Published online Jul 18, 2022. doi: 10.5312/wjo.v13.i7.631
Peer-review started: February 26, 2022
First decision: April 13, 2022
Revised: April 30, 2022
Accepted: June 22, 2022
Article in press: June 22, 2022
Published online: July 18, 2022
Processing time: 141 Days and 9.2 Hours
Rotator cuff pathology is a very common source of shoulder pain. Similarly, osteoarthritis of the glenohumeral joint can cause shoulder pain and produce similar symptoms. Surgical management can be indicated for both pathologies, however, outcomes data is limited when examining rotator cuff repair (RCR) in the setting of glenohumeral arthritis (GHOA). Thus, this study sought to determine outcomes for patients who undergo RCR in the setting of GHOA.
To evaluate if a relationship exists between outcomes of RCR in the setting of GHOA.
This was a retrospective analysis of patients who underwent arthroscopic rotator cuff repair with concurrent glenohumeral osteoarthritis between 2010-2017. Patients were stratified based on rotator cuff tear size and glenohumeral osteoarthritis severity. Cohorts were paired 1:1 with patients without glenohumeral osteoarthritis. Patients included had a minimum two year follow-up. Rate of conversion to total shoulder arthroplasty, complication rates following initial surgery, and patient-reported outcome measures were collected.
A total of 142 patients were included. The number of patients that required total shoulder arthroplasty within two years after index surgery was low. 2/71 (2.8%) patients with GHOA, and 1/71 (1.4%) without GHOA. Following rotator cuff repair, both groups showed favorable patient-reported outcomes.
Patients with glenohumeral osteoarthritis who underwent arthroscopic rotator cuff repair showed comparable outcomes to patients without glenohumeral osteoarthritis.
Core Tip: We evaluated a cohort of patients with mild to moderate glenohumeral arthritis who underwent rotator cuff repair. We retrospectively reviewed 71 patients with glenohumeral osteoarthritis (GHOA) (Glenohumeral Arthritis) who underwent concomitant rotator cuff repair, and matched these patients to 71 patients who underwent rotator cuff repair without GHOA. We evaluated patient reported outcomes and demographic information for both cohorts.
- Citation: Hong IS, Rao AJ, CarlLee TL, Meade JD, Hurwit DJ, Scarola G, Trofa DP, Schiffern SC, Hamid N, Connor PM, Fleischli JE, Saltzman BM. Outcomes after arthroscopic repair of rotator cuff tears in the setting of mild to moderate glenohumeral osteoarthritis. World J Orthop 2022; 13(7): 631-643
- URL: https://www.wjgnet.com/2218-5836/full/v13/i7/631.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i7.631
Rotator cuff pathology is a common source of shoulder pain. A significant proportion of individuals have rotator cuff tears with increasing age and can become disabled[1-3]. In older patients, onset of new symptoms correlate to the progression of rotator cuff tear size and increasing morbidity[3].
Like rotator cuff pathology, glenohumeral osteoarthritis (GHOA) is related to advancing age and is estimated to affect 16%-20% of adults over age 65[4,5]. It can be debilitating and a source of shoulder dysfunction, pain, and loss of motion[6,7].
Although rotator cuff pathology and GHOA are two prevalent shoulder pathologies, there are limited studies evaluating the relationship of GHOA to outcomes after rotator cuff repair (RCR)[8-11]. Cases of severe GHOA accompanied by rotator cuff pathology are most appropriately managed with either reverse total shoulder arthroplasty (RTSA) or total SA (TSA) with RCR. However, a recent study by Jeong et al[8] suggests that patients with mild GHOA and repair of large rotator cuff tears fare similarly to their counterparts without GHOA in terms of clinical outcomes and progression to GHOA. In contrast, another study found that GHOA was associated with lower outcome scores after RCR at 1-year follow-up[10].
Studies have shown that patients with concomitant GHOA and rotator cuff tears can range from 13%-27% of patients treated for rotator cuff tears; to our knowledge, the outcomes of these patients after RCR are lacking within literature[12,13]. This study evaluated the effect of the presence or absence of GHOA on short and mid-term clinical outcomes after arthroscopic repair of small to large rotator cuff tears, comparing the rates of conversion to shoulder arthroplasty (TSA or RTSA) as well as PROM’s at follow-up > 2 years from their RCR surgery. We hypothesized there would be no significant differences in clinical outcomes or rates of subsequent conversion to shoulder arthroplasty in patients with small to large rotator cuff tears undergoing arthroscopic repair with or without concurrent GHOA.
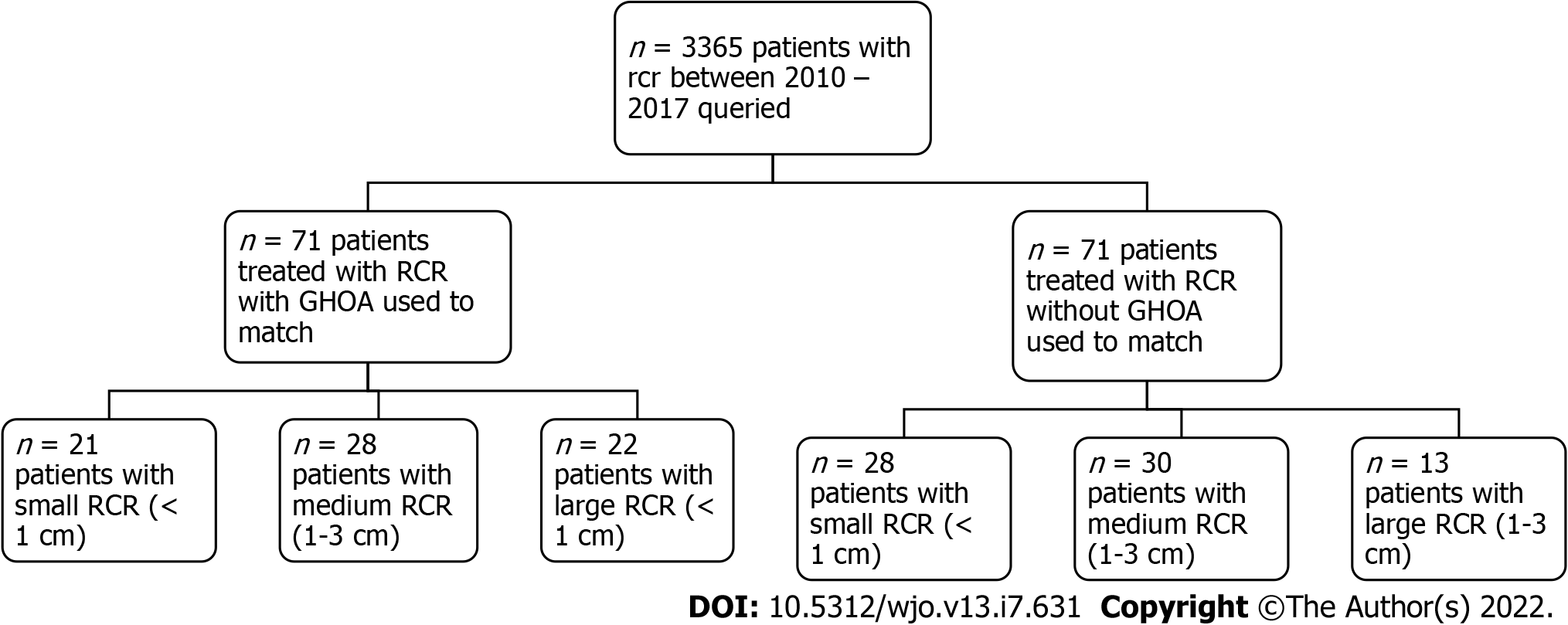
Following International Review Board approval, patients who underwent arthroscopic RCR of small (< 1 cm), medium (1-3 cm), or large (3-5 cm) rotator cuff tears with GHOA were identified at a large single-center academic orthopedic group. All patients treated between January 2010 and June 2017 were identified using Current Procedural Terminology code 29827 for “arthroscopy, shoulder, surgical, with rotator cuff repair.” Patients with GHOA were initially identified and paired with patients without GHOA. The three criteria for matching the patients involved: Age ± 3 years, clinical follow-up ± 1 year, and same sex (Figure 1A).
Inclusion criteria consisted of patients who: (1) Were 18 years old at the time of index surgery; (2) Had a rotator cuff tear measuring 0-5 cm; (3) Had a preoperative plain radiograph; (4) Had a preoperative magnetic resonance imaging (MRI); and (5) Had a minimum of 2 year follow-up after their index RCR procedure. Patients were excluded if they had any of the following: (1) Open physes; (2) Post-traumatic osteoarthritis; (3) Post-dislocation glenohumeral arthropathy; (4) Avascular necrosis; (5) Prior surgical intervention on the ipsilateral shoulder; and/or (6) Autoimmune conditions such as rheumatoid arthritis. The data was collected and stored using REDCap electronic data capture tools hosted at OrthoCarolina Research Institute[4].
The primary outcome variable was the rate of conversion to TSA or RTSA within 2 years from the index surgery. Secondary outcomes were clinical patient-reported outcome measures (PROs) including American Shoulder and Elbow Surgeons (ASES) score, Single Assessment Numeric Evaluation (SANE), VAS for pain, and Veterans RAND 12-Item Health Survey (VR-12).
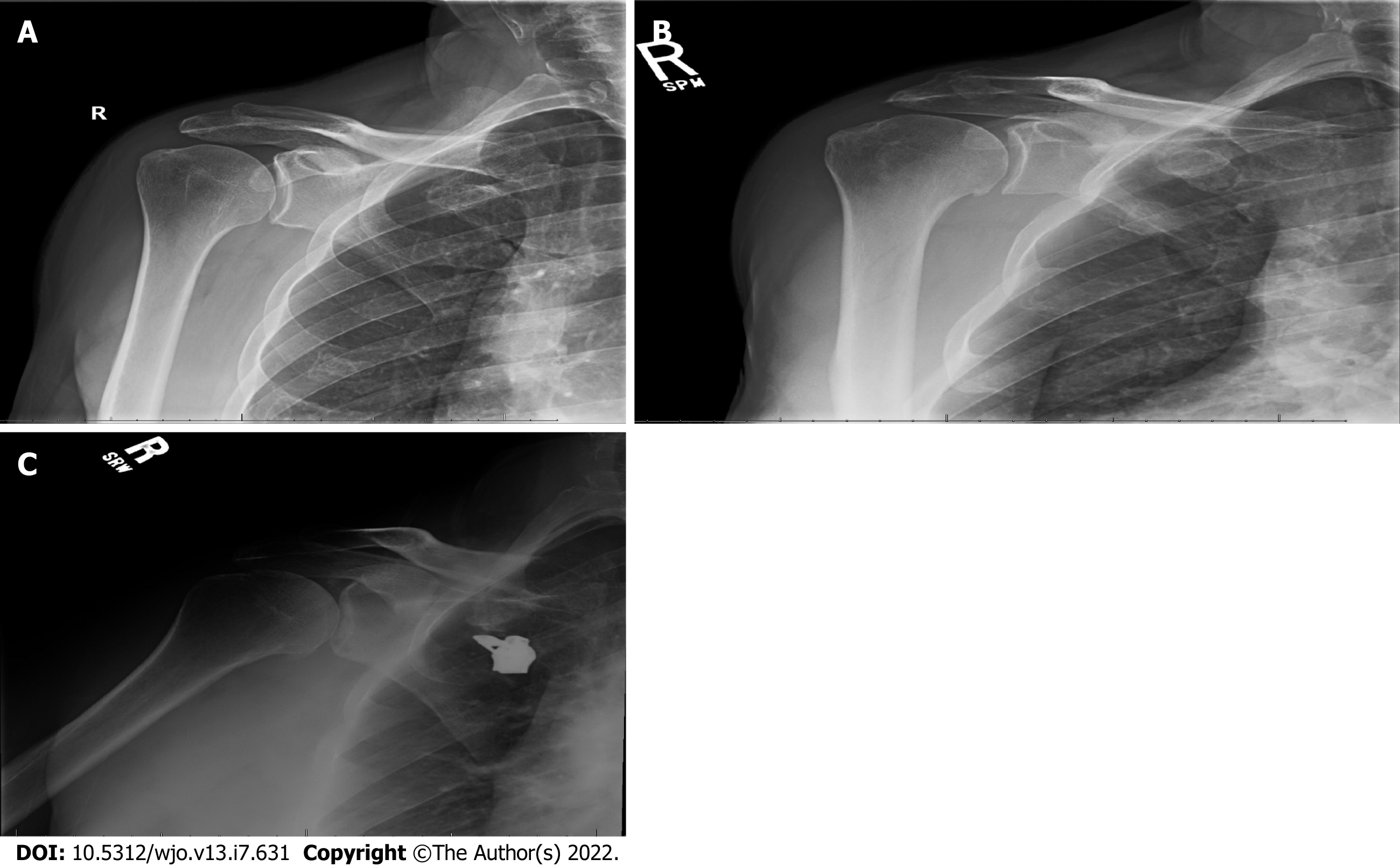
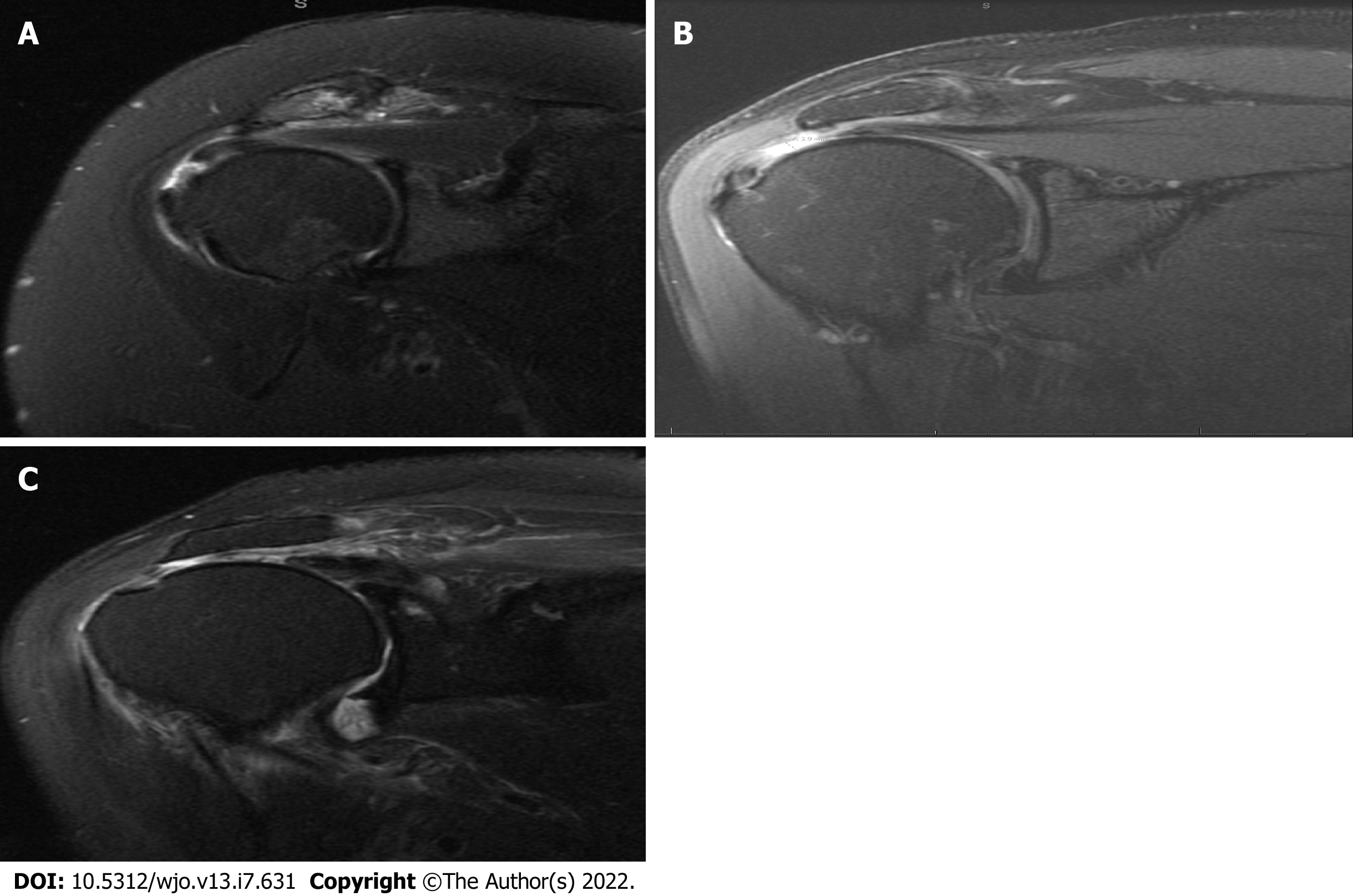
Demographical information such as age, sex, body mass index (BMI), smoking history, diabetes, and injury mechanism (ultra-low vs low vs high energy) where applicable was obtained. Using preoperative plain radiographs and MRI, the Samilson-Priesto Classification (Figure 2), Goutallier classification, and Warner atrophy grade were obtained to assess GHOA severity, fatty degeneration of rotator cuff muscles, and muscle atrophy, respectively. Each patient was classified based on the presence of GHOA in the setting of a small, medium, or large rotator cuff tear (Figure 3). The different rotator cuff tear sizes, largely based on level of retraction, were determined by two independent fellowship trained sports medicine and shoulder orthopedic surgeons using MRI imaging. Coronal oblique images were obtained and used to identify the tears, and were classified as either small (< 1 cm) medium (1-3 cm) and massive (< 5 cm).
The procedural variables captured using operative notes included: surgical technique, fixation technique, and concomitant procedures (e.g., distal clavicle excision, subacromial decompression, capsular release, debridement, chondroplasty, biceps tenotomy, and/or biceps tenodesis). Postoperative variables were measured: complications, re-operation (s) and the type of secondary procedure. PROs following surgery were collected during routine clinical follow-up at 2 or more years. Patients without the standard of care 2-year follow-up were contacted via phone or email to answer questions regarding PROs, subsequent rotator cuff re-tear, or re-operation outside of our institution.
All data underwent descriptive statistical analysis using SAS version 9.4 (SAS Institute, Cary, NC; http://www.sas.com/software/sas9). Two groups were defined based on presence or absence of primary GHOA and stratified based on rotator cuff tear size. For normally distributed continuous data, mean and standard deviation, were reported. For non-parametric continuous data, median and interquartile range were reported. Frequencies and proportions were reported for categorical variables. A Wilcoxon rank sum test was used for non-parametric continuous variables and a two-sample t test was used for normally distributed data. For categorical variables, a chi-square test (or Fisher’s exact test, where appropriate) was used for comparisons between groups. Significance was determined by an alpha level of 0.05.
Between January 2010 and June 2017, 71 patients were identified that underwent arthroscopic RCR of small to large tears with the presence of GHOA. These patients were subsequently matched with 71 patients without GHOA that underwent the same procedure.
The demographics of the comparison study groups can be found in Table 1. The median age at time of rotator cuff repair was 64 years (IQR 60, 70) for patients in both groups. They had an exact match by sex and 57.7% (41/71) of repairs were performed in males in each respective group. Median BMI at the time of repair was 29.8 (IQR 26.7, 33.2) and 28.5 (IQR 25.5, 31) respectively. In patients with GHOA, 57.7% (41/71) reported having never smoked tobacco products, 40.8% (29/71) have smoked previously and 1.4% (1/71) were actively smoking. In patients without GHOA, 60.6% (43/71) reported having never smoked tobacco products, 33.8% (24/71) have smoked previously and 5.6% (4/71) were actively smoking.
| With GHOA | Without GHOA | ||||||||
| Tear size group | Tear size group | ||||||||
| Overall (n = 142) | Case overall (n = 71) | Small (0-1 cm) (n = 21) | Medium (1-3 cm) (n = 28) | Large (3-5 cm) (n = 22) | Control overall (n = 71) | Small (0-1 cm) (n = 28) | Medium (1-3 cm) (n = 30) | Large (3-5 cm) (n = 13) | |
| Age (in yr) at surgery, median (IQR) | 64 (60, 70) | 64 (60, 70) | 63 (62, 67) | 63 (58, 67.5) | 66 (62, 71) | 64 (60, 70) | 63 (59.5, 68.5) | 65 (61, 70) | 63 (61, 69) |
| BMI, median (IQR) | 29.2 (25.8, 32.9) | 29.8 (26.7, 33.2) | 32.9 (29.4, 35.9) | 28.1 (24.5, 30.8) | 29 (27.3, 33.2) | 28.5 (25.5, 31) | 29.9 (27, 31) | 27.2 (24.5, 30.4) | 27.5 (24.7, 32.1) |
| Time (in yr) since DOS, median (IQR) | 8.1 (6.9, 9.3) | 8.2 (6.9, 9.3) | 8 (7.1, 9.4) | 8 (6.4, 9.3) | 8.3 (7.1, 8.9) | 8.1 (6.8, 9.3) | 8.3 (6.8, 9.6) | 8 (7.5, 8.8) | 7.8 (6.9, 9.3) |
| Tear size, median (IQR) | 2 (1, 3) | 2 (1, 3.5) | 1 (1, 1) | 2 (1.7, 2.6) | 4 (3.5, 4) | 1.5 (1, 2.5) | .5 (.5, 1) | 2 (1.5, 2.5) | 4 (3.7, 4.3) |
| Male | 82 (57.7) | 41 (57.7) | 10 (47.6) | 13 (46.4) | 18 (81.8) | 41 (57.7) | 13 (46.4) | 19 (63.3) | 9 (69.2) |
| Sex, n (%) | |||||||||
| Female | 60 (42.3) | 30 (42.3) | 11 (52.4) | 15 (53.6) | 4 (18.2) | 30 (42.3) | 15 (53.6) | 11 (36.7) | 4 (30.8) |
| Smoking, n (%) | |||||||||
| Never | 84 (59.2) | 41 (57.7) | 16 (76.2) | 14 (50.0) | 11 (50.0) | 43 (60.6) | 19 (67.9) | 19 (63.3) | 5 (38.5) |
| Previous | 53 (37.3) | 29 (40.8) | 5 (23.8) | 13 (46.4) | 11 (50.0) | 24 (33.8) | 7 (25.0) | 10 (33.3) | 7 (53.8) |
| Current | 5 (3.5) | 1 (1.4) | 0 (0) | 1 (3.6) | 0 (0) | 4 (5.6) | 2 (7.1) | 1 (3.3) | 1 (7.7) |
| Diabetes, n (%) | |||||||||
| No | 115 (81.0) | 57 (80.3) | 18 (85.7) | 24 (85.7) | 15 (68.2) | 58 (81.7) | 22 (78.6) | 27 (90.0) | 9 (69.2) |
| Yes | 27 (19.0) | 14 (19.7) | 3 (14.3) | 4 (14.3) | 7 (31.8) | 13 (18.3) | 6 (21.4) | 3 (10.0) | 4 (30.8) |
| Preoperative samilson-prieto score, n (%) | |||||||||
| None | 71 (50.0) | 1 (1.4) | 0 (0) | 1 (3.6) | 0 (0) | 70 (98.6) | 28 (100.0) | 29 (96.7) | 13 (100.0) |
| Mild (< 3 mm) | 62 (43.7) | 61 (85.9) | 18 (85.7) | 27 (96.4) | 16 (72.7) | 1 (1.4) | 0 (0) | 1 (3.3) | 0 (0) |
| Moderate (3 mm-7 mm) | 9 (6.3) | 9 (12.7) | 3 (14.3) | 0 (0) | 6 (27.3) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Goutallier classification, n (%) | |||||||||
| Grade 0 (normal muscle) | 95 (66.9) | 47 (66.2) | 18 (85.7) | 19 (67.9) | 10 (45.5) | 48 (67.6) | 23 (82.1) | 20 (66.7) | 5 (38.5) |
| Grade 1 (some fattystreaks) | 36 (25.4) | 18 (25.4) | 2 (9.5) | 7 (25.0) | 9 (40.9) | 18 (25.4) | 5 (17.9) | 8 (26.7) | 5 (38.5) |
| Grade 2 (< 50% fattymuscle atrophy) | 11 (7.7) | 6 (8.5) | 1 (4.8) | 2 (7.1) | 3 (13.6) | 5 (7.0) | 0 (0) | 2 (6.7) | 3 (23.1) |
| Muscle atrophy (warner grading system), n (%) | 0 (0) | ||||||||
| None | 107 (75.4) | 50 (70.4) | 18 (85.7) | 21 (75.0) | 11 (50.0) | 57 (80.3) | 24 (85.7) | 24 (80.0) | 9 (69.2) |
| Mild | 29 (20.4) | 17 (23.9) | 2 (9.5) | 5 (17.9) | 10 (45.5) | 12 (16.9) | 4 (14.3) | 5 (16.7) | 3 (23.1) |
| Moderate | 6 (4.2) | 4 (5.6) | 1 (4.8) | 2 (7.1) | 1 (4.5) | 2 (2.8) | 0 (0) | 1 (3.3) | 1 (7.7) |
| Primary GHOA, n (%) | |||||||||
| No | 71 (50.0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 71 (100.0) | 28 (100.0) | 30 (100.0) | 13 (100.0) |
| Yes | 71 (50.0) | 71 (100.0) | 21 (100.0) | 28 (100.0) | 22 (100.0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
Using the Samilson-Prieto classification to grade GHOA severity, 85.9% (61/71) had a grade of 1 (mild or < 3 mm), and 12.7% (9/71) had a grade of 2 (moderate or 3 mm - 7 mm). Goutallier classification of the rotator cuff revealed that patients with GHOA: 66.2% (47/71) had a grade of 0 (normal muscle), 25.4% (18/71) had a grade of 1 (some fatty streaks), and 8.5% (6/71) had a grade of 2 (less than 50% fatty muscle atrophy). In comparison, the Goutallier classification of the rotator cuff for patients without GHOA revealed: 67.6% (48/71) with grade of 0, 25.4% (18/71) with a grade of 1, and 7.0% (5/71) with a grade of 2. Finally, in patients with GHOA the Warner grading system for muscle atrophy revealed: 70.4% (50/71) with no atrophy, 23.9% (17/71) with mild atrophy, and 5.6% (4/71) with moderate atrophy. For patients without GHOA, the Warner grading system for muscle atrophy revealed: 80.3% (57/71) with no atrophy, 16.9% (12/71) with mild atrophy, and 2.8% (2/71) with moderate atrophy.
Detailed data regarding RCR surgical technique, type of anchors used, fixation method and concurrent procedures for patients with or without GHOA stratified by rotator cuff tear size can be found in Table 2.
| With GHOA | Without GHOA | ||||||||
| Tear size group | Tear size group | ||||||||
| Overall (n = 142) | Overall Case (n = 71) | Small (0-1 cm) (n = 21) | Medium (1-3 cm) (n = 28) | Large (3-5 cm) (n = 22) | Overall Control (n = 71) | Small (0-1 cm) (n = 28) | Medium (1-3 cm) (n = 30) | Large (3-5 cm) (n = 13) | |
| Single row, n (%) | |||||||||
| No | 124 (87.3) | 60 (84.5) | 16 (76.2) | 24 (85.7) | 20 (90.9) | 64 (90.1) | 26 (92.9) | 26 (86.7) | 12 (92.3) |
| Yes | 18 (12.7) | 11 (15.5) | 5 (23.8) | 4 (14.3) | 2 (9.1) | 7 (9.9) | 2 (7.1) | 4 (13.3) | 1 (7.7) |
| Double row, n (%) | |||||||||
| Yes | 122 (85.9) | 60 (84.5) | 17 (81.0) | 23 (82.1) | 20 (90.9) | 62 (87.3) | 24 (85.7) | 26 (86.7) | 12 (92.3) |
| No | 20 (14.1) | 11 (15.5) | 4 (19.0) | 5 (17.9) | 2 (9.1) | 9 (12.7) | 4 (14.3) | 4 (13.3) | 1 (7.7) |
| Medial row, n (%) | |||||||||
| Yes | 138 (97.2) | 69 (97.2) | 19 (90.5) | 28 (100.0) | 22 (100.0) | 69 (97.2) | 28 (100.0) | 28 (93.3) | 13 (100.0) |
| No | 4 (2.8) | 2 (2.8) | 2 (9.5) | 0 (0) | 0 (0) | 2 (2.8) | 0 (0) | 2 (6.7) | 0 (0) |
| Lateral row, n (%) | |||||||||
| Yes | 120 (84.5) | 61 (85.9) | 18 (85.7) | 23 (82.1) | 20 (90.9) | 59 (83.1) | 24 (85.7) | 24 (80.0) | 11 (84.6) |
| No | 22 (15.5) | 10 (14.1) | 3 (14.3) | 5 (17.9) | 2 (9.1) | 12 (16.9) | 4 (14.3) | 6 (20.0) | 2 (15.4) |
| Arthrotunneler, n (%) | |||||||||
| No | 139 (97.9) | 71 (100.0) | 21 (100.0) | 28 (100.0) | 22 (100.0) | 71 (100.0) | 28 (100.0) | 28 (93.3) | 12 (92.3) |
| Yes | 3 (2.1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 2 (6.7) | 1 (7.7) | ||
| Medial row fixation type, n (%) | |||||||||
| Missing for 6 patients | |||||||||
| Suture tied | 135 (95.1) | 67 (94.4) | 19 (90.5) | 26 (92.9) | 22 (100.0) | 68 (95.8) | 28 (100.0) | 28 (93.3) | 12 (92.3) |
| Knotless | 1 (0.7) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1.4) | 0 (0) | 0 (0) | 1 (7.7) |
| Medial row anchor type, n (%) | |||||||||
| Missing for 11 patients | |||||||||
| PEEK | 86 (60.6) | 53 (74.6) | 16 (76.2) | 21 (75.0) | 16 (72.7) | 33 (46.5) | 16 (57.1) | 12 (40.0) | 5 (38.5) |
| Knotted | 35 (24.6) | 10 (14.1) | 2 (9.5) | 5 (17.9) | 3 (13.6) | 25 (35.2) | 10 (35.7) | 11 (36.7) | 4 (30.8) |
| Knotless | 7 (4.9) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 7 (9.9) | 1 (3.6) | 5 (16.7) | 1 (7.7) |
| Plastic | 3 (2.1) | 3 (4.2) | 1 (4.8) | 0 (0) | 2 (9.1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Lateral row fixation type, n (%) | |||||||||
| Missing for 23 patients | |||||||||
| Knotless | 90 (63.4) | 46 (64.8) | 13 (61.9) | 16 (57.1) | 17 (77.3) | 44 (62.0) | 20 (71.4) | 18 (60.0) | 6 (46.2) |
| Suture tied | 29 (20.4) | 15 (21.1) | 5 (23.8) | 7 (25.0) | 3 (13.6) | 14 (19.7) | 4 (14.3) | 6 (20.0) | 4 (30.8) |
| Lateral row anchor type, n (%) | |||||||||
| Missing for 29 patients | |||||||||
| PEEK | 70 (49.3) | 28 (39.4) | 12 (57.1) | 8 (28.6) | 8 (36.4) | 42 (59.2) | 21 (75.0) | 15 (50.0) | 6 (46.2) |
| Plastic | 20 (14.1) | 20 (28.2) | 3 (14.3) | 8 (28.6) | 9 (40.9) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Knotted | 17 (12.0) | 6 (8.5) | 1 (4.8) | 4 (14.3) | 1 (4.5) | 11 (15.5) | 3 (10.7) | 4 (13.3) | 4 (30.8) |
| Knotless | 6 (4.2) | 3 (4.2) | 1 (4.8) | 1 (3.6) | 1 (4.5) | 3 (4.2) | 0 (0) | 3 (10.0) | 0 (0) |
| Concurrent procedures | |||||||||
| Distal clavicle excision, n (%) | |||||||||
| Yes | 79 (55.6) | 41 (57.7) | 15 (71.4) | 16 (57.1) | 10 (45.5) | 38 (53.5) | 16 (57.1) | 17 (56.7) | 5 (38.5) |
| No | 63 (44.4) | 30 (42.3) | 6 (28.6) | 12 (42.9) | 12 (54.5) | 33 (46.5) | 12 (42.9) | 13 (43.3) | 8 (61.5) |
| Subacromial decompression, n (%) | |||||||||
| Yes | 142 (100.0) | 71 (100.0) | 21 (100.0) | 28 (100.0) | 22 (100.0) | 71 (100.0) | 28 (100.0) | 30 (100.0) | 13 (100.0) |
| Capsular release, n (%) | |||||||||
| No | 133 (93.7) | 66 (93.0) | 20 (95.2) | 25 (89.3) | 21 (95.5) | 67 (94.4) | 26 (92.9) | 30 (100.0) | 11 (84.6) |
| Yes | 9 (6.3) | 5 (7.0) | 1 (4.8) | 3 (10.7) | 1 (4.5) | 4 (5.6) | 2 (7.1) | 0 (0) | 2 (15.4) |
| Labral debridement, n (%) | |||||||||
| No | 125 (88.0) | 63 (88.7) | 20 (95.2) | 24 (85.7) | 19 (86.4) | 62 (87.3) | 24 (85.7) | 26 (86.7) | 12 (92.3) |
| Yes | 17 (12.0) | 8 (11.3) | 1 (4.8) | 4 (14.3) | 3 (13.6) | 9 (12.7) | 4 (14.3) | 4 (13.3) | 1 (7.7) |
| Chondroplasty, n (%) | |||||||||
| No | 120 (84.5) | 54 (76.1) | 14 (66.7) | 20 (71.4) | 20 (90.9) | 66 (93.0) | 25 (89.3) | 28 (93.3) | 13 (100.0) |
| Yes | 22 (15.5) | 17 (23.9) | 7 (33.3) | 8 (28.6) | 2 (9.1) | 5 (7.0) | 3 (10.7) | 2 (6.7) | 0 (0) |
| Biceps tenotomy, n (%) | |||||||||
| No | 92 (64.8) | 44 (62.0) | 11 (52.4) | 20 (71.4) | 13 (59.1) | 48 (67.6) | 18 (64.3) | 23 (76.7) | 7 (53.8) |
| Yes | 50 (35.2) | 27 (38.0) | 10 (47.6) | 8 (28.6) | 9 (40.9) | 23 (32.4) | 10 (35.7) | 7 (23.3) | 6 (46.2) |
| Biceps tenodesis, n (%) | |||||||||
| No | 99 (69.7) | 54 (76.1) | 20 (95.2) | 19 (67.9) | 15 (68.2) | 45 (63.4) | 18 (64.3) | 17 (56.7) | 10 (76.9) |
| Yes | 43 (30.3) | 17 (23.9) | 1 (4.8) | 9 (32.1) | 7 (31.8) | 26 (36.6) | 10 (35.7) | 13 (43.3) | 3 (23.1) |
| If biceps tenodesis, n (%) | |||||||||
| Suprapectoral | 37 (26.1) | 11 (15.5) | 0 (0) | 5 (17.9) | 6 (27.3) | 26 (36.6) | 10 (35.7) | 13 (43.3) | 3 (23.1) |
| Subpectoral | 6 (4.2) | 6 (8.5) | 1 (4.8) | 4 (14.3) | 1 (4.5) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
The re-operation rate was 15.5% (11/71) and 8.5% (6/71) in patients with GHOA and without GHOA respectively. The mean follow-up period for both groups was 12.45 mo, with a range from 0-104 mo for the GHOA group, and 0-94 mo for the patients without GHOA. Within two years after rotator cuff repair, 2.8% (2/71) patients with GHOA underwent TSA or RTSA in the ipsilateral shoulder compared to 1.4% (1/71) patients without GHOA. Both patients developed rotator cuff arthropathy and pain with range of motion, and eventually underwent RTSA. The non GHOA patient eventually underwent an RTSA for rotator cuff arthropathy. Beyond the two year follow-up 4 patients with GHOA and 2 patients without GHOA underwent the conversion to TSA or RTSA. Complication rates after initial rotator cuff repair was 23.9% (17/71) and 18.3% (13/71) for patients with GHOA and without GHOA respectively and 12.7% (9/71) of patients with GHOA experienced rotator cuff re-tear after RCR compared to 11.3% (8/71) of patients without GHOA as determined by post op MRI or intra-operative findings (Table 3).
| With GHOA | Without GHOA | ||||||||
| Tear size group | Tear size group | ||||||||
| Overall (n = 142) | Case Overall (n = 71) | Small (0-1cm) (n = 21) | Medium (1-3cm) (n = 28) | Large (3-5cm) (n = 22) | Control Overall (n = 71) | Small (0-1cm) (n = 28) | Medium (1-3cm) (n = 30) | Large (3-5cm) (n = 13) | |
| Reoperation post RCR, n (%) | |||||||||
| No | 125 (88.0) | 60 (84.5) | 19 (90.5) | 23 (82.1) | 18 (81.8) | 65 (91.5) | 26 (92.9) | 28 (93.3) | 11 (84.6) |
| Yes | 17 (12.0) | 11 (15.5) | 2 (9.5) | 5 (17.9) | 4 (18.2) | 6 (8.5) | 2 (7.1) | 2 (6.7) | 2 (15.4) |
| Complications, n (%) | |||||||||
| Missing for 1 patient | |||||||||
| No | 111 (78.2) | 53 (74.6) | 16 (76.2) | 22 (78.6) | 15 (68.2) | 58 (81.7) | 22 (78.6) | 24 (80.0) | 12 (92.3) |
| Yes | 30 (21.1) | 17 (23.9) | 4 (19.0) | 6 (21.4) | 7 (31.8) | 13 (18.3) | 6 (21.4) | 6 (20.0) | 1 (7.7) |
| Wound issues, n (%) | |||||||||
| Missing for 131 patients | |||||||||
| No | 11 (7.7) | 9 (12.7) | 2 (9.5) | 3 (10.7) | 4 (18.2) | 2 (2.8) | 0 (0) | 2 (6.7) | 0 (0) |
| Infection, n (%) | |||||||||
| Missing for 131 patients | |||||||||
| No | 11 (7.7) | 9 (12.7) | 2 (9.5) | 3 (10.7) | 4 (18.2) | 2 (2.8) | 0 (0) | 2 (6.7) | 0 (0) |
| Stiffness, n (%) | |||||||||
| Missing for 126 patients | |||||||||
| Yes | 8 (5.6) | 5 (7.0) | 3 (14.3) | 1 (3.6) | 1 (4.5) | 3 (4.2) | 1 (3.6) | 2 (6.7) | 0 (0) |
| No | 8 (5.6) | 7 (9.9) | 0 (0) | 3 (10.7) | 4 (18.2) | 1 (1.4) | 0 (0) | 1 (3.3) | 0 (0) |
| Rotator cuff retear, n (%) | |||||||||
| Missing for 122 patients | |||||||||
| Yes | 17 (12.0) | 9 (12.7) | 0 (0) | 4 (14.3) | 5 (22.7) | 8 (11.3) | 3 (10.7) | 4 (13.3) | 1 (7.7) |
| No | 3 (2.1) | 2 (2.8) | 2 (9.5) | 0 (0) | 0 (0) | 1 (1.4) | 0 (0) | 1 (3.3) | 0 (0) |
| Other complication, n (%) | |||||||||
| Missing for 128 patients | |||||||||
| No | 8 (5.6) | 4 (5.6) | 1 (4.8) | 2 (7.1) | 1 (4.5) | 4 (5.6) | 1 (3.6) | 2 (6.7) | 1 (7.7) |
| Yes | 6 (4.2) | 3 (4.2) | 1 (4.8) | 1 (3.6) | 1 (4.5) | 3 (4.2) | 2 (7.1) | 1 (3.3) | 0 (0) |
| Other complication description, n (%) | |||||||||
| Pain | 1 (0.7) | 1 (1.4) | 1 (4.8) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Block related neuropraxia | 1 (0.7) | 1 (1.4) | 0 (0) | 1 (3.6) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Weakness | 1 (0.7) | 1 (1.4) | 0 (0) | 0 (0) | 1 (4.5) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Median nerve neuropathy | 1 (0.7) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1.4) | 1 (3.6) | 0 (0) | 0 (0) |
| Greater tuberosity fx | 1 (0.7) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1.4) | 1 (3.6) | 0 (0) | 0 (0) |
| Heterotopic ossification | 1 (0.7) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1.4) | 0 (0) | 1 (3.3) | 0 (0) |
| 1st reoperation diagnosis, n (%) | |||||||||
| Other | 13 (9.2) | 9 (12.7) | 2 (9.5) | 4 (14.3) | 3 (13.6) | 4 (5.6) | 1 (3.6) | 1 (3.3) | 2 (15.4) |
| Stiffness | 3 (2.1) | 2 (2.8) | 0 (0) | 1 (3.6) | 1 (4.5) | 1 (1.4) | 0 (0) | 1 (3.3) | 0 (0) |
| Hardware pain | 1 (0.7) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1.4) | 1 (3.6) | 0 (0) | 0 (0) |
| 1st reoperation other diagnosis, n (%) | |||||||||
| Rotator cuff arthropathy | 4 (2.8) | 3 (4.2) | 0 (0) | 2 (7.1) | 1 (4.5) | 1 (1.4) | 0 (0) | 0 (0) | 1 (7.7) |
| Rotator cuff retear | 4 (2.8) | 3 (4.2) | 0 (0) | 2 (7.1) | 1 (4.5) | 1 (1.4) | 0 (0) | 1 (3.3) | 0 (0) |
| Inflammatory arthritis | 1 (0.7) | 1 (1.4) | 1 (4.8) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Glenohumeral arthritis | 1 (0.7) | 1 (1.4) | 1 (4.8) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Retear RTC, rotator cuffarthropathy | 1 (0.7) | 1 (1.4) | 0 (0) | 0 (0) | 1 (4.5) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Greater tuberosity fracture | 1 (0.7) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1.4) | 1 (3.6) | 0 (0) | 0 (0) |
| Rotator cuff arthropathy | 1 (0.7) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1.4) | 0 (0) | 0 (0) | 1 (7.7) |
| 1st reoperation procedure, n (%) | |||||||||
| Conversion to RTSA | 8 (5.6) | 5 (7.0) | 1 (4.8) | 2 (7.1) | 2 (9.1) | 3 (4.2) | 1 (3.6) | 0 (0) | 2 (15.4) |
| Other | 6 (4.2) | 3 (4.2) | 0 (0) | 2 (7.1) | 1 (4.5) | 3 (4.2) | 1 (3.6) | 2 (6.7) | 0 (0) |
| Lysis of adhesions | 2 (1.4) | 2 (2.8) | 0 (0) | 1 (3.6) | 1 (4.5) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Conversion to TSA | 1 (0.7) | 1 (1.4) | 1 (4.8) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| 1st reoperation other procedure, n (%) | |||||||||
| Revision rotator cuff repair | 4 (2.8) | 3 (4.2) | 0 (0) | 2 (7.1) | 1 (4.5) | 1 (1.4) | 0 (0) | 1 (3.3) | 0 (0) |
| Removal of heterotopicossification | 1 (0.7) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1.4) | 0 (0) | 1 (3.3) | 0 (0) |
| Removal of hardware, RTC debridement | 1 (0.7) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1.4) | 1 (3.6) | 0 (0) | 0 (0) |
| 2nd reoperation post RCR, n (%) | |||||||||
| Missing for 1 patient | |||||||||
| No | 14 (9.9) | 10 (14.1) | 1 (4.8) | 5 (17.9) | 4 (18.2) | 4 (5.6) | 1 (3.6) | 2 (6.7) | 1 (7.7) |
| Yes | 2 (1.4) | 1 (1.4) | 1 (4.8) | 0 (0) | 0 (0) | 1 (1.4) | 0 (0) | 0 (0) | 1 (7.7) |
| 2nd reoperation diagnosis, n (%) | |||||||||
| Other | 2 (1.4) | 1 (1.4) | 1 (4.8) | 0 (0) | 0 (0) | 1 (1.4) | 0 (0) | 0 (0) | 1 (7.7) |
| 2nd reoperation other diagnosis, n (%) | |||||||||
| Insufficiency due to subscapularis failure | 1 (0.7) | 1 (1.4) | 1 (4.8) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Instability | 1 (0.7) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1.4) | 0 (0) | 0 (0) | 1 (7.7) |
| 2nd reoperation procedure, n (%) | |||||||||
| Other | 2 (1.4) | 1 (1.4) | 1 (4.8) | 0 (0) | 0 (0) | 1 (1.4) | 0 (0) | 0 (0) | 1 (7.7) |
| Conversion to TSA/RTSA within 2 yr post index DOS, n (%) | |||||||||
| No | 139 (97.9) | 69 (97.2) | 20 (95.2) | 28 (100.0) | 21 (95.5) | 70 (98.6) | 28 (100.0) | 30 (100.0) | 12 (92.3) |
| Yes | 3 (2.1) | 2 (2.8) | 1 (4.8) | 0 (0) | 1 (4.5) | 1 (1.4) | 0 (0) | 0 (0) | 1 (7.7) |
The Median VR-12 mental health component summary scores were 58.3 (IQR 44.8, 61.3) and 56.5 (IQR 47.5, 61.7) and the median VR-12 physical health component summary scores were 49.6 (IQR 40.2, 52.4) and 47.6 (IQR 36.6, 53.7) in patients with and without GHOA respectively. The overall median ASES score for the right shoulder was 98.3 (IQR 93.3, 100) in patients with or without GHOA; overall median ASES score for the left shoulders were 100 (IQR 91.7, 100) and 96.7 (86.7, 100) respectively. Finally, the overall median SANE score was 95 (IQR 90, 100) and 95 (IQR 85, 100) in patients with or without GHOA respectively. PROs did not show any significant difference according to rotator cuff tear size when patients with GHOA were compared with patients without GHOA (Table 4).
| Overall (n= 142) | With GHOA, Small tear (0-1 cm) (n= 21) | Without GHOA, Small tear (0-1 cm) (n= 28) | P value | With GHOA, Medium tear (1-3 cm) (n= 28) | Without GHOA, Medium tear (1-3 cm) (n= 30) | P value | With GHOA, Large tear (3-5 cm) (n= 22) | Without GHOA, Large tear (3-5 cm) (n= 13) | P value | |
| MCS, median (IQR) | 57.1 (46.5, 61.6) | 60.9 (37.6, 64.1) | 56.3 (44.4, 61.5) | > 0.99 | 59.3 (44.6, 61.3) | 58.3 (50, 62.8) | > 0.99 | 54.4 (48, 57.9) | 51 (47.3, 60.2) | > 0.99 |
| PCS, median (IQR) | 49.1 (40, 52.6) | 40.2 (29.6, 49.1) | 51.4 (42.4, 55) | 0.148 | 50 (44.9, 51.8) | 46.4 (35.1, 50.8) | > 0.99 | 52.7 (49.7, 55.4) | 41.8 (34.4, 53.3) | > 0.99 |
| VAS pain, median (IQR) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | > 0.99 | 0.0 (0.0, 1.0) | 0.0 (0.0, 1.0) | > 0.99 | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | > 0.99 |
| VAS instability, median (IQR) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | > 0.99 | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | - | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | - |
| ASES shoulder right, median (IQR) | 98.3 (93.3, 100) | 100 (95, 100) | 99.2 (95, 100) | > 0.99 | 98.3 (91.7, 100) | 95 (91.7, 100) | > 0.99 | 98.3 (93.3, 98.3) | 100 (95, 100) | > 0.99 |
| ASES shoulder left, median (IQR) | 98.3 (90, 100) | 100 (85, 100) | 98.3 (91.7, 100) | > 0.99 | 100 (93.3, 100) | 95.8 (87.5, 100) | > 0.99 | 100 (91.7, 100) | 90 (66.7, 100) | > 0.99 |
| SANE, median (IQR) | 95 (85, 100) | 96.5 (90, 100) | 100 (92.5, 100) | > 0.99 | 100 (95, 100) | 95 (80, 100) | > 0.99 | 90 (85, 95) | 85 (50, 100) | > 0.99 |
The results demonstrate the conversion to shoulder arthroplasty, patient-reported clinical outcome scores, and rates of re-operation were no different when comparing RCR done in the setting of GHOA vs without GHOA in short-term follow-up. Our results indicate that the presence of GHOA at the time of RCR did not seem to influence the progression of GHOA. There is general agreement within literature that severe primary GHOA is an appropriate indication for TSA or RTSA[14,15]. Additionally, rotator cuff tear arthropathy, rotator cuff insufficiency, and superior migration of humeral head - is considered another indication for RTSA[14-16]. While GHOA and rotator cuff tears both contribute to morbidity due to decreased shoulder function, there are limited studies evaluating the outcomes of joint-preserving treatment via RCR in the setting of GHOA.
A recent study by Jeong et al[8] retrospectively evaluated the clinical outcomes of large to massive RCR in patients with and without mild GHOA. The authors found that preoperative and postoperative variables (VAS scores, ROM, muscle strength, University of California, Los Angeles (UCLA) scores, and Constant scores) at final follow-up (2 years) showed no significant differences between the two groups. Our study also included VAS and similarly did not show any significant difference between groups at final follow up period of 2 years. Jeong et al[8] reported mean VAS scores in patients with large to massive tears with mild GHOA and without mild GHOA to be 0.3 ± 0.7 and 0.3 ± 0.8, respectively which are similar to our overall median VAS score of 0.0 (IQR 0.0, 0.0). These combined results indicate that patients with small to large rotator cuff repairs in the setting of mild to moderate GHOA can expect to have a pain score close to 0 after a minimum of 2 years after RCR.
A study by Kukkonen et al[10] evaluated outcomes using Constant scores in patients with or without GHOA after undergoing supraspinatus tendon repair with tear sizes ranging from 0.5 cm to 2.5 cm. Both pre and post-operative Constant scores were significantly lower in patients with GHOA. These results differ from ours and Jeong et al’s which showed no difference in PROs in patients with or without GHOA[8]. Kukkonen et al’s study only included males, had final follow-up of 1 year, and used the Kellgren-Lawrence classification to determine GHOA severity and status[10]. In contrast, our study and the study by Jeong et al[8] included males and females with a follow-up of 2 years and used the Samilson-Priesto classification for GHOA grading. A study of radiographic classifications of GHOA found that the Kellgren-Lawrence provided inferior inter-observer agreement in diagnosis of GHOA compared to Samilson-Priesto due to the challenge of identifying minor joint space narrowing in the non-weight bearing shoulder joint[17]. The aforementioned finding may limit comparative value of studies using different radiographic classification methods.
Overall, the results of our PROs after a short to medium term follow-up period show favorable results in VR-12, VAS, ASES, and SANE regardless of tear size or presence of GHOA. In patients with mild to moderate GHOA, there were no significant differences in all categories of PROs when comparing to patients without GHOA stratified by small to large rotator cuff tears. The minimal clinical important difference (MCID) was established to define minimum difference in PROs that is required to provide a clinically relevant benefit for patients rather than relying on statistically significant differences. The MCID for VR-12 PCS, MCS, VAS pain, ASES, and SANE following RCR has been reported to be 4.94, 5.99, 1.4, 21.0, and 11.80 respectively[18,19]. VR-12 PCS was the only PROs that showed MCID when patients with small or large rotator cuff tears were compared by presence or absence of GHOA. Surprisingly, patients with mild to moderate GHOA and small RCR had worse VR-12 PCS scores. A literature review of histopathology of rotator cuff tears showed that inflammatory cell infiltrate and number of blood vessels are inversely correlated with tear size[20]. Immunochemistry has also shown torn rotator cuff tendons with lower vascularity have fewer new nerve fibers and is linked to lower chronic pain[21].
The rate of conversion to TSA or RTSA within 2 years after RCR were low for patients with and without GHOA at 2.8% (2/71) and 1.4% (1/71), respectively. This is the first study to report conversion to TSA or RTSA as an outcome variable while comparing outcomes following RCR in patients with or without GHOA. Results of previous studies, which showed that the progression of GHOA did not negatively affect PROs at final follow-up in patients who underwent RCR or arthroscopic debridement of massive irreparable rotator cuff tears[8,22,23], led us to hypothesize patients with GHOA would have conversion rate to TSA or RTSA are comparable with patients without GHOA. The results of our study report good PROs and very low conversion rates to shoulder arthroplasty after RCR with concomitant GHOA.
Due to the retrospective design, there are aspects to patient selection and classification that may introduce confounding biases. The heterogeneous nature of the patients with regard to demographics, surgical technique, and being treated by multiple surgeons at a single academic institution may limit the ability to make accurate comparisons between groups. Furthermore, no preoperative PROs were obtained which may have served as a baseline measure to observe any improvements or exacerbations following RCR. Our follow-up period may be reflective of short- term outcomes with a lack of findings for longer-term outcomes (greater than 5 years or 10 years). However, a recent study by Manderle et al[24] showed that the vast majority of RCR patients achieve MCID, substantial clinical benefit and patient acceptable symptomatic state for various PROs within 1 year. Therefore, our minimum 2-year follow-up period may be sufficient to evaluate and make comparisons of the postoperative PROs following RCR in this patient population.
This study reveals comparable outcomes in patients following small, medium, and large RCR with or without GHOA. Within a clinical follow-up period of 2 years, there were low rates of conversion to TSA or RTSA and no significant statistical differences found in PROs between patients with and without GHOA. In patients with mild to moderate GHOA and small to large rotator cuff tears, RCR is an effective means of surgical intervention that allows for joint-preservation and satisfactory PROs at short and medium-term follow-up.
This study showed that patient reported outcomes in patients that have undergone a rotator cuff repair procedure, in the setting of Glenohumeral Osteoarthritis (GHOA) are favorable at short term (IE less than 2 year) follow-up. The rate of conversion to arthroplasty for these patients was also very low, indicating satisfaction with their outcomes.
There is a paucity of literature surrounding this topic, rotator cuff repair (RCR) in the setting of GHOA, so we felt it necessary to add to the literature with our own set of data in hopes of providing clinicians with more data surrounding this topic.
To determine patient report outcomes and rate of conversion to arthroplasty for patients with GHOA after undergoing a rotator cuff repair procedure. With favorable outcomes, and low conversion rates to arthroplasty, these objectives were realized in our data set.
This was a retrospective cohort study with patient follow-up via questionnaire by phone, email, or in person via clinic visits.
Our results showed a low rate of conversion to arthroplasty in both subgroups after undergoing RCR. Patient reported outcomes using standardized scales were also quite favorable in both subgroups.
Our study showed favorable outcomes with regards to patient reported outcomes. A low conversion rate to arthroplasty was also noted in the short term follow-up.
The future direction of our research will include longer term patient follow-up (IE greater than 5-10 years) to ascertain data on conversion to arthroplasty in the GHOA patient.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Pandey V, India; Roach CJ, United States S-Editor: Wang LL L-Editor: A P-Editor: Wang LL
| 1. | Yamaguchi K, Ditsios K, Middleton WD, Hildebolt CF, Galatz LM, Teefey SA. The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am. 2006;88:1699-1704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 446] [Cited by in RCA: 550] [Article Influence: 27.5] [Reference Citation Analysis (0)] |
| 2. | Keener JD, Steger-May K, Stobbs G, Yamaguchi K. Asymptomatic rotator cuff tears: patient demographics and baseline shoulder function. J Shoulder Elbow Surg. 2010;19:1191-1198. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 74] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 3. | Minagawa H, Yamamoto N, Abe H, Fukuda M, Seki N, Kikuchi K, Kijima H, Itoi E. Prevalence of symptomatic and asymptomatic rotator cuff tears in the general population: From mass-screening in one village. J Orthop. 2013;10:8-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 404] [Article Influence: 31.1] [Reference Citation Analysis (0)] |
| 4. | Ansok CB, Muh SJ. Optimal management of glenohumeral osteoarthritis. Orthop Res Rev. 2018;10:9-18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 5. | Oh JH, Chung SW, Oh CH, Kim SH, Park SJ, Kim KW, Park JH, Lee SB, Lee JJ. The prevalence of shoulder osteoarthritis in the elderly Korean population: association with risk factors and function. J Shoulder Elbow Surg. 2011;20:756-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 71] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 6. | Ibounig T, Simons T, Launonen A, Paavola M. Glenohumeral osteoarthritis: an overview of etiology and diagnostics. Scand J Surg. 2021;110:441-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 70] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 7. | Zhang Y, Jordan JM. Epidemiology of osteoarthritis. Clin Geriatr Med. 2010;26:355-369. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1498] [Cited by in RCA: 1357] [Article Influence: 84.8] [Reference Citation Analysis (0)] |
| 8. | Jeong HY, Jeon YS, Lee DK, Rhee YG. Rotator cuff tear with early osteoarthritis: how does it affect clinical outcome after large to massive rotator cuff repair? J Shoulder Elbow Surg. 2019;28:237-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Kerr R, Resnick D, Pineda C, Haghighi P. Osteoarthritis of the glenohumeral joint: a radiologic-pathologic study. AJR Am J Roentgenol. 1985;144:967-972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 71] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Kukkonen J, Joukainen A, Lehtinen J, Aärimaa V. The effect of glenohumeral osteoarthritis on the outcome of isolated operatively treated supraspinatus tears. J Orthop Sci. 2013;18:405-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Yamamoto A, Takagishi K, Osawa T, Yanagawa T, Nakajima D, Shitara H, Kobayashi T. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010;19:116-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 748] [Cited by in RCA: 952] [Article Influence: 59.5] [Reference Citation Analysis (0)] |
| 12. | Gartsman GM, Taverna E. The incidence of glenohumeral joint abnormalities associated with full-thickness, reparable rotator cuff tears. Arthroscopy. 1997;13:450-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 95] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Hsu HC, Luo ZP, Stone JJ, Huang TH, An KN. Correlation between rotator cuff tear and glenohumeral degeneration. Acta Orthop Scand. 2003;74:89-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 14. | Lin DJ, Wong TT, Kazam JK. Shoulder Arthroplasty, from Indications to Complications: What the Radiologist Needs to Know. Radiographics. 2016;36:192-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 42] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 15. | Mattei L, Mortera S, Arrigoni C, Castoldi F. Anatomic shoulder arthroplasty: an update on indications, technique, results and complication rates. Joints. 2015;3:72-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 16. | Nam D, Maak TG, Raphael BS, Kepler CK, Cross MB, Warren RF. Rotator cuff tear arthropathy: evaluation, diagnosis, and treatment: AAOS exhibit selection. J Bone Joint Surg Am. 2012;94:e34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 45] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 17. | Brox JI, Lereim P, Merckoll E, Finnanger AM. Radiographic classification of glenohumeral arthrosis. Acta Orthop Scand. 2003;74:186-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 48] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | Kim DM, Kim TH, Kholinne E, Park JH, Shin MJ, Kim H, Park D, Jeon IH, Koh KH. Minimal Clinically Important Difference, Substantial Clinical Benefit, and Patient Acceptable Symptomatic State After Arthroscopic Rotator Cuff Repair. Am J Sports Med. 2020;48:2650-2659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 132] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 19. | Zhou L, Natarajan M, Miller BS, Gagnier JJ. Establishing Minimal Important Differences for the VR-12 and SANE Scores in Patients Following Treatment of Rotator Cuff Tears. Orthop J Sports Med. 2018;6:2325967118782159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 48] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 20. | Longo UG, Berton A, Khan WS, Maffulli N, Denaro V. Histopathology of rotator cuff tears. Sports Med Arthrosc Rev. 2011;19:227-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 81] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 21. | Xu Y, Bonar F, Murrell GA. Neoinnervation in rotator cuff tendinopathy. Sports Med Arthrosc Rev. 2011;19:354-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 33] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 22. | Liem D, Lengers N, Dedy N, Poetzl W, Steinbeck J, Marquardt B. Arthroscopic debridement of massive irreparable rotator cuff tears. Arthroscopy. 2008;24:743-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 99] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 23. | Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377-381. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38562] [Cited by in RCA: 39839] [Article Influence: 2343.5] [Reference Citation Analysis (0)] |
| 24. | Manderle BJ, Gowd AK, Liu JN, Beletsky A, Nwachukwu BU, Nicholson GP, Bush-Joseph C, Romeo AA, Forsythe B, Cole BJ, Verma NN. Time Required to Achieve Clinically Significant Outcomes After Arthroscopic Rotator Cuff Repair. Am J Sports Med. 2020;48:3447-3453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |