Published online Oct 18, 2024. doi: 10.5312/wjo.v15.i10.991
Revised: August 21, 2024
Accepted: September 2, 2024
Published online: October 18, 2024
Processing time: 140 Days and 0.9 Hours
Extracorporeal shock wave therapy (ESWT) is increasingly being recognized as an advantageous alternative for treating non-union due to its efficacy and minimal associated complications. Non-union following Bernese periacetabular osteotomy (PAO) is particularly challenging, with a reported 55% delayed union and 8% non-union. Herein, we highlight a unique case of ischial non-union post-PAO treated successfully with a structured ESWT regimen.
A 50-year-old patient, diagnosed with left ischial non-union following the PAO, underwent six cycles of ESWT treatment across ten months. Each cycle, spaced four weeks apart, consisted of five consecutive ESWT sessions without anesthesia. Regular X-ray follow-ups showed progressive disappearance of the fracture line and fracture union. The patient ultimately achieved a satisfactory asymptomatic recovery and bone union.
The results from this case suggest that this ESWT regimen can be a promising non-invasive treatment strategy for non-union following PAO.
Core Tip: Non-union following periacetabular osteotomy is a postoperative complication that is challenging to resolve through conservative treatment alone and typically necessitates surgical intervention for effective management. A personalized extracorporeal shock wave therapy regimen can help us address this challenge effectively.
- Citation: Yan J, Zhu JY, Zhao FF, Xiao J, Li H, Wang MX, Guo J, Cui L, Xing GY. Extracorporeal shock wave therapy in treating ischial non-union following Bernese periacetabular osteotomy: A case report. World J Orthop 2024; 15(10): 991-996
- URL: https://www.wjgnet.com/2218-5836/full/v15/i10/991.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i10.991
Despite advancements in osteotomy techniques for acetabular dysplasia, non-union or delayed union remains a common postoperative complication, with an incidence rate of 8%[1]. Surgical treatments, while effective, are costly, uncertain, and often accompanied by complications, such as infection or neurovascular injury[2]. This necessitates the exploration of noninvasive alternatives. One such promising modality is extracorporeal shock wave therapy (ESWT), which has de
Treatment of deep-seated nonunions like the ischium, however, presents unique challenges. Achieving accurate energy delivery to the fracture site for successful bone healing is difficult due to the deep location of the ischium and its coverage by surrounding musculature[7]. This underscores the need for an optimized, short-term, and effective treatment regimen tailored to patients’ individual characteristics.
To our knowledge, no studies have yet proposed a standardized protocol for ESWT regarding the timing of treatment of femoral non-union. Furthermore, few studies have explored multiple treatments or cyclical regimens[6,8]. This case report aims to bridge this gap by presenting a unique case of successful non-union management of the left ischial ramus post-internal fixation with acetabular osteotomy screws, utilizing a cyclical ESWT regimen. This case report illuminates a potential pathway for the nonsurgical management of deep tissue non-union, contributing significant clinical value to the field.
A 50-year-old female patient was experiencing pain in her left hip and a limited range of motion when walking and squatting.
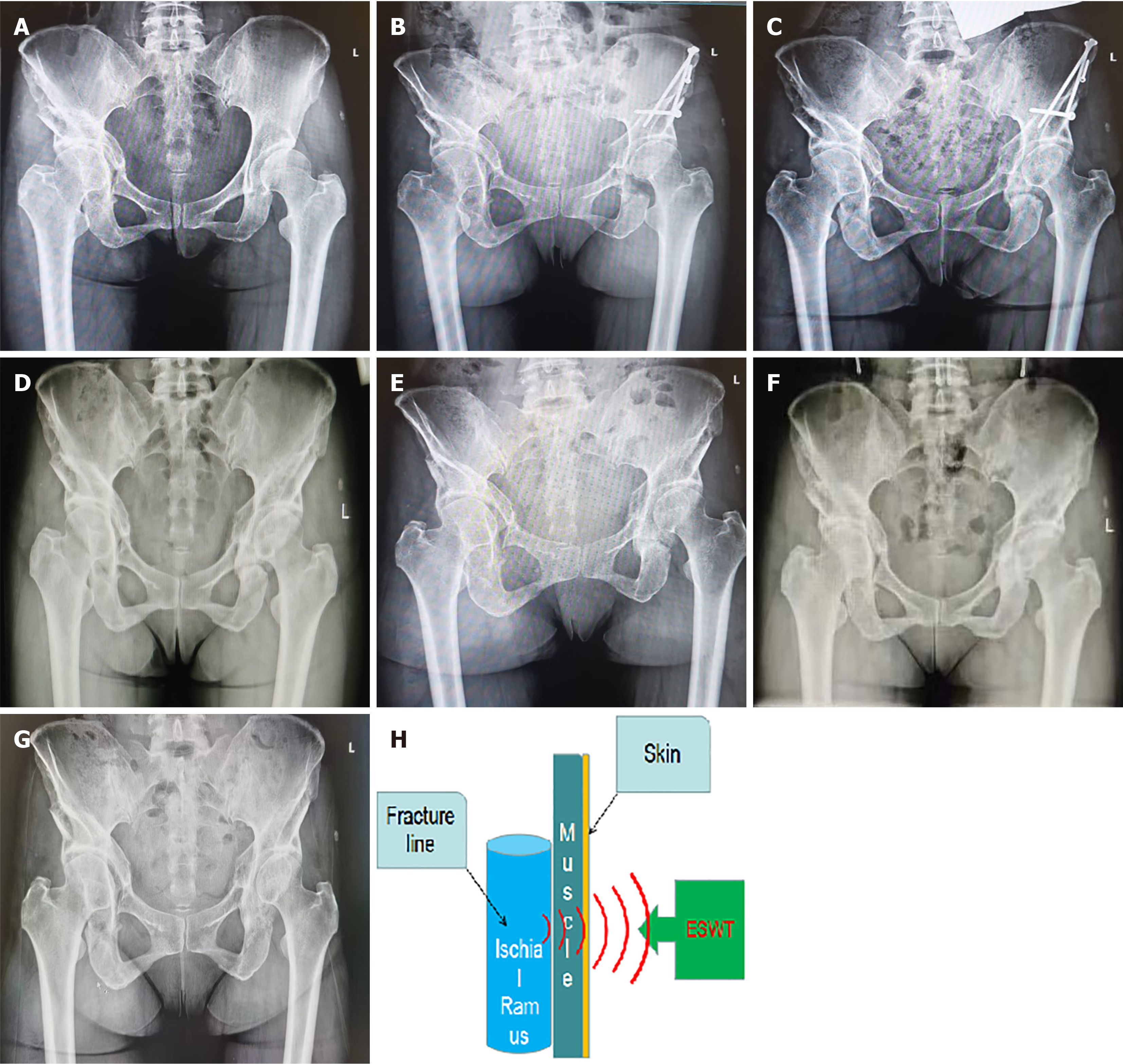
When known, the age, sex, body mass index, injury location, surgical procedure, past medical history, duration, and clinical description were recorded (Table 1). The patient underwent a left pelvic osteotomy procedure with corrective screw fixation on May 13, 2019, due to bilateral acetabular dysplasia (Figure 1A and B). The procedure involved an open approach, osteotomy, rotational correction, and screw fixation. In the year following her operation, she attended The Fourth Medical Center of our hospital every three months for X-ray examinations. These showed a clear fracture of the left ischial branch and gradual formation of surrounding sclerotic bone. However, the X-rays from the last three months did not show any notable evidence of callus formation (Figure 1C). Following a consultation at The Third Medical Center of our hospital, she was diagnosed with a non-union of the left ischium, prompting her to seek ESWT at the Third Medical Center's treatment room.
| Case | Age in year | Sex | Body mass index in kg/m2 | Location | Surgical procedure | Past medical history | Duration of non-union | Clinical description |
| 1 | 50 | Female | 23.81 | Left hip | Periacetabular osteotomy | (-) | > 13 months | Non-union, pain, restricted mobility |
There is no history of past illness.
The patient was healthy prior to her diagnosis of acetabular dysplasia before the operation. She had no notable personal or family history, had undergone a cesarean section, and had no history of blood transfusions.
The patient had an arc-shaped surgical scar approximately 20 cm long on the anterior side of her left hip, resulting from the periacetabular osteotomy (PAO) and orthopedic screw fixation through an anterior hip approach. She experienced pain during active flexion and hip extension, but passive movement was possible. No evident local tenderness was observed. Skin sensation, temperature, and blood circulation at the local site were normal.
Laboratory examinations were unnecessary.
X-ray imaging showed the left ischial branch in normal alignment, with a clear fracture line and no signs of bone union. The internal fixation position of the ilium osteotomy was correct and stable, with no displacement (Figure 1C).
Non-union of the ischium following a left PAO.
The patient underwent a structured ESWT regimen using a focused shock wave generator (HK.SWT-007, Huikan AG, China) device. The protocol included six cycles, each consisting of five ESWT sessions on alternate days, with a four-week interval between cycles. Each session lasted approximately 20 minutes and was conducted without local anesthesia (Figure 2). This personalized treatment regimen is tailored based on the feedback collected following each treatment session. We will evaluate the patient's pain levels and functional mobility pre-treatment and post-treatment through the visual analog scale (VAS) and comprehensive physical examination. We utilized this as a valid basis for assessing the duration of treatment efficacy and implementing regular follow-up evaluations. Upon completing each treatment re
The procedure is as follows: The patient was positioned supine with a flexed left hip to prevent occlusion of the is
The shock wave's direction was optimized to ensure unblocked energy delivery to the fracture ends, avoiding areas covered by internal fixation and neurovascular structures. Post-treatment examinations were conducted to assess local complications and the patient's condition. After the treatment, the patient resumed her usual weight-bearing condition and was advised to avoid strenuous activity.
The patient completed a total of six cycles of ESWT. After the final treatment cycle, a 10-month follow-up evaluation was conducted, which assessed local tenderness at the osteotomy site, hip range of motion, and weight-bearing capabilities of the affected limb. Notably, new bone formation at the bridging callus and circumferential osteotomy sites was observed on plain films after each cycle, with significant progression seen during the third to fourth treatment cycles and the first six months of the follow-up period.
The X-ray image also depicted a gradual decrease in the gap between the amputated ends and an enhancement in bone density around the original osteotomy site that continued to improve over time (Figure 1D and E). By the sixth month of imaging, the transverse fracture line had nearly disappeared (Figure 1F), indicating a fully formed bony union with co
As the fracture site healed, the patient's active pain was eliminated, and she resumed her daily activities without any abnormal symptoms (Figure 1G). Importantly, no local complications attributable to ESWT were observed during the entire treatment process (Figure 1H).
As defined by the United States Food and Drug Administration, non-union is characterized by persistent bone disruption or failure to achieve bone union within nine months post-surgery and a lack of union signs for at least three consecutive months[9,10]. In this case, the diagnosis of non-union was made based on radiographically discontinuous osseous union and radiographic penetration of the osteotomy site. Complete bone healing is defined as the formation of a bone bridge at the osteotomy site, with a continuous trabecular pattern observed. Various factors influence non-union, including sys
ESWT, first reported by Valchanou and Michailov in 1991 for treating cases of delayed union and non-union, has emerged as a promising technique. ESWT has been used to treat various musculoskeletal disorders, including rotator cuff calcific tendonitis, lateral epicondylitis, and chronic plantar fasciitis. The mechanisms of ESWT support its positive effects on bone biology through enhanced biomechanical properties (increased bone mass and strength) and angiogenesis[12]. However, a universally accepted standard for ESWT timing is yet to be established.
In this case study, the patient underwent osteotomy following the classical sequence without receiving anesthetic treatment for the ESWT, thus avoiding the risks and complications of anesthesia. High patient compliance is a crucial factor due to the extended duration of this type of treatment. Each course of treatment only lasted 20 minutes, and our patient only needed six courses of treatment, with a short interval (about four weeks) before the next cycle. At the sixth month of follow-up, the non-union had healed, and the patient could participate in normal physical activity at his last visit. No local complications were observed throughout the treatment regimen.
The characteristics of our treatment regimen can be summarized as 'repeatability' and 'fractionation', corresponding to 5 times per cycle and a total of 6 cycles with shorter intervals in the regimen, respectively. A significant advantage of our treatment regimen is that the ESWT with fractional repetition allows progressive shock wave stimulation of the treated area while maintaining the same total number of prior treatments, giving the body a proper interval of time to repair itself. This case study illustrates the potential of ESWT in treating ischial non-union after PAO and proposes a new therapeutic approach for this condition.
Although this is only a case study and not representative, it provides valuable insights into the potential of ESWT as a non-surgical treatment option for deep bone non-union. Further research is needed to optimize ESWT treatment protocols and accumulate more clinical experience in treating ischial non-union after PAO.
The findings from this case study suggest that a structured, multi-cycle, short-interval ESWT regimen can significantly improve non-union healing in patients who prefer non-surgical treatment options. Consequently, this ESWT regimen might present a promising and viable therapeutic strategy for managing ischial non-union following PAO. While these results are encouraging, further research is necessary to validate and optimize this treatment approach, contributing to the broader understanding and management of such orthopedic conditions.
| 1. | Selberg CM, Davila-Parrilla AD, Williams KA, Kim YJ, Millis MB, Novais EN. What Proportion of Patients Undergoing Bernese Periacetabular Osteotomy Experience Nonunion, and What Factors are Associated with Nonunion? Clin Orthop Relat Res. 2020;478:1648-1656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 2. | Shearman AD, Hashemi-Nejad A, Bankes MJ, Lewis AD. Surgical management of chronic pelvic instability following periacetabular osteotomy nonunion. Hip Int. 2020;30:787-792. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 3. | Kuo SJ, Su IC, Wang CJ, Ko JY. Extracorporeal shockwave therapy (ESWT) in the treatment of atrophic non-unions of femoral shaft fractures. Int J Surg. 2015;24:131-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 4. | Mittermayr R, Haffner N, Feichtinger X, Schaden W. The role of shockwaves in the enhancement of bone repair - from basic principles to clinical application. Injury. 2021;52 Suppl 2:S84-S90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 5. | Dahm F, Feichtinger X, Vallant SM, Haffner N, Schaden W, Fialka C, Mittermayr R. High-energy extracorporeal shockwave therapy in humeral delayed and non-unions. Eur J Trauma Emerg Surg. 2022;48:3043-3049. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 6. | Cacchio A, Giordano L, Colafarina O, Rompe JD, Tavernese E, Ioppolo F, Flamini S, Spacca G, Santilli V. Extracorporeal shock-wave therapy compared with surgery for hypertrophic long-bone nonunions. J Bone Joint Surg Am. 2009;91:2589-2597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 97] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 7. | Hausdorf J, Lutz A, Mayer-Wagner S, Birkenmaier C, Jansson V, Maier M. Shock wave therapy for femoral head necrosis-Pressure measurements inside the femoral head. J Biomech. 2010;43:2065-2069. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Vulpiani MC, Vetrano M, Conforti F, Minutolo L, Trischitta D, Furia JP, Ferretti A. Effects of extracorporeal shock wave therapy on fracture nonunions. Am J Orthop (Belle Mead NJ). 2012;41:E122- E127. [PubMed] |
| 9. | Bishop JA, Palanca AA, Bellino MJ, Lowenberg DW. Assessment of compromised fracture healing. J Am Acad Orthop Surg. 2012;20:273-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 199] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 10. | Schlundt C, Bucher CH, Tsitsilonis S, Schell H, Duda GN, Schmidt-Bleek K. Clinical and Research Approaches to Treat Non-union Fracture. Curr Osteoporos Rep. 2018;16:155-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 80] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 11. | Nicholson JA, Makaram N, Simpson A, Keating JF. Fracture nonunion in long bones: A literature review of risk factors and surgical management. Injury. 2021;52 Suppl 2:S3-S11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 182] [Article Influence: 36.4] [Reference Citation Analysis (0)] |
| 12. | Searle HK, Lewis SR, Coyle C, Welch M, Griffin XL. Ultrasound and shockwave therapy for acute fractures in adults. Cochrane Database Syst Rev. 2023;3:CD008579. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/