Published online Dec 18, 2024. doi: 10.5312/wjo.v15.i12.1191
Revised: September 27, 2024
Accepted: October 21, 2024
Published online: December 18, 2024
Processing time: 121 Days and 17.6 Hours
Achilles tendon rupture is a common orthopedic injury, with an annual incidence of 11-37 per 100000 people, significantly impacting daily life. Minimally invasive surgery, increasingly favored for its reduced risks and comparable fixation strength to open surgery, addresses these challenges. Despite advantages like ac
To evaluate a nursing-led rapid rehabilitation program for minimally invasive Achilles tendon repair surgery, providing evidence-based early recovery in
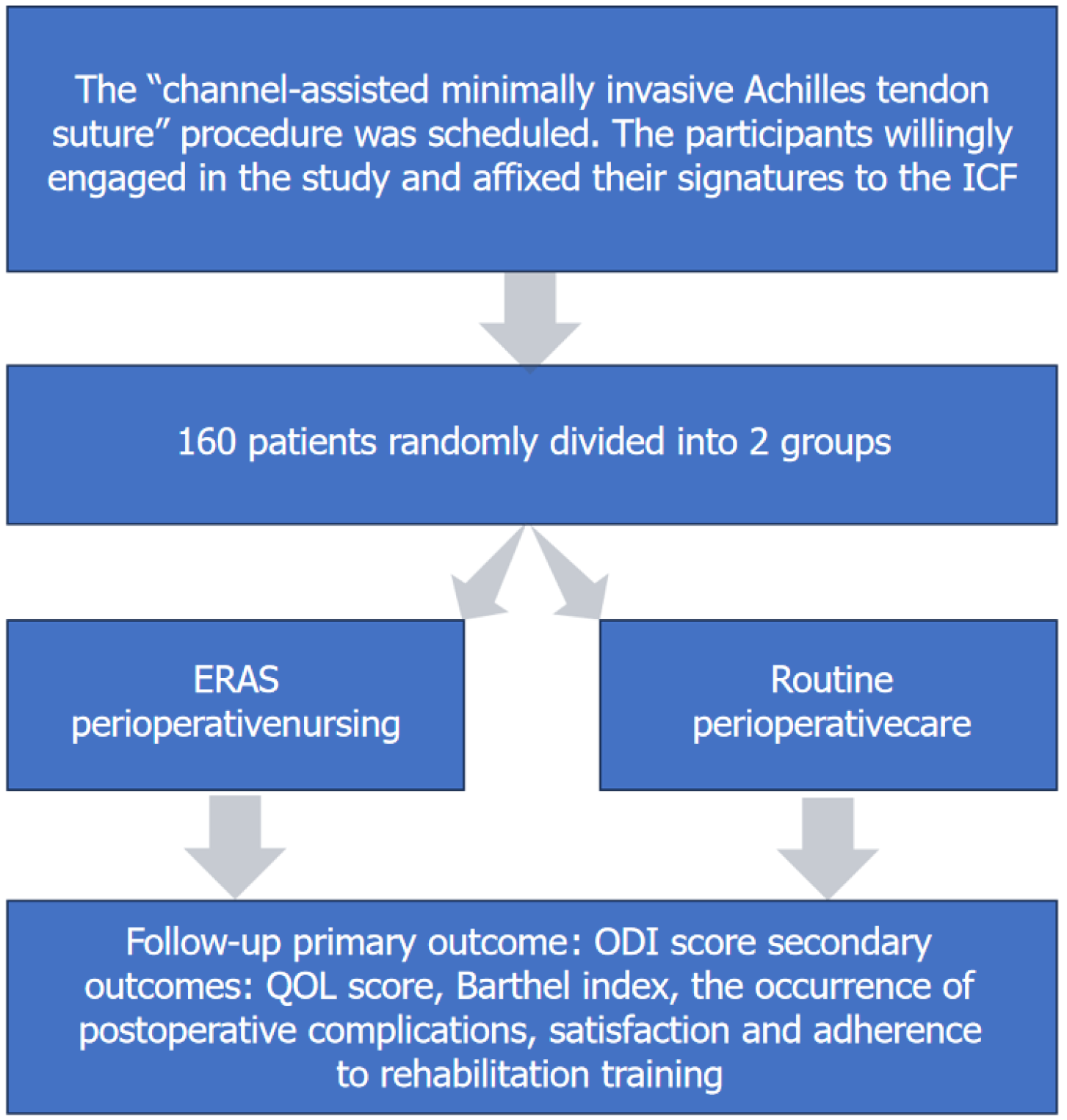
This study enrolled 160 patients undergoing channel-assisted minimally invasive Achilles tendon repair randomized into experimental and control groups. The experimental group received perioperative rapid rehabilitation nursing care, while the control group received standard care. The primary outcome measure was the Oswestry disability index score, with secondary outcomes including quality of life, Barthel index, patient satisfaction with nursing, incidence of co
All 160 patients completed the follow-up. The experimental group showed significantly greater improvements in key efficacy indicators: Postoperative Oswestry disability index score (8.688 vs 18.88, P < 0.0001), quality of life score (53.25 vs 38.99, P < 0.0001), and Barthel index (70.44 vs 51.63, P < 0.0001). The experimental group had a lower incidence of deep vein thrombosis (1.25% vs 10.00%, P = 0.0339) with a relative risk of 0.1250 (95% confidence interval: 0.02050-0.7421). Infection rates were lower in the experimental group (2.50% vs 11.25%, P = 0.0564). Hospital stay (5.40 days vs 7.26 days, P < 0.0001) and postoperative bed rest (3.34 days vs 5.42 days, P < 0.0001) were significantly shorter. Patient satisfaction was 100% in the experimental group vs 87.50% in the control group
The rapid rehabilitation intervention significantly reduced pain, shortened hospital stays, and lowered com
Core Tip: This study highlighted the substantial benefits of implementing a nursing-led rapid rehabilitation program for patients undergoing minimally invasive Achilles tendon repair. By integrating rapid rehabilitation strategies, patients experienced faster recovery, reduced pain, shorter hospital stays, and lower complication rates. The program not only improved functional outcomes and quality of life but also enhanced patient satisfaction and adherence to rehabilitation protocols. This approach provides valuable evidence supporting its adoption as a standard practice for optimizing postoperative care and recovery.
- Citation: Yan XJ, Zhang WH. Enhanced recovery after surgery protocols for minimally invasive treatment of Achilles tendon rupture: Prospective single-center randomized study. World J Orthop 2024; 15(12): 1191-1199
- URL: https://www.wjgnet.com/2218-5836/full/v15/i12/1191.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i12.1191
Achilles tendon rupture is a common and severe orthopedic injury, with an annual incidence rate of 11-37 per 100000 people[1-3], which has a significant impact on patients’ daily lives[4]. Currently, surgery is the primary treatment for Achilles tendon rupture, and minimally invasive surgery is increasingly favored by researchers due to its ability to significantly reduce surgical risks while providing fixation strength comparable to open surgery[5-7]. According to numerous studies, the re-rupture rate after Achilles tendon repair surgery is approximately 3.1%-3.5%[8].
However, despite the many advantages of minimally invasive surgery in treating Achilles tendon rupture, such as reduced trauma and accelerated recovery, there are still significant challenges in perioperative care[9]. Although the importance of emotional support and pain management is increasingly recognized, individualized and continuous care is often difficult to implement in practice[10,11]. This can result in unnecessary anxiety and pain for patients before and after surgery, affecting their compliance.
Moreover, specific strategies for early rehabilitation remain controversial. It is challenging to scientifically and effectively carry out ankle joint function exercises and gradual weight-bearing training while ensuring safety, which is a key step in the patient’s recovery process[12-14]. The lack of personalized treatment plans is also a significant issue, as it overlooks the substantial differences between patients in terms of age, physical condition, and extent of injury, thereby limiting the optimization of rehabilitation outcomes. In summary, these issues in perioperative care for minimally invasive Achilles tendon surgery affect both treatment efficacy and the patient’s rehabilitation experience.
There is a greater demand for the understandability and coherence of rehabilitation care guidelines for patients undergoing minimally invasive Achilles tendon surgery. Although the benefits of rapid rehabilitation care have been widely reported, it is still not broadly implemented in most rehabilitation care plans domestically and internationally[15]. Therefore, there is a need to develop personalized and standardized rapid rehabilitation care protocols[16]. This study was a single-center, randomized, double-blind, parallel-controlled clinical trial investigating the efficacy of a rapid rehabilitation surgical care protocol in patients undergoing minimally invasive Achilles tendon surgery with channel-assisted follow-up.
From January 2023 to December 2023, 160 patients undergoing “channel-assisted minimally invasive Achilles tendon suturing” at the Third Medical Center of the People’s Liberation Army General Hospital were selected as research subjects and randomly divided into a control group and an intervention group using a random number table, with 80 cases in each group. Inclusion criteria were: Patients with a history of Achilles tendon rupture not exceeding 3 weeks before surgery; preoperative risk factor assessments such as American Society of Anesthesiologists Physical Status Classification System score, nutritional assessment, and body mass index; and patients willing to participate in the study and sign an informed consent form. Exclusion criteria included: Calcaneal tuberosity avulsion fractures; autoimmune diseases; rheumatoid arthritis; diabetes; patients with a heavy drinking and smoking history; and those with open Achilles tendon ruptures[7]. After obtaining approval from the hospital Institutional Review Board and securing signed informed consent from the patients, the study was officially initiated. Comparison of general data between the two groups showed no statistically significant differences, indicating rigorous study design and good balance between groups.
Using the Oswestry disability index (ODI) as the primary endpoint, the sample size for each group was calculated using the formula:
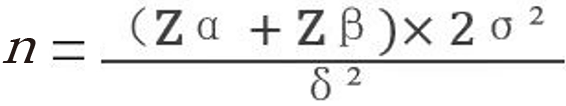
And a sample size ratio of 1:1. Referencing clinical data from the department for ODI, the calculation yielded 71 cases per group. Considering the loss to follow-up rate and the practical situation of the hospital, the final sample size was determined to be 80 cases per group.
To ensure the effectiveness of the study, the following measures were strictly implemented to adhere to the blinding principles: (1) Spatial isolation: Participants receiving different nursing interventions were placed in separate wards to prevent cross-information transmission; (2) Confidentiality mechanism: Except for the directly involved nursing staff, investigators and other relevant personnel were not informed about the details of participants’ nursing assignments; (3) Role division and information barriers: Throughout the trial process, the roles of outcome assessors and intervention implementers were strictly separated. The former were unaware of the participants’ group assignments, while the latter did not participate in the outcome measurement process[8]; (4) Result sealing and awareness limitation: During the trial period, all investigators, staff, and participants were prohibited from accessing any information about measurement results or the trial process; and (5) Interaction restriction: Participants were strictly prohibited from discussing the nursing interventions they received to prevent cross-influence.
Patients included in the study completed baseline assessments 1 week prior to enrollment and involved ODI scores, quality of life (QOL) scores, and other QOL indicators as well as demographic parameters. On the 7th postoperative day, the same indicators were re-evaluated, and data on postoperative bed rest duration, hospital stay length, adverse event rates, satisfaction, and compliance were recorded.
These included detailed dietary guidance, scientific rehabilitation training, comprehensive health education, personalized psychological counseling, and proactive prevention and intervention of complications. In terms of pain management, the analgesic regimen was adjusted in real time based on the patient’s specific condition and individual responses[10]. For rehabilitation training, a series of quantifiable and adjustable intensity rehabilitation programs were designed, such as the use of continuous passive motion devices and rehabilitation robots. Regarding psychological support, interventions such as cognitive behavioral therapy and the establishment of support networks were imp
One day before surgery, the responsible nurse introduced the relevant requirements of perioperative fast-track care to the patient. Multimedia formats, such as short videos and PowerPoint presentations, were used to provide perioperative education to the patient, covering aspects such as preoperative and postoperative dietary arrangements, early functional exercises, time to get out of bed, and methods to relieve pain. On the day of surgery, a personalized diet plan and a preventive analgesic strategy was formulated by referring to the consensus guidelines of fast-track surgery experts[16] and the recommendations of the American Society of Anesthesiologists[17] and taking into account the patient’s con
Regarding the scientific use of Achilles tendon boots and weight-bearing training guidance, it was crucial to emphasize the importance of proper brace usage so that patients and their families could more scientifically engage in medical and rehabilitation care. The decision to use an Achilles tendon boot should be made by a senior orthopedic surgeon. If the boot was used: Postoperative weeks 0-1: The ankle should be strictly fixed in a plantar flexion position of 20°-30°. Postoperative weeks 2-3: The boot should fix the ankle at 30° of plantar flexion. The appropriate weight-bearing levels should be determined based on the patient’s individual differences and tolerance. Postoperative weeks 4-5: The ankle should be fixed at 20° of plantar flexion. At this stage, it was emphasized that the patient should perform active plantar flexion and dorsiflexion exercises while maintaining the ankle in the plantar flexion position. Postoperative weeks 6-7: Free plantar flexion activity within a 0°-30° range is allowed. After 6 weeks, the range of motion for the ankle should be gradually increased to a neutral position, and Achilles tendon massage should be given daily during this period. Postoperative weeks 8-12: The Achilles tendon boot should be gradually removed, and exercises to strengthen the calf muscles should be initiated. Postoperative weeks 13-16: Begin slow jogging with the full foot in contact with the ground, gradually increasing the exercise volume and incorporating small-scale training. For individuals engaged in moderate physical labor, they can gradually return to work. Postoperative weeks 17-20: If no significant discomfort is experienced, athletes can start participating in formal training programs.
Baseline data: Basic characteristic data, including age, sex, and other indicators, were collected within 7 days prior to patient enrollment.
Primary outcome indicators: The ODI score is used to comprehensively assess the patient’s functional recovery level. Measurements were taken once before treatment and again before discharge.
Secondary outcome indicators: The QOL score and Barthel index, along with the occurrence of postoperative complications, including but not limited to infections, deep vein thrombosis, and poor wound healing, were reported. Additionally, patient satisfaction and adherence to rehabilitation training were evaluated. These indicators help assess the practical value and effectiveness of rapid recovery care interventions in the rehabilitation process of patients undergoing minimally invasive Achilles tendon repair.
We used the Statistical Package for the Social Sciences (SPSS, version 24.0; IBM Corp., Armonk, NY, United States) for data analysis. For measurement data that followed a normal distribution, we expressed the data as mean ± standard deviation. For measurement data that did not follow a normal distribution, we described the data using the median and interquartile range. Categorical data were presented as n (%), where n represents the number of observations and% indicates the proportion relative to the total sample size. The Shapiro-Wilk test was used to assess the normality of the data distribution. Continuous variables between groups were compared using t-tests or analysis of variance, and categorical variables were compared using the χ² test. A P value of less than 0.05 was considered statistically significant (Figure 1).
In the design and implementation of this randomized controlled clinical trial, we placed a high priority on ensuring that the experimental group and the control group were well-matched in baseline characteristics to minimize the impact of potential confounding variables on subsequent efficacy and safety evaluations. Baseline data for all participants included in the study were systematically and comprehensively collected and organized before they were assigned to each group and received the corresponding interventions, thereby ensuring the reliability of the data with respect to its prospective nature and reference benchmark. Detailed baseline characteristic data are provided in Table 1.
| Parameter | Experimental group | Control group | χ2/t | P value |
| Sex | 0.63 | 0.43 | ||
| Male | 38 | 33 | - | - |
| Female | 42 | 47 | - | - |
| Age | 37.46 | 36.00 | 0.29 | 0.75 |
| BMI | 23.76 | 23.44 | 0.74 | 0.46 |
| Before surgery ODI | 30.31 | 30.69 | 0.11 | 0.90 |
| Before surgery QOL | 18.16 | 18.83 | 0.34 | 0.74 |
| Before surgery Barthel | 30.75 | 31.13 | 0.16 | 0.91 |
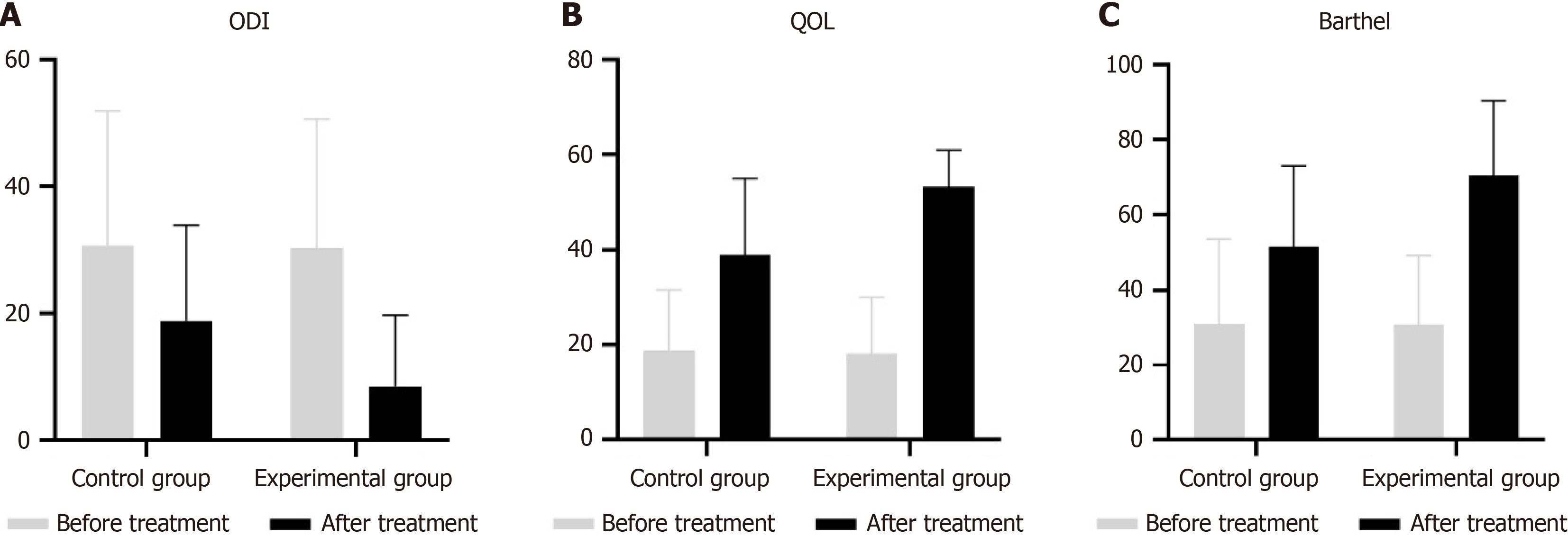
Compared to the conventional care group, we found that the experimental group showed significant improvements in ODI scores, QOL scores, and Barthel index after implementing the accelerated rehabilitation external care plan.
The ODI scores revealed that both groups had similar preoperative values, with the control group at 30.69 [95% confidence interval (CI): 25.95-35.43] and the experimental group at 30.31 (95%CI: 25.78-34.85). However, a significant postoperative improvement was observed in the experimental group, whose ODI score dropped to 8.688 (95%CI: 6.249-11.13) compared to a decrease of 18.88 (95%CI: 15.51-22.24) in the control group.
In terms of QOL, preoperative scores were also comparable, with the control group scoring 18.83 (95%CI: 15.96-21.69) and the experimental group 18.16 (95%CI: 15.51-20.82). After surgery, the QOL of the control group improved to 38.99 (95%CI: 35.42-42.55), whereas the experimental group saw a more pronounced increase to 53.25 (95%CI: 51.53-54.97), underscoring the benefits of the Enhanced Recovery After Surgery (ERAS) care plan.
Barthel index scores followed a similar pattern, showing no significant difference preoperatively: 31.13 (95%CI: 26.16-36.09) for the control group vs 30.75 (95%CI: 26.63-34.87) for the experimental group. Postoperatively, the score of control group increased to 51.63 (95%CI: 46.86-56.39), while the experimental group achieved a noteworthy score of 70.44 (95%CI: 65.99-74.89), highlighting their improved capacity for daily activities (Figure 2).
In the comparative analysis, the experimental group demonstrated significant postoperative recovery advantages over the control group. Specifically, the experimental group had an average postoperative bed rest duration of only 3.34 days, which was notably shorter than the 5.42 days for the control group. Additionally, their hospital stay was significantly reduced to 5.40 days, well below the 7.26 days of the control group. These results indicate that patients in the experimental group were able to recover more quickly from the surgical effects and reduce the hospital burden.
More notably, in terms of complications control, the incidence of deep vein thrombosis in the experimental group was only 1 case (0.01%), and the infection rate was 2 cases (0.02%). In contrast, the control group had an incidence of deep vein thrombosis in 8 cases (10.00%) and infections in 9 cases (11.25%). These data strongly demonstrated that the accelerated recovery care measures are significantly more effective than traditional care plans in preventing postoperative complications, particularly deep vein thrombosis and infections, thereby greatly enhancing patient recovery quality and safety (Table 2).
| Group | Number of cases | Postoperative bed rest duration | Length of hospital stay | Deep vein thrombosis | Infection |
| Control group | 80 | 5.42 ± 2.46 | 7.26 ± 2.70 | 8 (10.00) | 9 (11.25) |
| Experimental group | 80 | 3.34 ± 1.77 | 5.40 ± 2.76 | 1 (0.01) | 2 (0.02) |
| χ² | - | 4.339 | 3.440 | 5.769 | 4.783 |
| P value | - | 0.009 | 0.000 | 0.001 | 0.001 |
In evaluating patient satisfaction and compliance, the experimental group achieved significantly better results compared to the control group. Regarding satisfaction, 53 patients (66.25%) in the experimental group reported being satisfied, far exceeding the 11 patients (13.75%) in the control group. Additionally, none of the patients in the experimental group reported poor satisfaction, whereas 20 patients (25.00%) in the control group expressed lower satisfaction levels. In terms of compliance, the experimental group also showed superior performance, with 79 patients (98.75%) meeting the standard for excellent compliance, including 59 patients (73.75%) rated as excellent. In contrast, only 20 patients (25.00%) in the control group had good compliance, with an excellent rate of just 65.00%. The experimental group had only 1 case (1.25%) of poor compliance, while the control group had a significantly higher rate of 35.00%. These data clearly demonstrated that our accelerated recovery care program not only greatly improved patient satisfaction but also significantly optimized adherence to treatment plans, further validating the effectiveness of this strategy in enhancing patient satisfaction and ensuring treatment outcomes (Table 3 and Table 4).
| Group | Number of cases | Satisfied | Better | General | Inferior | Overall satisfaction |
| Control group | 80 | 11 (13.75) | 38 (47.50) | 11 (13.75) | 20 (25.00) | 60 (87.50) |
| Experimental group | 80 | 53 (66.25) | 20 (25.00) | 7 (8.75) | 0 (0.00) | 80 (100.00) |
| χ² | - | - | - | - | - | 7.786 |
| P value | - | - | - | - | - | 0.005 |
| Group | Number of cases | Good compliance | Moderate compliance | Poor adherence | Compliance rate |
| Control group | 80 | 20 (25.00) | 32 (40.00) | 28 (35.00) | 52 (65.00) |
| Experimental group | 80 | 59 (73.75) | 20 (25.00) | 1 (1.25) | 79 (98.75) |
| χ² | - | - | - | - | 6.44 |
| P value | - | - | - | - | 0.015 |
The findings from this study demonstrated that the fast-track surgical care model applied to minimally invasive Achilles tendon rupture surgeries yielded superior patient outcomes compared to traditional care methods. Patients who received fast-track care showed significant improvements in functional recovery, as evidenced by higher Barthel index scores, lower ODI scores, and enhanced QOL post-surgery. Additionally, these patients exhibited better adherence to rehabilitation exercises and greater satisfaction with nursing services. Quantitative indicators such as shorter postoperative bed rest duration, reduced hospital stays, and a lower incidence of complications like deep vein thrombosis and infections further underscored the effectiveness of the fast-track care approach.
These findings aligned with previous studies that highlight the benefits of fast-track surgery in promoting faster recovery, reducing complications, and shortening hospital stays for various surgical procedures[17,18]. Similar results have been observed in fast-track programs for orthopedic surgeries, where early mobilization, personalized rehabilitation, and efficient pain management contribute to improved outcomes[19,20]. For example, studies on fast-track protocols for knee and hip replacements have shown analogous benefits in terms of reduced hospital stays and enhanced recovery, underscoring the generalizability of the fast-track model across surgical domains[21]. However, the present study is unique in its focus on Achilles tendon rupture, an area that has not been extensively explored in the context of fast-track care. Existing literature on Achilles tendon repair emphasizes the importance of early rehabilitation and individualized care, both of which are key components of the fast-track protocol used in this study[22]. By integrating early mobilization strategies with personalized care, our results contributed to the growing evidence supporting fast-track protocols as an effective approach for orthopedic conditions. It is crucial to delve into the challenges and future directions of ERAS[16].
Despite these positive outcomes, this study had several limitations. First, the time points for data collection were limited to the admission and discharge phases, potentially overlooking important intermediate progressions in patient recovery. This lack of continuous monitoring restricts a deeper understanding of the dynamic changes in patient recovery throughout the treatment process. Future studies should incorporate more frequent data collection to capture trends and fluctuations during the perioperative period. Second, although efforts were made to control potential biases, residual biases related to sample selection, data collection, and analysis could have influenced the results. Non-random errors may have affected the internal validity of the study. Third, although our study further confirmed that ERAS can shorten hospital stays, the reasons why patients stay longer were ignored. Fourth, the complexity of the ERAS protocol may lead to “partial ERAS” instead of full implementation. Further studies are necessary to further subdivide the effectiveness of each component in ERAS. Finally, the statistical methods employed were relatively basic, limiting the exploration of more complex relationships between variables. The use of advanced techniques such as multivariate regression or machine learning algorithms could provide greater insight into the intricate factors influencing recovery outcomes[23-25].
The findings from this study have several important implications for clinical practice, health policy, and future research. In terms of practice, the fast-track care model presents an effective and patient-centered approach that can be integrated into existing perioperative care strategies[26-28], particularly for minimally invasive orthopedic surgeries. This model promotes early rehabilitation, personalized care plans, and proactive pain management, all of which contribute to faster recovery and higher patient satisfaction. From a policy perspective, adopting fast-track protocols can help optimize healthcare resources by reducing hospital stays and lowering the incidence of postoperative complications[17,23,29], ultimately leading to cost savings and improved patient throughput.
Future research should focus on refining ERAS protocols through personalized interventions, leveraging advanced statistical models to tailor care strategies to individual patient profiles[30]. Large-scale randomized controlled trials are crucial for validation of the universal applicability of recommended elements and for ensuring consistent implementation effectiveness[31,32]. Detailed observational studies complement RCTs by exploring specific impacts of preoperative, intraoperative, and postoperative elements on recovery outcomes, providing nuanced data for optimizing ERAS pathways across diverse clinical contexts.
The fast-track surgical care model offers significant advantages for patients undergoing minimally invasive Achilles tendon rupture repair. By addressing the current challenges in perioperative care, such as the need for personalized rehabilitation plans and efficient pain management, this model has the potential to improve both clinical outcomes and patient satisfaction. Further research is needed to refine these protocols and expand their application across different surgical procedures and patient populations.
| 1. | Aurich M, Becherer L, Rammelt S. [Surgical or non-operative treatment of acute Achilles tendon rupture : What does the current literature say?]. Orthopadie (Heidelb). 2024;53:740-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Ivanova VS, Sieu Tong KP, Neagu C, King CM. Current Concepts in Achilles Tendon Ruptures. Clin Podiatr Med Surg. 2024;41:153-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 3. | Järvinen TA, Kannus P, Maffulli N, Khan KM. Achilles tendon disorders: etiology and epidemiology. Foot Ankle Clin. 2005;10:255-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 345] [Cited by in RCA: 369] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 4. | Sheth U, Wasserstein D, Jenkinson R, Moineddin R, Kreder H, Jaglal SB. The epidemiology and trends in management of acute Achilles tendon ruptures in Ontario, Canada: a population-based study of 27 607 patients. Bone Joint J. 2017;99-B:78-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 105] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 5. | Seow D, Islam W, Randall GW, Azam MT, Duenes ML, Hui J, Pearce CJ, Kennedy JG. Lower re-rupture rates but higher complication rates following surgical versus conservative treatment of acute achilles tendon ruptures: a systematic review of overlapping meta-analyses. Knee Surg Sports Traumatol Arthrosc. 2023;31:3528-3540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 6. | Westin O, Nilsson Helander K, Grävare Silbernagel K, Samuelsson K, Brorsson A, Karlsson J. Patients with an Achilles tendon re-rupture have long-term functional deficits and worse patient-reported outcome than primary ruptures. Knee Surg Sports Traumatol Arthrosc. 2018;26:3063-3072. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 7. | Wu Y, Lin L, Li H, Zhao Y, Liu L, Jia Z, Wang D, He Q, Ruan D. Is surgical intervention more effective than non-surgical treatment for acute Achilles tendon rupture? A systematic review of overlapping meta-analyses. Int J Surg. 2016;36:305-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 8. | Wang R, Huang L, Jiang S, You G, Zhou X, Wang G, Zhang L. Immediate mobilization after repair of Achilles tendon rupture may increase the incidence of re-rupture: a systematic review and meta-analysis of randomized controlled trials. Int J Surg. 2024;110:3888-3899. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Braunstein M, Baumbach SF, Boecker W, Carmont MR, Polzer H. Development of an accelerated functional rehabilitation protocol following minimal invasive Achilles tendon repair. Knee Surg Sports Traumatol Arthrosc. 2018;26:846-853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 10. | Bushnell MC, Ceko M, Low LA. Cognitive and emotional control of pain and its disruption in chronic pain. Nat Rev Neurosci. 2013;14:502-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1012] [Cited by in RCA: 1439] [Article Influence: 110.7] [Reference Citation Analysis (0)] |
| 11. | Fitzcharles MA, Cohen SP, Clauw DJ, Littlejohn G, Usui C, Häuser W. Nociplastic pain: towards an understanding of prevalent pain conditions. Lancet. 2021;397:2098-2110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 229] [Cited by in RCA: 710] [Article Influence: 142.0] [Reference Citation Analysis (0)] |
| 12. | Barfod KW, Nielsen F, Helander KN, Mattila VM, Tingby O, Boesen A, Troelsen A. Treatment of acute Achilles tendon rupture in Scandinavia does not adhere to evidence-based guidelines: a cross-sectional questionnaire-based study of 138 departments. J Foot Ankle Surg. 2013;52:629-633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 13. | Kearney RS, Parsons N, Underwood M, Costa ML. Achilles tendon rupture rehabilitation: a mixed methods investigation of current practice among orthopaedic surgeons in the United Kingdom. Bone Joint Res. 2015;4:65-69. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Suchak AA, Bostick GP, Beaupré LA, Durand DC, Jomha NM. The influence of early weight-bearing compared with non-weight-bearing after surgical repair of the Achilles tendon. J Bone Joint Surg Am. 2008;90:1876-1883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 146] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 15. | Ljungqvist O, Scott M, Fearon KC. Enhanced Recovery After Surgery: A Review. JAMA Surg. 2017;152:292-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1487] [Cited by in RCA: 2422] [Article Influence: 269.1] [Reference Citation Analysis (0)] |
| 16. | Lobo DN, Joshi GP, Kehlet H. Challenges in Enhanced Recovery After Surgery (ERAS) research. Br J Anaesth. 2024;133:717-721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 17] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 17. | Ljungqvist O, de Boer HD, Balfour A, Fawcett WJ, Lobo DN, Nelson G, Scott MJ, Wainwright TW, Demartines N. Opportunities and Challenges for the Next Phase of Enhanced Recovery After Surgery: A Review. JAMA Surg. 2021;156:775-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 202] [Article Influence: 40.4] [Reference Citation Analysis (0)] |
| 18. | Gillis C, Ljungqvist O, Carli F. Prehabilitation, enhanced recovery after surgery, or both? A narrative review. Br J Anaesth. 2022;128:434-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 171] [Article Influence: 42.8] [Reference Citation Analysis (0)] |
| 19. | Soffin EM, YaDeau JT. Enhanced recovery after surgery for primary hip and knee arthroplasty: a review of the evidence. Br J Anaesth. 2016;117:iii62-iii72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 221] [Article Influence: 27.6] [Reference Citation Analysis (0)] |
| 20. | Debono B, Wainwright TW, Wang MY, Sigmundsson FG, Yang MMH, Smid-Nanninga H, Bonnal A, Le Huec JC, Fawcett WJ, Ljungqvist O, Lonjon G, de Boer HD. Consensus statement for perioperative care in lumbar spinal fusion: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Spine J. 2021;21:729-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 313] [Cited by in RCA: 257] [Article Influence: 51.4] [Reference Citation Analysis (0)] |
| 21. | Zhu S, Qian W, Jiang C, Ye C, Chen X. Enhanced recovery after surgery for hip and knee arthroplasty: a systematic review and meta-analysis. Postgrad Med J. 2017;93:736-742. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 140] [Cited by in RCA: 229] [Article Influence: 25.4] [Reference Citation Analysis (0)] |
| 22. | Yin L, Wu Y, Ren C, Wang Y, Fu T, Cheng X, Li R, Nie M, Mu Y. Treatment of acute achilles tendon rupture with the panda rope bridge technique. Injury. 2018;49:726-729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 23. | Kowalsky SJ, Zenati MS, Steve J, Esper SA, Lee KK, Hogg ME, Zeh HJ 3rd, Zureikat AH. A Combination of Robotic Approach and ERAS Pathway Optimizes Outcomes and Cost for Pancreatoduodenectomy. Ann Surg. 2019;269:1138-1145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 69] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 24. | Williams SB, Cumberbatch MGK, Kamat AM, Jubber I, Kerr PS, McGrath JS, Djaladat H, Collins JW, Packiam VT, Steinberg GD, Lee E, Kassouf W, Black PC, Cerantola Y, Catto JWF, Daneshmand S. Reporting Radical Cystectomy Outcomes Following Implementation of Enhanced Recovery After Surgery Protocols: A Systematic Review and Individual Patient Data Meta-analysis. Eur Urol. 2020;78:719-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 93] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 25. | Wang SK, Wang QJ, Wang P, Li XY, Cui P, Wang DF, Chen XL, Kong C, Lu SB. The impact of frailty on clinical outcomes of older patients undergoing enhanced recovery after lumbar fusion surgery: a prospective cohort study. Int J Surg. 2024;110:4785-4795. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 26. | Holte K, Foss NB, Andersen J, Valentiner L, Lund C, Bie P, Kehlet H. Liberal or restrictive fluid administration in fast-track colonic surgery: a randomized, double-blind study. Br J Anaesth. 2007;99:500-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 182] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 27. | Lu D, Wang X, Shi G. Perioperative enhanced recovery programmes for gynaecological cancer patients. Cochrane Database Syst Rev. 2012;12:CD008239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 28. | Adamina M, Gié O, Demartines N, Ris F. Contemporary perioperative care strategies. Br J Surg. 2013;100:38-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 29. | Garriga C, Murphy J, Leal J, Price A, Prieto-Alhambra D, Carr A, Arden NK, Rangan A, Cooper C, Peat G, Fitzpatrick R, Barker K, Judge A. Impact of a national enhanced recovery after surgery programme on patient outcomes of primary total knee replacement: an interrupted time series analysis from "The National Joint Registry of England, Wales, Northern Ireland and the Isle of Man". Osteoarthritis Cartilage. 2019;27:1280-1293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 30. | Sauro KM, Smith C, Ibadin S, Thomas A, Ganshorn H, Bakunda L, Bajgain B, Bisch SP, Nelson G. Enhanced Recovery After Surgery Guidelines and Hospital Length of Stay, Readmission, Complications, and Mortality: A Meta-Analysis of Randomized Clinical Trials. JAMA Netw Open. 2024;7:e2417310. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 96] [Article Influence: 48.0] [Reference Citation Analysis (0)] |
| 31. | Mendez E, Puig G, Barquero M, Leon A, Bellafont J, Colomina MJ. Enhanced recovery after surgery: a narrative review on patient blood management recommendations. Minerva Anestesiol. 2023;89:906-913. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 32. | Kehlet H, Lobo DN. Exploring the need for reconsideration of trial design in perioperative outcomes research: a narrative review. EClinicalMedicine. 2024;70:102510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/