Published online Oct 18, 2023. doi: 10.5312/wjo.v14.i10.763
Peer-review started: May 31, 2023
First decision: July 19, 2023
Revised: August 16, 2023
Accepted: September 6, 2023
Article in press: September 6, 2023
Published online: October 18, 2023
Processing time: 137 Days and 11.1 Hours
Proximal femur fractures, including both intracapsular (femoral neck fractures) and extracapsular fractures (intertrochanteric femoral fractures, IFFs), affect around 1.5 million people per year worldwide. Mechanical failures of inter
To describe the surgical complexity and the procedure-related complication rates in patients with trochanteric nailing failure and treated with THA.
Patients referred to our level I trauma center between April 2012 and July 2018 with failed cephalomedullary nailing following trochanteric fractures were retrospectively recruited. All patients underwent a salvage surgical procedure, i.e., cephalomedullary nail removal and conversion to THA. The same surgical and anesthesiology team performed the surgical procedures under spinal anesthesia. All patients underwent clinical and radiographic follow-ups for at least 24 mo. Complications and re-operations were recorded.
Seventy-four patients met the inclusion criteria (male: 29; female: 45; mean age: 73.8-years-old; range: 65-89) and were included in the current study. The average operative time was 117 min (76-192 min). The average blood loss was 585 mL (430-1720 mL). Among the 74 patients, 43 (58.1%) required transfusion of three or more blood units. Two patients died within the 4th d after surgery because of pulmonary embolism, and 1 patient died 9 mo after surgery due to ischemic myocardial infarction. The complication rate in the 71 patients who completed the minimum 24-mo follow-up was 22.5%. In 3 cases out of 71 (4.2%) periprosthetic acetabular fracture was observed during the follow-up. One of these periacetabular fractures occurred intraoperatively. An intraoperative periprosthetic femur fracture was observed in 5 patients out of 71 (7.0%). Four of these patients needed a re-operation to fix the fracture with plates and cerclages; in one of these patients, femoral stem revision was also necessary. In 4 patients out of 71 (5.6%), an early THA dislocation was observed, whereas in 1 case (1.4%) a late THA dislocation was observed. Three patients out of 71 (4.2%) developed a periprosthetic joint infection during the study follow-up.
The present study demonstrated that salvage options for IFF fixation failure are complex procedures with a relevant intraoperative and postoperative complication rate.
Core Tip: The present study demonstrated that salvage options for intertrochanteric femoral fracture fixation failure deal with intraoperative and postoperative complications at a higher rate compared to primary elective total hip arthroplasty.
- Citation: Solarino G, Bizzoca D, Dramisino P, Vicenti G, Moretti L, Moretti B, Piazzolla A. Total hip arthroplasty following the failure of intertrochanteric nailing: First implant or salvage surgery? World J Orthop 2023; 14(10): 763-770
- URL: https://www.wjgnet.com/2218-5836/full/v14/i10/763.htm
- DOI: https://dx.doi.org/10.5312/wjo.v14.i10.763
Proximal femur fractures (PFFs), including both intracapsular (femoral neck fractures, FNFs) and extracapsular fractures (intertrochanteric femoral fractures, IFFs), affect around 1.5 million people per year worldwide, thus constituting a major public health problem[1]. PFFs are the most common traumatic injuries in elderly people and significantly impact patients’ health status, potentially leading to a reduced quality of life, increased disability and higher mortality rate[1,2]. In Italy, PFFs have an estimated annual prevalence of 78000, with 90% of injuries occurring in patients older than 65 years[3]. Nonetheless, as life expectancy is constantly increasing, the annual number is supposed to steadily increase by reaching 8.2 million fractures in 2050 worldwide[3-6].
IFFs, accounting for more than 60% of PFFs, have an annual mortality rate of 15%-20%[4]. It has also been reported that the incidence of IFF is increasing more than the incidence of PFF in the elderly[7]. Fox et al[7], in a prospective study on 923 elderly patients comparing patients with IFF and FNF, observed that patients with IFFs were older and showed a worse pre-injury health status. They also were less likely to recover to the pre-fracture level of functioning at the 2-mo follow-up.
IFFs need surgical management and could be treated both with intramedullary and extramedullary implants[1,3]. However, a recent meta-analysis by Zhang et al[8] stated that the current evidence indicates short intramedullary nails may be a better choice than dynamic hip screws in the treatment of IFFs. Compared to dynamic hip screws, intra
The surgical planning of IFFs and implant choice is critically influenced by the stability of the fracture pattern[9]. A stable fracture resists displacement after adequate reduction and fixation and generally includes two fragment fractures with an intact posteromedial cortical calcar[9]. The intact medial buttress allows the proximal femur to redistribute stress and resist medial compressive loads[10]. On the other hand, an unstable fracture may collapse even after adequate reduction and fixation[10]. Unstable patterns include fractures with a compromised medial calcar (comminuted patterns or fractures with a large posteromedial fragment), fractures with a subtrochanteric extension, reverse obliquity fractures, or intertrochanteric fractures that involve the lateral cortical wall[9,10].
Treatment of unstable fractures is still challenging, and several factors may influence the surgical technique and implant choice[9,10]. Cephalomedullary nailing revealed a biomechanical superiority compared with an extramedullary fixation for unstable fracture patterns since it can resist higher loading forces and provide greater stability reducing the distance from the implant and the hip joint diminishing the bending moment across the implant/fracture construct[11-15]. Fixation failure after surgery to treat IFF is a serious complication. Many factors seem to influence the stability of the fixation during follow-up including the patient’s age, female sex, poor bone quality, device choice, fracture reduction quality, and presence of neurological comorbidities that may affect the rehabilitation process[16].
This study aimed to describe the surgical complexity and the procedure-related complication rates, in patients referring with trochanteric nailing failure and treated with total hip arthroplasty (THA) or hemiarthroplasty.
Patients referred to our level I trauma center between April 2012 and July 2018 with failed trochanteric nailing were retrospectively recruited according to inclusion and exclusion criteria. Ethical clearance was obtained from our center’s clinical research ethics board as per the 1964 Declaration of Helsinki, and all patients gave informed consent before enrolment in the study.
The inclusion criteria included: age greater than 65-years-old; good cognitive state; and osteoporosis, defined as lumbar T-score ≤ -2.5 (all patients performed a DEXA scan during hospitalization). The exclusion criteria included: Moderate cognitive impairment (defined as mini-mental state examination < 19); a history of malignant neoplasm; hemoglobin < 10 g/dL at baseline; severely obese patients, i.e., body mass index ≥ 35 kg/m2; a life expectancy of fewer than 3 mo; medical illness or cognitive disorders precluding participation in the follow-up examination; concomitant lower-limb fractures; and traumatic head injury.
Patient demographics, including age, sex, body mass index, and comorbidities were recorded at recruitment. All patients underwent THA via the Hardinge approach, with the patient positioned in lateral decubitus. Adhesions were cleared around scar tissue, fully exposing the trochanter and enabling assessment of the greater and lesser trochanters and calcar femoral. The surgical procedures were performed by the same surgical and anesthesiology team under spinal anesthesia.
Cefazolin (2 g intravenously) or, if contraindicated, clindamycin (600 mg i.v.) was given 60 min before incision. Subcutaneous injection of low molecular-weight heparin (enoxaparin 4000 UI once a day, started 12 h after surgery) was administered for antithrombotic prophylaxis in all patients until the return to full weight-bearing.
Surgical time, blood transfusion rate and perioperative and major complications were assessed. All patients underwent a minimum 24-mo clinical and radiographic follow-up. Complications and reoperations were recorded.
Statistical analysis was performed using STATA/MP 14 for Windows (StataCorp LP, College Station, United States). All data were described as mean, median, and standard deviation.
The main data of the study are reported in Table 1. Seventy-four patients met the inclusion and exclusion criteria (male: 29; female: 45; mean age: 73.8-years-old; range: 65-89) and were included in the current study. The recruited patients were originally referred with the following fracture patterns: 31-A1.2 (58 out of 74; 78.38%); 31-A1.3 (9 out of 74; 12.16%); 31-A2.2 (5 out of 74; 6.76%); and 31- A2.3 (2 out of 74; 2.7%).
| Item | Patients, n = 74 |
| Age in yr | |
| mean ± SD | 73.80 ± 7.85 |
| Range | 65-89 |
| Sex | |
| Female | 45 (60.8) |
| BMI in kg/m2 | |
| mean ± SD | 28.70 ± 4.43 |
| Side | |
| Right | 43 (58.1) |
| Mean operating time in min, mean ± SD | 77.0 ± 35.5 |
| Patients undergoing ≥ 3, blood transfusion | 43 (58.1) |
The trochanteric nail failure modality included: cut-out in 39 cases out of 74 (50.65%); non-union in 13 patients out of 74 (17.56%); peri-implant fracture in 12 patients out of 74 (16.20%); cut-through in 8 patients out of 74 (10.80%); and femoral head avascular necrosis in 2 patients out of 74 (2.70%).
The average operation time was 117 min (76-192 min). The average blood loss was 585 mL (430-1720 mL). Among the 74 patients, 43 patients (58.10%) required transfusion of three or more blood units.
All the patients underwent nail conversion to THA. Cemented stems were used in 19 patients out of 64 (25.68%), whereas uncemented stems were employed in 55 patients out of 74 (74.32%). Among the latter, long stems were used in 39 patients out of 74 (52.70%). Cemented cups were implanted in 18 patients out of 74 (24.32%), whereas in 56 patients out of 74 (75.68%) cementless cups were used. Dual-mobility cups were implanted in 16 patients out of 74 (21.62%).
Table 2 shows the complications observed during the study follow-up. Seventy-one patients completed the minimum 24 mo of clinical and radiological follow-up (range: 25-85 mo). Two patients (2.70%) died within 4 d after surgery because of pulmonary embolism. One patient (1.35%) died 9 mo after surgery due to ischemic myocardial infarction. The overall complication rate in the 71 patients who completed the minimum 24-mo follow-up was 22.5%.
| Item | Patients, n = 74 |
| Dead | 3 (4.00) |
| Periprosthetic acetabular fractures | 3 (4.00) |
| Periprosthetic femoral fractures | 5 (6.76) |
| THA dislocation | 5 (6.76) |
| Periprosthetic joint infections | 3 (4.00) |
In 3 cases (4.23%) periprosthetic acetabular fracture was observed during the follow-up. One of these periacetabular fractures occurred intraoperatively. In 5 patients (7.00%), an intraoperative periprosthetic femur fracture was observed. Four of these patients needed a re-operation to fix the fracture with plates and cerclages; in one of these patients, femoral stem revision was also necessary. In 4 patients (5.60%) an early THA dislocation was observed, and 1 case (1.40%) a late THA dislocation was observed.
Three patients (4.23%) developed a periprosthetic joint infections (PJI) during the study follow-up. Two of them were early treated with debridement, antibiotics, irrigation, and retention of the prosthesis protocol; the other one was a late-onset infection requiring the THA explant and definitive conversion to Girdlestone procedure.
Table 3 shows the study data detailed by patients’ sexes. Note that a higher percentage of perioperative complications was observed in male patients.
| Item | Males, n = 29 | Females, n = 45 | P value |
| Age in yr | |||
| mean ± SD | 72.90 ± 9.85 | 74.40 ± 8.65 | 0.087 |
| Range | 67-89 | 65-87 | |
| BMI in kg/m2 | |||
| mean ± SD | 28.60 ± 4.03 | 28.90 ± 4.55 | 0.650 |
| Side | |||
| Right | 17 (58.62) | 26 (57.78) | 0.580 |
| Operating time in min, mean ± SD | 84.0 ± 41.50 | 72.22 ± 32.34 | 0.003a |
| Patients undergoing ≥ 3, blood transfusion | 19 (65.50) | 24 (53.30) | 0.002a |
| Complications | |||
| Dead | 2 (6.89) | 1 (2.22) | 0.0011 |
| Periprosthetic acetabular fractures | 2 (6.89) | 1 (2.22) | 0.001a |
| Periprosthetic femoral fractures | 1 (3.45) | 4 (8.90) | 0.001a |
| THA dislocation | 2 (6.89) | 3 (6.70) | 0.630 |
| Periprosthetic joint infections | 2 (6.89) | 1 (2.22) | 0.001a |
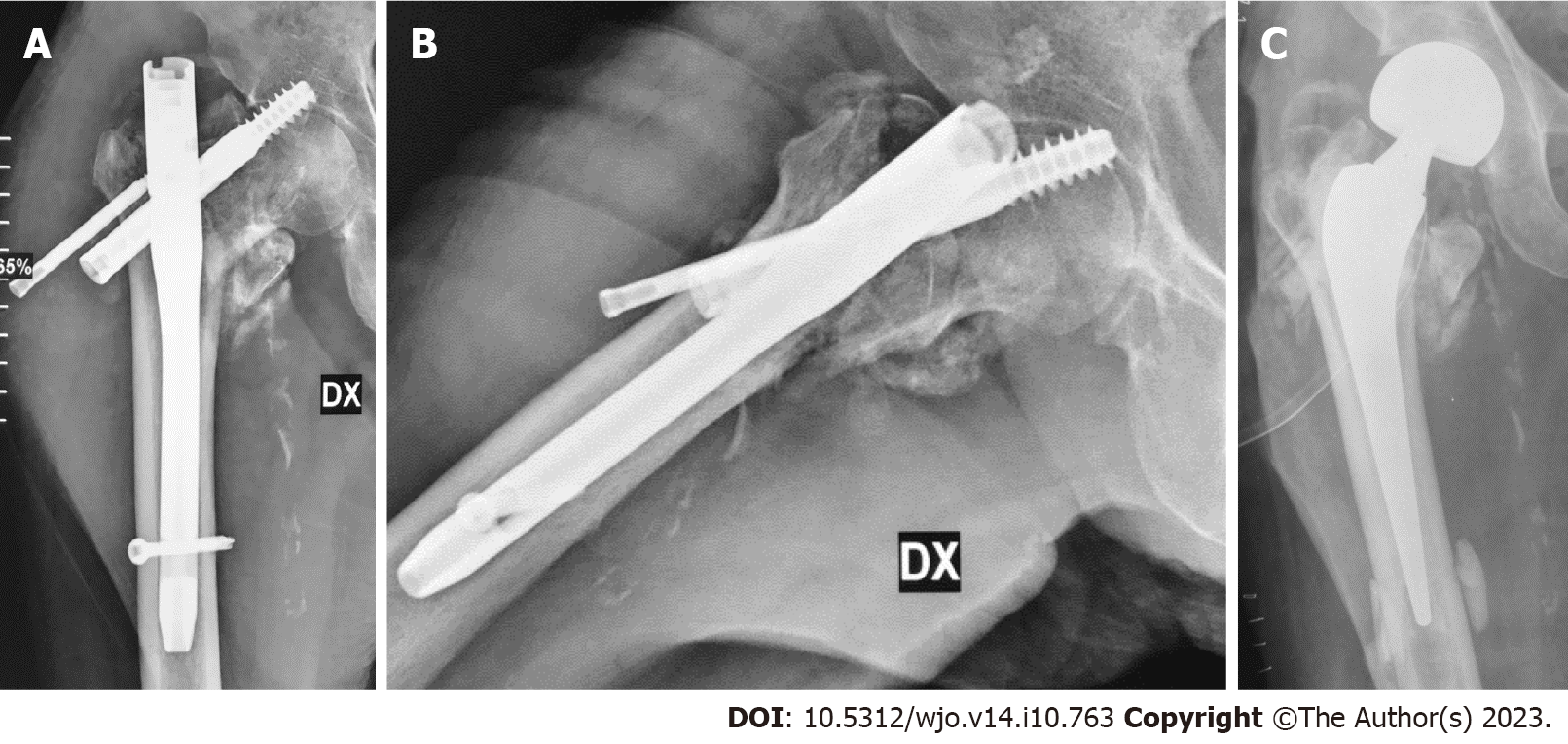
Figure 1 shows a case of complex femoral nailing failure in a female patient aged 81.
IFF is a common fracture injury among the elderly. Conservative treatment can result in prolonged periods in bed and/or lower limb shortening with varus deformity and is limited to very unstable patients with high perioperative risk[17]. Surgical treatment with cephalomedullary nails, compression hip screws, and the paracortical proximal plate has become the standard of care[9]. Despite the advanced acknowledge and skills in the surgical management of IFF, internal fixation is often associated with significant failure, ranging from 3%-12%.
The patients at increased risk of failure are the elderly, females, and osteoporotic patients[18,19]. Fixation failure depends on several factors, including poor bone quality, fracture comminution and biomechanical stability, quality of reduction, and fixation. Despite several technological improvements that have been produced in the last two decades, fixation failure due to mechanical and biological complications still occurs and can lead to potentially devastating scenarios[20-23]. Mechanical complications are cut-out, cut-through, peri-implant fractures, or implant fractures.
The most common mechanical complication observed in our study was the lateral mobilization of the cephalic screw, i.e., cutting out (55.71% of cases). Many factors are associated with a higher risk of cut-out, including a tip-to-apex distance greater than 25 mm, an unstable fracture pattern, an inadequate fracture reduction that may lead to a varus deformity of the femoral neck, and positioning of lag screw outside of the center-center or inferior center of the femoral neck[24-26]. The medial mobilization of the cephalic screw or blade toward the hip joint is also called cut-through.
Salvage procedures currently used for failed internal fixation of IFF are revision osteosynthesis or conversion to hip arthroplasty. The term salvage procedures in patients undergoing salvage surgeries are used to indicate a considerable decrease in pain level and an increase in functional recovery after treatment[27-34].
Revision osteosynthesis is mostly utilized in patients younger than 50-years-old, with high life expectancy and satisfactory bone quality[27,28]. It implies femoral head sparing and re-fixation performed via hardware exchange (blade/screw), bone graft augmentation (autologous or allograft) acting as a plug-in case of joint perforation, and a new blade/screw insertion either cemented or uncemented[29]. On the other hand, conversion to THA as a salvage option is preferred for elderly patients with severely impaired articular surfaces allowing early weight bearing and mobilization[20,21,29]. As already mentioned, salvage THA is a complex procedure and includes several technical hurdles hindering successful surgical outcomes including bone loss and/or deformity, poor bone stock, and the presence of non-union or malunion[20].
Our study differentiated salvage procedure-related complications into intraoperative and postoperative complications. Intraoperatively, we considered major complications, such as an increased skin-to-skin operative time compared to primary THA implant, intraoperative blood loss, and intraoperative fractures. Intraoperative fractures were the most common intraoperative complication including one acetabular fracture and five femoral fractures occurring during acetabular reaming and femoral canal broaching, respectively. They may be related to a combination of factors such as previous osteoporosis, incomplete fracture union, and weakening of the bone after hardware removal.
Intraoperative acetabular fractures may be related to disuse osteopenia and/or the presence of previous osteoporosis. Great trochanter fractures may be attributable to an amount of bone loss to the medial aspect of the greater trochanter due to a wider diameter of proximal nails, a lateral entry site of the lag screw in the greater trochanter, and excessive stress during hardware removal[35].
Skin-to-skin operative time and intraoperative bleeding were higher. Compared to patients undergoing primary THA, salvage procedures require two steps. The first operative time includes adhesion clearance around scar tissue, exposure of the greater trochanter, and hardware removal. The second operative time includes prosthetic joint implantation. This procedure is challenging and technically demanding because of distorted proximal femur anatomy, poor bone stock, medial or lateral wall incompetence, and the presence of screw holes causing potential cement extrusion[30,31].
During the postoperative period after patient discharge, complications were further categorized as early major and late major complications. Early major complications included four cases of dislocation and two PJIs. Late major complications included 1 case of late dislocation and 1 case of periprosthetic infection.
Early postoperative dislocation is an important orthopedic complication after the salvage of THA. The dislocation rate in patients undergoing salvage arthroplasty after fixation failure of IFF seems to be higher compared to patients undergoing primary THA or salvage arthroplasty for FNF. This complication may be related to many factors: loss of abductor mechanism; shortening of limb length; and misorientation of prosthetic components[32].
The surgical site infection risk rate increases with an increasing number of revision surgeries performed. Our results (two early and one late PJI), similar to other results available within the current literature, revealed an increased PJI rate in salvage options compared to primary elective THA[36,37].
Surgical treatment for IFF fixation failure is a challenging procedure. Despite updated surgical skills in the surgical management of IFF, internal fixation failure rates are diagnosed in up to 12% of cases. Salvage options are the mainstay of their treatment allowing early weight bearing and stimulating functional recovery to the pre-injury level. This study analyzed difficulties during a salvage procedure, i.e., cephalomedullary nail removal and THA implant, after failed fixation of IFF. The present study demonstrated that salvage options for IFF fixation failure deal with intraoperative and postoperative complications at a higher rate than primary elective THA. Based on the present study findings, it is mandatory to adequately plan the surgical treatment in patients with PFFs since high rates of perioperative local and systemic complications are more common during revision surgery (or a salvage procedure).
Proximal femur fractures (PFFs), including both intracapsular (femoral neck fractures) and extracapsular fractures (intertrochanteric femoral fractures, IFFs), affect around 1.5 million people per year worldwide. Mechanical failures of intertrochanteric nailing in IFFs could be managed with revision total hip arthroplasty (THA).
To assess if the conversion of failed nailing to THA in patients with previous PFFs has a high perioperative complication rate.
To describe the surgical complexity and the procedure-related complication rates, in patients referring with trochanteric nailing failure and treated with THA
Patients referred to our level I trauma center between April 2012 and July 2018 with failed cephalomedullary nailing following trochanteric fractures were retrospectively recruited. All patients underwent a salvage surgical procedure, i.e., cephalomedullary nail removal and conversion to THA. The surgical procedures were performed by the same surgical and anesthesiology team under spinal anesthesia. All patients underwent clinical and radiographic follow-ups for a minimum of 24 mo. Complications and re-operations were recorded.
Seventy-four patients met the inclusion criteria (male: 29; female: 45; mean age: 73.8-years-old; range: 65-89) and were included in the current study. The average operative time was 117 min (76-192 min). The average blood loss was 585 mL (430-1720 mL). Of the 74 patients, 43 patients (58.1%) required transfusion of three or more blood units. Two patients died within the 4th d after surgery because of pulmonary embolism. One patient died 9 mo after surgery due to ischemic myocardial infarction. The complication rate in the 71 patients who completed the minimum 24-mo follow-up was 22.50%. In 3 cases (4.23%) periprosthetic acetabular fracture was observed during the follow-up. One of these periacetabular fractures occurred intraoperatively. An intraoperative periprosthetic femur fracture was observed in 5 patients (7.00%). Four of these patients needed a re-operation to fix the fracture with plates and cerclages; in one of these patients, femoral stem revision was also necessary. In 4 patients (5.60%) an early THA dislocation was observed, whereas in 1 patient (1.40%) a late THA dislocation was observed. Three patients (4.23%) developed a periprosthetic joint infection during the study follow-up.
The present study demonstrated that salvage options for IFF fixation failure are complex procedures with a relevant intraoperative and postoperative complication rate.
Based on the present study findings, it is mandatory to adequately plan the surgical treatment in patients with PFFs since a revision surgery has a risk of high rates of perioperative local and systemic complications.
| 1. | Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl DA, Cooper C; IOF Working Group on Epidemiology and Quality of Life. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int. 2012;23:2239-2256. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1083] [Cited by in RCA: 1047] [Article Influence: 74.8] [Reference Citation Analysis (0)] |
| 2. | Mattisson L, Bojan A, Enocson A. Epidemiology, treatment and mortality of trochanteric and subtrochanteric hip fractures: data from the Swedish fracture register. BMC Musculoskelet Disord. 2018;19:369. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 169] [Cited by in RCA: 206] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 3. | Innocenti M, Civinini R, Carulli C. Proximal femoral fractures: Epidemiology. Cases in Miner and Bone Metabol. 2009;6:117-119. [DOI] [Full Text] |
| 4. | Sambrook P, Cooper C. Osteoporosis. Lancet. 2006;367:2010-2018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 936] [Cited by in RCA: 953] [Article Influence: 47.7] [Reference Citation Analysis (0)] |
| 5. | Piazzolla A, Bizzoca D, Solarino G, Moretti L, Moretti B. Vertebral fragility fractures: clinical and radiological results of augmentation and fixation-a systematic review of randomized controlled clinical trials. Aging Clin Exp Res. 2020;32:1219-1232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 6. | Veronese N, Maggi S. Epidemiology and social costs of hip fracture. Injury. 2018;49:1458-1460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 307] [Cited by in RCA: 629] [Article Influence: 78.6] [Reference Citation Analysis (0)] |
| 7. | Fox KM, Magaziner J, Hebel JR, Kenzora JE, Kashner TM. Intertrochanteric versus femoral neck hip fractures: differential characteristics, treatment, and sequelae. J Gerontol A Biol Sci Med Sci. 1999;54:M635-M640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 125] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 8. | Zhang K, Zhang S, Yang J, Dong W, Wang S, Cheng Y, Al-Qwbani M, Wang Q, Yu B. Proximal femoral nail vs. dynamic hip screw in treatment of intertrochanteric fractures: a meta-analysis. Med Sci Monit. 2014;20:1628-1633. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 9. | Tawari AA, Kempegowda H, Suk M, Horwitz DS. What makes an intertrochanteric fracture unstable in 2015? J Orthop Trauma. 2015;29 Suppl 4:S4-S9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 59] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 10. | Lu Y, Uppal HS. Hip Fractures: Relevant Anatomy, Classification, and Biomechanics of Fracture and Fixation. Geriatr Orthop Surg Rehabil. 2019;10:2151459319859139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 72] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 11. | Marsillo E, Pintore A, Asparago G, Oliva F, Maffulli N. Cephalomedullary nailing for reverse oblique intertrochanteric fractures 31A3 (AO/OTA). Orthop Rev (Pavia). 2022;14:38560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 70] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 12. | Queally JM, Harris E, Handoll HH, Parker MJ. Intramedullary nails for extracapsular hip fractures in adults. Cochrane Database Syst Rev. 2014;CD004961. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 53] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 13. | Bizzoca D, Bortone I, Vicenti G, Caringella N, Rifino F, Moretti B. Gait analysis in the postoperative assessment of intertrochanteric femur fractures. J Biol Regul Homeost Agents. 2020;34:345-351. [PubMed] |
| 14. | Méndez-Ojeda MM, Herrera-Rodríguez A, Álvarez-Benito N, González-Pacheco H, García-Bello MA, Álvarez-de la Cruz J, Pais-Brito JL. Treatment of Trochanteric Hip Fractures with Cephalomedullary Nails: Single Head Screw vs. Dual Integrated Compression Screw Systems. J Clin Med. 2023;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 15. | Zeelenberg ML, Nugteren LHT, Plaisier AC, Loggers SAI, Joosse P, Den Hartog D, Verhofstad MHJ, van Lieshout EMM; STABLE-HIP Study Group. Extramedullary versus intramedullary fixation of stable trochanteric femoral fractures: a systematic review and meta-analysis. Arch Orthop Trauma Surg. 2023;143:5065-5083. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Haidukewych GJ, Berry DJ. Hip arthroplasty for salvage of failed treatment of intertrochanteric hip fractures. J Bone Joint Surg Am. 2003;85:899-904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 138] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 17. | Valera M, Bonifacio L, Basman S. Outcome of surgery for unstable intertrochanteric fractures in octogenarians. Malays Orthop J. 2014;8:26-31. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Matre K, Havelin LI, Gjertsen JE, Vinje T, Espehaug B, Fevang JM. Sliding hip screw versus IM nail in reverse oblique trochanteric and subtrochanteric fractures. A study of 2716 patients in the Norwegian Hip Fracture Register. Injury. 2013;44:735-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 126] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 19. | Ovesen O, Andersen M, Poulsen T, Nymark T, Overgaard S, Rock ND. The trochanteric gamma nail versus the dynamic hip screw: a prospective randomised study. One-year follow-up of 146 intertrochanteric fractures. Hip Int. 2006;16:293-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Luthringer TA, Elbuluk AM, Behery OA, Cizmic Z, Deshmukh AJ. Salvage of failed internal fixation of intertrochanteric hip fractures: clinical and functional outcomes of total hip arthroplasty vs hemiarthroplasty. Arthroplast Today 2018; 4: 383-391. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 21. | Mabry TM, Prpa B, Haidukewych GJ, Harmsen WS, Berry DJ. Long-term results of total hip arthroplasty for femoral neck fracture nonunion. J Bone Joint Surg Am. 2004;86:2263-2267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 41] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 22. | Goodnough LH, Wadhwa H, Tigchelaar SS, DeBaun MR, Chen MJ, Graves ML, Gardner MJ. Indications for cement augmentation in fixation of geriatric intertrochanteric femur fractures: a systematic review of evidence. Arch Orthop Trauma Surg. 2022;142:2533-2544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 23. | Ibrahim I, Appleton PT, Wixted JJ, DeAngelis JP, Rodriguez EK. Implant cut-out following cephalomedullary nailing of intertrochanteric femur fractures: Are helical blades to blame? Injury. 2019;50:926-930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 24. | Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995;77:1058-1064. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 865] [Cited by in RCA: 912] [Article Influence: 29.4] [Reference Citation Analysis (0)] |
| 25. | Aicale R, Maffulli N. Greater rate of cephalic screw mobilisation following proximal femoral nailing in hip fractures with a tip-apex distance (TAD) and a calcar referenced TAD greater than 25 mm. J Orthop Surg Res. 2018;13:106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 26. | Haynes RC, Pöll RG, Miles AW, Weston RB. Failure of femoral head fixation: a cadaveric analysis of lag screw cut-out with the gamma locking nail and AO dynamic hip screw. Injury. 1997;28:337-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 120] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 27. | Lionel L, Guido C, Rodrigo B, Danilo T, Jorge B, Carlos S. Salvage procedure for cut-through after surgical fixation of trochanteric fractures with TFN. Eur J Orthop Surg Traumatol. 2022;32:611-618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 28. | Dziadosz D. Considerations with failed intertrochanteric and subtrochanteric femur fractures: how to treat, revise, and replace. J Orthop Trauma. 2015;29 Suppl 4:S17-S21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 29. | Angelini M, McKee MD, Waddell JP, Haidukewych G, Schemitsch EH. Salvage of failed hip fracture fixation. J Orthop Trauma. 2009;23:471-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 69] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 30. | Zhang B, Chiu KY, Wang M. Hip arthroplasty for failed internal fixation of intertrochanteric fractures. J Arthroplasty. 2004;19:329-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 102] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 31. | DeHaan AM, Groat T, Priddy M, Ellis TJ, Duwelius PJ, Friess DM, Mirza AJ. Salvage hip arthroplasty after failed fixation of proximal femur fractures. J Arthroplasty. 2013;28:855-859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 32. | Mortazavi SM, R Greenky M, Bican O, Kane P, Parvizi J, Hozack WJ. Total hip arthroplasty after prior surgical treatment of hip fracture is it always challenging? J Arthroplasty. 2012;27:31-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 75] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 33. | Taheriazam A, Saeidinia A. Salvage of failed dynamic hip screw fixation of intertrochanteric fractures. Orthop Res Rev. 2019;11:93-98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 34. | Srivastav S, Mittal V, Agarwal S. Total hip arthroplasty following failed fixation of proximal hip fractures. Indian J Orthop. 2008;42:279-286. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 39] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 35. | Exaltacion JJ, Incavo SJ, Mathews V, Parsley B, Noble P. Hip arthroplasty after intramedullary hip screw fixation: a perioperative evaluation. J Orthop Trauma. 2012;26:141-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 36. | Douglas SJ, Remily EA, Sax OC, Pervaiz SS, Delanois RE, Johnson AJ. How Does Conversion Total Hip Arthroplasty Compare to Primary? J Arthroplasty. 2021;36:S155-S159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 37. | Qin CD, Helfrich MM, Fitz DW, Oyer MA, Hardt KD, Manning DW. Differences in Post-Operative Outcome Between Conversion and Primary Total Hip Arthroplasty. J Arthroplasty. 2018;33:1477-1480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mostafavinia A, Iran; Veltman ES, Netherlands S-Editor: Chen YL L-Editor: Filipodia P-Editor: Chen YL