Published online Jan 18, 2024. doi: 10.5312/wjo.v15.i1.73
Peer-review started: November 18, 2023
First decision: December 7, 2023
Revised: December 20, 2023
Accepted: December 29, 2023
Article in press: December 29, 2023
Published online: January 18, 2024
Processing time: 58 Days and 16.8 Hours
Total hip arthroplasty is as an effective intervention to relieve pain and improve hip function. Approaches of the hip have been exhaustively explored about pros and cons. The efficacy and the complications of hip approaches remains in
To compare the efficacy and complications of hip approaches that have been published in all MAs and randomized controlled trials (RCTs).
MAs were identified from MEDLINE and Scopus from inception until 2023. RCTs were then updated from the latest MA to September 2023. This study included studies which compared hip approaches and reported at least one outcome such as Harris Hip Score (HHS), dislocation, intra-operative fracture, wound compli
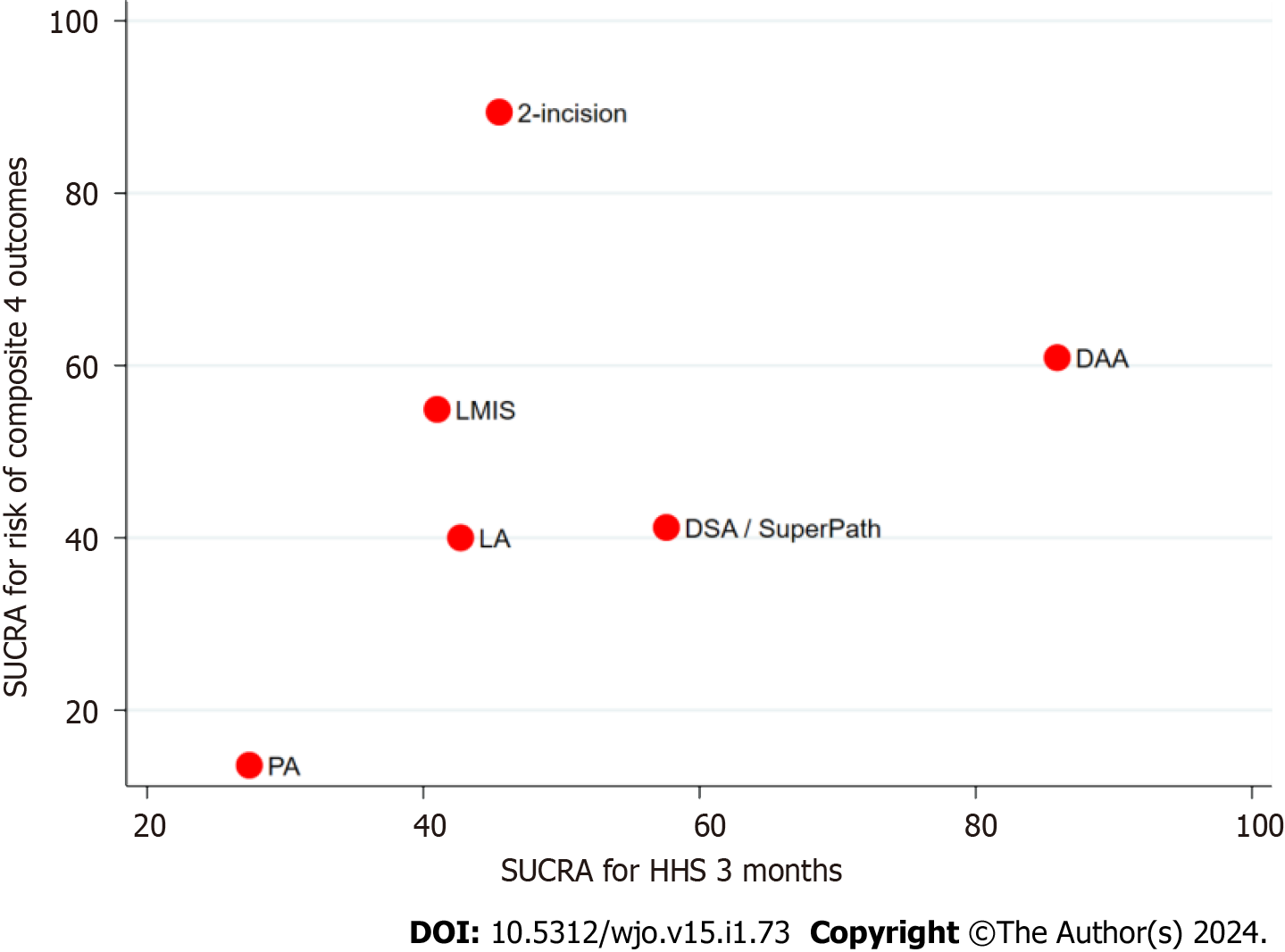
Finally, twenty-eight MAs (40 RCTs), and 13 RCTs were retrieved. In total 47 RCTs were included for reanalysis. The results of corrected covered area showed high degree (13.80%). Among 47 RCTs, most of the studies were low risk of bias in part of random process and outcome reporting, while other domains were medium to high risk of bias. DAA significantly provided higher HHS at three months than PA [pooled unstandardized mean difference (USMD): 3.49, 95% confidence interval (CI): 0.98, 6.00 with SUCRA: 85.9], followed by DSA/SuperPath (USMD: 1.57, 95%CI: -1.55, 4.69 with SUCRA: 57.6). All approaches had indifferent dislocation and intraoperative fracture rates. SUCRA comparing early functional outcome and composite complications (dislocation, intra-operative fracture, wound complication, and nerve injury) found DAA was the best approach followed by DSA/SuperPath.
DSA/SuperPath had better earlier functional outcome than PA, but still could not overcome the result of DAA. This technique might be the other preferred option with acceptable complications.
Core Tip: Total hip arthroplasty (THA) is as an effective intervention to relieve pain and improve hip function. Many minimally invasive surgeries have been proposed to preserve soft tissue and promote early recovery. Direct anterior approach and direct superior approach, the most popular and the newest technique, respectively have been explored about pros and cons to compare with previous conventional techniques. The results are still inconclusive. This is the first umbrella review that has included all systematic reviews and meta-analysis comparing the efficacy and complications among approaches of THA for patients in term of post-operative functional score and post-operative complications.
- Citation: Nitiwarangkul L, Hongku N, Pattanaprateep O, Rattanasiri S, Woratanarat P, Thakkinstian A. Which approach of total hip arthroplasty is the best efficacy and least complication? World J Orthop 2024; 15(1): 73-93
- URL: https://www.wjgnet.com/2218-5836/full/v15/i1/73.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i1.73
Total hip arthroplasty (THA) is an effective intervention for improvement of pain and hip function[1-4]. More than 1.4 million hip replacements are annually performed worldwide. Hip prosthesis has been established since 1950s[5]. Porous structure or bottom profile dimples of the ball type promote longevity, osteointegration and medullary revascularization[6-9]. Various bearing surfaces (i.e., titanium on polyethylene, cobalt chromium molybdenum, ceramic, and polycrystalline diamond[10]), have been applied to optimize corrosive quality, stress reduction, contact pressure[11] and prevent osteolysis[2-4]. Survival of total hip replacement is not only influenced by deformation of prosthesis[2], acetabular cup inclination, body mass index (BMI)[3] and effects of pressure during walking[12,13], but it also depends on surgical approaches to the hip joint. Meanwhile, bleeding, wound problems, abductor muscle disruption and dislocation/instability were considered as common complications[7].
Approaches of the hip have been exhaustively explored about pros and cons. A conventional technique is the posterior approach (PA) by cutting short external rotator muscles. This technique provides a good exposure, but increases risk of hip dislocation[14]. Many minimally invasive surgeries (MIS) have been proposed to preserve soft tissue; promote early recovery, and lessen complications[6]. Direct lateral approach (LA) preserves posterior joint capsule, but may jeopardize superior gluteal nerve. Direct anterior approach (DAA) through an intermuscular plane[14] is the most popular, and preferred technique. Two-incision method combined anterior, to allow the acetabular cup placement, and posterior directions[15]. Mini-lateral approach (LMIS) can be performed with a shorter oblique skin incision without splitting or detaching muscle. Recently, direct superior approach (DSA) and supercapsular percutaneously-assisted total hip (SuperPath) are the newest MIS technique for PA by sparing the iliotibial band, obturator externus and quadratus femoris muscle[16,17]. An evidence from a randomized controlled trial (RCT) indicated that DSA was preferred to the posterolateral approach in terms of blood loss, gait, and muscle strength[18]. SuperPath technique allowed shorter incision length[19], and early mobilization[17].
Many systematic reviews and meta-analysis (MA) of THA[6,20-46] showed that DAA could be beneficial for early hip function, and post-operative pain than other techniques[6,23,28,30,34-36,42,44,45]. Contradictory, it came up with a higher incidence of nerve injury[28,32,42,45,47], and inconsistent issues of other complications[6,31,37,39,44]. PA may be inferior to DAA, and other various hip approaches including DSA/SuperPath. A recent network MA reported conventional PA contributed to poorer hip function, insignificant complications, but had the advantage in shorter operative time when compared to DAA, DSA/SuperPath, MIS direct LA/anterolateral/PA[48]. Nevertheless, clinical important outcomes including hip dislocation, intra-operative fracture and wound complications were not considered. A comprehensive review of relevant MAs should lead to properly identify the best hip approach. This study hypothesized that various hip approaches provide different results. Therefore, an umbrella review was aimed to systematically appraise the quality of previous evidences and re-estimate the treatment effects and complication rates among THA approaches by re-pooling data. Update searching was filtered by the last search of when the previous MA was done, and at least 13 RCTs were recently added. A risk-benefit assessment (RBA) was also performed.
An umbrella review of MAs was conducted with the following guidelines in the Preferred Reporting Items for Systematic Reviews and MA (PRISMA)[49]. The review protocol was registered in the international prospective register of systematic reviews; PROSPERO (CRD42017072580).
PubMed and Scopus databases were used to identify data from an inception to the date of September 2023. Search terms were constructed according to patients (P), interventions (I), comparators (C), and outcomes (O), see Supplemen
This study was divided into two parts, previous MAs exploration and update searching. First, previous MAs were explored and RCTs in those studies were retrieved. Previous MAs were eligible if they met the following criteria: systematic reviews of RCTs, use MA to obtain pooled effect size for outcomes that we are interested in among PA, LA, DAA, 2-incisions, LMIS, and DSA/SuperPath. One reviewer selected studies by titles and abstracts and another reviewer randomly checked about the accuracy. If a decision could not be made, the full texts were retrieved and reviewed. Any disagreement was resolved by discussion with a supervisor.
Second, updated searching was done and filtered from the last search of previous MA. Eligible RCTs were published in English language, studied in patients who underwent primary THA, compared with any pair among the hip approaches and reported at least one of the interested outcomes; Harris Hip Score (HHS), dislocation, intra-operative fracture, operative time, length of hospital stays, incision length, operative blood loss, wound complication, nerve injury, and visual analog scale (VAS). Studies were excluded if patients underwent bilateral THAs, or revision THA; had severe soft tissue damage; fracture or severe acetabular bone loss; computer navigation or robotic assisted surgery; modified techniques of each interested approach, i.e., mini-posterior, modified PA; learning curve of surgeon; reported only long term outcomes; RCTs with randomization of other interventions rather than interested hip approaches, RCTs with randomization only of intervention groups comparing with one control group; and multiple publications.
The interested interventions were PA, LA, DAA, 2-incisions, LMIS, and DSA/SuperPath. The primary outcomes were HHS, dislocation, and intra-operative fracture. HHS ranged from 0 to 100, at follow up time of ≤ three months, six months, and one year[50]. Dislocation was diagnosed if a femoral head was not in the acetabular cup within the six-month post-operative period. Intra-operative fracture was defined as any fracture which occurred in the operative field.
The secondary outcomes were operative time (time at incision to the last stitch of wound closure, minutes), length of hospital stay (d), incision length (cm), operative blood loss (mL), wound complication (dehiscence, infection), nerve injury and VAS (0-10).
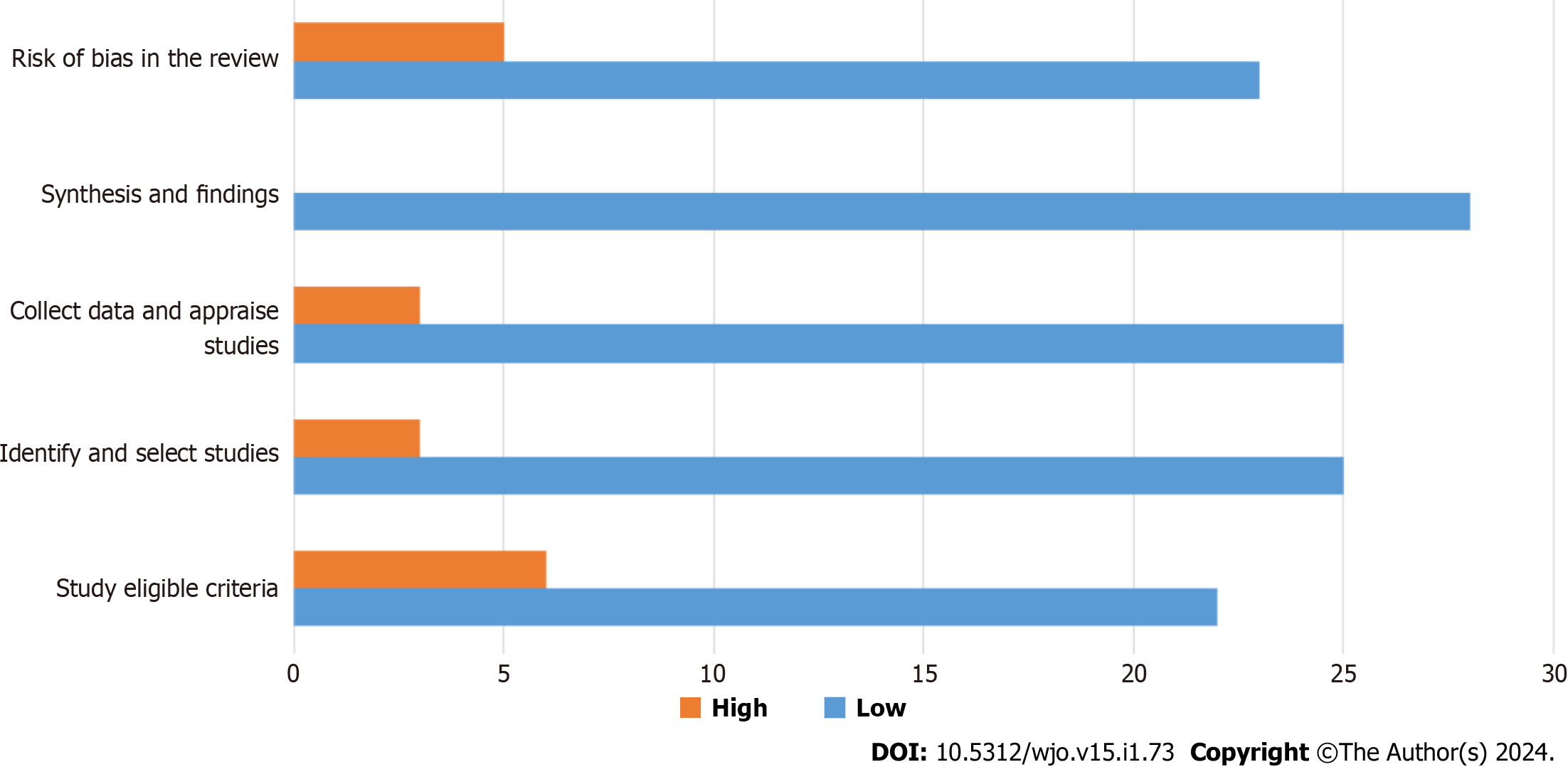
Risk of bias assessment was performed using a Risk of Bias Assessment Tool for Systematic Reviews (ROBIS)[51], which comprises three phases. Phase I assessed whether a systematic review/MA clearly stated their PICOS. Phase II assessed bias in the review process of study eligible criteria, identification and study selection, data collection and study appraisal and synthesis/finding. They were rated as low, high or unclear. The last phase was an overall judgement.
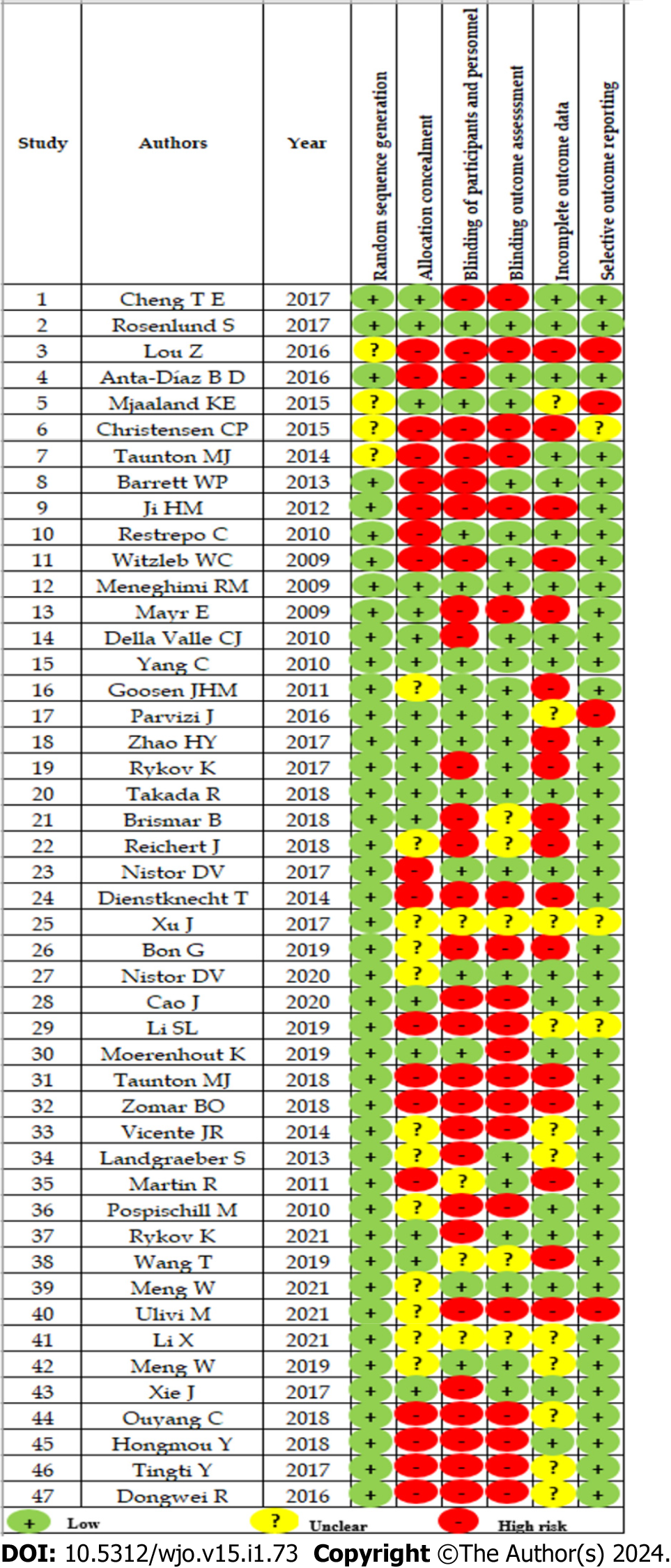
For each RCT, study quality was evaluated using The Cochrane Collaboration’s tool for assessing risk of bias in randomized trials[52] This includes random sequence allocation, allocation concealment, blinding patients and assessors, blinding outcome assessment, incomplete outcome data management, and selective outcome reporting.
Characteristics of MAs were extracted including, databases used, last search date, number of included studies, type of intervention (PA, LA, DAA, 2-incisions, LMIS, and DSA/SuperPath), risk of bias assessment and outcomes of interest. Specific methods and findings were also extracted including pooled effect size along with 95% confidence interval (CI), pooling methods (fixed and random effects), heterogeneity assessment (i.e., I2 and Cochran Q test) and publication bias.
Furthermore, characteristics of the individual RCTs included in MA were also extracted to re-pool with updated RCTs beyond the last searching of previous MAs. Data was extracted including with general characteristics of study, patients and intervention-outcomes. Additionally, contingency data of interventions and outcomes were extracted for pooling dichotomous outcomes. Number of patients and mean value along with standard deviation were retrieved for pooling with continuous data.
The data extraction was independently performed by two reviewers. Disagreement was resolved by discussion with a supervisor.
The statistical methods of this study were reviewed by Sasivimol Rattanasiri, PhD, Associate Professor from the Department of Clinical Epidemiology and Biostatistics, Faculty of Medicine Ramathibodi Hospital, Mahidol University. Characteristics, results and risk of bias of MAs were summarized by using descriptive analysis. Overlapping studies were assessed using corrected covered area (CCA) to detect that previous individual RCTs were not included in previous MAs more than once. The citation matrix was constructed which assigned previous MAs in the first column and included individual RCTs in rows. The CCA was then classified as slight, moderate, high, and very high overlap if the CCA was 0% to 5%, 6% to 10%, 11% to 15%, and > 15%, respectively. Higher CCA reflects lower additional information across MAs.
This study also re-estimated the pooled effect size [e.g., risk ratio (RR) or unstandardized mean difference (USMD)] using the data from individual RCTs that were included in these MAs and adding more studies by updating from the last search in the year 2019 from previous MAs. A fixed-effects model was used, if there was no evidence of heterogeneity, otherwise, the random-effects model was applied. Heterogeneity was present if P value for Q test was < 0.100 and I2 was 25% or higher. Publication bias was determined by asymmetrical funnel plots and significant Egger’s test. Constructed contour-enhanced funnel plots were further performed to distinguish between heterogeneity and publication bias.
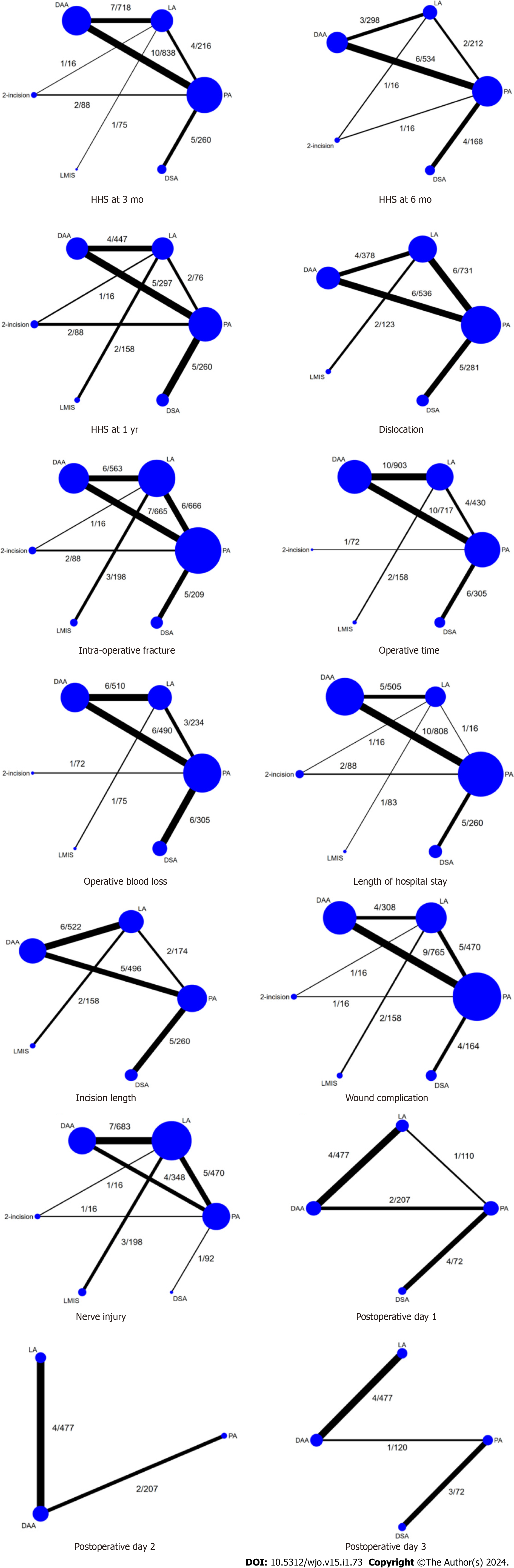
A network MA (NMA) was conducted in the re-pooling process to estimate the mixed relative intervention effects by a two-stage approach. Six interventions (PA, reference, LA, DAA, 2-incisions, LMIS, and DSA/SuperPath) were coded as one, two, three, four, five, and six. Regression analysis with logit-link for dichotomous and identity-link for continuous outcomes was applied for each study. The coefficients and variance-covariance were then pooled using a multivariate MA with a consistency model, and estimated relative treatment effects. Inconsistency assumption was checked using a global Chi-square test. An adjusted funnel plot was constructed for publication bias assessment. Probability of being the best intervention was estimated and ranked using surface under cumulative ranking curve (SUCRA). All analyses were performed using STATA version 17.0, StataCorp, College Station, Texas, United States. P value < 0.05 was considered statistical significance.
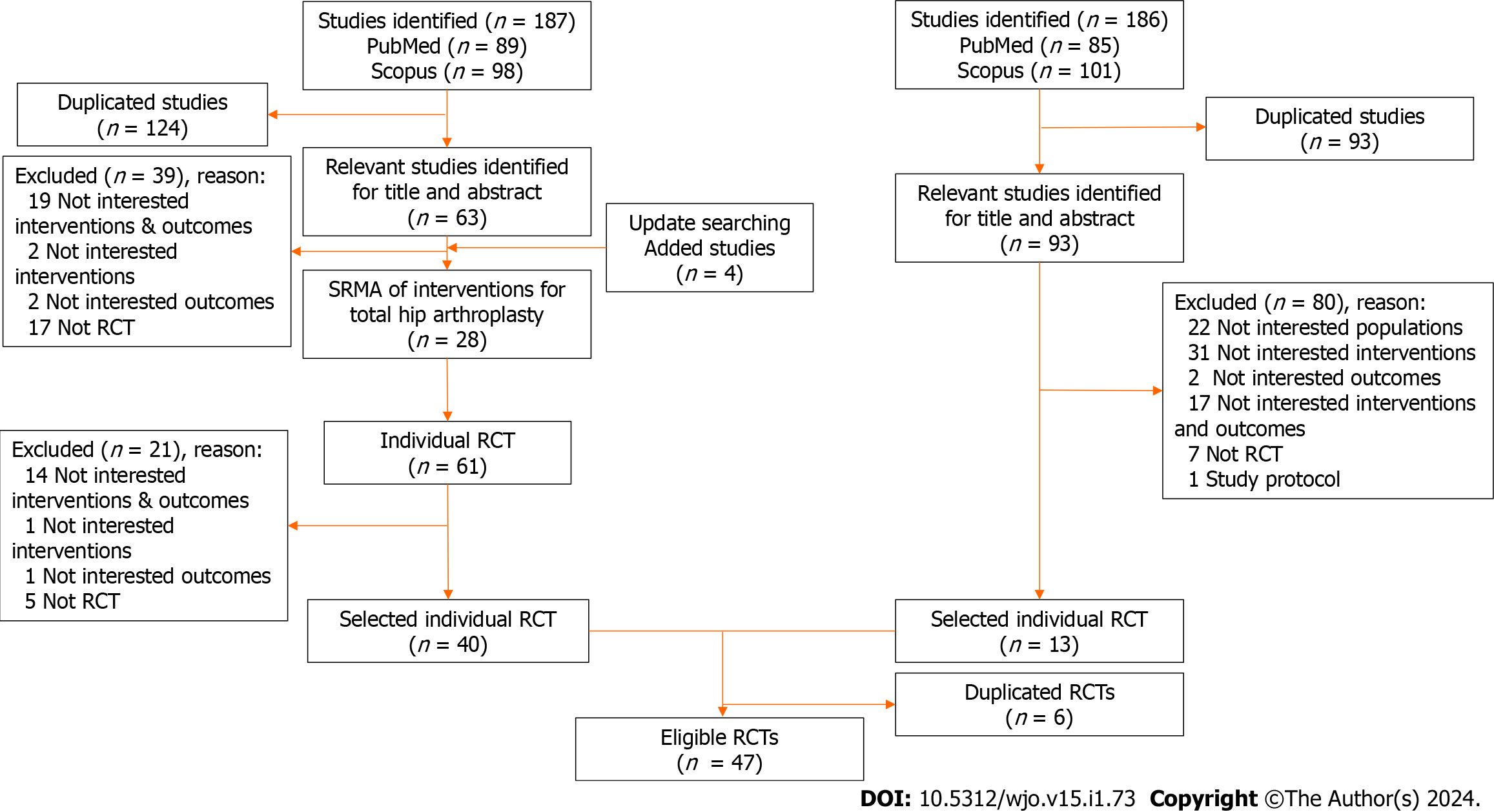
For the first part, 28 MAs[6,20-46] were identified from PubMed and Scopus according to PICOS, including 61 RCTs. Finally, 40 RCTs were retrieved from previous MAs after screening for the eligible criteria and removing duplicated studies. For the second part, a total number of 85 and 101 studies were identified from PubMed and Scopus according to PICO. Thirteen RCTs met the inclusion criteria, and six duplicated studies were found. Finally, 47 RCTs[18,19,53-97] from both parts were included (Figure 1). The results of estimated CCA showed high degree (13.80%) of overlapping of individual RCTs among previous MAs (Supplementary Table 2).
The characteristics of 28 MAs are described in Table 1. Seventeen MAs included only RCTs. Twelve MAs including both RCTs and observational studies. These studies were published between the year 2014 and 2023 and had total sample sizes which ranged from 475 to 283036.
| Ref. | Last search | Study design | Number of included studies | Sample size | Intervention | Reference | Outcome |
| Putananon et al[37], 2018 | February, 2017 | RCT | 14 | 1201 | PA/LA/DAA/PA2 | PA | HHS, VAS, complications |
| Higgins et al[6], 2015 | February, 2014 | RCT & nRCT | 17 | 2302 | PA/DAA | PA | HHS, VAS, blood loss, intra-operative fracture, operative time, length of hospital stay, dislocation |
| Miller et al[34], 2018 | June, 2017 | RCT & nRCT | 13 | 1044 | PA/DAA | PA | HHS, dislocation, intra-operative fracture, wound infection |
| Wang et al[44], 2018 | June, 2018 | RCT | 9 | 754 | PA/DAA | PA | HHS, VAS, incision length, operative time, length of hospital stay, operative blood loss, intra-operative fracture, dislocation |
| Miller et al[35], 2018 | June, 2017 | RCT | 7 | 609 | PA/DAA | PA | Incision length, length of hospital stay, operative time, operative blood loss, pain score, complication |
| Kucukdurmaz et al[30], 2019 | January, 2018 | RCT & nRCT | 17/1 | 1543 | PA/LA/DAA | PA | HHS, operative time, incision length, VAS, neurapraxia, intra-operative fracture, wound infection, dislocation |
| Jia et al[28], 2019 | August, 2016 | RCT & nRCT | 4/16 | 7377 | PA/DAA | PA | HHS, length of hospital stay, operative time, VAS, dislocation, neurapraxia, intra-operative fracture |
| Wang et al[43], 2019 | October, 2018 | RCT | 5 | 475 | LA/DAA | LA | HHS, VAS, operative time, operative blood loss, length of hospital stay, complication |
| Migliorini et al[32], 2021 | September, 2019 | RCT & nRCT | 20/39 | 10675 | PA/LA/DAA | PA | Dislocation, nerve injury, revision |
| Migliorini et al[33], 2020 | October, 2019 | RCT & nRCT | 13/23 | 4383 | PA/LA/DAA | PA | Length of hospital stay, operative time, operative blood loss |
| Cha et al[22], 2020 | October, 2019 | RCT | 8 | 673 | PA/LA/DAA | PA | Operative time, Operative blood loss |
| Peng et al[36], 2020 | November, 2019 | RCT | 7 | 600 | PA/DAA | PA | HHS, VAS, operative time, operative blood loss, length of hospital stay, incision length |
| Docter et al[24], 2020 | June, 2019 | RCT & nRCT | 19/50 | 283036 | PA/LA/DAA | PA | Dislocation, intra-operative fracture, infection |
| Yang et al[45], 2020 | June, 2019 | RCT | 11 | 932 | PA/DAA | PA | VAS, neurapraxia, intra-operative fracture, infection, dislocation, operative time, operative blood loss, length of hospital stay |
| Chen et al[23], 2020 | 2020 | RCT & nRCT | 4 /14 | 34873 | PA/DAA | PA | HHS, VAS, operative time, operative blood loss, length of hospital stay, dislocation, intra-operative fracture |
| Sun et al[42], 2021 | June, 2019 | RCT & nRCT | 3 /6 | 22698 | PA/DAA | PA | HHS, operative time, operative blood loss, length of hospital stay, complication |
| Awad et al[21], 2021 | 2021 | RCT & nRCT | 7/22 | 8576 | PA/DAA | PA | HHS, operative time, operative blood loss, length of hospital stay, complication |
| Huerfano et al[27], 2021 | 2021 | RCT & nRCT | 5/20 | 7172 | PA/DAA/ | PA | Dislocation |
| Gazendam et al[25], 2022 | 2021 | RCT | 25 | 2339 | PA/LA/ALA/DAA | PA | HHS, VAS, length of hospital stay, complication |
| Ge et al[26], 2021 | 2021 | RCT & nRCT | 3/3 | 526 | DSA/SuperPath/PA | PA | HHS, operative time, operative blood loss, incision length, VAS, length of hospital stay |
| Joseph et al[29], 2023 | 2022 | RCT | 7 | 730 | DSA/SuperPath/PA | PA | HHS, operative time, operative blood loss, incision length, VAS, length of hospital stay, complication |
| Lazaru et al[31], 2021 | 2021 | RCT | 9 | 998 | DAA/PA | PA | HHS, operative time, operative blood loss, incision length, VAS |
| O’connor et al[105], 2021 | 2021 | No RCT | 15 | 1872 | DAA/non-DAA | PA, ALA, LA | Infection |
| Ramadanov et al[39], 2021 | 2021 | RCT | 16 | 1392 | DSA/SuperPath/DAA/PA | PA | HHS, operative time, operative blood loss, incision length, VAS |
| Ramadanov et al[40], 2021 | 2021 | RCT | 24 | 2074 | DSA/SuperPath/DAA/PA | PA | HHS, operative time, operative blood loss, incision length, VAS, complication |
| Ramadanov et al[41], 2022 | 2022 | RCT | 20 | 1501 | SuperPath/DAA/PA | PA | HHS, operative time, operative blood loss, incision length |
| Ramadanov et al[38], 2022 | 2022 | RCT | 14 | 1021 | SuperPath/PA | PA | HHS, operative time, operative blood loss, incision length, VAS, complication |
| Zhou et al[46], 2022 | 2022 | RCT | 15 | 1450 | DAA/PA/LA | PA, LA | HHS, operative time, length of hospital stay, complication |
| Ang et al[20], 2023 | 2023 | RCT | 24 | 2010 | DAA/LA/PA | PA | HHS, operative time, length of hospital stay, complication |
Flow chart of excluded studies with explanations according to PRISMA guidelines was constructed. Most studies were from USA, Europe and China. The numbers of included studies were thirteen PA vs DAA[53,54,56-58,69,75,84,85,87,88,94,96], thirteen LA vs DAA[55,59,61,67,71,74,76,77,79,81,82,86,97], seven PA vs LA[63,65,83,90-92,95], one PA vs two-incision[60], one PA vs LA vs two-incision[72], three LMIS vs LA[66,70,80], seven DSA/SuperPath vs PA[18,19,64,68,73,78,93] and two DSA/SuperPath vs LA[62,89]. The mean age was 51 to 76 years, BMI 21-31 kg/m2, 13%-65% male and 20%-100% had hip osteoarthritis (Table 2).
| Ref. | Country | Mean age | BMI | Male (%) | ASA | F/U (wk) | Diagnosis (% OA) | Intervention |
| Li et al[68], 2021 | China | 76.35 | 22.85 | 53.13 | NR | NR | NR | DSA/SuperPath vs PA |
| Ulivi et al[18], 2021 | Italy | 72.98 | 23.51 | 37.78 | NR | 26 | NR | DSA/SuperPath vs PA |
| Meng et al[19], 2021 | China | 64.90 | 23.09 | 42.50 | 2.35 | 52 | NR | DSA/SuperPath vs PA |
| Rykov et al[84], 2021 | Netherlands | 62.50 | 28.20 | 41.30 | 1.59 | 52 | NR | DAA vs PA |
| Cao et al[56], 2020 | China | 61.90 | 24.90 | 42.31 | NR | 26 | NR | DAA vs PA |
| Nistor et al[76], 2020 | Romania | 62.63 | 28.15 | 41.07 | NR | 52 | NR | DAA vs LA |
| Meng et al[73], 2019 | China | 51.00 | 21.49 | 100.00 | 1.66 | 52 | NR | DSA/SuperPath vs PA |
| Wang et al[91], 2019 | China | 55.39 | 23.09 | 59.26 | NR | 52 | 100.00 | LA vs PA |
| Moerenhout et al[75], 2020 | Switzerland | 69.66 | 27.10 | 52.73 | 1.90 | 260 | NR | DAA vs PA |
| Li et al[67], 2019 | China | 62.00 | 23.26 | 73.33 | NR | 26 | 42.00 | DAA vs LA |
| Bon et al[54], 2019 | France | 68.12 | 26.58 | 44.00 | NR | NR | 100.00 | DAA vs PA |
| Ouyang et al[78], 2018 | China | 56.00 | 23.19 | 70.83 | 2.21 | NR | 20.83 | DSA/SuperPath vs PA |
| Zomar et al[97], 2018 | Canada | 60.11 | 29.73 | 52.56 | NR | 12 | 100.00 | DAA vs LA |
| Taunton et al[88], 2018 | United States | 64.51 | 29.48 | 51.00 | NR | 52 | 100.00 | DAA vs PA |
| Brismar et al[55], 2018 | Sweden | 66.75 | 26.88 | 35.00 | 1.61 | NR | 51.00 | DAA vs LA |
| Reichert et al[81], 2018 | Germany | 62.58 | 28.20 | NR | NR | NR | 100.00 | DAA vs LA |
| Takada et al[86], 2018 | Japan | 62.60 | 24.40 | 13.33 | NR | NR | 100.00 | DAA vs LA |
| Xie et al[93], 2017 | China | 65.54 | 23.84 | 66.30 | NR | 52 | 100.00 | DSA/SuperPath vs PA |
| Cheng et al[57], 2017 | Australia | 61.28 | 28.01 | 45.20 | 1.96 | 12 | 100.00 | DAA vs PA |
| Xu et al[94], 2017 | China | 58.27 | 24.49 | 60.92 | NR | NR | NR | DAA vs PA |
| Nistor et al[77], 2017 | Romania | 63.75 | 28.04 | 40.00 | NR | NR | 100.00 | DAA vs LA |
| Rosenlund et al[83], 2017 | Denmark | 61.03 | 27.51 | 65.00 | 1.32 | 52 | NR | LA vs PA |
| Rykov et al[85], 2017 | Netherlands | NR | NR | NR | NR | NR | 84.80 | DAA vs PA |
| Zhao et al[96], 2017 | China | 63.53 | NR | NR | NR | NR | NR | DAA vs PA |
| Anta-Díaz et al[59], 2016 | Spain | 64.14 | 26.75 | 52.52 | NR | 52 | 100.00 | DAA vs LA |
| Parvizi et al[79], 2016 | United States | NR | NR | NR | NR | NR | 100.00 | DAA vs LA |
| Luo et al[69], 2016 | China | NR | NR | NR | NR | NR | NR | LA vs PA |
| Christensen et al[58], 2015 | United States | 64.71 | 30.78 | 47.10 | NR | NR | NR | DAA vs PA |
| Mjaaland et al[74], 2015 | Norway | 66.42 | 27.65 | 33.50 | 1.85 | NR | 100.00 | DAA vs LA |
| Vicente et al[90], 2015 | Brazil | 55.94 | 27.38 | 55.36 | NR | 24 | 52.68 | LA vs PA |
| Dienstknecht et al[61], 2014 | Germany | 61.53 | 29.14 | 44.06 | 2.26 | NR | 100.00 | DAA vs LA |
| Taunton et al[87], 2014 | United States | 64.23 | 28.45 | 46.30 | NR | 52 | NR | DAA vs PA |
| Landgraeber et al[66], 2013 | Germany | 70.66 | 26.90 | 34.21 | 2.06 | 156 | 100.00 | LMIS vs LA |
| Barrett et al[53], 2013 | United States | 62.31 | 29.89 | 55.20 | NR | 52 | NR | DAA vs PA |
| Ji et al[65], 2012 | S. Korea | 51.49 | 24.30 | 57.10 | NR | 150 | 37.20 | LA vs PA |
| Martin et al[70], 2011 | Belgium | 64.92 | 30.00 | 31.33 | 2.14 | 52 | Most | LMIS vs LA |
| Goosen et al[63], 2011 | Netherlands | 62.00 | 26.45 | 48.30 | NR | NR | NR | LA vs PA |
| Pospischill et al[80], 2010 | Austria | 61.25 | 25.70 | 50.00 | NR | 12 | 100.00 | LMIS vs LA |
| Yang et al[95], 2010 | China | 57.78 | 22.77 | 50.91 | NR | NR | 20 | LA vs PA |
| Della Valle et al[60], 2010 | United States | 62.46 | 27.45 | 31.90 | 2.06 | NR | 100.00 | 2-incision vs PA |
| Restrepo et al[82], 2010 | United States | 59.95 | 25.18 | 39.39 | 2.13 | NR | NR | DAA vs LA |
| Mayr et al[71], 2009 | Switzerland | 68.02 | 27.99 | 42.42 | NR | NR | NR | DAA vs LA |
| Meneghini et al[72], 2009 | United States | 54.00 | 26.00 | NR | NR | NR | NR | 2-incision vs LA vs PA |
| Witzleb et al[92], 2009 | Germany | 55.88 | 27.75 | 48.33 | NR | 12 | 56.70 | LA vs PA |
| Yan et al[89], 2017 | China | 65.42 | 23.97 | 46.10 | NR | 60 | NR | SuperPath vs LA |
| Yuan et al[64], 2018 | China | 75.03 | 22.54 | 55.56 | NR | 72 | NR | SuperPath vs PA |
| Dongwei et al[62], 2016 | China | 58.21 | NR | NR | NR | 12 | 100.00 | SuperPath vs LA |
Among 47 RCTs, most studies were low risk of bias for random sequence generation (89.4%), allocation concealment (36.2%), blinding of participants (29.8%), blinding outcome assessment (46.8%), incomplete outcome of data (40.4%), and selective outcome reporting (85.1%) (Figure 2, Supplementary Table 3). The ROBIS results from multiple reviews is shown in Figure 3.
Primary outcomes: According to functional outcomes, DAA significantly yielded the highest HHS at three months when compared with PA and LA (USMD: 2.79, 95%CI: 1.03, 4.55; and USMD: 3.76, 95%CI: 1.67, 5.85, respectively). There was no clinically significant difference of HHS at six months (DAA vs LA) and one year (DAA vs PA, DAA vs LA). All pairwise comparisons between hip approaches revealed no statistically significant dislocation and intraoperative fracture rate (Supplementary Tables 4 and 5).
Secondary outcomes: DSA/SuperPath and DAA had significant longer operative time than PA (18.55 min, 95%CI: 4.84, 32.27; and 17.17 min, 95%CI: 10.91, 23.42, respectively). DAA allowed shorter length of hospital stays than PA and LA (-0.39 d, 95%CI: -0.57, -0.21; and -0.57 d, 95%CI: -1.02, -0.11, orderly). Incision lengths of DAA and DSA/SuperPath were significantly shorter than PA (USMD: -2.2; 95%CI: -4.21, -0.19; and USMD: -4.38, 95%CI: -5.61, -3.16, respectively). Furthermore, DAA also had significantly shorter incision length than LA with USMD of -1.27 (95%CI: -2.22, -0.33).
Among, the newer techniques (DAA and DSA/SuperPath) DAA encountered with higher operative blood loss than PA with USMD of 52.02 mL (95%CI: 3.77, 100.27), but DSA yielded a better result when compared to PA with USMD of -17.54 mL (-66.09, 31.01). DAA significantly increased nerve injury when compared to PA with pooled RR 13.57 (95%CI: 3.17, 58.10). There was no significant nerve injury and wound complication rates among other treatment pairs (Supplementary Tables 4 and 5).
Heterogeneity was detected and explored for source of heterogeneity (Supplementary Table 6). Funnel plots and countour enhanced funnel plot were constructed (Supplementary Figure 1).
Network maps were constructed according to the interventions and outcomes (Figure 4).
Primary outcomes: DAA significantly demonstrated higher HHS at three months and one year than PA (pooled USMD: 3.49, 95%CI: 0.98, 6.00; and pooled USMD: 1.76, 95%CI: 1,12, 2.40, respectively). DAA also contributed higher HHS at one year when compared to 2-incisions, DSA/SuperPath, LA, and PA with pooled USMDs 3.70 (95%CI: 0.62, 6.78), 1.34 (95%CI: 0.39, 2.29), 1.17 (95%CI: 0.20, 2.14), and 1.76 (95%CI: 1.12, 2.40), respectively (Table 3).
| Risk ratio/unstandardized mean difference (95%CI) | ||||||
| PA | LA | DAA | 2-incision | LMIS | DSA/SuperPath | |
| HHS ≤ 3 mo | ||||||
| PA | [27.4; 0.0] | 0.74 (-2.24, 3.72) | 3.49 (0.98, 6.00) | 0.83 (-7.50, 9.16) | 0.02 (-10.13, 10.17) | 1.57 (-1.55, 4.69) |
| LA | -0.74 (-3.72, 2.24) | [42.7; 0.5] | 2.75 (-0.02, 5.52) | 0.09 (-8.64, 8.81) | -0.72 (-10.43, 8.99) | 0.83 (-2.91, 4.57) |
| DAA | -3.49 (-6.00, | -2.75 (-5.52, 0.02) | [85.9; 47.5] | -2.66 (-11.31, 5.99) | -3.47 (-13.56, 6.63) | -1.92 (-5.67, 1.83) |
| 2-incision | -0.81 (-13.86, 12.24) | -0.09 (-8.81, 8.64) | 2.66 (-5.99, 11.31) | [45.5; 20.7] | -0.81 (-13.86, 12.24) | 0.74 (-8.12, 9.61) |
| LMIS | -0.02 (-10.17, 10.13) | 0.72 (-8.99, 10.43) | 3.47 (-6.63, 13.56) | 0.81 (-12.24, 13.86) | [41.0; 22.1] | 1.55 (-8.85, 11.95) |
| DSA/SuperPath | -1.57 (-4.69, 1.55) | -0.83 (-4.57, 2.91) | 1.92 (-1.83, 5.67) | -0.74 (-9.61, 8.12) | -1.55 (-11.95, 8.85) | [57.6; 9.2] |
| HHS 6 mo | ||||||
| PA | [42.2; 3.0] | -0.21 (-1.67, 1.25) | 0.22 (-0.95, 1.39) | 1.85 (-14.14, 17.84) | NR | 0.35 (-0.84, 1.53) |
| LA | 0.21 (-1.25, 1.67) | [33.2; 4.1] | 0.43 (-1.50, 2.36) | 2.06 (-13.94, 18.05) | NR | 0.55 (-0.88, 1.98) |
| DAA | -0.22 (-1.39, 0.95) | -0.43 (-2.36, 1.50) | [55.9; 19.3] | 1.63 (-14.41, 17.67) | NR | 0.13 (-1.62, 1.87) |
| 2-incision | -1.85 (-17.84, 14.14) | -2.06 (-18.05, 13.94) | -1.63 (-17.67, 14.41) | [57.6; 55.2] | NR | -1.50 (-17.52, 14.51) |
| LMIS | NR | NR | NR | NR | NR | NR |
| DSA/SuperPath | -0.35 (-1.53, 0.84) | -0.55 (-1.98, 0.88) | -0.13 (-1.87, 1.62) | 1.50 (-14.51, 17.52) | NR | [61.1; 18.4] |
| HHS 1 yr | ||||||
| PA | [27.5; 0.0] | 0.60 (-0.55, 1.74) | 1.76 (1.12, 2.40) | -1.93 (-4.95, 1.08) | 1.43 (-2.16, 5.02) | 0.42 (-0.28, 1.12) |
| LA | -0.60 (-1.74, 0.55) | [54.8; 0.0] | 1.17 (0.20, 2.14) | -2.53 (-5.75, 0.69) | 0.83 (-2.57, 4.23) | -0.18 (-1.52, 1.17) |
| DAA | -1.76 (-2.40, | -1.17 (-2.14, | [90.7; 55.4] | -3.70 (-6.78, -0.62) | -0.34 (-3.87, 3.20) | -1.34 (-2.29, -0.39) |
| 2-incision | 1.93 (-1.08, 4.95) | 2.53 (-0.69, 5.75) | 3.70 (0.62, 6.78) | [6.0; 0.6] | 3.36 (-1.32, 8.04) | 2.35 (-0.74, 5.45) |
| LMIS | -1.43 (-5.02, 2.16) | -0.83 (-4.23, 2.57) | 0.34 (-3.20, 3.87) | -3.36 (-8.04, 1.32) | [70.8; 43.7] | -1.01 (-4.66, 2.65) |
| DSA/SuperPath | -0.42 (-1.12, 0.28) | 0.18 (-1.17, 1.52) | 1.34 (0.39, 2.29) | -2.35 (-5.45, 0.74) | 1.01 (-2.65, 4.66) | [50.2; 0.3] |
| Dislocation | ||||||
| PA | [50.8; 8.6] | 1.01 (0.34, 2.97) | 0.90 (0.52, 1.57) | NR | 1.00 (0.08, 11.81) | 1.28 (0.29, 5.57) |
| LA | 0.99 (0.34, 2.94) | [49.8; 15.2] | 0.90 (0.29, 2.74) | NR | 0.99 (0.11, 9.14) | 1.27 (0.20, 7.90) |
| DAA | 1.11 (0.64, 1.92) | 1.11 (0.37, 3.40) | [61.5; 21.9] | NR | 1.11 (0.09, 13.27) | 1.41 (0.29, 6.82) |
| 2-incision | NR | NR | NR | NR | NR | NR |
| LMIS | 1.00 (0.08, 11.85) | 1.01 (0.11, 9.28) | 0.90 (0.08, 10.85) | NR | [50.9; 37.3] | 1.28 (0.07, 22.70) |
| DSA/SuperPath | 0.78 (0.18, 3.42) | 0.79 (0.13, 4.90) | 0.71 (0.15, 3.41) | NR | 0.78 (0.04, 13.88) | [37.2; 17.0] |
| Intra-operative fracture | ||||||
| PA | [67.3; 17.2] | 1.33 (0.49, 3.58) | 0.96 (0.36, 2.57) | 1.84 (0.19, 18.35) | 2.19 (0.22, 21.84) | 1.75 (0.37, 8.35) |
| LA | 0.75 (0.28, 2.02) | [49.0; 6.6] | 0.72 (0.26, 1.95) | 1.39 (0.12, 15.36) | 1.65 (0.21, 13.12) | 1.31 (0.21, 8.36) |
| DAA | 1.05 (0.39, 2.82) | 1.39 (0.51, 3.78) | [70.7; 30.3] | 1.93 (0.17, 22.48) | 2.29 (0.23, 22.94) | 1.83 (0.29, 11.65) |
| 2-incision | 0.54 (0.05, 5.39) | 0.72 (0.07, 8.00) | 0.52 (0.04, 6.03) | [41.5; 19.9] | 1.19 (0.05, 28.49) | 0.95 (0.06, 15.27) |
| LMIS | 0.46 (0.05, 4.55) | 0.61 (0.08, 4.84) | 0.44 (0.04, 4.36) | 0.84 (0.04, 20.20) | [33.6; 15.1] | 0.80 (0.05, 12.88) |
| DSA/SuperPath | 0.57 (0.12, 2.73) | 0.76 (0.12, 4.84) | 0.55 (0.09, 3.47) | 1.05 (0.07, 16.97) | 1.25 (0.08, 20.20) | [37.9; 10.9] |
DAA was the best rank of HHS at three and twelve months with the SUCRAs of 85.9 and 90.7, respectively. Whereas at 6 mo, DSA was the best rank with the SUCRAs of 61.1. Six approaches demonstrated non-significant difference in dislocation and intraoperative fracture rates. The lowest dislocation rate was found in DAA (SUCRA: 61.5) followed by LMIS (SUCRA: 50.9) and the lowest intraoperative fracture rate was from DAA (SUCRA: 70.7) followed by PA (SUCRA: 67.3).
SUCRAs of benefit in improving HHS and risk in dislocation and fracture, indicated that DAA was the highest in HHS, dislocation and intra-operative fractures. PA was the worst in HHS with the third rank of dislocation and the second rank of intraoperative fracture.
Secondary outcomes: The newer techniques, LA, DAA, LMIS and DSA/SuperPath, took significantly longer operative time than the conventional PA with USMD of 10.38 (2.04, 18.71) min, 15.38 (8.64, 22.12) min, 23.86 (4.25, 43.47) min, and 18.74 (9.69, 27.79) min, respectively. In contrast, among the newer techniques, DSA took significantly shorter length of hospital stay than other approaches except for LMIS with USMD of -1.67 (-3.28, -0.06) d, -1.36 (-2.36, -0.35) d, -2.08 (-3.12, -1.04) d, and -1.56 (-2.44, -0.69) d when compared with 2-incisions, DAA, LA and PA, respectively.
For incision length, DSA/SuperPath was the shortest and PA was the longest one. Conversely, operative blood loss was higher among the newer techniques without statistical significance. Regarding to the complications, LMIS tended to have the highest wound infection rate. The 2-incisions and DAA had significantly more nerve injury rate than PA with USMDs of 18.97 (2.41, 149.62) and 9.82 (3.06, 31.58). Moreover, DAA was -1.35 (95%CI: -2.55, -0.14) and -0.70 (95%CI:
| Risk ratio/Unstandardized mean difference (95%CI) | ||||||
| PA | LA | DAA | 2 incisions | LMIS | DSA/SuperPath | |
| Operative time | ||||||
| PA | [98.6; 93.2] | 10.38 (2.04, 18.71) | 15.38 (8.64, 22.12) | 21.00 (-4.27, 46.27) | 23.86 (4.25, 43.47) | 18.74 (9.69, 27.79) |
| LA | -10.38 (-18.71, | [70.7; 0.7] | 5.01 (-2.66, 12.68) | 10.62 (-15.99, 37.24) | 13.49 (-4.26, 31.23) | 8.36 (-3.12, 19.84) |
| DAA | -15.38 (-22.12, | -5.01 (-12.68, 2.66) | [46.0; 0.0] | 5.62 (-20.54, 31.78) | 8.48 (-10.86, 27.81) | 3.35 (-7.58, 14.29) |
| 2-incision | -21.00 (-46.27, | -10.62 (-37.24, 15.99) | -5.62 (-31.78, 20.54) | [33.8; 5.3] | 2.86 (-29.13, 34.85) | -2.26 (-29.11, 24.58) |
| LMIS | -23.86 (-43.47, | -13.49 (-31.23, 4.26) | -8.48 (-27.81, 10.86) | -2.86 (-34.85, 29.13) | [19.6; 0.8] | -5.12 (-26.26, 16.01) |
| DSA/SuperPath | -18.74 (-27.79, | -8.36 (-19.84, 3.12) | -3.35 (-14.29, 7.58) | 2.26 (-24.58, 29.11) | 5.12 (-16.01, 26.26) | [31.4; 0.0] |
| Length of hospital stay | ||||||
| PA | [45.5; 0.0] | 0.52 (-0.36, 1.39) | -0.21 (-0.84, 0.43) | 0.11 (-1.29, 1.51) | 0.32 (-2.12, 2.76) | -1.56 (-2.44, -0.69) |
| LA | -0.52 (-1.39, 0.36) | [16.9; 0.0] | -0.72 (-1.52, 0.07) | -0.41 (-1.92, 1.10) | -0.20 (-2.48, 2.08) | -2.08 (-3.12, -1.04) |
| DAA | 0.21 (-0.43, 0.84) | 0.72 (-0.07, 1.52) | [61.3; 0.7] | 0.31 (-1.17, 1.80) | 0.52 (-1.89, 2.94) | -1.36 (-2.36, -0.35) |
| 2-incision | -0.11 (-1.51, 1.29) | 0.41 (-1.10, 1.92) | -0.31 (-1.80, 1.17) | [42.6; 3.0] | 0.21 (-2.52, 2.94) | -1.67 (-3.28, -0.06) |
| LMIS | -0.32 (-2.76, 2.12) | 0.20 (-2.08, 2.48) | -0.52 (-2.94, 1.89) | -0.21 (-2.94, 2.52) | [35.8; 6.3] | -1.88 (-4.38, 0.62) |
| DSA/SuperPath | 1.56 (0.69, 2.44) | 2.08 (1.04, 3.12) | 1.36 (0.35, 2.36) | 1.67 (0.06, 3.28) | 1.88 (-0.62, 4.38) | [97.9; 90.0] |
| Incision length | ||||||
| PA | [4.0; 0.0] | -1.53 (-3.86, 0.81) | -2.54 (-4.64, -0.45) | NR | -3.42 (-7.99, 1.16) | -5.15 (-7.29, -3.01) |
| LA | 1.53 (-0.81, 3.86) | [31.1; 0.0] | -1.02 (-3.00, 0.96) | NR | -1.89 (-5.82, 2.04) | -3.62 (-6.52, -0.72) |
| DAA | 2.54 (0.45, 4.64) | 1.02 (-0.96, 3.00) | [55.4; 1.8] | NR | -0.87 (-5.27, 3.53) | -2.60 (-5.45, 0.24) |
| 2-incision | NR | NR | NR | NR | NR | NR |
| LMIS | 3.42 (-1.16, 7.99) | 1.89 (-2.04, 5.82) | 0.87 (-3.53, 5.27) | NR | [66.5; 24.5] | -1.73 (-6.62, 3.16) |
| DSA/SuperPath | 5.15 (3.01, 7.29) | 3.62 (0.72, 6.52) | 2.60 (-0.24, 5.45) | NR | 1.73 (-3.16, 6.62) | [92.9; 73.7] |
| Operative blood loss | ||||||
| PA | [61.6; 10.7] | -25.66 (-117.26, 65.95) | 23.03 (-56.18, 102.24) | 46.00 (-185.02, 277.02) | 59.67 (-177.38, 296.72) | 23.02 (-56.58, 102.62) |
| LA | 25.66 (-65.95, 117.26) | [75.9; 35.1] | 48.69 (-47.77, 145.15) | 71.66 (-176.86, 320.18) | 85.33 (-133.30, 303.96) | 48.68 (-62.19, 159.55) |
| DAA | -23.03 (-102.24, 56.18) | -48.69 (-145.15, 47.77) | [44.0; 5.6] | 22.97 (-221.26, 267.19) | 36.64 (-202.33, 275.61) | -0.01 (-108.84, 108.82) |
| 2-incision | -46.00 (-277.02, 185.02) | -71.66 (-320.18, 176.86) | -22.97 (-267.19, 221.26) | [41.9; 24.3] | 13.67 (-317.33, 344.68) | -22.98 (-267.33, 221.37) |
| LMIS | -59.67 (-296.72, 177.38) | -85.33 (-303.96, 133.30) | -36.64 (-275.61, 202.33) | -13.67 (-344.68, 317.33) | [34.4; 17.5] | -36.65 (-281.79, 208.49) |
| DSA/SuperPath | -23.02 (-102.62, 56.58) | -48.68 (-159.55, 62.19) | 0.01 (-108.82, 108.84) | 22.98 (-221.37, 267.33) | 36.65 (-208.49, 281.79) | [42.2; 6.8] |
| Wound complication | ||||||
| PA | [70.0; 16.2] | 2.26 (0.72, 7.06) | 1.31 (0.59, 2.88) | 0.80 (0.04, 18.03) | 5.45 (0.60, 49.61) | 1.00 (0.15, 6.79) |
| LA | 0.44 (0.14, 1.38) | [31.0; 0.9] | 0.58 (0.18, 1.87) | 0.36 (0.02, 7.11) | 2.41 (0.36, 16.00) | 0.44 (0.05, 4.11) |
| DAA | 0.77 (0.35, 1.69) | 1.73 (0.53, 5.62) | [54.8; 5.2] | 0.62 (0.03, 14.29) | 4.18 (0.45, 38.77) | 0.77 (0.10, 6.09) |
| 2-incision | 1.24 (0.06, 27.95) | 2.81 (0.14, 56.24) | 1.62 (0.07, 37.72) | [68.8; 46.2] | 6.79 (0.20, 234.54) | 1.24 (0.03, 48.08) |
| LMIS | 0.18 (0.02, 1.67) | 0.41 (0.06, 2.75) | 0.24 (0.03, 2.22) | 0.15 (0.00, 5.09) | [12.5; 1.3] | 0.18 (0.01, 3.41) |
| DSA/SuperPath | 1.00 (0.15, 6.79) | 2.26 (0.24, 20.99) | 1.31 (0.16, 10.38) | 0.80 (0.02, 31.03) | 5.45 (0.29, 101.44) | [62.8; 30.2] |
| Nerve injury | ||||||
| PA | [79.7; 25.6] | 2.97 (0.89, 9.97) | 9.82 (3.06, 31.58) | 18.97 (2.41, 149.62) | 1.08 (0.11, 10.20) | 1.00 (0.02, 49.35) |
| LA | 0.34 (0.10, 1.13) | [49.4; 0.5] | 3.30 (1.22, 8.94) | 6.38 (0.81, 50.31) | 0.36 (0.05, 2.41) | 0.34 (0.01, 19.93) |
| DAA | 0.10 (0.03, 0.33) | 0.30 (0.11, 0.82) | [17.9; 0.0] | 1.93 (0.22, 16.92) | 0.11 (0.01, 0.93) | 0.10 (0.00, 5.96) |
| 2-incision | 0.05 (0.01, 0.42) | 0.16 (0.02, 1.24) | 0.52 (0.06, 4.54) | [9.0; 0.2] | 0.06 (0.00, 0.94) | 0.05 (0.00, 4.35) |
| LMIS | 0.93 (0.10, 8.81) | 2.76 (0.41, 18.42) | 9.13 (1.07, 77.77) | 17.63 (1.07, 291.08) | [75.1; 31.9] | 0.93 (0.01, 83.77) |
| DSA/SuperPath | 1.00 (0.02, 49.35) | 2.97 (0.05, 176.30) | 9.82 (0.17, 575.31) | 18.97 (0.23, 1564.11) | 1.08 (0.01, 97.00) | [69.0; 41.8] |
The first and the second probability of being the best interventions were as follows: Operative time (PA and LA), length of hospital stay (DSA/SuperPath and DAA), incision length (DSA/SuperPath and LMIS), operative blood loss (LA and PA), wound complication (PA and 2-incisions), and nerve injury (PA and LMIS). Benefit in raising HHS and risks of operative outcomes were simultaneously plotted. A clustered ranking plot was constructed for comparing overall complications and early functional outcome of each approach (Figure 5).
Adjusted funnel plots showed no evidence of asymmetry except the results of HHS at twelve weeks, length of hospital stays and incision length (Supplementary Figure 2). No evidence of inconsistency assumption was found among direct MA and NMA except those in HHS at six months, and incision length (Supplementary Table 7).
This umbrella review summarized the findings of multiple MAs comparing each THA approach in terms of efficacy and complications. DAA was the highest rank for HHS, dislocation and intra-operative fractures. DSA/SuperPath might be beneficial for short incision length and length of hospital stay. PA diminished operative blood loss and operative time. On the other hand, PA was the worst in HHS with the third rank of dislocation and the second rank of intraoperative fracture.
For primary outcomes, HHS, which is the clinician-based outcome measure frequently used to evaluate patients following a THA, showed advantages in DAA from most of the previous MAs[30,34,44,98]. The results of this study re-pooled RCTs after adding DSA/SuperPath, the newest technique, showed that DAA remained in the first ranking without statistical significance from the second rank DSA/SuperPath. Even though DAA was significantly higher HHS at three months than PA (USMD: 3.49, 95%CI: 0.98, 6.00), the differences did not meet the minimally clinical significance (15.9-18.0 points)[99]. Positive properties of DAA in functional outcomes may be explained by: (1) The approach through tensor fascia lata and sartorius interval without muscle dissection; (2) preserved posterior soft tissue; (3) less muscle damage supported by low level of creatinine kinase and inflammatory responses [Interleukin (IL): IL-6, IL-8, IL-10, and tumor necrotic factor (TNF)] as well as good soft tissue response in magnetic resonance imaging[59]; (4) less post-operative pain, excellent cadence, pelvic tilt and sagittal balance[96]; and (5) good recovery outcomes with unnecessary for physical therapy[74]. DSA/SuperPath preserved the gluteus minimus and tensor fasciae latae muscles[17,16]. This could promote post-operative ambulatory and functional status[16]. Without a learning curve, DSA allowed good prosthesis positioning and comparable functional outcomes to the mini-posterolateral hip approach[16].
For dislocation rate, which is the most common complication of THA, especially in PA, DAA still provided the best result without significant difference from other approaches. Its effects in prevention of hip dislocation are from: (1) The supine position allows anatomical pelvic alignment and precise acetabular cup positioning[96]; and (2) fluoroscopic guidance supports cup and stem placement and preserves posterior soft tissue. LMIS was the second rank for hip dislocation. This method avoids muscular detachment by approaching between the tensor fascia lata and gluteus medius. Preservation of the gluteus medius would preclude Trendelenburg gait, secure good hip function[66,70,80], and might prevent hip dislocation.
Lastly, the intra-operative fracture rate showed disadvantages in DAA from most of the previous MAs studies[28,30,37]. The results from this study re-pooled RCTs stated in the opposite way. DAA became the first rank in lowering intra-operative fracture rate instead of PA. This could be surgeon’s experience or familiarity with DAA to prevent fracture complication. DAA required performer’s experience of at least 60-100 cases to achieve optimal operative time, blood loss, and acceptable complications[100-102]. Mastery in this technique may help in femoral canal broaching and component application to prevent intra-operative fracture. PA was the second rank for intra-operative fracture such as one calcar crack[53]. DSA/SuperPath still had higher rate of intra-operative fracture than DAA and PA without statistical significance. DSA/SuperPath may cause intra-operative fracture from limited proximal femoral exposure, and is unsuitable for proximal femoral deformity[17].
For secondary outcomes, previous MAs show pros and cons between DAA and PA. DAA was better in terms of short length of hospital stay, incision length and decreased VAS pain. The downsides were raised nerve injury rate, operative time, and operative blood loss. Nerve injury can be avoided by: (1) Placing the incision more lateral than a traditional sartorius/tensor fascia lata interval; and (2) carefully performing fascial and subcutaneous layer closures to preclude the lateral femoral cutaneous nerve entrapment[103]. High blood loss was associated with long operation time[56]. Prolonged operative time and high blood loss may be caused by: (1) The fracture table and fluoroscopic set up time; (2) posterior capsular bleeding due to limited visualization; and (3) stretching and detaching the tensor fascia lata in MIS technique[85]. However, some studies[35,36,44] reported insignificantly different complications from other techniques. The results of this study re-pooled RCTs, which showed DSA/SuperPath allowed more advantages over PA, and could diminish length of hospital stay, incision length, wound complication and nerve injury rate more than DAA. For operative blood loss, DSA/SuperPath tended to have better results than DAA, but could not overcome PA. Even though SuperPath required shorter incision length than PA, soft tissue injury and long operative time contributed to high blood loss[19].
This study has strengths in many aspects. First, this study summarized all MAs assessing hip approaches in terms of efficacy and complications. The recently proposed DSA/SuperPath was considered and ranked in the analysis. In addition, this study also re-pooled data and updated new studies since the last MAs in 2023 and added RBA. All included studies were RCTs, the best available evidences with good quality (low risk of biases). However, limitations could not be avoided. The quality assessment of included MAs and RCTs indicated that some included RCTs were at high risk of bias. The results cannot be considered as independent set of evidence due to high degree of overlap with CCA of 11.0%-15.0% (14.9%). Exclusion of mini-posterior and modified posterior techniques precluded evaluation of the results among these approaches.
For clinical application, the best approaches regarding the primary outcome and the major complication were DAA, followed by DSA/SuperPath with lower overall complication rate (Figure 5). Surgeons need to select according to their familiarity. For training program, the DAA and DSA/SuperPath techniques are recommended. Lastly, DSA/SuperPath might be the good choice for surgeons who are familiar with PA in order to achieve better outcomes and reduce major complications. Furthermore, DSA/SuperPath is another choice of MIS technique for surgeons who are not familiar in anterior direction, which can lead to many problems such as infection[104] or vascular injury[105,106]. Also, DSA has been reported as “no learning curve” compared to mini-PA[16].
This umbrella review and updated re-pooling date from RCTs published indicate that DSA/SuperPath which is the newest technique has better functional outcome (HHS) than PA, but still cannot overcome the result of DAA. In terms of complications, it is still in the middle between PA and DAA. Future study should be conducted to update the information of DSA/SuperPath and directly compare with DAA and PA.
Various hip approaches have been proposed for total hip arthroplasty. Many systematic reviews and meta-analysis (MAs) reported their benefits for hip function, and pain relief. The disadvantages, such as hip dislocation, intra-operative fracture, blood loss, and nerve injury, depended on types of surgical techniques. This is the first umbrella review comprehensively compared six approaches including direct anterior (DAA), direct superior (DSA)/supercapsular percutaneously-assisted total hip (SuperPath), lateral (LA), mini-lateral (LMIS), 2-incision, and posterior approach (PA) techniques.
Comparisons of different hip approaches, particularly DSA/SuperPath to PA in terms of important clinical outcomes and complications have not yet been in previous network MAs.
To compare hip approaches including DAA, DSA/SuperPath, LA, LMIS, 2-incision, and PA. The best approach is determined by constructing cluster ranking plots between benefits of Harris Hip Score (HHS), and risks of hip dislocation, intra-operative fracture, wound complication, and nerve injury.
MA and updated randomized controlled trials (RCTs) were identified from large two databases (MEDLINE and Scopus) up to year 2023. Two evaluators independently assessed the quality, and extracted data from included studies comparing hip approaches, and reporting at least one outcomes of interest. This review was performed with robust methodology by re-pooling data, network MA, surface under cumulative ranking curve, corrected covered area for overlapping studies, and publication bias assessment.
Considering HHS, clinical important outcomes and complications, re-pooled 47 RCTs demonstrated DAA was the best hip approach followed by DSA/SuperPath. These evidences were from moderate quality RCTs without publication bias. High degree of CCA indicated overlapping between RCTs among previous MAs.
DSA/SuperPath provided good functional outcome in the middle between PA and DAA. Without learning curve, this approach might be useful for surgeons who are familiar to PA or inexperienced in DAA to avoid adverse outcomes.
Future study should be conducted to update the information of DSA/SuperPath and directly compare with DAA and PA.
The authors would like to thank Napaphat Poprom, Stephen Pinder, and Nattakrit Tongpoonsakdi from the Department of Clinical Epidemiology and Biostatistics, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand.
| 1. | Laupacis A, Bourne R, Rorabeck C, Feeny D, Wong C, Tugwell P, Leslie K, Bullas R. The effect of elective total hip replacement on health-related quality of life. J Bone Joint Surg Am. 1993;75:1619-1626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 424] [Cited by in RCA: 422] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 2. | Ammarullah MI, Hidayat T, Lamura MD, Jamari J. Relationship between deformation and running-in wear on hard-on-hard bearings from metal, ceramic, and diamond materials for total hip prosthesis. J Tribology. 2023;38:69. |
| 3. | Ammarullah MI, Santoso G, Gatot Santoso, Sugiharto S, Supriyono T, Kurdi O, Tauviqirrahman M, Winarni TI, Jamari J. Tresca stress study of CoCrMo-on-CoCrMo bearings based on body mass index using 2D computational model. J Tribology. 2022;33:31-38. |
| 4. | Hidayat T, Ismail R, Tauviqirrahman M, Saputra E, Ammarullah MI, Lamura MD, Bayuseno A, Jamari J. Investigation of mesh model for a finite element simulation of the dual-mobility prosthetic hip joint. J Tribology. 2023;38:118-1401. |
| 5. | Lee JM. The Current Concepts of Total Hip Arthroplasty. Hip Pelvis. 2016;28:191-200. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (1)] |
| 6. | Higgins BT, Barlow DR, Heagerty NE, Lin TJ. Anterior vs. posterior approach for total hip arthroplasty, a systematic review and meta-analysis. J Arthroplasty. 2015;30:419-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 285] [Article Influence: 25.9] [Reference Citation Analysis (0)] |
| 7. | Healy WL, Iorio R, Clair AJ, Pellegrini VD, Della Valle CJ, Berend KR. Complications of Total Hip Arthroplasty: Standardized List, Definitions, and Stratification Developed by The Hip Society. Clin Orthop Relat Res. 2016;474:357-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 165] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 8. | Jamari J, Ammarullah MI, Saad APM, Syahrom A, Uddin M, van der Heide E, Basri H. The Effect of Bottom Profile Dimples on the Femoral Head on Wear in Metal-on-Metal Total Hip Arthroplasty. J Funct Biomater. 2021;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 110] [Cited by in RCA: 86] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 9. | Salaha ZFM, Ammarullah MI, Abdullah NNAA, Aziz AUA, Gan HS, Abdullah AH, Abdul Kadir MR, Ramlee MH. Biomechanical Effects of the Porous Structure of Gyroid and Voronoi Hip Implants: A Finite Element Analysis Using an Experimentally Validated Model. Materials (Basel). 2023;16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 49] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 10. | Ammarullah MI, Hartono R, Supriyono T, Santoso G, Sugiharto S, Permana MS. Polycrystalline Diamond as a Potential Material for the Hard-on-Hard Bearing of Total Hip Prosthesis: Von Mises Stress Analysis. Biomedicines. 2023;11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 67] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
| 11. | Jamari J, Ammarullah MI, Santoso G, Sugiharto S, Supriyono T, van der Heide E. In Silico Contact Pressure of Metal-on-Metal Total Hip Implant with Different Materials Subjected to Gait Loading. Metals. 2022;12:1241. [RCA] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 49] [Article Influence: 12.3] [Reference Citation Analysis (1)] |
| 12. | Ammarullah MI, Afif IY, Maula MI, Winarni TI, Tauviqirrahman M, Akbar I, Basri H, van der Heide E, Jamari J. Tresca Stress Simulation of Metal-on-Metal Total Hip Arthroplasty during Normal Walking Activity. Materials (Basel). 2021;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 132] [Cited by in RCA: 92] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 13. | Jamari J, Ammarullah MI, Santoso G, Sugiharto S, Supriyono T, Permana MS, Winarni TI, van der Heide E. Adopted walking condition for computational simulation approach on bearing of hip joint prosthesis: review over the past 30 years. Heliyon. 2022;8:e12050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 45] [Article Influence: 11.3] [Reference Citation Analysis (1)] |
| 14. | Moretti VM, Post ZD. Surgical Approaches for Total Hip Arthroplasty. Indian J Orthop. 2017;51:368-376. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 68] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 15. | Ki SC, Kim BH, Ryu JH, Yoon DH, Chung YY. Total hip arthroplasty using two-incision technique. Clin Orthop Surg. 2011;3:268-273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (1)] |
| 16. | Barrett AA, Ezzibdeh RM, Horst PK, Roger DJ, Amanatullah DF. Direct Superior Approach to the Hip for Total Hip Arthroplasty. JBJS Essent Surg Tech. 2019;9:e17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 17. | Quitmann H. Supercapsular percutaneously assisted (SuperPath) approach in total hip arthroplasty : Surgical technique and preliminary results. Oper Orthop Traumatol. 2019;31:536-546. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Ulivi M, Orlandini L, Vitale JA, Meroni V, Prandoni L, Mangiavini L, Rossi N, Peretti GM. Direct superior approach versus posterolateral approach in total hip arthroplasty: a randomized controlled trial on early outcomes on gait, risk of fall, clinical and self-reported measurements. Acta Orthop. 2021;92:274-279. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 19. | Meng W, Gao L, Huang Z, Wang H, Wang D, Luo Z, Bai Y, Wang G, Zhou Z. Supercapsular percutaneously-assisted total hip (SuperPath) versus mini-incision posterolateral total hip arthroplasty for hip osteoarthritis: a prospective randomized controlled trial. Ann Transl Med. 2021;9:392. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Ang JJM, Onggo JR, Stokes CM, Ambikaipalan A. Comparing direct anterior approach versus posterior approach or lateral approach in total hip arthroplasty: a systematic review and meta-analysis. Eur J Orthop Surg Traumatol. 2023;33:2773-2792. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 62] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 21. | Awad ME, Farley BJ, Mostafa G, Saleh KJ. Direct anterior approach has short-term functional benefit and higher resource requirements compared with the posterior approach in primary total hip arthroplasty: a meta-analysis of functional outcomes and cost. Bone Joint J. 2021;103-B:1078-1087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 22. | Cha Y, Yoo JI, Kim JT, Park CH, Choy W, Ha YC, Koo KH. Disadvantage during Perioperative Period of Total Hip Arthroplasty Using the Direct Anterior Approach: a Network Meta-Analysis. J Korean Med Sci. 2020;35:e111. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 23. | Chen W, Sun JN, Zhang Y, Chen XY, Feng S. Direct anterior versus posterolateral approaches for clinical outcomes after total hip arthroplasty: a systematic review and meta-analysis. J Orthop Surg Res. 2020;15:231. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 24. | Docter S, Philpott HT, Godkin L, Bryant D, Somerville L, Jennings M, Marsh J, Lanting B. Comparison of intra and post-operative complication rates among surgical approaches in Total Hip Arthroplasty: A systematic review and meta-analysis. J Orthop. 2020;20:310-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 25. | Gazendam A, Bozzo A, Ekhtiari S, Kruse C, Hiasat N, Tushinski D, Bhandari M. Short-term outcomes vary by surgical approach in total hip arthroplasty: a network meta-analysis. Arch Orthop Trauma Surg. 2022;142:2893-2902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 26. | Ge Y, Chen Z, Chen Q, Fu Y, Fan M, Li T, Shan L, Tong P, Zhou L. A Systematic Review and Meta-Analysis of the SuperPATH Approach in Hip Arthroplasty. Biomed Res Int. 2021;2021:5056291. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 27. | Huerfano E, Bautista M, Huerfano M, Nossa JM. Use of Surgical Approach Is Not Associated With Instability After Primary Total Hip Arthroplasty: A Meta-analysis Comparing Direct Anterior and Posterolateral Approaches. J Am Acad Orthop Surg. 2021;29:e1126-e1140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 28. | Jia F, Guo B, Xu F, Hou Y, Tang X, Huang L. A comparison of clinical, radiographic and surgical outcomes of total hip arthroplasty between direct anterior and posterior approaches: a systematic review and meta-analysis. Hip Int. 2019;29:584-596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 64] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 29. | Joseph VM, Nagy M; Board TN. Systematic review and meta-analysis on SuperPATH approach versus conventional approaches for hip arthroplasty. Hip Int. 2023;33:655-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 30. | Kucukdurmaz F, Sukeik M, Parvizi J. A meta-analysis comparing the direct anterior with other approaches in primary total hip arthroplasty. Surgeon. 2019;17:291-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 31. | Lazaru P, Bueschges S, Ramadanov N. Direct anterior approach (DAA) vs. conventional approaches in total hip arthroplasty: A RCT meta-analysis with an overview of related meta-analyses. PLoS One. 2021;16:e0255888. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 32. | Migliorini F, Trivellas A, Eschweiler J, Driessen A, Lessi F, Tingart M, Aretini P. Nerve palsy, dislocation and revision rate among the approaches for total hip arthroplasty: a Bayesian network meta-analysis. Musculoskelet Surg. 2021;105:1-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 33. | Migliorini F, Trivellas A, Eschweiler J, El Mansy Y, Mazzanti MC, Tingart M, Aretini P. Hospitalization length, surgical duration, and blood lost among the approaches for total hip arthroplasty: a Bayesian network meta-analysis. Musculoskelet Surg. 2020;104:257-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 34. | Miller LE, Gondusky JS, Bhattacharyya S, Kamath AF, Boettner F, Wright J. Does Surgical Approach Affect Outcomes in Total Hip Arthroplasty Through 90 Days of Follow-Up? A Systematic Review With Meta-Analysis. J Arthroplasty. 2018;33:1296-1302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 126] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 35. | Miller LE, Kamath AF, Boettner F, Bhattacharyya SK. In-hospital outcomes with anterior versus posterior approaches in total hip arthroplasty: meta-analysis of randomized controlled trials. J Pain Res. 2018;11:1327-1334. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 36. | Peng L, Zeng Y, Wu Y, Zeng J, Liu Y, Shen B. Clinical, functional and radiographic outcomes of primary total hip arthroplasty between direct anterior approach and posterior approach: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2020;21:338. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 37. | Putananon C, Tuchinda H, Arirachakaran A, Wongsak S, Narinsorasak T, Kongtharvonskul J. Comparison of direct anterior, lateral, posterior and posterior-2 approaches in total hip arthroplasty: network meta-analysis. Eur J Orthop Surg Traumatol. 2018;28:255-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 81] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 38. | Ramadanov N. An Updated Meta-Analysis of Randomized Controlled Trials on Total Hip Arthroplasty through SuperPATH versus Conventional Approaches. Orthop Surg. 2022;14:807-823. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 17] [Reference Citation Analysis (0)] |
| 39. | Ramadanov N, Bueschges S, Liu K, Lazaru P, Marintschev I. Comparison of short-term outcomes between direct anterior approach (DAA) and SuperPATH in total hip replacement: a systematic review and network meta-analysis of randomized controlled trials. J Orthop Surg Res. 2021;16:324. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 40. | Ramadanov N, Bueschges S, Liu K, Lazaru P, Marintschev I. Direct anterior approach vs. SuperPATH vs. conventional approaches in total hip replacement: A network meta-analysis of randomized controlled trials. Orthop Traumatol Surg Res. 2021;107:103058. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 41. | Ramadanov N, Bueschges S, Liu K, Lazaru P, Marintschev I. Direct and indirect comparisons in network meta-analysis of SuperPATH, direct anterior and posterior approaches in total hip arthroplasty. Sci Rep. 2022;12:16778. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 42. | Sun X, Zhao X, Zhou L, Su Z. Direct anterior approach versus posterolateral approach in total hip arthroplasty: a meta-analysis of results on early post-operative period. J Orthop Surg Res. 2021;16:69. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 43. | Wang Z, Bao HW, Hou JZ. Direct anterior versus lateral approaches for clinical outcomes after total hip arthroplasty: a meta-analysis. J Orthop Surg Res. 2019;14:63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 44. | Wang Z, Hou JZ, Wu CH, Zhou YJ, Gu XM, Wang HH, Feng W, Cheng YX, Sheng X, Bao HW. A systematic review and meta-analysis of direct anterior approach versus posterior approach in total hip arthroplasty. J Orthop Surg Res. 2018;13:229. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 155] [Article Influence: 19.4] [Reference Citation Analysis (0)] |
| 45. | Yang XT, Huang HF, Sun L, Yang Z, Deng CY, Tian XB. Direct Anterior Approach Versus Posterolateral Approach in Total Hip Arthroplasty: A Systematic Review and Meta-analysis of Randomized Controlled Studies. Orthop Surg. 2020;12:1065-1073. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 46. | Zhou Z, Li Y, Peng Y, Jiang J, Zuo J. Clinical efficacy of direct anterior approach vs. other surgical approaches for total hip arthroplasty: A systematic review and meta-analysis based on RCTs. Front Surg. 2022;9:1022937. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 47. | Miller LE, Gondusky JS, Kamath AF, Boettner F, Wright J, Bhattacharyya S. Influence of surgical approach on complication risk in primary total hip arthroplasty. Acta Orthop. 2018;89:289-294. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 70] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 48. | Yan L, Ge L, Dong S, Saluja K, Li D, Reddy KS, Wang Q, Yao L, Li JJ, Roza da Costa B, Xing D, Wang B. Evaluation of Comparative Efficacy and Safety of Surgical Approaches for Total Hip Arthroplasty: A Systematic Review and Network Meta-analysis. JAMA Netw Open. 2023;6:e2253942. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 48] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 49. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6253] [Cited by in RCA: 7872] [Article Influence: 463.1] [Reference Citation Analysis (3)] |
| 50. | Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737-755. [PubMed] |
| 51. | Whiting P, Savović J, Higgins JP, Caldwell DM, Reeves BC, Shea B, Davies P, Kleijnen J, Churchill R; ROBIS group. ROBIS: A new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. 2016;69:225-234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 718] [Cited by in RCA: 1463] [Article Influence: 133.0] [Reference Citation Analysis (0)] |
| 52. | Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA; Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18487] [Cited by in RCA: 26232] [Article Influence: 1748.8] [Reference Citation Analysis (4)] |
| 53. | Barrett WP, Turner SE, Leopold JP. Prospective randomized study of direct anterior vs postero-lateral approach for total hip arthroplasty. J Arthroplasty. 2013;28:1634-1638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 367] [Article Influence: 28.2] [Reference Citation Analysis (0)] |
| 54. | Bon G, Kacem EB, Lepretre PM, Weissland T, Mertl P, Dehl M, Gabrion A. Does the direct anterior approach allow earlier recovery of walking following total hip arthroplasty? A randomized prospective trial using accelerometry. Orthop Traumatol Surg Res. 2019;105:445-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 55. | Brismar BH, Hallert O, Tedhamre A, Lindgren JU. Early gain in pain reduction and hip function, but more complications following the direct anterior minimally invasive approach for total hip arthroplasty: a randomized trial of 100 patients with 5 years of follow up. Acta Orthop. 2018;89:484-489. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 56. | Cao J, Zhou Y, Xin W, Zhu J, Chen Y, Wang B, Qian Q. Natural outcome of hemoglobin and functional recovery after the direct anterior versus the posterolateral approach for total hip arthroplasty: a randomized study. J Orthop Surg Res. 2020;15:200. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 57. | Cheng TE, Wallis JA, Taylor NF, Holden CT, Marks P, Smith CL, Armstrong MS, Singh PJ. A Prospective Randomized Clinical Trial in Total Hip Arthroplasty-Comparing Early Results Between the Direct Anterior Approach and the Posterior Approach. J Arthroplasty. 2017;32:883-890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 136] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 58. | Christensen CP, Jacobs CA. Comparison of Patient Function during the First Six Weeks after Direct Anterior or Posterior Total Hip Arthroplasty (THA): A Randomized Study. J Arthroplasty. 2015;30:94-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 125] [Article Influence: 11.4] [Reference Citation Analysis (1)] |
| 59. | De Anta-Díaz B, Serralta-Gomis J, Lizaur-Utrilla A, Benavidez E, López-Prats FA. No differences between direct anterior and lateral approach for primary total hip arthroplasty related to muscle damage or functional outcome. Int Orthop. 2016;40:2025-2030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 60] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 60. | Della Valle CJ, Dittle E, Moric M, Sporer SM, Buvanendran A. A prospective randomized trial of mini-incision posterior and two-incision total hip arthroplasty. Clin Orthop Relat Res. 2010;468:3348-3354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 61. | Dienstknecht T, Lüring C, Tingart M, Grifka J, Sendtner E. Total hip arthroplasty through the mini-incision (Micro-hip) approach versus the standard transgluteal (Bauer) approach: a prospective, randomised study. J Orthop Surg (Hong Kong). 2014;22:168-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 62. | Wang XD, Lan H, Hu ZX, Li KN, Wang ZH, Luo J, Long XD. SuperPATH Minimally Invasive Approach to Total Hip Arthroplasty of Femoral Neck Fractures in the Elderly: Preliminary Clinical Results. Orthop Surg. 2020;12:74-85. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 63. | Goosen JH, Kollen BJ, Castelein RM, Kuipers BM, Verheyen CC. Minimally invasive versus classic procedures in total hip arthroplasty: a double-blind randomized controlled trial. Clin Orthop Relat Res. 2011;469:200-208. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 55] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 64. | Yuan H, Zhu J, Sun Z, Zhang Z. [Comparison of effectiveness between SuperPATH approach and posterolateral approach in total hip arthroplasty]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2018;32:14-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 65. | Ji HM, Kim KC, Lee YK, Ha YC, Koo KH. Dislocation after total hip arthroplasty: a randomized clinical trial of a posterior approach and a modified lateral approach. J Arthroplasty. 2012;27:378-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 73] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 66. | Landgraeber S, Quitmann H, Güth S, Haversath M, Kowalczyk W, Kecskeméthy A, Heep H, Jäger M. A prospective randomized peri- and post-operative comparison of the minimally invasive anterolateral approach versus the lateral approach. Orthop Rev (Pavia). 2013;5:e19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 67. | Li SL, Yang XT, Tian XB, Sun L. [Early functional recovery of direct anterior approach versus anterolateral approach for total hip arthroplasty]. Beijing Da Xue Xue Bao Yi Xue Ban. 2019;51:268-272. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 68. | Li X, Ma L, Wang Q, Rong K. Comparison of total hip arthroplasty with minimally invasive SuperPath approach vs. conventional posterolateral approach in elderly patients: A one-year follow-up randomized controlled research. Asian J Surg. 2021;44:531-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 69. | Luo ZL, Chen M, Shang XF, Hu F, Ni Z, Cheng P, Ji XF, Wu KR, Zhang XQ. [Direct anterior approach versus posterolateral approach for total hip arthroplasty in the lateral decubitus position]. Zhonghua Yi Xue Za Zhi. 2016;96:2807-2812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 70. | Martin R, Clayson PE, Troussel S, Fraser BP, Docquier PL. Anterolateral minimally invasive total hip arthroplasty: a prospective randomized controlled study with a follow-up of 1 year. J Arthroplasty. 2011;26:1362-1372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 56] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 71. | Mayr E, Nogler M, Benedetti MG, Kessler O, Reinthaler A, Krismer M, Leardini A. A prospective randomized assessment of earlier functional recovery in THA patients treated by minimally invasive direct anterior approach: a gait analysis study. Clin Biomech (Bristol, Avon). 2009;24:812-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 134] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 72. | Meneghini RM, Smits SA. Early discharge and recovery with three minimally invasive total hip arthroplasty approaches: a preliminary study. Clin Orthop Relat Res. 2009;467:1431-1437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 30] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 73. | Meng W, Huang Z, Wang H, Wang D, Luo Z, Bai Y, Gao L, Wang G, Zhou Z. Supercapsular percutaneously-assisted total hip (SuperPath) versus posterolateral total hip arthroplasty in bilateral osteonecrosis of the femoral head: a pilot clinical trial. BMC Musculoskelet Disord. 2019;21:2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 74. | Mjaaland KE, Kivle K, Svenningsen S, Pripp AH, Nordsletten L. Comparison of markers for muscle damage, inflammation, and pain using minimally invasive direct anterior versus direct lateral approach in total hip arthroplasty: A prospective, randomized, controlled trial. J Orthop Res. 2015;33:1305-1310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 80] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 75. | Moerenhout K, Derome P, Laflamme GY, Leduc S, Gaspard HS, Benoit B. Direct anterior versus posterior approach for total hip arthroplasty: a multicentre, prospective, randomized clinical trial. Can J Surg. 2020;63:E412-E417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 64] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 76. | Nistor DV, Bota NC, Caterev S, Todor A. Are physical therapy pain levels affected by surgical approach in total hip arthroplasty? A randomized controlled trial. Orthop Rev (Pavia). 2020;12:8399. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 77. | Nistor DV, Caterev S, Bolboacă SD, Cosma D, Lucaciu DOG, Todor A. Transitioning to the direct anterior approach in total hip arthroplasty. Is it a true muscle sparing approach when performed by a low volume hip replacement surgeon? Int Orthop. 2017;41:2245-2252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 78. | Ouyang C, Wang H, Meng W, Luo Z, Wang D, Pei F, Zhou Z. [Randomized controlled trial of comparison between the SuperPATH and posterolateral approaches in total hip arthroplasty]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2018;32:1500-1506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 79. | Parvizi J, Restrepo C, Maltenfort MG. Total Hip Arthroplasty Performed Through Direct Anterior Approach Provides Superior Early Outcome: Results of a Randomized, Prospective Study. Orthop Clin North Am. 2016;47:497-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 68] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 80. | Pospischill M, Kranzl A, Attwenger B, Knahr K. Minimally invasive compared with traditional transgluteal approach for total hip arthroplasty: a comparative gait analysis. J Bone Joint Surg Am. 2010;92:328-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 77] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 81. | Reichert JC, von Rottkay E, Roth F, Renz T, Hausmann J, Kranz J, Rackwitz L, Nöth U, Rudert M. A prospective randomized comparison of the minimally invasive direct anterior and the transgluteal approach for primary total hip arthroplasty. BMC Musculoskelet Disord. 2018;19:241. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 82. | Restrepo C, Parvizi J, Pour AE, Hozack WJ. Prospective randomized study of two surgical approaches for total hip arthroplasty. J Arthroplasty. 2010;25:671-9.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 201] [Article Influence: 12.6] [Reference Citation Analysis (1)] |
| 83. | Rosenlund S, Broeng L, Holsgaard-Larsen A, Jensen C, Overgaard S. Patient-reported outcome after total hip arthroplasty: comparison between lateral and posterior approach. Acta Orthop. 2017;88:239-247. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 84. | Rykov K, Meys TWGM, Knobben BAS, Sietsma MS, Reininga IHF, Ten Have BLEF. MRI Assessment of Muscle Damage After the Posterolateral Versus Direct Anterior Approach for THA (Polada Trial). A Randomized Controlled Trial. J Arthroplasty. 2021;36:3248-3258.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 85. | Rykov K, Reininga IHF, Sietsma MS, Knobben BAS, Ten Have BLEF. Posterolateral vs Direct Anterior Approach in Total Hip Arthroplasty (POLADA Trial): A Randomized Controlled Trial to Assess Differences in Serum Markers. J Arthroplasty. 2017;32:3652-3658.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 64] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 86. | Takada R, Jinno T, Miyatake K, Hirao M, Kimura A, Koga D, Yagishita K, Okawa A. Direct anterior versus anterolateral approach in one-stage supine total hip arthroplasty. Focused on nerve injury: A prospective, randomized, controlled trial. J Orthop Sci. 2018;23:783-787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 54] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 87. | Taunton MJ, Mason JB, Odum SM, Springer BD. Direct anterior total hip arthroplasty yields more rapid voluntary cessation of all walking aids: a prospective, randomized clinical trial. J Arthroplasty. 2014;29:169-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 149] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 88. | Taunton MJ, Trousdale RT, Sierra RJ, Kaufman K, Pagnano MW. John Charnley Award: Randomized Clinical Trial of Direct Anterior and Miniposterior Approach THA: Which Provides Better Functional Recovery? Clin Orthop Relat Res. 2018;476:216-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 113] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 89. | Yan T, Tian S, Wang Y, Yang X, Li T, Liu J, Pan P, Wang R, Wang D, Sun K. [Comparison of early effectiveness between SuperPATH approach and Hardinge approach in total hip arthroplasty]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2017;31:17-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 90. | Vicente JR, Miyahara HS, Luzo CM, Gurgel HM, Croci AT. Total hip arthroplasty using a posterior minimally invasive approach - results after six years. Rev Bras Ortop. 2015;50:77-82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 91. | Wang T, Shao L, Xu W, Chen H, Huang W. Comparison of morphological changes of gluteus medius and abductor strength for total hip arthroplasty via posterior and modified direct lateral approaches. Int Orthop. 2019;43:2467-2475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 92. | Witzleb WC, Stephan L, Krummenauer F, Neuke A, Günther KP. Short-term outcome after posterior versus lateral surgical approach for total hip arthroplasty - A randomized clinical trial. Eur J Med Res. 2009;14:256-263. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 30] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 93. | Xie J, Zhang H, Wang L, Yao X, Pan Z, Jiang Q. Comparison of supercapsular percutaneously assisted approach total hip versus conventional posterior approach for total hip arthroplasty: a prospective, randomized controlled trial. J Orthop Surg Res. 2017;12:138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 94. | Xu J, Zhuang WD, Li XW, Yu GY, Lin Y, Luo FQ, Xiao YH. [Comparison of the effects of total hip arthroplasty via direct anterior approach and posterolateral piriformis-sparing approach]. Beijing Da Xue Xue Bao Yi Xue Ban. 2017;49:214-220. [PubMed] |
| 95. | Yang C, Zhu Q, Han Y, Zhu J, Wang H, Cong R, Zhang D. Minimally-invasive total hip arthroplasty will improve early postoperative outcomes: a prospective, randomized, controlled trial. Ir J Med Sci. 2010;179:285-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 30] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 96. | Zhao HY, Kang PD, Xia YY, Shi XJ, Nie Y, Pei FX. Comparison of Early Functional Recovery After Total Hip Arthroplasty Using a Direct Anterior or Posterolateral Approach: A Randomized Controlled Trial. J Arthroplasty. 2017;32:3421-3428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 132] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 97. | Zomar BO, Bryant D, Hunter S, Howard JL, Vasarhelyi EM, Lanting BA. A randomised trial comparing spatio-temporal gait parameters after total hip arthroplasty between the direct anterior and direct lateral surgical approaches. Hip Int. 2018;28:478-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 98. | Yue C, Kang P, Pei F. Comparison of Direct Anterior and Lateral Approaches in Total Hip Arthroplasty: A Systematic Review and Meta-Analysis (PRISMA). Medicine (Baltimore). 2015;94:e2126. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 84] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 99. | Singh JA, Schleck C, Harmsen S, Lewallen D. Clinically important improvement thresholds for Harris Hip Score and its ability to predict revision risk after primary total hip arthroplasty. BMC Musculoskelet Disord. 2016;17:256. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 85] [Cited by in RCA: 164] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 100. | Duijnisveld BJ, van den Hout JAAM, Wagenmakers R, Koenraadt KLM, Bolder SBT. No Learning Curve of the Direct Superior Approach in Total Hip Arthroplasty. Orthop Surg. 2020;12:852-860. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 101. | Realyvasquez J, Singh V, Shah AK, Ortiz D 3rd, Robin JX, Brash A, Kurapatti M, Davidovitch RI, Schwarzkopf R. The direct anterior approach to the hip: a useful tool in experienced hands or just another approach? Arthroplasty. 2022;4:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 102. | Nairn L, Gyemi L, Gouveia K, Ekhtiari S, Khanna V. The learning curve for the direct anterior total hip arthroplasty: a systematic review. Int Orthop. 2021;45:1971-1982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 69] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 103. | Pirruccio K, Evangelista PJ, Haw J, Goldberg T, Sheth NP. Safely Implementing the Direct Anterior Total Hip Arthroplasty: A Methodological Approach to Minimizing the Learning Curve. J Am Acad Orthop Surg. 2020;28:930-936. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 104. | Ropars M, Morandi X, Huten D, Thomazeau H, Berton E, Darnault P. Anatomical study of the lateral femoral cutaneous nerve with special reference to minimally invasive anterior approach for total hip replacement. Surg Radiol Anat. 2009;31:199-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 59] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 105. | O'Connor CM, Anoushiravani AA, Acosta E, Davidovitch RI, Tetreault MW. Direct Anterior Approach Total Hip Arthroplasty Is Not Associated with Increased Infection Rates: A Systematic Review and Meta-Analysis. JBJS Rev. 2021;9:e20.00047. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 106. | Mortazavi SMJ, Kazemi M, Noaparast M. Femoral artery intimal injury following total hip arthroplasty through the direct anterior approach: a rare but potential complication. Arthroplast Today. 2019;5:288-291. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Thailand
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ammarullah MI, Indonesia S-Editor: Chen YL L-Editor: A P-Editor: Guo X