Published online Jan 18, 2024. doi: 10.5312/wjo.v15.i1.52
Peer-review started: September 11, 2023
First decision: November 23, 2023
Revised: November 28, 2023
Accepted: December 19, 2023
Article in press: December 19, 2023
Published online: January 18, 2024
Processing time: 127 Days and 1.7 Hours
Distal humerus elbow fractures are one of the most common traumatic fractures seen in pediatric patients and present as three main types: Supracondylar (SC), lateral condyle (LC), and medial epicondyle (ME) fractures.
To evaluate the epidemiology of pediatric distal humerus fractures (SC, LC, and ME) from an American insurance claims database.
A retrospective review was performed on patients 17 years and younger with the ICD 9 and 10 codes for SC, LC and ME fractures based on the IBM Truven MarketScan® Commercial and IBM Truven MarketScan Medicare Supplemental databases. Patients from 2015 to 2020 were queried for treatments, patient age, sex, length of hospitalization, and comorbidities.
A total of 1133 SC, 154 LC, and 124 ME fractures were identified. SC fractures had the highest percentage of operation at 83%, followed by LC (78%) and ME frac
In the insurance claims databases used, SC fractures were the most reported, followed by LC fractures, and finally ME fractures. Age was identified to be a factor for how a pediatric distal humerus fractures, with patients with SC and LC fractures being younger than those with ME fractures. The peak age per injury per sex was similar to reported historic central tendencies, despite reported trends for younger physiologic development.
Core Tip: In this insurance claims databases used, supracondylar (SC) fractures were the most reported, followed by lateral condyle (LC) and finally medial epicondyle (ME) fractures. Age was identified to be a factor for how a pediatric distal humerus fractures, with patients with SC and LC fractures being younger than those with ME fractures. The peak age per injury per sex was similar to reported historic central tendencies, despite reported trends for younger physiologic development.
- Citation: Klahs KJ, Dertinger JE, Mello GT, Thapa K, Sandler AB, Garcia EJJ, Parnes N. Epidemiologic investigation of pediatric distal humerus fractures: An American insurance claims database study. World J Orthop 2024; 15(1): 52-60
- URL: https://www.wjgnet.com/2218-5836/full/v15/i1/52.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i1.52
Distal humerus fractures are one of the most common traumatic fractures seen in pediatric patients and present as three main types: Supracondylar (SC), lateral condyle (LC), and medial epicondyle (ME) fractures[1]. Historically, SC fractures are the most common with LC and ME fractures trailing after in incidence[1-3].
The pattern in which the pediatric distal humerus fractures is heavily influenced by both the force vector of injury as well as the remaining unfused ossification centers at the elbow[4,5]. SC fractures typically occur in children aged 5-10 years and are the result of a fall onto an outstretched arm[3-6]. LC fractures typically occur in children aged 4-10 years and are the result of a varus or valgus applied force to the elbow in extension[7]. ME fractures typically present in an older age group at 9-14 years[1,2,8-10]. Etiology consists of either trauma or an avulsion type injury from an overpull of the flexor-pronator mass[8-10].
The ossification centers and fusion at the elbow follow a very predictable sequential pattern[4,5]. Factors that influence the timing of ossification center fusion include injury across the physis, systemic diseases such as diabetes and hypothyroidism, endogenous stress hormones, and elevated estrogen at puberty[11]. Earlier ages of puberty have been observed in American children over the past three decades[12-14]. This phenomenon has implications for the age and injury pattern seen in American children now, in comparison with historic epidemiologic data.
The purpose of this study was to identify current epidemiologic data for pediatric distal humerus fractures between 2015-2020 in two insurance claims databases. The goal was to distinguish possible anthropometric differences with historic data. We hypothesized an overall younger central tendency for each of these injuries as compared to historic data, with a larger effect in females when compared with male patients. The clinical application of this investigation is intended to better predict injury patterns and counsel patients on modes of treatment.
From January 2015 to December 2020, we identified 1411 patients with an ICD 9 or 10 code designating them as having a SC, LC, or ME fracture. We included the ICD 9 codes 812.41 and 812.51 as well as the ICD 10 codes S42.41 and S42.42 (SC fractures). Also, ICD 9 codes 812.42 and 812.52 as well as ICD 10 code S42.45 (LC fractures) were included. Finally, we included ICD 9 codes 812.43 and 812.53 as well as ICD 10 code S42.44 (ME fractures). Selected patients were queried for CPT code treatments, patient age, sex, length of hospitalization, and comorbidities.
The patients were identified in the IBM Truven MarketScan® Commercial and IBM Truven MarketScan Medicare Supplemental databases. These databases contain de-identified, integrated, person-specific claim data. They are a conglomerate of three separate patient populations. The largest segment contains health information from participating large company employer-based health insurance, the second contains Medicare beneficiaries with supplemental insurance provided by their employer, and the third includes 11 contributing state’s Medicaid health information.
Data was organized by injury, patient age, and sex. Central tendency was calculated between the 25th and 75th percentiles. The distribution of continuous variables was assessed by the Kolmogorov-Smirnov test, and those with a normal distribution were analyzed by the unpaired t-test. Ordinal data was analyzed by the Chi-Square test or one-way analysis of variance for multiple variables. The comparison of proportions test was utilized for percentage analysis. Data entries were considered statistically significant if P < 0.05.
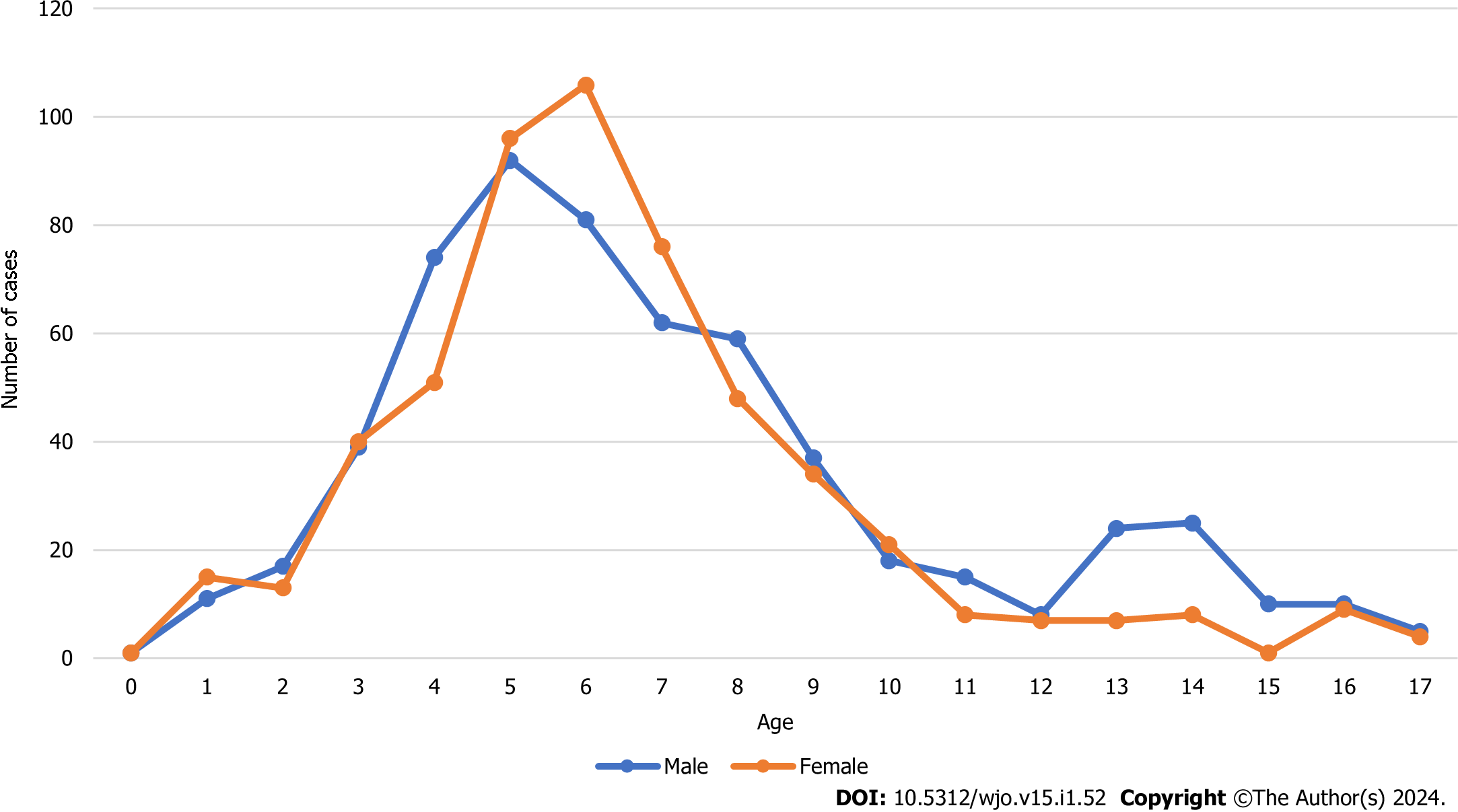
There were a total of 1133 patients with SC fractures at an average age of 6.76 ± 3.31 years, and 52% were male. There were 939 operative patients, 54% of which were male. Operative SC fracture patients were younger than nonoperative patients (6.32 ± 2.81 years vs 8.86 ± 4.53 years, P < 0.0001). The average age of male patients with SC fractures was 7.04 ± 3.56 years, with 50% having a fall between the ages of 5 and 9 years. The average age of female patients with SC fractures was 6.45 ± 2.98 years, with 50% having a fall between the ages of 5 and 7 years. Male patients were older than female patients (7.04 ± 3.56 years vs 6.45 ± 2.98 years, P =0.002) (Table 1, Figure 1).
| Treatment | Number of patients | Age (yr) | Male (%) |
| All SC patients | 1133 | 6.76 ± 3.31 | 52 |
| SC non-operative | 194 | 8.86 ± 4.53 | 54 |
| SC operative | 939 | 6.32 ± 2.81 | 52 |
| SC non-operative vs operative | P < 0.0001 | P = 0.61 | |
| SC male | 588 | 7.04 ± 3.56 | 100 |
| SC female | 545 | 6.45 ± 2.98 | 0 |
| SC male vs female | P = 0.002 |
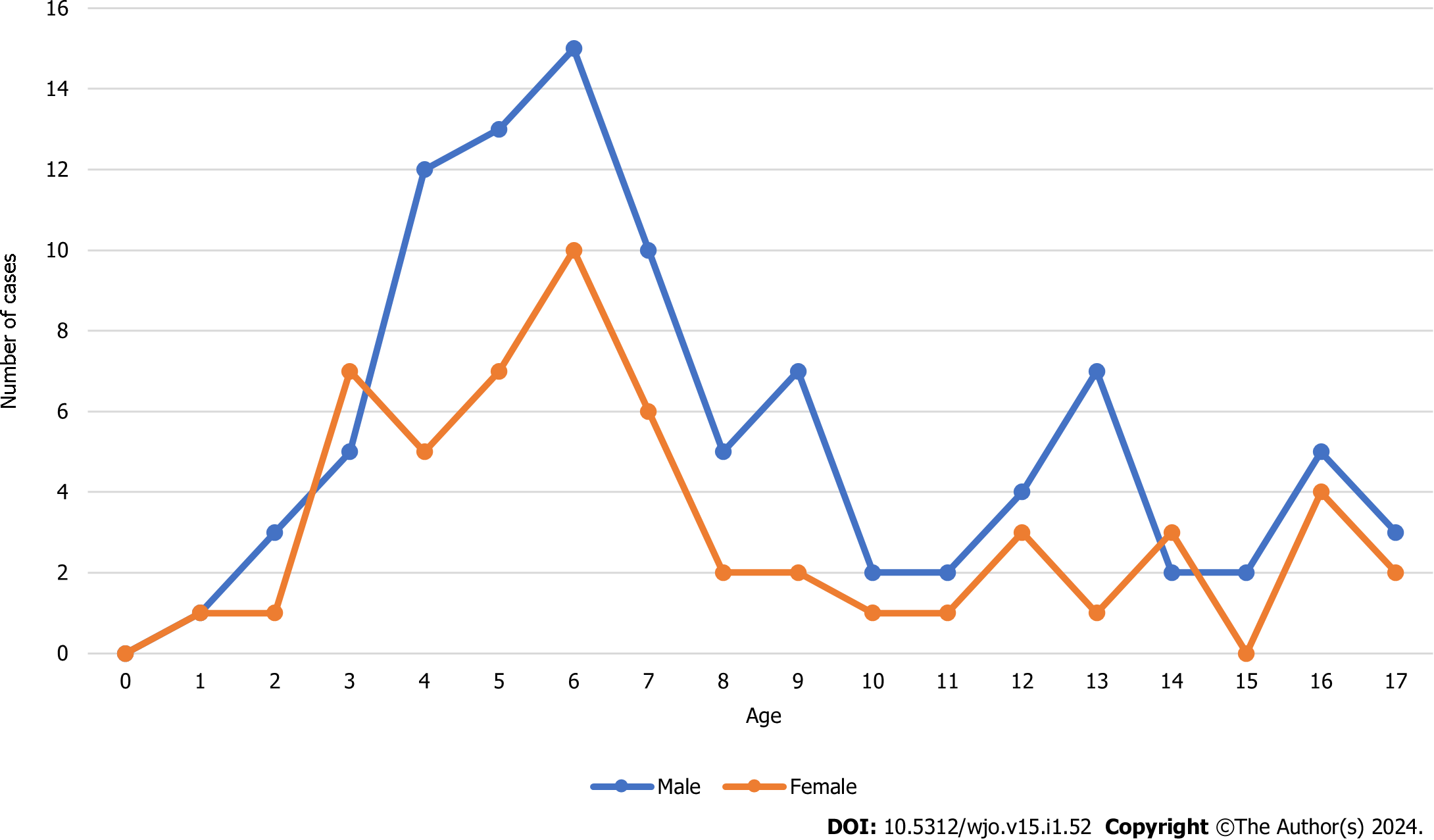
There were a total of 154 patients with LC fractures with an average age of 7.75 ± 4.2 years, and 64% were male. There were 120 operative patients, 63% of which were male. Operative LC fracture patients were older than nonoperative patients (9.62 ± 4.91 years vs 7.22 ± 3.81 years, P = 0.009). The average age of male patients with LC fractures was 7.84 ± 4.1 years, with 50% having a fall between the ages of 5 and 10 years. The average age of female patients with LC fractures was 7.59 ± 4.38 years, with 50% having a fall between the ages of 4 and 10 years (Table 2, Figure 2).
| Treatment | Number of patients | Age (yr) | Male (%) |
| All LC patients | 154 | 7.75 ± 4.2 | 64 |
| LC non-operative | 34 | 7.22 ± 3.81 | 65 |
| LC operative | 120 | 9.62 ± 4.91 | 63 |
| LC non-operative vs operative | P = 0.009 | P = 0.83 | |
| LC male | 98 | 7.84 ± 4.1 | 100 |
| LC female | 56 | 7.59 ± 4.38 | 0 |
| LC male vs female | P = 0.72 |
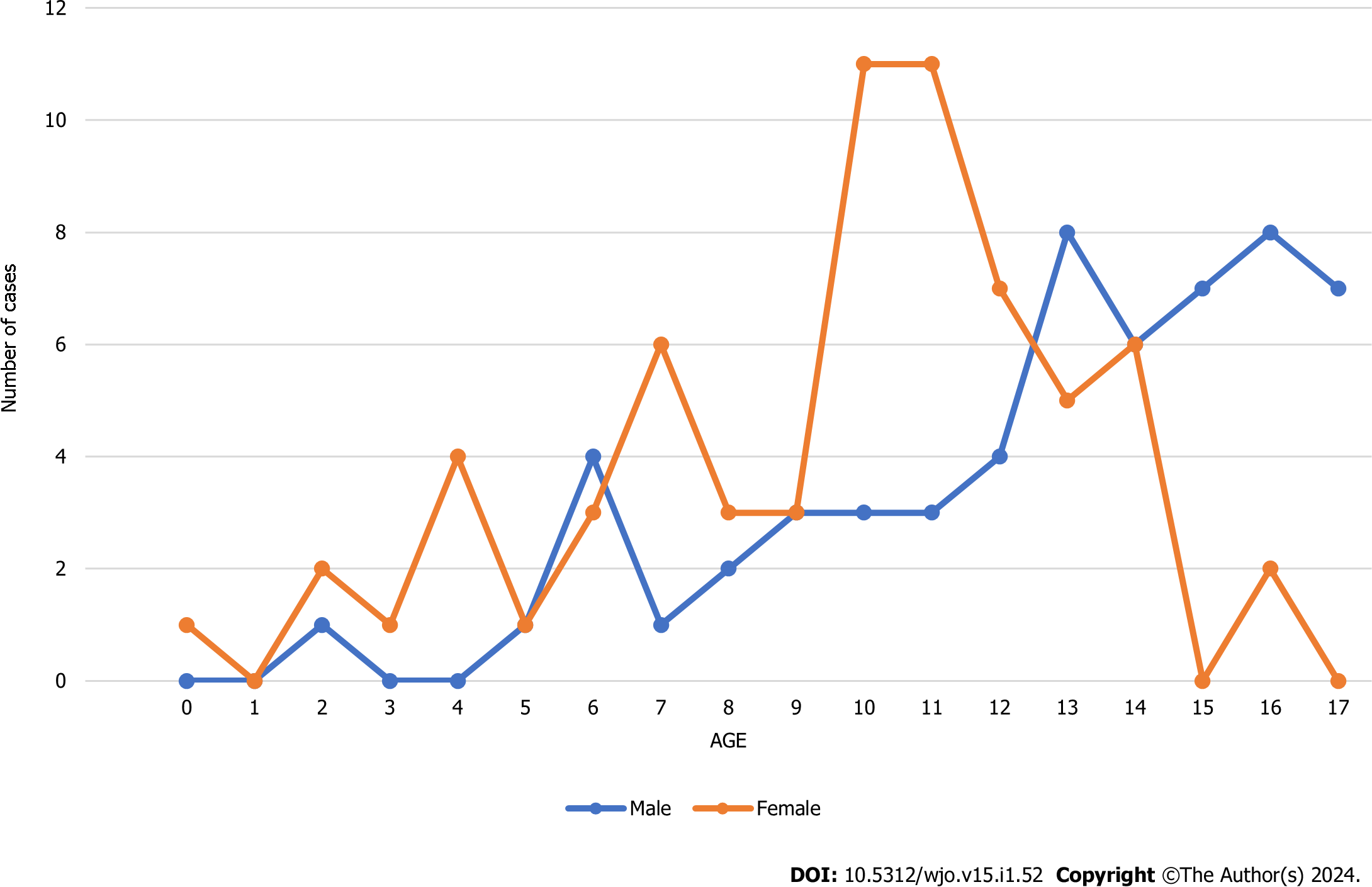
There were a total of 124 patients with ME fractures with an average age of 11 ± 3.86 years, and 47% were male. There were 51 operative patients, 45% of which were male. Operative ME fracture patients were older than nonoperative patients (12 ± 2.58 years vs 10 ± 4.43 years, P = 0.0045). The average age of male patients with ME fractures was 12.62 ± 3.67 years, with 50% having a fall between the ages of 10 and 15 years. The average age of female patients with ME fractures was 9.62 ± 3.52 years, with 50% having a fall between the ages of 7 and 12 years. Male patients were older than female patients (12 ± 3.67 years vs 9.62 ± 3.52 years, P < 0.0001) (Table 3, Figure 3).
| Treatment | Number of patients | Age (yr) | Male (%) |
| All ME patients | 124 | 11 ± 3.86 | 47 |
| ME non-operative | 73 | 10 ± 4.43 | 48 |
| ME operative | 51 | 12 ± 2.58 | 45 |
| ME non-operative vs operative | P = 0.0045 | P = 0.74 | |
| ME male | 58 | 12.62 ± 3.67 | 100 |
| ME female | 66 | 9.62 ± 3.52 | 0 |
| ME male vs female | P ≤ 0.0001 |
When comparing across injury types, there was a statistically significant difference in the percentage of operative patients between SC and ME (83% vs 41%, P < 0.0001), and between LC and ME (78% vs 41%, P < 0.0001). Operative SC fracture patients were younger than those with LC (6.32 ± 2.81 years vs 9.62 ± 4.91 years, P < 0.0001) as well as ME fractures (6.32 ± 2.81 years vs 12 ± 2.58 years, P < 0.0001). Operative LC fracture patients were younger than those with ME fractures (9.62 ± 4.91 years vs 12 ± 2.58 years, P = 0.001). There was a statistical difference in sex among operative patients with SC (52% male), LC (63% male), and ME fractures (45% male) (P < 0.05; Table 4).
| Treatment | Total | Percentage of total (%) | Age (yr) | Male (%) |
| Operative SC | 939 | 83 | 6.32 ± 2.81 | 52 |
| Operative LC | 120 | 78 | 9.62 ± 4.91 | 63 |
| Operative ME | 51 | 41 | 12 ± 2.58 | 45 |
| Operative SC vs LC | P = 0.13 | P < 0.0001 | P = 0.03 | |
| Operative SC vs ME | P < 0.0001 | P < 0.0001 | P = 0.01 | |
| Operative LC vs ME | P < 0.0001 | P = 0.001 | P = 0.002 |
Pediatric distal humerus fractures are commonly encountered and therefore warrant continued epidemiologic investigation. SC fractures were the most represented in this study, followed by LC and finally ME fractures. American children may be undergoing developmental changes at earlier timepoints than in previous generations or in non-Western countries. This study identified differences in age and sex among the three injury types as well as in operative rate among injury types, with ME fractures having the lowest and SC fractures the highest operative rate.
Multiple contemporary studies have identified younger ages at which American female children and, to a lesser extent, male children undergo puberty[12-14]. A leading theory is directly linked with the simultaneous youth obesity epidemic in America[15-17]. Adiposity increases circulating estrogen and not only can initiate puberty, but it also has been found to directly close the physis[11,17-20]. Despite these population-wide trends, the effect on the distal humerus physis has not been shown in the orthopaedic literature. Peering back on previously published epidemiologic studies provides a comparison to our current landscape. One of the earliest pediatric elbow fracture epidemiologic studies collected the data from 1950-1979 in Sweden and found the average age of patients to be 7.4 ± 3.1 years for SC, 8.7 ± 3.9 years for LC, and ME 12 ± 2.3 years for ME fractures[21]. More recently, a Canadian study published results from 2002-2010 and found an interquartile range of 3 to 6 years for all SC fractures[22]. Epidemiologic data has been published on non-Western populations with lower childhood obesity rates[23,24]. A 2013 Iranian study identified 8.1 ± 2.31 years old as the average age for all pediatric elbow fractures[25]. Similarly, an Indonesian study collecting data between 2009 to 2018 found the average age for all pediatric elbow fractures at 7.3 years[26]. In the American patient databases used, we did not observe any large age shifts from previous generations or for non-Western countries. Additional comparison studies can be found in Supplementary material[5,20-22,27-52].
Our study identified differences in patient sex distribution across the various fracture types. The 1998 study by Cheng et al[5] identified the sequence for the six pediatric elbow ossification centers and demonstrated that males lag about two years behind females. Our data coincides with the sex differences in ossification centers and physeal maturation, with male patients being older than female patients on average in SC and ME fractures[4,5]. The highest percentage of operative male patients was noted in those with LC fractures, while the lowest percent operative males was seen in those with ME fractures. In previous studies, ME fractures occur more frequently in a male population, likely due to mismatch between muscular strength and ME fusion site[7-9]. Our study identified more female ME fracture patients, possibly due to the increase in overall ligamentous laxity, larger elbow carrying angle, and continued increased involvement of women in overhead athletics[53-58].
There were several limitations to this study. The data is retrospective in nature and were collected from de-identified insurance claims databases, so we were unable to read operative notes, review radiology exams, and analyze patient factors such as mode of injury, time from injury, body mass index, and follow-up. We also could only compare chronologic age and not bone age, which may be a better metric for this age group.
In the insurance claims databases used, SC fractures were the most reported, followed by LC and finally ME fractures. Age was identified to be a factor for how a pediatric distal humerus fractures, with SC and LC fracture patients being younger than ME fracture patients. The peak age per injury per sex is similar to reported historic central tendencies, despite reported trends for younger physiologic development. These results will help more accurately predict the type and treatment of distal humerus fractures in the American pediatric population.
Distal humerus fractures are one of the most common traumatic fractures seen in pediatric patients and present as three main types: Supracondylar (SC), lateral condyle (LC), and medial epicondyle (ME) fractures and as such warrant continued, updated epidemiological evaluation.
The American pediatric population may be physiologically maturing at younger ages as compared to previous generations. This study aimed to look at common pediatric elbow injuries in relation to age and sex.
To explore patient age, sex, injury type, and treatment type for three common distal humerus fractures.
A retrospective database review was performed.
SC fractures were the most reported, followed by LC and finally ME fractures.
Age is a factor for how a pediatric distal humerus fractures, with patients with SC and LC fractures being younger than those with ME fractures.
The peak age per injury per sex is similar to reported historic central tendencies, despite reported trends for younger physiologic development.
We acknowledge Abby G. Klahs, B.S. for statistical support. We acknowledge Rachel K. Klahs, B.A. for English language review.
| 1. | Saeed W, Waseem M. Elbow Fractures Overview. 2023 Aug 7. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. [PubMed] |
| 2. | Gottschalk HP, Eisner E, Hosalkar HS. Medial epicondyle fractures in the pediatric population. J Am Acad Orthop Surg. 2012;20:223-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 106] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 3. | Abzug JM, Herman MJ. Management of supracondylar humerus fractures in children: current concepts. J Am Acad Orthop Surg. 2012;20:69-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 63] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 4. | Patel B, Reed M, Patel S. Gender-specific pattern differences of the ossification centers in the pediatric elbow. Pediatr Radiol. 2009;39:226-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 52] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 5. | Cheng JC, Wing-Man K, Shen WY, Yurianto H, Xia G, Lau JT, Cheung AY. A new look at the sequential development of elbow-ossification centers in children. J Pediatr Orthop. 1998;18:161-167. [PubMed] |
| 6. | Tom JE, Eckhoff MD, Tadlock JC, Garcia EJ. A 10-Year National Analysis of Pediatric Elbow Fractures. Clin Pediatr (Phila). 2023;62:433-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 7. | Abzug JM, Dua K, Kozin SH, Herman MJ. Current Concepts in the Treatment of Lateral Condyle Fractures in Children. J Am Acad Orthop Surg. 2020;28:e9-e19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 47] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 8. | Beck JJ, Bowen RE, Silva M. What's New in Pediatric Medial Epicondyle Fractures? J Pediatr Orthop. 2018;38:e202-e206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 9. | Ogawa K, Yoshida A, Matsumura N, Inokuchi W. Fracture-Separation of the Medial Humeral Epicondyle Caused by Arm Wrestling: A Systematic Review. Orthop J Sports Med. 2022;10:23259671221087606. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 10. | Hallwachs A, Weber M, Liu R, Baldwin K, Mistovich J. Operative Management of Pediatric Medial Epicondyle Fractures: Lessons Better Learned the Easy Way: Current Concept Review. J Pediatr Orthop Soc North Am Nov. 2021;3. [DOI] [Full Text] |
| 11. | Ağırdil Y. The growth plate: a physiologic overview. EFORT Open Rev. 2020;5:498-507. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 64] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 12. | Biro FM, Greenspan LC, Galvez MP. Puberty in girls of the 21st century. J Pediatr Adolesc Gynecol. 2012;25:289-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 99] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 13. | Herman-Giddens ME, Slora EJ, Wasserman RC, Bourdony CJ, Bhapkar MV, Koch GG, Hasemeier CM. Secondary sexual characteristics and menses in young girls seen in office practice: a study from the Pediatric Research in Office Settings network. Pediatrics. 1997;99:505-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1220] [Cited by in RCA: 974] [Article Influence: 33.6] [Reference Citation Analysis (0)] |
| 14. | Herman-Giddens ME, Steffes J, Harris D, Slora E, Hussey M, Dowshen SA, Wasserman R, Serwint JR, Smitherman L, Reiter EO. Secondary sexual characteristics in boys: data from the Pediatric Research in Office Settings Network. Pediatrics. 2012;130:e1058-e1068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 216] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 15. | Gurnani M, Birken C, Hamilton J. Childhood Obesity: Causes, Consequences, and Management. Pediatr Clin North Am. 2015;62:821-840. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 200] [Article Influence: 18.2] [Reference Citation Analysis (1)] |
| 16. | Chavarro JE. Invited Commentary: Childhood Adiposity and the Onset of Puberty-It Turns Out There Is More to Be Learned. Am J Epidemiol. 2022;191:17-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 17. | Deardorff J, Reeves JW, Hyland C, Tilles S, Rauch S, Kogut K, Greenspan LC, Shirtcliff E, Lustig RH, Eskenazi B, Harley K. Childhood Overweight and Obesity and Pubertal Onset Among Mexican-American Boys and Girls in the CHAMACOS Longitudinal Study. Am J Epidemiol. 2022;191:7-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 18. | Frisch RE. Body fat, menarche, fitness and fertility. Hum Reprod. 1987;2:521-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 192] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 19. | Rosenfield RL, Lipton RB, Drum ML. Thelarche, pubarche, and menarche attainment in children with normal and elevated body mass index. Pediatrics. 2009;123:84-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 254] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 20. | Schubert CM, Chumlea WC, Kulin HE, Lee PA, Himes JH, Sun SS. Concordant and discordant sexual maturation among U.S. children in relation to body weight and BMI. J Adolesc Health. 2005;37:356-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Landin LA, Danielsson LG. Elbow fractures in children. An epidemiological analysis of 589 cases. Acta Orthop Scand. 1986;57:309-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 145] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 22. | Khoshbin A, Leroux T, Wasserstein D, Wolfstadt J, Law PW, Mahomed N, Wright JG. The epidemiology of paediatric supracondylar fracture fixation: a population-based study. Injury. 2014;45:701-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 23. | Taghizadeh S, Khodayari-Zarnaq R, Farhangi MA. Childhood obesity prevention policies in Iran: a policy analysis of agenda-setting using Kingdon's multiple streams. BMC Pediatr. 2021;21:250. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 24. | Sulistiadi W, Kusuma D, Amir V, Tjandrarini DH, Nurjana MA. Growing Up Unequal: Disparities of Childhood Overweight and Obesity in Indonesia's 514 Districts. Healthcare (Basel). 2023;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 25. | Behdad A, Behdad S, Hosseinpour M. Pediatric elbow fractures in a major trauma center in iran. Arch Trauma Res. 2013;1:172-175. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 26. | Sananta P, Sintong L, Prasetio B, Putera MA, Andarini S, Kalsum U, Dradjat RS. Elbow Fracture in Children at Saiful Anwar General Hospital, Nine Years Experiences. Open Access Maced J Med Sci. 2019;7:4069-4071. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 27. | Holt JB, Glass NA, Shah AS. Understanding the Epidemiology of Pediatric Supracondylar Humeral Fractures in the United States: Identifying Opportunities for Intervention. J Pediatr Orthop. 2018;38:e245-e251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 79] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 28. | Pilla NI, Rinaldi J, Hatch M, Hennrikus W. Epidemiological Analysis of Displaced Supracondylar Fractures. Cureus. 2020;12:e7734. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 29. | Anjum R, Sharma V, Jindal R, Singh TP, Rathee N. Epidemiologic pattern of paediatric supracondylar fractures of humerus in a teaching hospital of rural India: A prospective study of 263 cases. Chin J Traumatol. 2017;20:158-160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 30. | Baig MN. A Review of Epidemiological Distribution of Different Types of Fractures in Paediatric Age. Cureus. 2017;9:e1624. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 31. | Ip D, Tsang WL. Medial humeral epicondylar fracture in children and adolescents. J Orthop Surg (Hong Kong). 2007;15:170-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 32. | Haxhija EQ, Mayr JM, Grechenig W, Höllwarth ME. Treatment of medial epicondylar apophyseal avulsion injury in children. Oper Orthop Traumatol. 2006;18:120-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 33. | Lee HH, Shen HC, Chang JH, Lee CH, Wu SS. Operative treatment of displaced medial epicondyle fractures in children and adolescents. J Shoulder Elbow Surg. 2005;14:178-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 74] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 34. | Farsetti P, Potenza V, Caterini R, Ippolito E. Long-term results of treatment of fractures of the medial humeral epicondyle in children. J Bone Joint Surg Am. 2001;83:1299-1305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 107] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 35. | Pimpalnerkar AL, Balasubramaniam G, Young SK, Read L. Type four fracture of the medial epicondyle: a true indication for surgical intervention. Injury. 1998;29:751-756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 36. | Duun PS, Ravn P, Hansen LB, Buron B. Osteosynthesis of medial humeral epicondyle fractures in children. 8-year follow-up of 33 cases. Acta Orthop Scand. 1994;65:439-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 29] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 37. | Skak SV, Grossmann E, Wagn P. Deformity after internal fixation of fracture separation of the medial epicondyle of the humerus. J Bone Joint Surg Br. 1994;76:297-302. [PubMed] |
| 38. | Fowles JV, Slimane N, Kassab MT. Elbow dislocation with avulsion of the medial humeral epicondyle. J Bone Joint Surg Br. 1990;72:102-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 89] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 39. | Wilson NI, Ingram R, Rymaszewski L, Miller JH. Treatment of fractures of the medial epicondyle of the humerus. Injury. 1988;19:342-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 51] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 40. | Hines RF, Herndon WA, Evans JP. Operative treatment of Medial epicondyle fractures in children. Clin Orthop Relat Res. 1987;170-174. [PubMed] |
| 41. | Dias JJ, Johnson GV, Hoskinson J, Sulaiman K. Management of severely displaced medial epicondyle fractures. J Orthop Trauma. 1987;1:59-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 44] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 42. | van Niekerk JL, Severijnen RS. Medial epicondyle fractures of the humerus. Neth J Surg. 1985;37:141-144. [PubMed] |
| 43. | Papavasiliou VA. Fracture-separation of the medial epicondylar epiphysis of the elbow joint. Clin Orthop Relat Res. 1982;172-174. [PubMed] |
| 44. | Bede WB, Lefebvre AR, Rosman MA. Fractures of the medial humeral epicondyle in children. Can J Surg. 1975;18:137-142. [PubMed] |
| 45. | Milch H. FRACTURES AND FRACTURE DISLOCATIONS OF THE HUMERAL CONDYLES. J Trauma. 1964;4:592-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 148] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 46. | Jakob R, Fowles JV, Rang M, Kassab MT. Observations concerning fractures of the lateral humeral condyle in children. J Bone Joint Surg Br. 1975;57:430-436. [PubMed] |
| 47. | Badelon O, Bensahel H, Mazda K, Vie P. Lateral humeral condylar fractures in children: a report of 47 cases. J Pediatr Orthop. 1988;8:31-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 72] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 48. | Marcheix PS, Vacquerie V, Longis B, Peyrou P, Fourcade L, Moulies D. Distal humerus lateral condyle fracture in children: when is the conservative treatment a valid option? Orthop Traumatol Surg Res. 2011;97:304-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 38] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 49. | Flynn JC, Richards JF Jr, Saltzman RI. Prevention and treatment of non-union of slightly displaced fractures of the lateral humeral condyle in children. An end-result study. J Bone Joint Surg Am. 1975;57:1087-1092. [PubMed] |
| 50. | Conner AN, Smith MG. Displaced fractures of the lateral humeral condyle in children. J Bone Joint Surg Br. 1970;52:460-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 32] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 51. | Launay F, Leet AI, Jacopin S, Jouve JL, Bollini G, Sponseller PD. Lateral humeral condyle fractures in children: a comparison of two approaches to treatment. J Pediatr Orthop. 2004;24:385-391. [PubMed] |
| 52. | Hardacre JA, Nahigian SH, Froimson AI, Brown JE. Fractures of the lateral condyle of the humerus in children. J Bone Joint Surg Am. 1971;53:1083-1095. [PubMed] |
| 53. | Cruz AI Jr, Steere JT, Lawrence JT. Medial Epicondyle Fractures in the Pediatric Overhead Athlete. J Pediatr Orthop. 2016;36 Suppl 1:S56-S62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 54. | Hansen M, Kjaer M. Sex Hormones and Tendon. Adv Exp Med Biol. 2016;920:139-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 59] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 55. | Sharma K, Mansur DI, Khanal K, Haque MK. Variation of carrying angle with age, sex, height and special reference to side. Kathmandu Univ Med J (KUMJ). 2013;11:315-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 56. | Wright CL, Patel J, Hettrich CM. Sports-Related Shoulder Injuries Among Female Athletes. Curr Rev Musculoskelet Med. 2022;15:637-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 57. | Farana R, Strutzenberger G, Exell T, Skypala J, Wiltshire H, Irwin G. Sex differences in elbow and wrist joint loading during the cartwheel and round off with different hand positions performed by young gymnasts. J Sports Sci. 2019;37:1449-1456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 58. | Beals RK. The normal carrying angle of the elbow. A radiographic study of 422 patients. Clin Orthop Relat Res. 1976;194-196. [PubMed] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Govindarajan KK, India S-Editor: Qu XL L-Editor: Wang TQ P-Editor: Chen YX