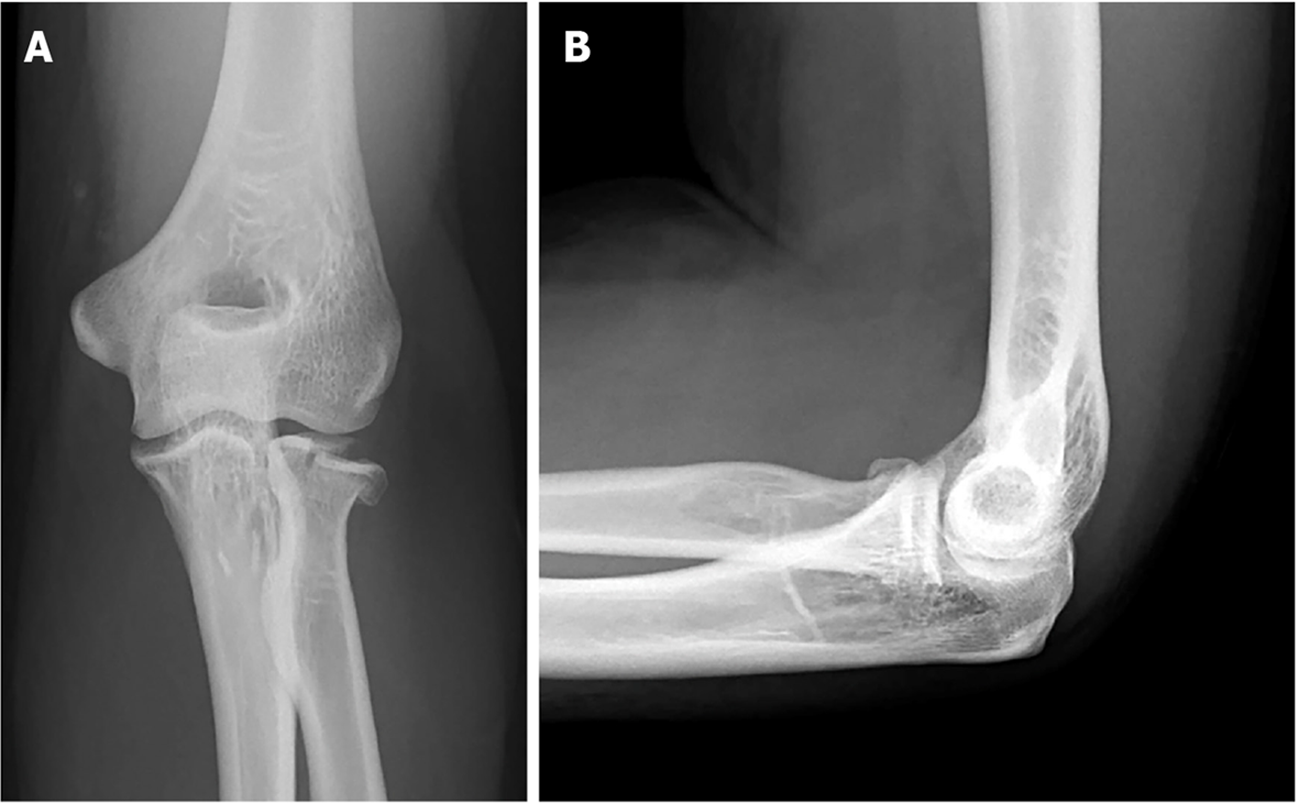
Patient three is a 58 year old functionally well lady with a significant past medical history of poorly controlled diabetes mellitus and hyperlipidaemia who sustained a closed Monteggia - variant fracture dislocation after a fall from standing height. (Figure 5) Pre – operatively, a computer tomography scan confirmed a comminuted olecranon fracture with a large ulnar butterfly fragment as well as a comminuted radial head fracture.
Intra-operatively, the olecranon fracture was fixed with traditional titanium implants (Zimmer ALPs system) whilst the radial head fracture was fixed with two Magnezix CS 2.7 mm headless compression screws.
By 6 wk post-operatively, she had obtained 10 to 130 degrees of elbow flexion, as well as 60 degrees and 50 degrees of pronation and supination respectively. At 6 months, this further improved to 0 to 150 degrees of flexion and 80 degrees of pronation and supination. At this point, she was pain free, and had returned to work as a machine operator without any difficulties. Fracture union was noted.
Radiographically, peri-implant radiolucencies became prominent around the 6 wk post-op, and gradually reduced up to the point of latest follow up at 1 year. At 6 months post-op, we noted breakage of one of the radial head screws, and by the 1 year post-op, the embedded magnesium implants were barely visible on the lateral view (Figure 6).
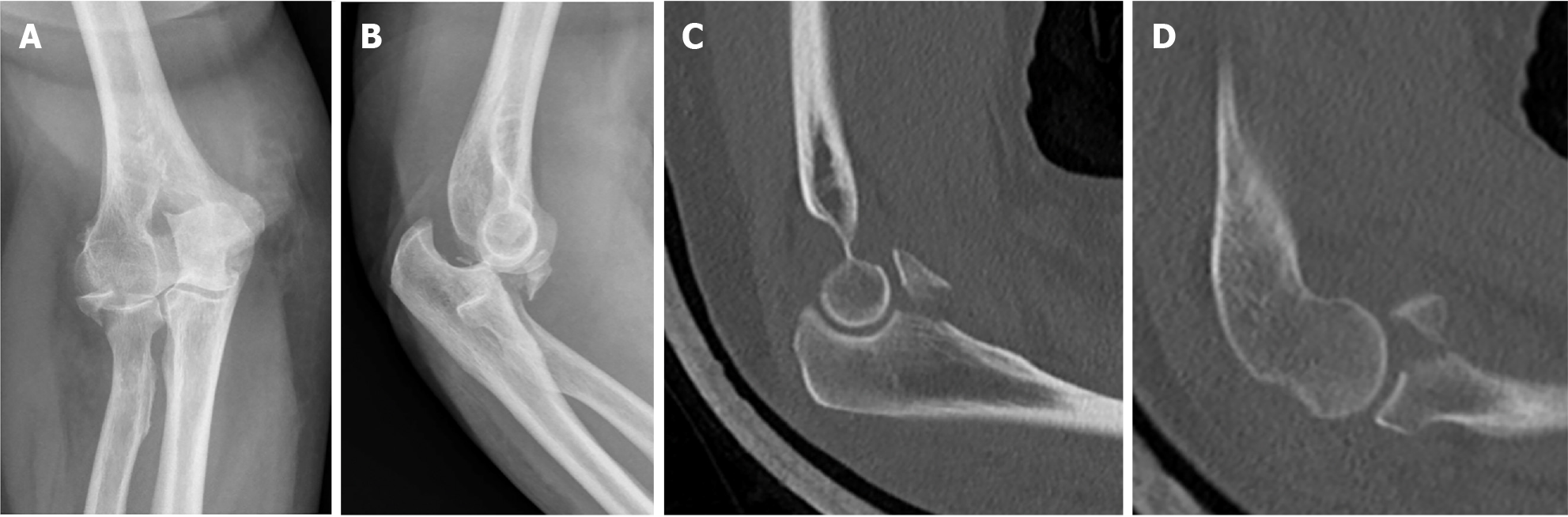
Patient four is a 38 year old male with no significant past medical history who sustained a closed Mason type 2 radial head fracture after a fall from a height (Figure 7).
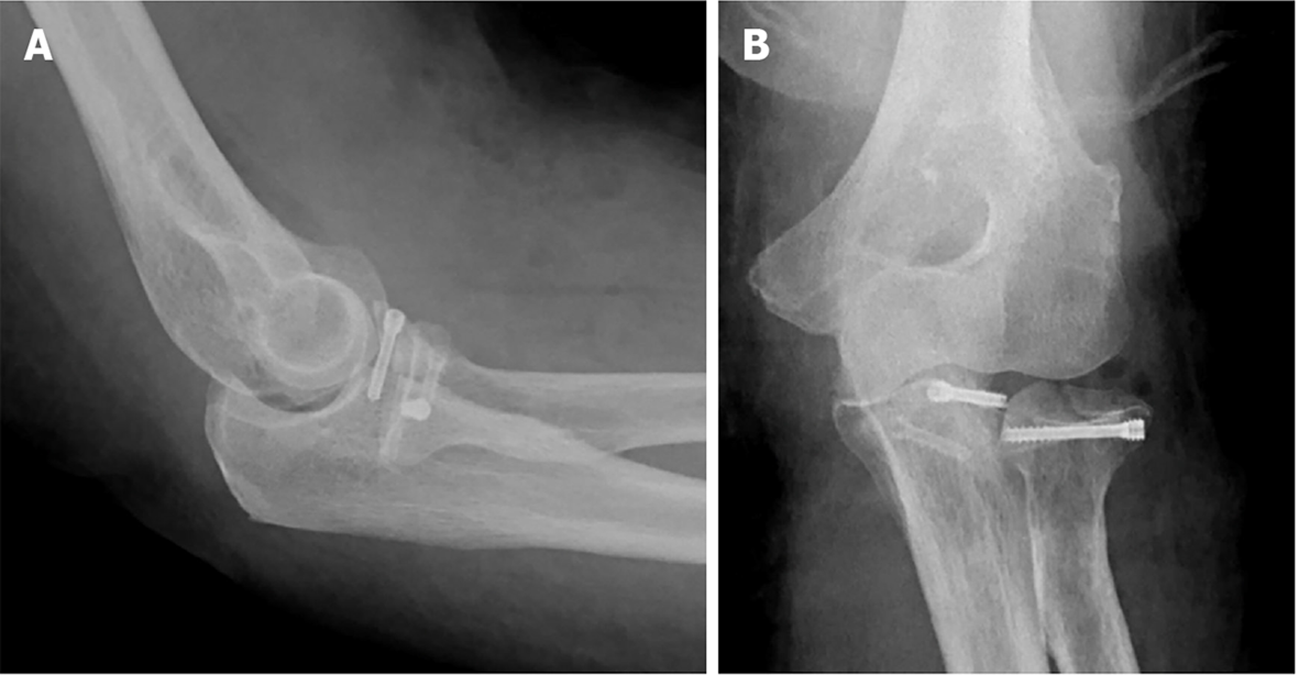
Intra-operatively, two Magnezix CS 2.7 mm screws were utilised for fixation and compression of the fracture. Full elbow range of motion was confirmed intra-operatively prior to closure (Figure 8).
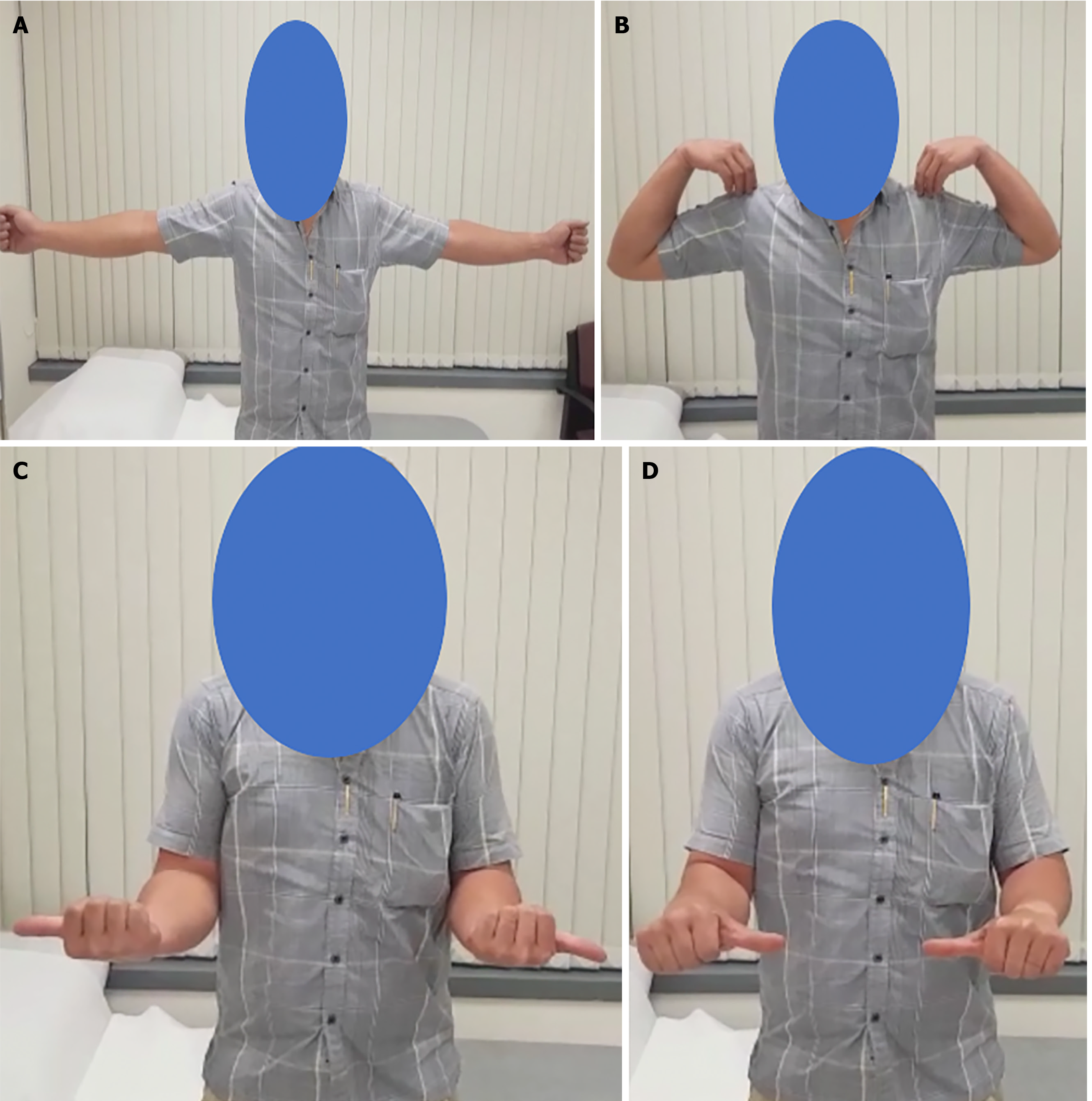
By 6 wk post-op, he had obtained 0 to 150 degrees of elbow flexion and 90 degrees of both pronation and supination, almost identical to the contralateral limb (Figure 9).
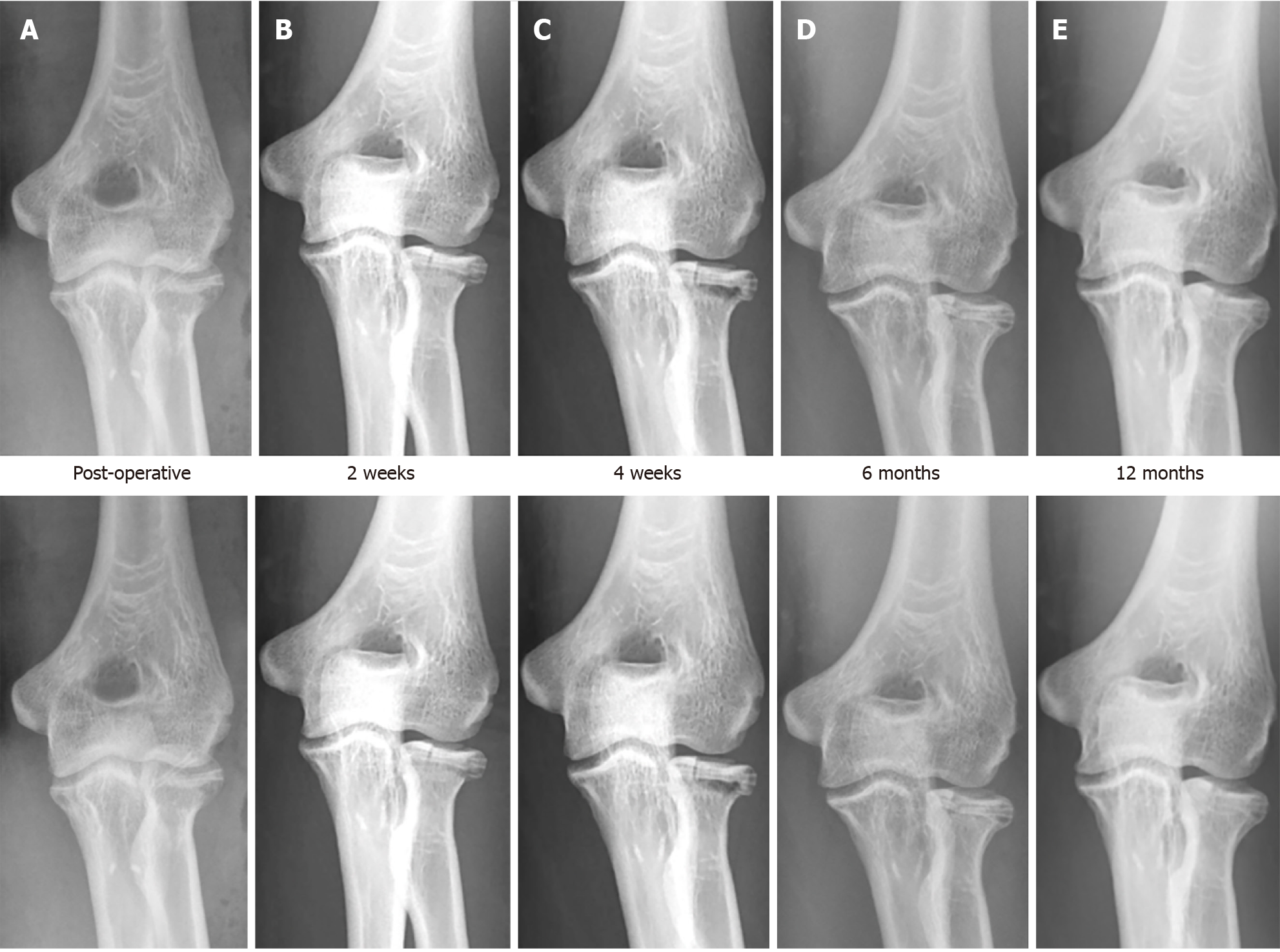
Radiographically we noted the appearance of peri-implant radiolucencies at 2 wk post-operatively, which became more pronounced by 4 wk before reducing significantly by 6 months and almost completely disappearing by 1 year. This observation is in keeping with gradual dissipation of hydrogen produced as a result of magnesium degradation. The distal tip of one of the Magnezix CS screws was noted to have broken off at 6 months post-operatively, during which time the fracture had already healed with no loss of fracture reduction. At 1 year, the broken screw tip had resorbed and was barely visible (Figure 10).
At the point of last follow up, the patient remained clinically asymptomatic and reported no perceivable differences functionally with the contra-lateral limb with a MEP of 100 points and a DASH score of 0.8 points.
Patient five is a 76 year old lady with good pre-morbid function who sustained a closed terrible triad injury (Regan and Morrey type 3 coronoid fracture and Mason 4 radial head fracture) (Figure 11).
Intra-operatively, both the radial head fracture and the coronoid fracture were fixed with a combination of one titanium (Medartis 2.0/2.5 mm Low Compression Screw) and one Magnezix CS 2.7 mm screw (Figure 12).
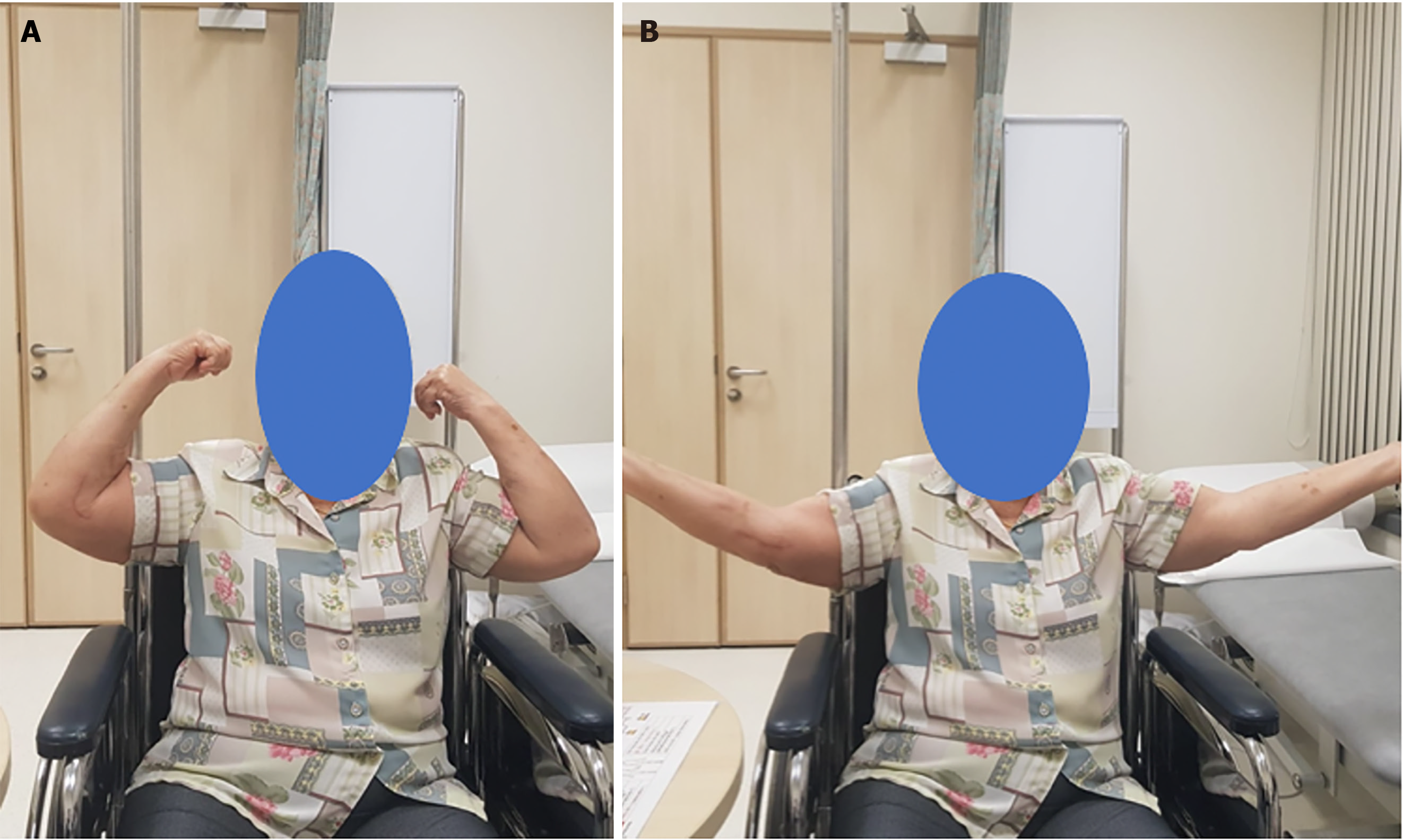
At 6 months post-op, the patient was noted to have elbow flexion from 10–130 degrees and full prono/supination which was identical to the contra-lateral limb. At the point of last follow up, she was pain free and was independent in all activities of daily living, and reported a MEPS of 100 points and a DASH score of 10.3 points (Figure 13).
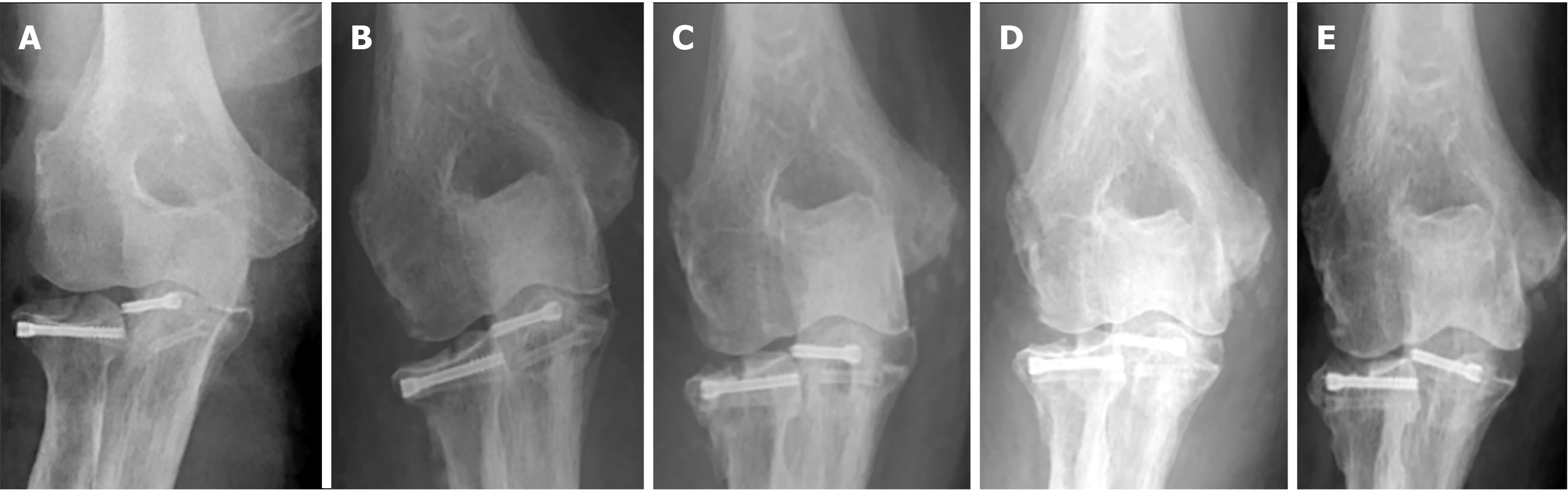
In similar fashion to patient two, at the 4 wk post-op, radiolucencies were noted over both Magnezix CS screws which reduced significantly by 6 months and almost completely disappeared by 1 year. Neither of screws had broken at 1 year post-op (Figure 14).
In our series of patients, we noted the presence of radiolucencies as early as 2 wk post-operatively, which consistently became more pronounced by 4 to 6 wk post-operatively. Significant reduction in radiolucencies were noted by 6 months post-operatively, and radiolucencies were minimal and barely visible by 1 year post-operatively.
At the one year mark post-operatively, we noted screw breakage in 3 out of 6 fractures, of which 2 occurred at 6 months post-operatively and 1 occurred within the first 6 wk. Two of these breakages (Patient three and four) occurred along the distal screw threads, whilst in the remaining case (Patient one), screw breakage occurred before the 6 wk post-operatively proximally near the screw head. We postulate that a potential reason for the earlier breakage is due to the longer length of screw used.
Magnesium implants were first described in an orthopaedic setting in 1906 by Lambotte[9] who then utilized a magnesium plate to treat a seventeen-year-old child with pseudoarthrosis and severe malalignment of the distal third of the tibia. Despite that, its popularity never took off due to two key reasons. Firstly, rapid corrosion of magnesium inadvertently resulted in pre-mature implant failure and secondly, contact of the magnesium implant with other metals resulted in a florid electrochemical reaction as Lambotte found out in his index experiment after his patient developed severe pain and extensive subcutaneous gas cavities post operatively due to the aforementioned reaction[9].
The advent of technologically advanced Magnesium Alloys, such as MgYREZr which solved the problem of rapid magnesium degradation, has prompted a re-birth in the utilization and popularity of these implants when the first commercially available Conformité Européenne approved magnesium implant became available in 2013 (MAGNEZIX® compression screw from Syntellix).
During this period of time, the vast majority of clinical studies published were in the setting of forefoot deformity correction surgeries such as chevron osteotomies of the first metatarsal, with only a handful of clinical studies documenting its use in the orthopaedic trauma setting.
In our review of the existing literature, we identified a total of 10 existing studies[10-19] reporting on the utilization of magnesium implants in the setting of orthopaedic trauma. Of these 10 studies, only 1 reported unsatisfactory outcomes[13] and did not recommend the use of magnesium implants, with 1 study still ongoing[15] (Table 2).
| Fracture | Ref. and Journal | Methodology | Results |
| Elbow fractures – Capitellum fracture | Biber et al[10], 2016; Case Reports in Orthopedics | Case report of 73 yr old female with a humerus capitellum fracture | Successful results with complete fracture union and full elbow range of motion |
| Elbow fractures – Distal humerus fractures (Lateral column) | Aktan et al[11], 2018; Cureus | Case report of 50 yr old male with bi-column distal humerus fracture | Successful results with complete fracture union at four months, and elbow range of motion from 5-130 degrees |
| Hand fractures – Scaphoid fractures | Könneker et al[15], 2019 | Multi-centre RCT: 190 patients | Pending |
| Hand fractures – Scaphoid fractures | Meier et al[13], 2016 | Case series of five patients with acute scaphoid fractures treated with a single Magnesium screw | Unsatisfactory results with 3 out of 5 patients experiencing extensive osteolysis and bone cyst; All had good wrist scores and fracture union eventually |
| Hand fractures – Scaphoid fractures | Grieve et al[14], 2017; Hand Surg Rehab | Case series; 3 Scaphoid fractures (Two acute and one revision); 3 Intercarpal fusions | One acute scaphoid fracture lost to follow up; All other cases united except 1 case (partial union at twelve weeks) |
| Hand fractures – Radial styloid fractures | Turan et al[12]; Thieme Medical Publishers | Case series; 2 patients with isolated radial styloid fractures | Good fracture union in both patients with no complications |
| Young displaced neck of femur fractures | Yu et al[16], 2015; BMC, Musculoskeletal disorders | Case series of 19 patients; Mg screws used to fix vascularized iliac bone graft | Successful results with 94.7% union |
| Tibial spine avulsion fractures | Gigante et al[17], 2018; Injury | Case series of three paediatric patients treated surgically with Magnesium screws | Successful results with all three patients obtaining excellent functional recovery |
| Ankle fractures – Isolated lateral malleolus | Acar et al[18], 2018; Cureus | Case report of a 19 yr old female with an isolated Weber A fracture | Successful results with complete fracture union at 8 wk, AOFAS score 100 points at 2 yr |
| Ankle fractures – Medial malleolar fractures | Kose et al[19], 2018; Archives of Orthopaedic and Trauma Surgery | Case series of 11 medial malleolar fractures (Isolated, Bi-malleolar or Tri-malleolar) | Successful results with 100% fracture union, Mean AOFS score of 94.9 at time of final follow up |
In fractures involving the elbow, Biber et al[10] and Aktan et al[11] both reported positive results utilizing magnesium implants intra-articular distal humerus fractures. Biber’s case report documented the utility of the Magnezix CS cannulated compression screw in a patient with a prior radial head replacement who suffered a capitellar fracture and Aktan et al[11] documented their experience utilizing two magnesium compression screws for reduction of the distal humerus articular surface in a patient with a distal humerus fracture. Both patients reported successful results with complete fracture union and functional elbow range of motion at the time of latest follow up.
Although there have been reports of magnesium screws being utilized for fractures of the phalanges mentioned, we were unable to find any case reports or studies in the English literature. Apart from Turan et al[12] case series documenting successful outcomes in two radial styloid fractures, the remaining existing studies in the setting of hand trauma primarily pertain to its utility in scaphoid fractures. This is natural as the Magnezix CS screw is based on a Herbert screw design (variable pitch, headless, cannulated design) which was originally developed for use in compressive osteosynthesis of scaphoid fractures[3].
In Meier et al’s 2016 review, a single magnesium compression screw was used for fixation of various scaphoid fractures[13]. Although all patients eventually exhibited excellent wrist functional outcome scores 1 year post-operatively and all fractures eventually consolidated, he observed significant osteolysis and bone cysts in 3 out of 5 patients which resulted in a significant delay of around six months before sufficient consolidation occurred to allow return to physical work, and hence did not recommend its use in scaphoid fractures. Conversely, Grieve et al[14] documented positive results in his series of 3 scaphoid fractures. At present, a multi-centre, randomized control trial comparing outcomes of scaphoid fractures treated with magnesium and titanium screws by Könneker et al[15] is ongoing (stated to conclude by late 2020) and will hopefully shed more light on the topic.
In fractures involving the lower limb, there is existing literature documenting outcomes when used as an adjunct in young neck of femur fractures[16], tibial spine fractures[17] in paediatric patients, as well as isolated lateral[18] and medial malleolus[19] fractures. All reported positive clinical and radiological outcomes.
Despite the multiple benefits[1-4,20-24] of these magnesium implants (Table 3) and the emergence of these aforementioned studies citing positive outcomes, it is important to also highlight several considerations when opting to utilize these implants.
| Pros | Cons |
| Bioabsorbable and osteoconductive[1,20]; Higher stability than existing polymers[21,22]; Similar stiffness to bone – less stress shielding[4]; Good biocompatibility[1-4]; Minimal artefacts on MRI and CT[23] | Production of hydrogen gas creates peri-implant radiolucencies[3]; Risk of osteolysis[3,24]; Unproven long term track record |
The first important consideration, and arguably the biggest disadvantage of utilizing magnesium implants are the expected production of peri-implant lucencies due to hydrogen gas produced during the process of magnesium degradation. Clinicians may find it difficult to differentiate this from post-operative complications such as infection or loosening of implants. Although studies have demonstrated that these radiolucencies do gradually disappear from anywhere between 3 to 17 months[3], the presence of persistent radiolucencies (which appear as early as 2 wk post-operatively as seen in our series), may cause anxiety to both the clinician and the patient.
Secondly, magnesium implants are also known to be associated with osteolysis[24], which was postulated to occur when the body is unable to adequately clear the products of magnesium degeneration from the implantation site, leading to the migration of osteoclasts to the implantation site. This, coupled with the aforementioned issue of expected post-operative radiolucencies is particularly concerning given the fact that symptoms of osteolysis do not usually occur[25] until there is sufficient bone loss to result in aseptic loosening of the implant, by which point implant failure is likely to occur.
Our review of the literature identified 3 studies[5,26,27] comparing outcomes in magnesium and conventional implants. May et al’s study recruited a total of 48 patients with medial malleolus fractures undergoing compression screw fixation of which 23 had magnesium screws implanted whilst 25 had conventional screws implanted[26]. In his study, with a minimum follow up of 1 year, no differences in clinical outcomes between both groups were noted, with similar AOFAS clinical outcome scores, and a 100% union rate in both groups. Complication rates were also similar with no deep infection or osteomyelitis noted in both groups. However, 5 patients with conventional titanium implants, compared to none in the magnesium screw group required removal of implants for symptomatic hardware, highlighting the key benefit of using magnesium implants.
The remaining two studies recruited patients undergoing distal metatarsal osteotomies for hallux valgus. Acar et al[5] retrospectively compared two groups of 17 patients undergoing surgery with both implants, whilst Plaass et al[27] conducted a randomized control trial of 26 patients. Both studies reported similar therapeutic outcomes with regards to functional and radiographical outcomes, with no differences in complication rates or union rates.
Although the literature appears to suggest that these bioabsorbable magnesium screws provide similar efficacy to conventional implants, interpreting the data must performed with caution at this juncture due to the small collective number of patients analysed, and the heterogeneity of clinical indications amongst studies. In our search of the literature, there were no comparative studies analyzing the efficacy of both implants when used in peri-articular fractures around the elbow, with only two case reports[10-11] available in the literature, similarly documenting successful outcomes as reported in our series.
Limitations of our study include a relatively small sample size although our case series represents one of the largest case series documenting the outcomes of magnesium screws in upper limb fractures. Furthermore, as there are few other studies on the topic, comparing and analysing our outcomes is challenging. Further studies are needed to evaluate the topic further such as a study with a control group.
Our case series serves to add to the paucity of literature on the utilization of magnesium screws in upper limb fractures. In our series, all patients exhibited good short to medium term clinical outcomes with no complications or revision surgeries required, and significantly none of our patients developed any clinical signs or symptoms of synovitis or allergic reactions. Although further larger studies with longer follow-ups are required before the implant can be unequivocally proven superior or equal to conventional existing implants, these implants appear to be a promising innovation for the modern orthopaedic surgeon.
Larger trials such as randomized control trials with larger patient numbers should be conducted.
Bio-absorbable magnesium screws can be used in peri-articular fractures of the elbow.
All fractures healed successfully and no patient required removal of implants or suffered any major complications.
Our paper was based on a retrospective case series design. Intra-operatively, a standardized surgical technique was utilized for insertion of the magnesium implants. Post – operatively, clinic visits were standardized and physical exam findings, functional scores, and radiographs were obtained at each visit. All complications were recorded.
Our findings will help clinicians in two main areas. Firstly, clinicians considering using the implant for their patients have a detailed case series to refer to. Secondly, clinicians considering research on the topic have a large sample size (relative to the existing literature) to aid in conducting future studies especially systematic reviews or meta–analysis.
To ascertain if bio-asborbable magnesium screws are clinically efficaceous in treating peri-articular elbow fractures.
Magnesium screws are gaining popularity in orthopaedic trauma surgery. No case series has been published documenting its use in peri-articular fractures of the elbow.
| 1. | Waizy H, Diekmann J, Weizbauer A, Reifenrath J, Bartsch I, Neubert V, Schavan R, Windhagen H. In vivo study of a biodegradable orthopedic screw (MgYREZr-alloy) in a rabbit model for up to 12 months. J Biomater Appl. 2014;28:667-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 104] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 2. | Zhang E, Xu L, Yu G, Pan F, Yang K. In vivo evaluation of biodegradable magnesium alloy bone implant in the first 6 months implantation. J Biomed Mater Res A. 2009;90:882-893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 150] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 3. | Kose O. Magnesium (MgYREZr) bioabsorbable screws in orthopedic surgery, A narrative review, Military medicine worldwide, 2019. Available from: https://aleamed.eu/wp-content/uploads/2019/11/Köse_2019_Military_Medicine_Review.pdf. |
| 4. | Chakraborty Banerjee P, Al-Saadi S, Choudhary L, Harandi SE, Singh R. Magnesium Implants: Prospects and Challenges. Materials (Basel). 2019;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 81] [Cited by in RCA: 104] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 5. | Acar B, Kose O, Turan A, Unal M, Kati YA, Guler F. Comparison of Bioabsorbable Magnesium versus Titanium Screw Fixation for Modified Distal Chevron Osteotomy in Hallux Valgus. Biomed Res Int. 2018;2018:5242806. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 47] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 6. | Atkinson HD, Khan S, Lashgari Y, Ziegler A. Hallux valgus correction utilising a modified short scarf osteotomy with a magnesium biodegradable or titanium compression screws - a comparative study of clinical outcomes. BMC Musculoskelet Disord. 2019;20:334. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 7. | Choo JT, Lai SHS, Tang CQY, Thevendran G. Magnesium-based bioabsorbable screw fixation for hallux valgus surgery - A suitable alternative to metallic implants. Foot Ankle Surg. 2019;25:727-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 8. | Nabiyouni M, Brückner T, Zhou H, Gbureck U, Bhaduri SB. Magnesium-based bioceramics in orthopedic applications. Acta Biomater. 2018;66:23-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 182] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 9. | Witte F. The history of biodegradable magnesium implants: a review. Acta Biomater. 2010;6:1680-1692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1267] [Cited by in RCA: 654] [Article Influence: 40.9] [Reference Citation Analysis (0)] |
| 10. | Biber R, Pauser J, Geßlein M, Bail HJ. Magnesium-Based Absorbable Metal Screws for Intra-Articular Fracture Fixation. Case Rep Orthop. 2016;2016:9673174. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 11. | Aktan C, Ertan MB, Turan A, Kose O. Fixation of Small Osteochondral Fragments in a Comminuted Distal Humerus Fracture with Magnesium Bioabsorbable Screws: A Case Report. Cureus. 2018;10:e3752. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Turan A, Kati YA, Acar B, Kose O. Magnesium Bioabsorbable Screw Fixation of Radial Styloid Fractures: Case Report. J Wrist Surg. 2020;9:150-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Meier R, Panzica M. First results with a resorbable MgYREZr compression screw in unstable scaphoid fractures show extensive bone cysts. Handchir Mikrochir Plast Chir. 2017;49:37-41. [RCA] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 14. | Grieve P, O'Carroll S, Albastaki O. Six cas de série de patients de Magnezix®. Une vis métallique absorbable pour la fixation de la fracture du carpe et des fusions entre les carpes. Hand Surg Rehab. 2017;36:488-489. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Könneker S, Krockenberger K, Pieh C, von Falck C, Brandewiede B, Vogt PM, Kirschner MH, Ziegler A. Comparison of SCAphoid fracture osteosynthesis by MAGnesium-based headless Herbert screws with titanium Herbert screws: protocol for the randomized controlled SCAMAG clinical trial. BMC Musculoskelet Disord. 2019;20:357. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 16. | Yu X, Zhao D, Huang S, Wang B, Zhang X, Wang W, Wei X. Biodegradable magnesium screws and vascularized iliac grafting for displaced femoral neck fracture in young adults. BMC Musculoskelet Disord. 2015;16:329. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 17. | Gigante A, Setaro N, Rotini M, Finzi SS, Marinelli M. Intercondylar eminence fracture treated by resorbable magnesium screws osteosynthesis: A case series. Injury. 2018;49 Suppl 3:S48-S53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 18. | Acar B, Unal M, Turan A, Kose O. Isolated Lateral Malleolar Fracture Treated with a Bioabsorbable Magnesium Compression Screw. Cureus. 2018;10:e2539. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 19. | Kose O, Turan A, Unal M, Acar B, Guler F. Fixation of medial malleolar fractures with magnesium bioabsorbable headless compression screws: short-term clinical and radiological outcomes in eleven patients. Arch Orthop Trauma Surg. 2018;138:1069-1075. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 48] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 20. | Liu C, Ren Z, Xu Y, Pang S, Zhao X, Zhao Y. Biodegradable Magnesium Alloys Developed as Bone Repair Materials: A Review. Scanning. 2018;2018:9216314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 96] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 21. | Losertova M, Stamborska M. Comparison of deformation behaviour of 316L stainless steel and Ti6AI4V alloy applied in traumatology. METABK. 2016;55:667-670; ISSN 0543. |
| 22. | Sidambe AT. Biocompatibility of Advanced Manufactured Titanium Implants-A Review. Materials (Basel). 2014;7:8168-8188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 467] [Cited by in RCA: 277] [Article Influence: 23.1] [Reference Citation Analysis (0)] |
| 23. | Sonnow L, Könneker S, Vogt PM, Wacker F, von Falck C. Biodegradable magnesium Herbert screw - image quality and artifacts with radiography, CT and MRI. BMC Med Imaging. 2017;17:16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 24. | Maradze D, Musson D, Zheng Y, Cornish J, Lewis M, Liu Y. High Magnesium Corrosion Rate has an Effect on Osteoclast and Mesenchymal Stem Cell Role During Bone Remodelling. Sci Rep. 2018;8:10003. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 25. | Saleh KJ, Thongtrangan I, Schwarz EM. Osteolysis: medical and surgical approaches. Clin Orthop Relat Res. 2004;138-147. [PubMed] |
| 26. | May H, Alper Kati Y, Gumussuyu G, Yunus Emre T, Unal M, Kose O. Bioabsorbable magnesium screw versus conventional titanium screw fixation for medial malleolar fractures. J Orthop Traumatol. 2020;21:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 58] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 27. | Plaass C, von Falck C, Ettinger S, Sonnow L, Calderone F, Weizbauer A, Reifenrath J, Claassen L, Waizy H, Daniilidis K, Stukenborg-Colsman C, Windhagen H. Bioabsorbable magnesium versus standard titanium compression screws for fixation of distal metatarsal osteotomies - 3 year results of a randomized clinical trial. J Orthop Sci. 2018;23:321-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 88] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Singapore
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Primadhi RA, Indonesia S-Editor: Liu JH L-Editor: A P-Editor: Li X