Published online Jan 18, 2024. doi: 10.5312/wjo.v15.i1.61
Peer-review started: October 23, 2023
First decision: November 29, 2023
Revised: December 1, 2023
Accepted: December 27, 2023
Article in press: December 27, 2023
Published online: January 18, 2024
Processing time: 84 Days and 22.6 Hours
Adolescent idiopathic scoliosis remains a major problem due to its high incidence, high risk, and high cost. One of the aims of the management in scoliosis is to correct the deformity. Many techniques are available to correct scoliosis defor
To develop a set of tools named Scoliocorrector Fatma-UI (SCFUI) to aid three-dimensional correction and to evaluate the efficacy, safety, and functional outcome.
This study consists of two stages. In the first stage, we developed the SCFUI and tested it in finite element and biomechanical tests. The second stage was a single-blinded randomized clinical trial to evaluate the SCFUI compared to direct vertebral rotation (DVR). Forty-four subjects with adolescent idiopathic scoliosis were randomly allocated into the DVR group (n = 23) and SCFUI group (n = 21). Radiological, neurological, and functional outcome was compared between the groups.
Finite element revealed the maximum stress of the SCFUI components to be between 31.2 - 252 MPa. Biomechanical analysis revealed the modulus elasticity of SCFUI was 9561324 ± 633277 MPa. Both groups showed improvement in Cobb angle and sagittal profile, however the rotation angle was lower in the SCFUI group (11.59 ± 7.46 vs 18.23 ± 6.39, P = 0.001). Neurological and functional outcome were comparable in both groups.
We concluded that SCFUI developed in this study resulted in similar coronal and sagittal but better rotational correction compared to DVR. The safety and functional outcomes were also similar to DVR.
Core Tip: We developed a novel set of tools to aid in the three-dimensional correction of adolescent idiopathic scoliosis. We performed finite element and biomechanical tests on the tools and evaluated its radiological, neurological and functional outcomes in a randomized clinical trial to ensure its efficacy and safety.
- Citation: Phedy P, Dilogo IH, Indriatmi W, Supriadi S, Prasetyo M, Octaviana F, Noor Z. Scoliocorrector Fatma-UI for correction of adolescent idiopathic scoliosis: Development, effectivity, safety and functional outcome. World J Orthop 2024; 15(1): 61-72
- URL: https://www.wjgnet.com/2218-5836/full/v15/i1/61.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i1.61
Adolescent idiopathic scoliosis (AIS) remains a major problem due to its high incidence, high risk, and high cost. The incidence of AIS is as high as 13%[1]. The management of AIS is also subject to a high risk of complications such as death, pseudoarthrosis, infection, neurological deficits, and pedicle screw misplacements[2]. The cost needed to manage AIS reached USD 55.000 in 1997 and USD 177.000 in 2012 and continues to increase[3].
One of the aims of management in adolescent idiopathic scoliosis is to correct the deformity. While coronal correction remains the major aim, corrections in sagittal and axial planes are also necessary. Both sagittal and axial plane deformity are associated with a decrease in lung function[4,5].
Many techniques are available to correct scoliosis deformities. However, all of them are far from ideal to achieve three-dimensional correction in scoliosis[6]. Direct vertebral rotation (DVR) gives excellent coronal and rotational correction but causes thoracic hypokyphosis[7]. Its safety is also questioned[8]. Posteromedial translation is reported to result in good coronal and sagittal correction but its rotational correction is questioned[6]. Sublaminar fixation point in posteromedial translation is located posterior to the rotational axis in scoliosis and may affect the axial correction[9]. Posteromedial translation also requires a universal clamp and sublaminar band, which are not available in many countries.
The aim of this study is to develop a set of tools named Scoliocorrector Fatma-UI (SCFUI) to aid three-dimensional scoliosis correction and to evaluate the efficacy, safety, and functional outcome of the tools in AIS surgery.
This study consists of two stages. The first stage was the development of the SCFUI, as well as finite element and biomechanical analysis to evaluate the validity and safety of the SCFUI. The second stage was a single-blinded randomized clinical trial to evaluate the effectivity, safety, and functional outcome of the SCFUI compared to DVR.
Development of SCFUI started in January to May 2020 in the Integrated Creative Learning Laboratory, Faculty of Technics, University of Indonesia. We listed anticipated benefits of the tools as well as ways to achieve them and formulated them in conceptual design. The conceptual design was subsequently developed into a technical design with an initial size complying with pedicle screws available in the market. Technical design was developed in Solidworks v.2017 software. The design was tested in finite element analysis using ANSYS v.2020 software. We tested the design by static structural method, no separation contact, automatic mesh, and stainless-steel 316L material with a testing force of 800N. We modified the size and design until the stress was lower than the yield strength of stainless steel 316L. Using Ultimaker Cura v.11, we modified the size and orientation of the SCFUI design to comply with the building machine. SCFUI was built using CNC milling Harford 1000 × 500 × 500 dan CNC Milling Eccoca 1050 × 550 × 500. The prototype was then tested using Universal Testing Machine Tensilon RTF 2350. Four hundred Newton force was used to pull SCFUI with a speed of 50 mm/s ten times, and the modulus of elasticity was recorded. The stress-strain curve was also generated. The prototype was pulled until the failure point to measure the maximum force and the response at the failure point.
The second stage of the study was conducted in Fatmawati General Hospital from June 2020 to June 2021. The inclusion criteria were adolescent patients aged 11 to 18 with Lenke 1 idiopathic scoliosis 40-100 degrees without a history of previous spinal surgery. Forty-four subjects were randomized into the intervention group (SCFUI, n = 21) and control group (DVR, n = 23) using Randlist® software. The subject was blinded to the randomization. Ethical clearances from the Faculty of Medicine University of Indonesia number 615/UN2.F1/ETIK/PPM.00.02/2020 and Fatmawati General Hospital number DM01.01/VIII.2/294/2020 were obtained before the study.
Under general anesthetic and intraoperative neuromonitoring, the subject was put prone on two bolsters in the chest and pelvis region and fixed to the surgical table. The spine was exposed from the upper to lower instrumented vertebra (LIV). The upper instrumented vertebra (UIV) was the neutral vertebra cranial to upper-end vertebra while LIV was the last significantly touched vertebra. Screws were inserted into UIV, 1 level distal to UIV, apical vertebra, 1 level proximal and 1 level distal to apical vertebra, 1 level proximal to LIV and LIV. Whenever there were more than three subsequent vertebrae to UIV or LIV, additional screws were placed until there were no more than three instrumented subsequent vertebrae. The screws were inserted free hand without any specific attempt to hit the cortical bone in front of the vertical body, as it would increase risk of injury. A correction was performed according to the group allocation, and the wound was closed layer by layer.
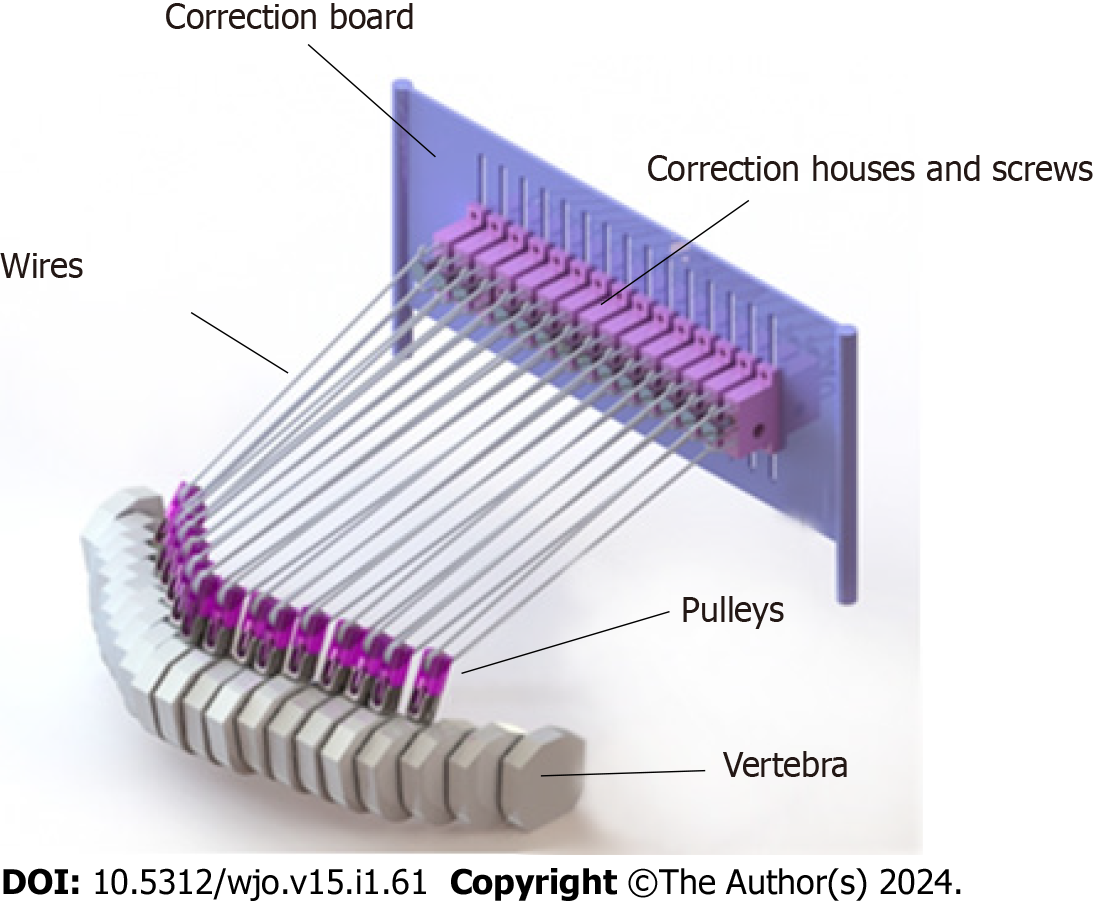
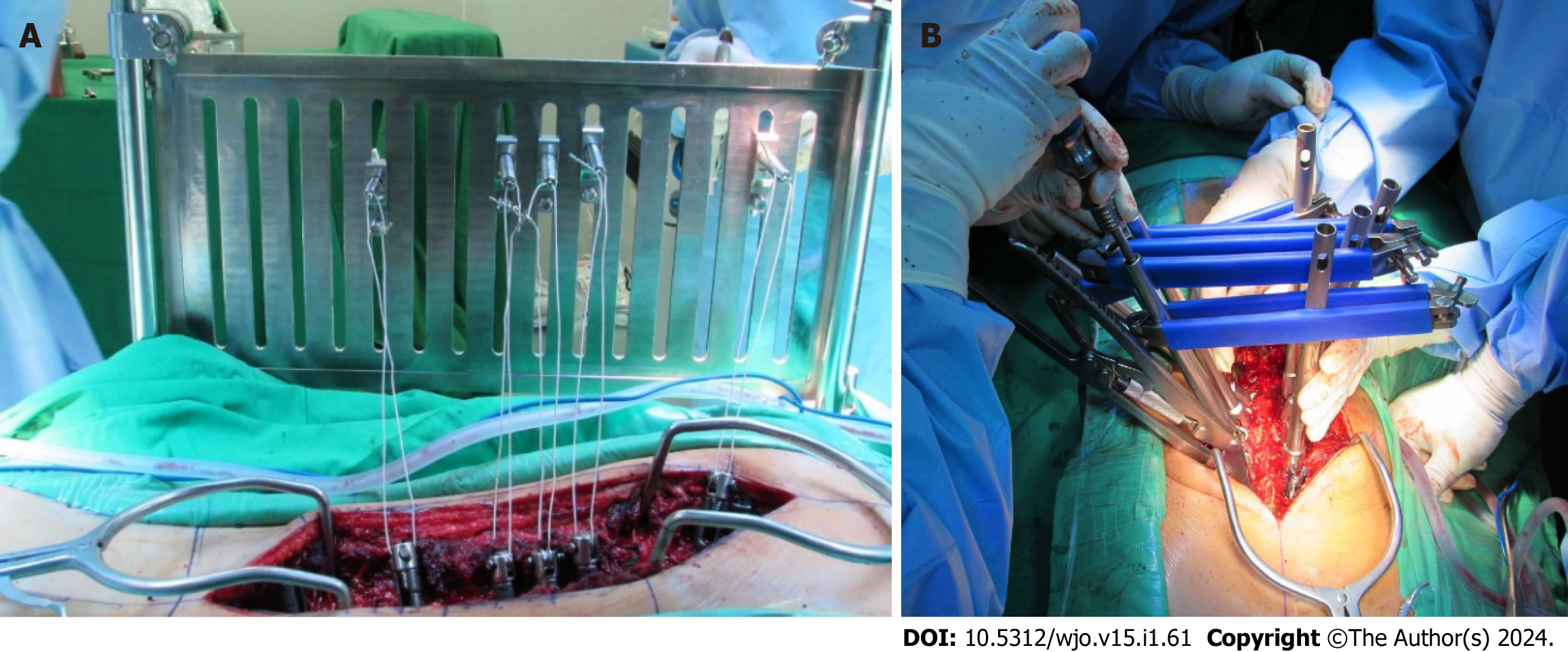
For the intervention group, five pulleys were attached to the apical, one level above and below the apical screw, and to the closest screw proximal and distal to the apical screws. The correction board was attached to the surgical table on the concave side. Five correction screws and their housing were assembled and attached to the correction board according to the normal sagittal profile and intended direction of pulling. The lowest screw housing should be at least 5 cm higher than the most prominent point of the curve. Five wires were fixed to the correction screws and housings and circled to the pulleys to form moveable pulleys. A correction was achieved by gradually and alternately rotating the correction screws to pull the moveable pulleys. The pull was stopped when correction was achieved, screw rotation was maximized, or whenever there was a screw pullout. The convex rod was attached and secured with set screws. Pulleys were removed, and the concave rod was attached and secured with set screws.
For the control group, both rods were inserted and loosely secured with set screws. Tubes were inserted into the screws closest to the apical vertebrae. The vertebrae were rotated as neutral as possible and set screws were tightened. Other tubes were inserted into apical dan periapical screws and rotated while counter-rotation was performed on the distal neutral tubes. All set screws were tightened.
For radiological outcome, the coronal cobb angle and T5-12 kyphosis angle were measured from a standing radiograph, and rotational angle (RaSag) of the apical vertebra was measured from computed tomography (CT) scan. The radiograph and CT scan were obtained preoperatively and within 10 d after surgery. Intraoperative motor evoked potential, somatosensory evoked potential, and electromyography as well as post-operative motor power of the lower extremity were also recorded. Functional outcome was also measured using the SRS-22 questionnaire. The data were compared between groups, and statistical analysis was performed using STATA v. 14.
We first identified the needs and then the principles and methods to fulfill the needs. The concept is shown in Table 1. Based on the concept, we developed a set of tools consisting of a correction board, correction screw, and its housing, wire, and pulley. The pulley is attached to pedicle screws and pulled toward correction screws secured by screw housing on the correction board (Figure 1).
| Need | Principle | Method |
| High failure load | Fixation of vertebrae using gold standard in spine surgery | Pedicle screw fixation |
| Good coronal correction | Long medial translation | Wire pulls from outside of the body |
| Good rotational correction | The correction axis should be anterior to the rotational axis of scoliosis | Pedicle screw fixation as it reaches to anterior corpus |
| Long posteromedial translation | Wire pulls from outside of the body | |
| Good sagittal correction | The pulling point height can be adjusted to a normal sagittal profile | Pulling board to accommodate height adjustment of pulling point |
| Long posterior translation | Wire pulls from outside of the body | |
| Low correction force | Mechanical advantages | Moveable pulley |
| Optimal pulling vector | The pulling vector could be adjusted | Moveable pulley |
| Controllable correction | Gradual correction | Screw threads to control gradual correction |
| Efficient | Correction could be maintained | Screw threads to maintain correction |
| Low risk of neurological injury due to sublaminar fixation | Others fixation anchor | Pedicle screw fixation |
| Low risk of neurological injury due to medial breaching | Avoid derotation of screws toward spinal canal | Wire pulls to the lateral vertebral canal |
| No risk of foreign body reaction | No extra implant | Removal of tools after correction is achieved |
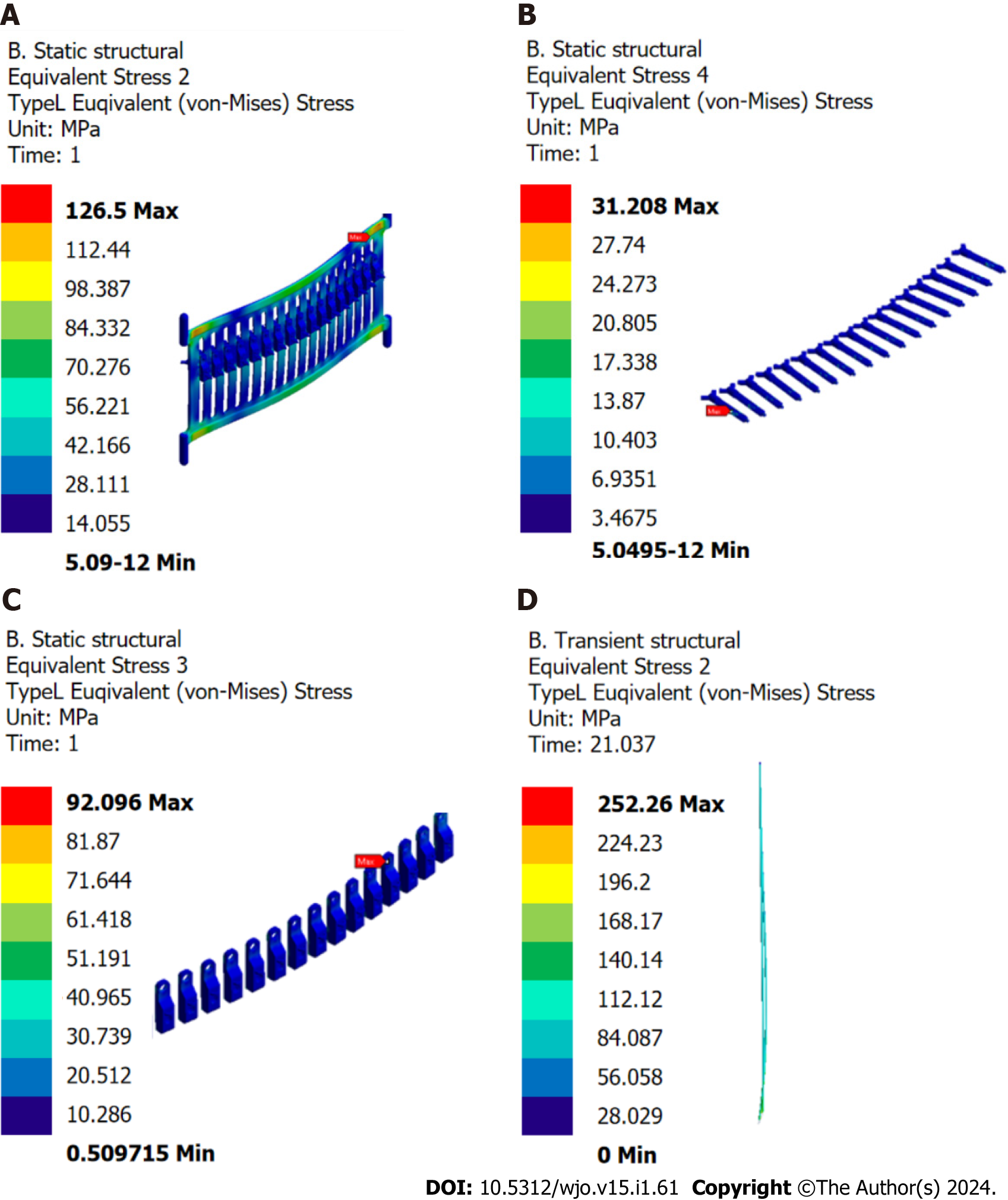
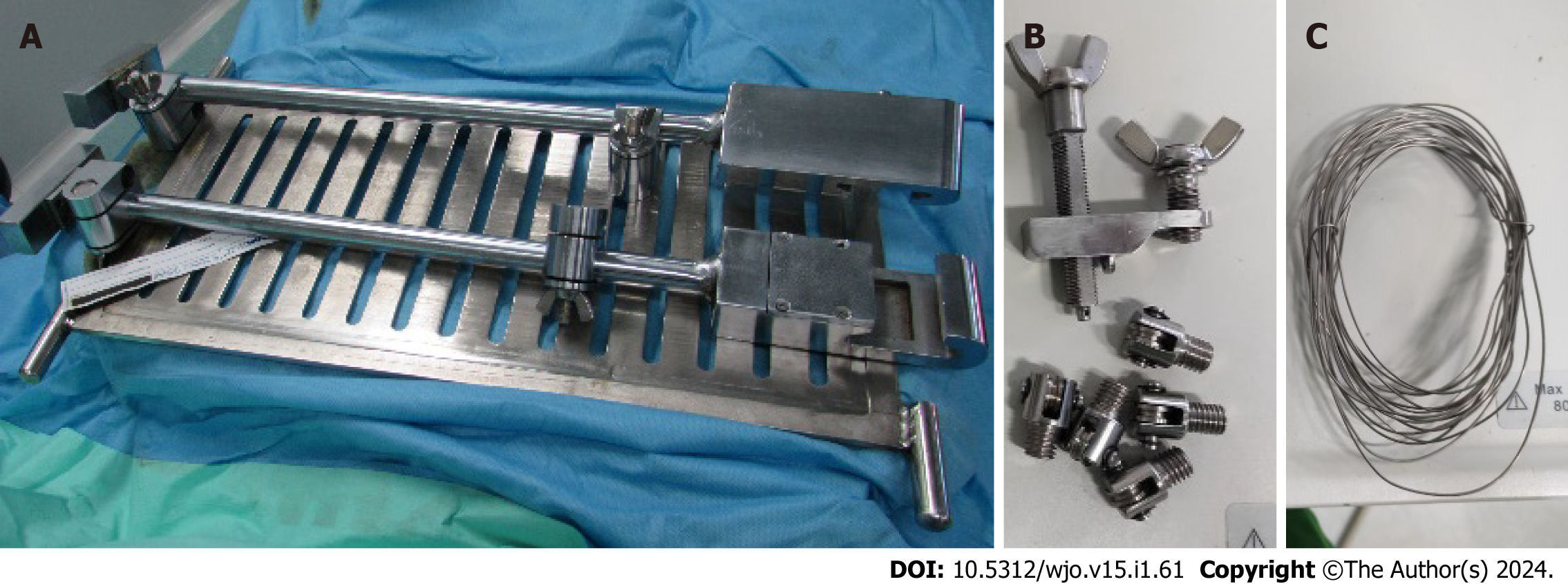
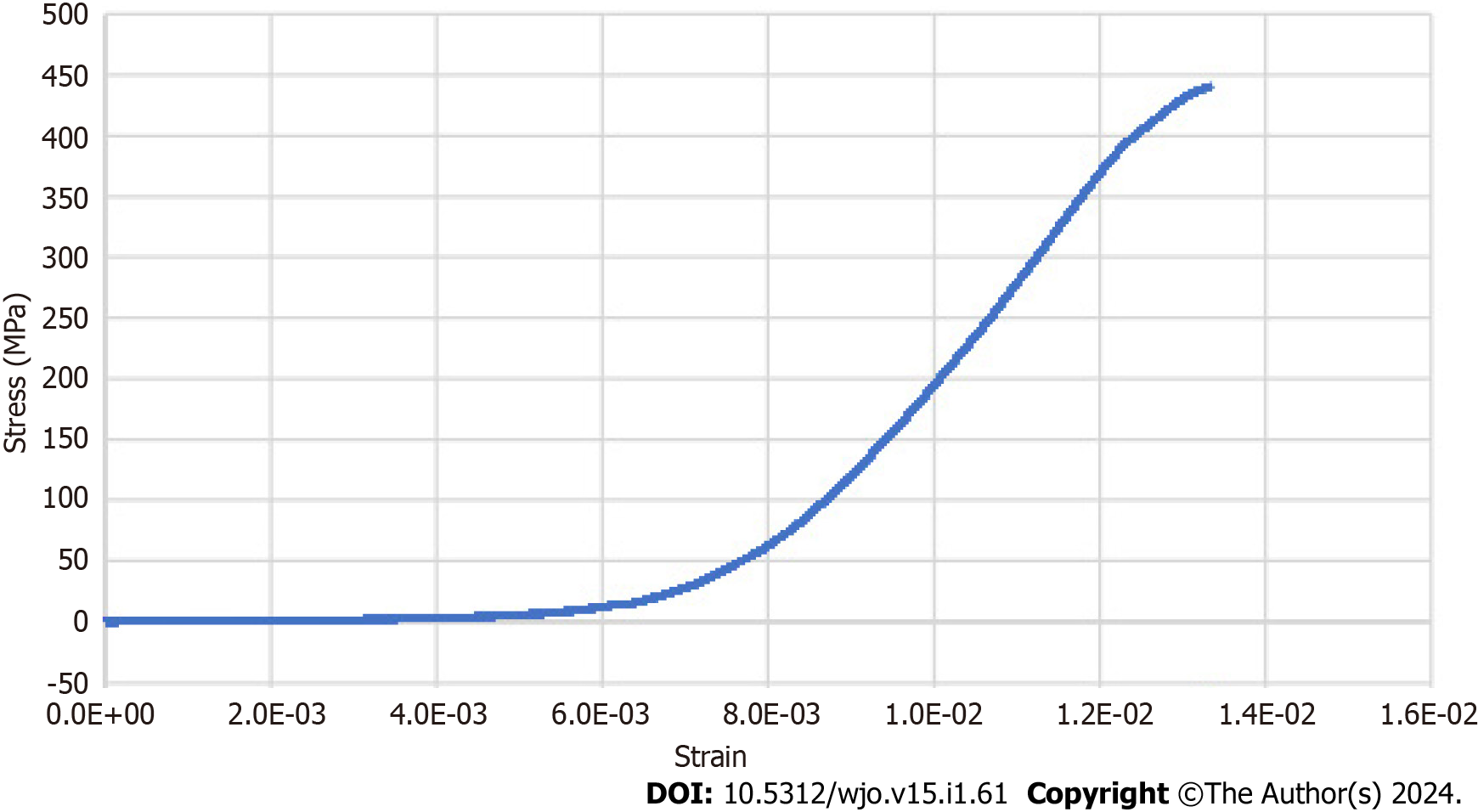
From the finite element analysis, the maximum stress of the correction board, correction screw, screw housing, and wire were 126.5 MPa, 31.2 MPa, 92.1 MPa, and 252 MPa, respectively (Figure 2). Passing finite element analysis, the SCFUI prototype was built (Figure 3). Biomechanical analysis revealed the modulus elasticity of SCFUI to be 9561324 ± 633277 MPa. The stress-strain curve is shown in Figure 4. Failure of SCFUI was observed at 800 Nm as detachment of wire from correction screw.
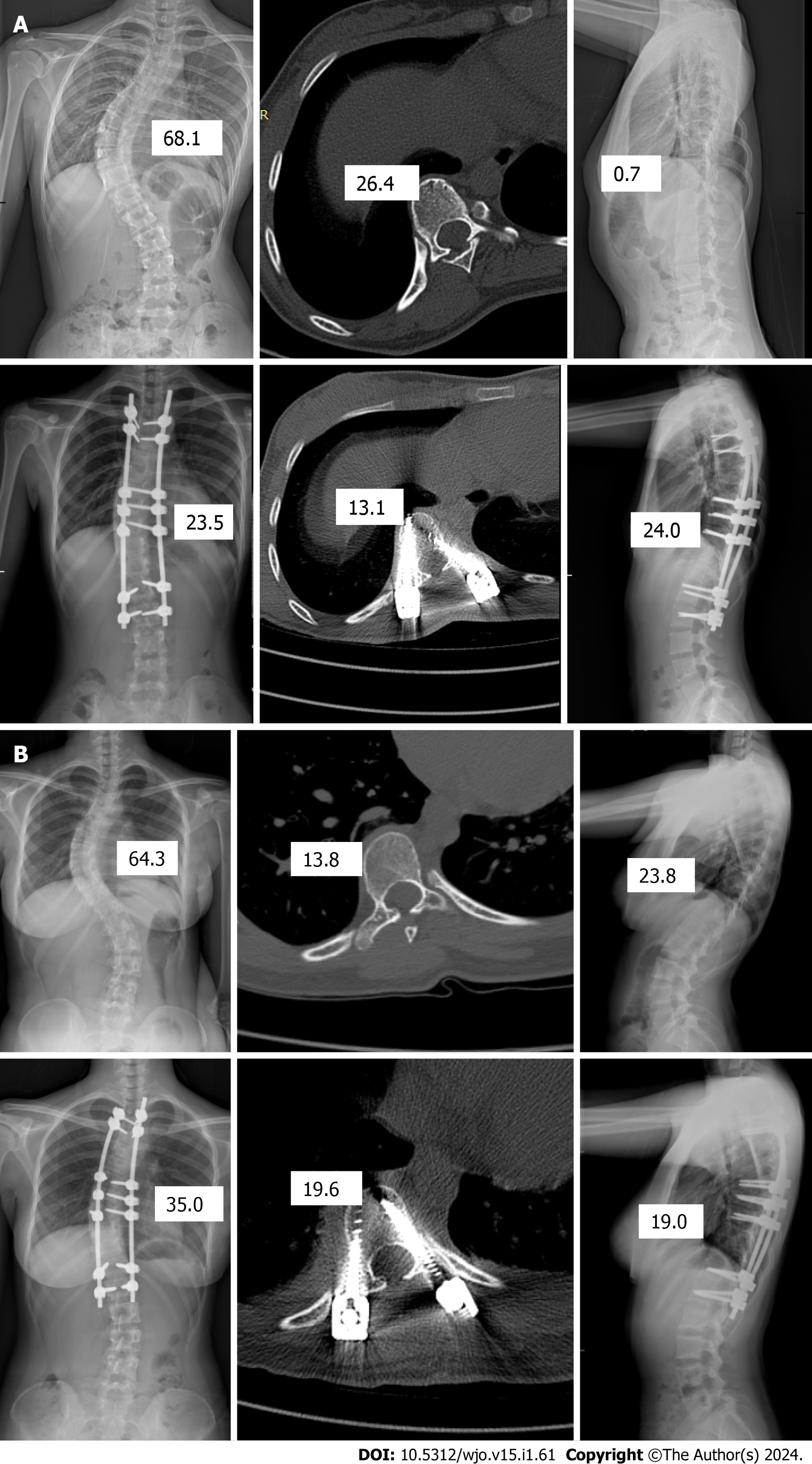
Baseline characteristics of research subjects are shown in Table 2, while corrections using intervention and control groups are in Figure 5. Body weight, coronal curve, and rotational angle in the control group were higher than in the intervention group.
| Characteristic | Intervention group, n = 21 | Control group, n = 23 | P value |
| Clinical | |||
| Age - yr, mean (SD) | 15.92 (0.35) | 15.73 (1.51) | 0.331 |
| Sex | |||
| Male | 2 (9.52) | 4 (17.39) | 0.672 |
| Female | 19 (90.48) | 19 (82.61) | |
| Body height - cm, mean (SD) | 155.24 (7.52) | 157.48 (6.1) | 0.141 |
| Body weight - kg, mean (SD) | 44.11 (5.66) | 47.95 (6.78) | 0.021 |
| Radiological | |||
| Cobb angle - degree, mean (SD) | 57.19 (6.78) | 62.58 (8.51) | 0.011 |
| Sagittal angle - degree, mean (SD) | 17.7 (6.7) | 20.08 (9.71) | 0.181 |
| Rotational angle - degree, mean (SD) | 14.76 (6.73) | 19.42 (7.81) | 0.021 |
| Sagittal profile | |||
| Hypokyphosis | 14 (66.67) | 12 (52.17) | 0.332 |
| Normokyphosis | 7 (33.33) | 11 (47.83) | |
| Functional | |||
| SRS score - 22, mean (SD) | 70.14 (6.81) | 68.61 (6.85) | 0.231 |
| Function domain, mean (SD) | 4.13 (0.29) | 4 (0.47) | 0.131 |
| Pain domain, mean (SD) | 3.55 (0.54) | 3.61 (0.64) | 0.381 |
| Self-image domain, mean (SD) | 2.47 (0.6) | 2.42 (0.59) | 0.371 |
| Mental health domain, median (range) | 4 (3-5) | 3.6 (3-4.6) | 0.413 |
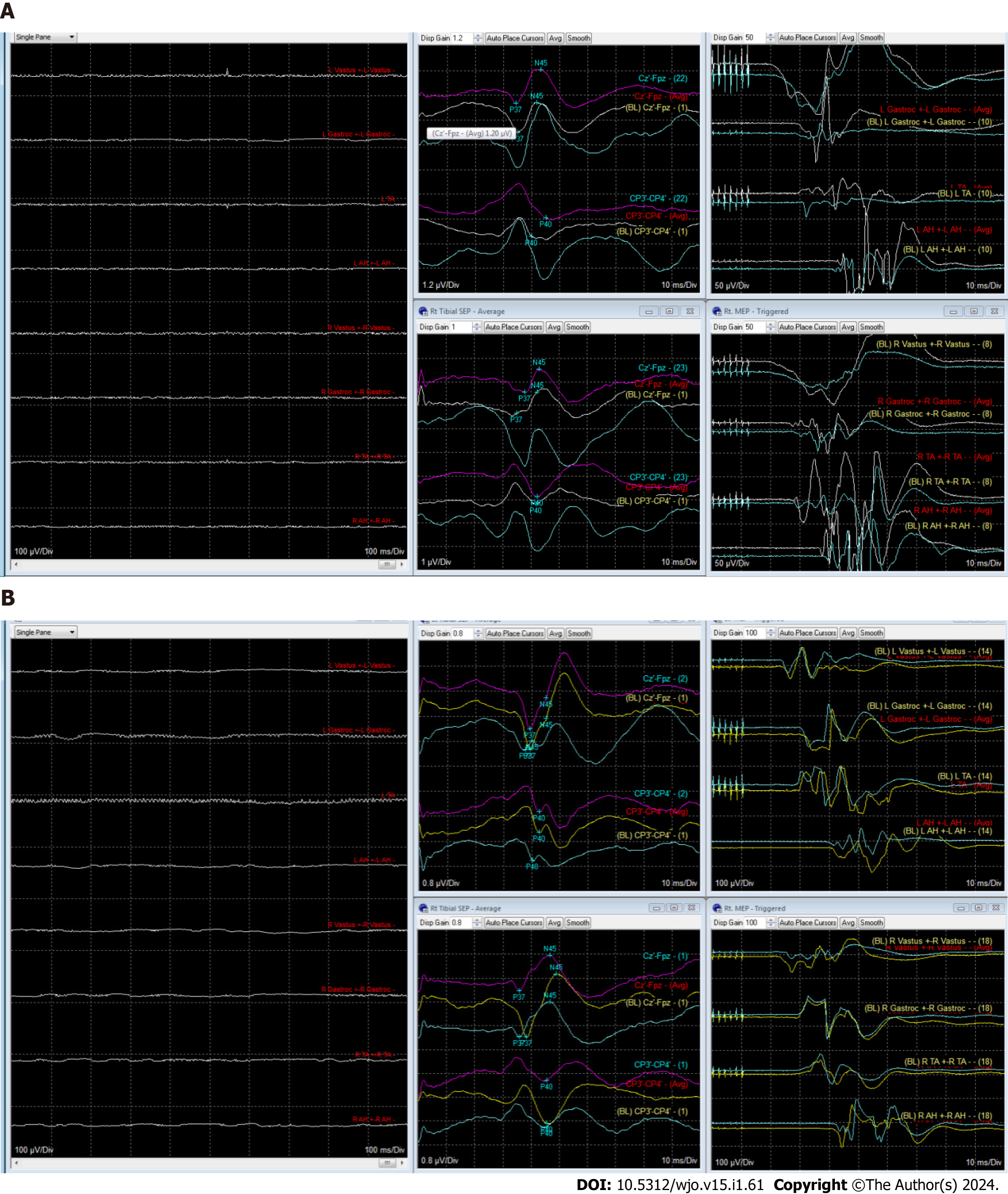
Postoperatively, only rotational angle in the control group was higher than the intervention group (Table 3 and Figure 6). No abnormality of motor-evoked potential, somatosensory-evoked potential, or neurotonic discharge was found during surgery in either group (Figure 7). Postoperatively, no motor deficit was found in any group. During the study, no adverse event, screw pullout, or wire breakage was observed.
| Characteristic | Intervention group, n = 21 | Control group, n = 23 | P value |
| Clinical | |||
| Body height - cm, mean (SD) | 159.28 (7.73) | 161.13 (6) | 0.191 |
| Body weight - kg, mean (SD) | 44.19 (5.1) | 48 (6.86) | 0.021 |
| Radiological | |||
| Cobb angle - degree, mean (SD) | 16.28 (10.36) | 20.79 (8.72) | 0.061 |
| Coronal correction - percent, mean (SD) | 71.92 (17.55) | 67.39 (17.55) | 0.161 |
| Sagittal angle - degree, mean (SD) | 20.16 (4.75) | 20.32 (6.63) | 0.531 |
| Rotational angle - degree, mean (SD) | 11.59 ± 7.46 | 18.23 ± 6.39 | 0.0011 |
| Sagittal profile | |||
| Hypokyphosis | 11 (52.38) | 10 (43.49) | 0.562 |
| Normokyphosis | 10 (47.62) | 13 (56.52) | |
| Functional | |||
| SRS-22 score, median (range) | 63 (50-84) | 68 (43-79) | 0.623 |
| Function domain, mean (SD) | 1.81 (0.41) | 1.94 (0.42) | 0.171 |
| Pain domain, mean (SD) | 2.68 (0.56) | 2.67 (0.58) | 0.481 |
| Self-image domain, median (range) | 3.4 (2.4-4.6) | 3.6 (1.8-4.4) | 0.833 |
| Mental health domain, mean (SD) | 3.21 (0.68) | 3.37 (0.74) | 0.231 |
| Satisfaction, median (range) | 4.5 (4-5) | 4.5 (3-5) | 0.43 |
In the development of SCFUI, stainless-steel 316L was used as the material. Stainless-steel 316L is strong, stain-resistant, low maintenance, and economical[10]. It is also one of the most used alloys for spinal implants[11,12].
In finite element analysis, the highest stress was observed in the wire. However, the stress was lower than the yield strength and ultimate strength of stainless steel 316L[13]. It indicates that SCFUI is in the elastic phase, meaning that it can withstand force without any change in shape or failure[10,13]. During the analysis, the force used is far higher than the force required in clinical application or the force to cause screw pullout[13]. Moveable pulley configuration in SCFUI also gives a mechanical advantage to lower the force needed to correct the deformity up to 200%[14]. Biomechanical studies validated the finding of finite element analysis. The modulus elasticity of SCFUI is lower than the modulus elasticity of stainless-steel 316L and the stress-strain curve is proportional[13]. Hooke law describes that if the stress is proportional to the strain, a material is in the elastic condition; thus it will return to its initial shape whenever the force is removed[15].
At the point of failure, the wire attachment to the correction screw will be detached. The detachment occurs slowly and can be observed with the naked eye. The finding emphasizes the safety of SCFUI, as in the event of failure, it will not endanger the patient.
The SCFUI is therefore compliant with the ASTM F2193 standard[16]. ASTM F2193 is the international standard for the development of surgical instruments for spinal surgery. It included the design, strength, and safety of the instrument.
Coronal correction is important in the evaluation of surgery outcomes. For patients, coronal correction is the main indicator of the success of surgery. Medically, coronal correction is correlated to functional outcome[17]. In SCFUI, pedicle screw fixation is the use of higher force for correction. Moreover, the moveable pulley increases the force acting on the spine twofold. It also optimized the vector of pull.
Our coronal correction is similar to correction using posteromedial translation by Mazda et al[6]. They reported coronal correction of 66% ± 13%. A meta-analysis reported the coronal correction of scoliosis surgery was 60%-80% regardless of technique used for correction[18].
Evaluation of the sagittal profile is also important. An imbalance of the sagittal profile will result in poor pulmonary function and increased complications[19]. In our study, both techniques gave a good sagittal profile. The reported hypokyphosis due to DVR was not observed in our study.
SFCUI uses the correction board as the pulling point for translation. It allows a longer distance of posteromedial translation. However, the advantage of SCFUI over DVR for sagittal correction was not proven in our study. The advantage of SCFUI for sagittal correction is negated by the use of pedicle screws, which can also cause hypokyphosis. Moreover, the DVR in our study resulted in good sagittal correction.
Rotational correction is also emphasized in scoliosis correction[20]. Poor rotation will result in rib cage asymmetry and decreased respiratory function[21,22]. In our study, a better rotation correction was achieved by SCFUI. SCFUI utilized pedicle screw fixation that penetrate the vertebral body, thus allowing a fixation axis anterior to the rotation axis in scoliosis. Fixation points anterior to the rotational axis is mandatory to achieve adequate torsion for vertebra derotation[9]. However, it should be noted that our result is subject to bias, as a bigger rotational angle was found in the control group before the study.
We did not find any neurological deficits in our study. It might indicate that both techniques were safe. Nevertheless, scoliosis in our study was limited to a mild curve in which the incidence of neurological deficit is quite low[23]. The incidence of the neurological deficit will increase by the severity of the curve and the presence of hyperkyphosis[23,24]. None of the subjects in our study had hyperkyphosis.
SCFUI was developed with a novel design and complied with the international standard for spinal instruments[16]. The efficacy, safety, and functional outcomes had also been evaluated in the clinical study. However, our study was subject to several limitations. We did not measure the duration needed to assemble the correction tools until the correction was performed, nor whether bleeding occurred during the period. SCFUI is quite heavy and its assembly takes time. Further study is necessary to simplify the assembly and to reduce the size and weight. Scoliosis evaluated in this study was also very narrow, limited to Lenke type 1 curve only. Further study involving wider Lenke criteria should be performed.
We concluded that SCFUI developed in this study comply with the international standard for spinal instrument. It resulted in similar coronal and sagittal but potentially better rotational correction compared to DVR. The safety and functional outcomes were also similar to DVR.
Adolescent idiopathic scoliosis remains a main problem in orthopedics due to its high incidence, high risk, and high cost.
Ideal correction of scoliosis should be three-dimensional. However, many techniques failed to achieve three-dimensional correction.
We developed a novel set of tools to aid three-dimensional correction of adolescent idiopathic scoliosis.
We performed finite element and biomechanical test for the tools, and evaluated its radiological, neurological and functional outcomes in a randomized clinical trial to ensure its efficacy and safety.
The tools developed passed the finite element analysis and biomechanical test as well as clinical study.
We developed a novel set of tools to aid three-dimensional correction of adolescent idiopathic scoliosis.
A simplification of the tools.
| 1. | Hengwei F, Zifang H, Qifei W, Weiqing T, Nali D, Ping Y, Junlin Y. Prevalence of Idiopathic Scoliosis in Chinese Schoolchildren: A Large, Population-Based Study. Spine (Phila Pa 1976). 2016;41:259-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 71] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 2. | Weiss HR, Goodall D. Rate of complications in scoliosis surgery - a systematic review of the Pub Med literature. Scoliosis. 2008;3:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 153] [Cited by in RCA: 167] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 3. | Raudenbush BL, Gurd DP, Goodwin RC, Kuivila TE, Ballock RT. Cost analysis of adolescent idiopathic scoliosis surgery: early discharge decreases hospital costs much less than intraoperative variables under the control of the surgeon. J Spine Surg. 2017;3:50-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 4. | Rhee JM, Bridwell KH, Won DS, Lenke LG, Chotigavanichaya C, Hanson DS. Sagittal plane analysis of adolescent idiopathic scoliosis: the effect of anterior versus posterior instrumentation. Spine (Phila Pa 1976). 2002;27:2350-2356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 140] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 5. | Di Silvestre M, Lolli F, Bakaloudis G, Maredi E, Vommaro F, Pastorelli F. Apical vertebral derotation in the posterior treatment of adolescent idiopathic scoliosis: myth or reality? Eur Spine J. 2013;22:313-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 65] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 6. | Mazda K, Ilharreborde B, Even J, Lefevre Y, Fitoussi F, Penneçot GF. Efficacy and safety of posteromedial translation for correction of thoracic curves in adolescent idiopathic scoliosis using a new connection to the spine: the Universal Clamp. Eur Spine J. 2009;18:158-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 83] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 7. | Watanabe K, Nakamura T, Iwanami A, Hosogane N, Tsuji T, Ishii K, Nakamura M, Toyama Y, Chiba K, Matsumoto M. Vertebral derotation in adolescent idiopathic scoliosis causes hypokyphosis of the thoracic spine. BMC Musculoskelet Disord. 2012;13:99. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 56] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 8. | Urbanski W, Wolanczyk MJ, Jurasz W, Kulej M, Morasiewicz P, Dragan SL, Sasiadek M, Dragan SF. The impact of direct vertebral rotation (DVR) on radiographic outcome in surgical correction of idiopathic scoliosis. Arch Orthop Trauma Surg. 2017;137:879-885. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 31] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 9. | Lee SM, Suk SI, Chung ER. Direct vertebral rotation: a new technique of three-dimensional deformity correction with segmental pedicle screw fixation in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2004;29:343-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 281] [Cited by in RCA: 294] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 10. | Coe JD, Arlet V, Donaldson W, Berven S, Hanson DS, Mudiyam R, Perra JH, Shaffrey CI. Complications in spinal fusion for adolescent idiopathic scoliosis in the new millennium. A report of the Scoliosis Research Society Morbidity and Mortality Committee. Spine (Phila Pa 1976). 2006;31:345-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 282] [Cited by in RCA: 305] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 11. | Sae-Jung S, Jirarattanaphochai K, Saengnipanthkul S. The invention of new anterior spinal instrumentation prototype: a structural analysis of KKU expandable cage. J Med Assoc Thai. 2007;90:1621-1626. [PubMed] |
| 12. | Majid K, Crowder T, Baker E, Baker K, Koueiter D, Shields E, Herkowitz HN. Analysis of in vivo corrosion of 316L stainless steel posterior thoracolumbar plate systems: a retrieval study. J Spinal Disord Tech. 2011;24:500-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | ASM Material Data Sheet. [cited July 3, 2023]. Available from: https://asm.matweb.com/search/SpecificMaterial.asp?bassnum=mq316q. |
| 14. | Endi M. Materi IPA SMP kelas 8 (viii): usaha dan pesawat sederhana [Internet]. [cited September 3, 2023]. Available from: https://www.belajaripa.com/2020/11/ipa-smp-8-usaha-dan-pesawat-sederhana.html. |
| 15. | Kurva Tegangan Regangan (Stress-Strain Curve) Pada Uji Tarik. [cited July 3, 2023]. Available from: https://www.etsworlds.id/2020/01/kurva-tegangan-regangan-stress-strain.html. |
| 16. | Standard Specifications and Test Methods for Components Used in the Surgical Fixation of the Spinal Skeletal System . [DOI] [Full Text] |
| 17. | Ghandehari H, Mahabadi MA, Mahdavi SM, Shahsavaripour A, Seyed Tari HV, Safdari F. Evaluation of Patient Outcome and Satisfaction after Surgical Treatment of Adolescent Idiopathic Scoliosis Using Scoliosis Research Society-30. Arch Bone Jt Surg. 2015;3:109-113. [PubMed] |
| 18. | Son SM, Choi SH, Goh TS, Park W, Lee JS. Efficacy and Safety of Direct Vertebral Rotation in the Surgical Correction of Scoliosis: A Meta-Analysis. World Neurosurg. 2019;124:e641-e648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | Schroerlucke SR, Akbarnia BA, Pawelek JB, Salari P, Mundis GM Jr, Yazici M, Emans JB, Sponseller PD; Growing Spine Study Group. How does thoracic kyphosis affect patient outcomes in growing rod surgery? Spine (Phila Pa 1976). 2012;37:1303-1309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 59] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 20. | Lam GC, Hill DL, Le LH, Raso JV, Lou EH. Vertebral rotation measurement: a summary and comparison of common radiographic and CT methods. Scoliosis. 2008;3:16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 98] [Cited by in RCA: 104] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 21. | Adam CJ, Askin GN, Pearcy MJ. Gravity-induced torque and intravertebral rotation in idiopathic scoliosis. Spine (Phila Pa 1976). 2008;33:E30-E37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 22. | Cui G, Watanabe K, Nishiwaki Y, Hosogane N, Tsuji T, Ishii K, Nakamura M, Toyama Y, Chiba K, Matsumoto M. Loss of apical vertebral derotation in adolescent idiopathic scoliosis: 2-year follow-up using multi-planar reconstruction computed tomography. Eur Spine J. 2012;21:1111-1120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 23. | Qiu Y, Wang S, Wang B, Yu Y, Zhu F, Zhu Z. Incidence and risk factors of neurological deficits of surgical correction for scoliosis: analysis of 1373 cases at one Chinese institution. Spine (Phila Pa 1976). 2008;33:519-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 94] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 24. | Murphy RF, Mooney JF 3rd. Complications following spine fusion for adolescent idiopathic scoliosis. Curr Rev Musculoskelet Med. 2016;9:462-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 61] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non-Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Indonesia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Peng B, China; Yan ZQ, China S-Editor: Liu JH L-Editor: Filipodia P-Editor: Guo X