Published online Dec 18, 2022. doi: 10.5312/wjo.v13.i12.1038
Peer-review started: July 25, 2022
First decision: October 17, 2022
Revised: October 22, 2022
Accepted: November 30, 2022
Article in press: November 30, 2022
Published online: December 18, 2022
Processing time: 143 Days and 21.1 Hours
The reparability of large or massive rotator cuff tears is difficult to determine pre-operatively. We previously identified age ≥ 65 years, acromiohumeral interval ≤ 6 mm, and anteroposterior tear size ≥ 22 mm as risk factors for rotator cuff repair failure. We therefore developed a rotator cuff reparability score where each of the above risk factors is assigned a score of one point.
To determine the accuracy of a rotator cuff reparability score.
This was a retrospective cohort study of recruited patients with large or massive rotator cuff tears treated at our institution between January 2013 and December 2019. Exclusion criteria were revision surgery and patients with contraindications for surgery. All patients underwent arthroscopic rotator cuff repair and were categorized into either complete or partial rotator cuff repair. Rotator cuff reparability scores were calculated for each patient. The sensitivity, specificity, positive and negative predictive value, and positive and negative likelihood ratio were assessed. A receiver operating characteristic curve was plotted to determine the optimal cut-off rotator cuff reparability score.
Eighty patients (mean age, 61 years; range, 25–84 years; 41 females and 39 males) were recruited. Intra- and inter-observer reliabilities were good to excellent. The number of patients with 0, 1, 2, and 3 risk factors for rotator cuff repair failure were 24, 33, 17, and 6, respectively. Complete repair was performed in all patients without risk factors. Two of the 33 patients with one risk factor and seven of the 17 patients with two risk factors underwent partial repair. One of the six patients with three risk factors underwent complete repair. The area under the curve was 0.894. The optimal cut-off score was two points with a sensitivity of 85.71% and a specificity of 83.33%.
A rotator cuff reparability score of two was determined to be the optimal cut-off score for predicting the reparability of large or massive rotator cuff tears.
Core Tip: This is retrospective study to evaluate the accuracy of a novel rotator cuff reparability score. In large or massive rotator cuff tears, arthroscopic rotator cuff repair is not always feasible. The reparability of large or massive rotator cuff tears can be more accurately determined after intra-operative arthroscopy. The identification of pre-operative risk factors for rotator cuff tear repair failure may facilitate improvements in management and provide patients with more accurate treatment information. Accordingly, we developed a novel scoring system to predict the likelihood of rotator cuff repair failure.
- Citation: Prasathaporn N, Kuptniratsaikul V, Thamrongskulsiri N, Itthipanichpong T. Accuracy of the rotator cuff reparability score. World J Orthop 2022; 13(12): 1038-1046
- URL: https://www.wjgnet.com/2218-5836/full/v13/i12/1038.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i12.1038
The recommended treatment option for rotator cuff tears is arthroscopic surgery. Complete rotator cuff repair yields superior functional outcomes with a lower rate of recurrent tears compared to partial rotator cuff repair or arthroscopic debridement[1,2]. Partial rotator cuff repair may initially improve functional outcomes; however, half of patients are reportedly dissatisfied with the results of partial rotator cuff repair at long-term follow-up[3]. Prior to arthroscopic rotator cuff surgery, a variety of salvage operations, such as superior capsular reconstruction, tendon transfer, subacromial balloon spacer, and reverse total shoulder arthroplasty, should be planned. Furthermore, arthroscopic repair of large or massive rotator cuff tears may not always be feasible. The reparability of large or massive rotator cuff tears can be more accurately determined during intra-operative arthroscopy. Pre-operative risk factors for rotator cuff repair failure may improve management planning and provide patients with more reliable treatment information.
Age, tendon retraction, rotator cuff tendon tear size, fatty infiltration, muscle atrophy, and superior humeral head migration are reported predictors of the reparability of large rotator cuff tears[4-7]. Our previous study identified age, acromiohumeral interval (AHI), anteroposterior (AP) tear size, and AHI as pre-operative clinical and radiographic parameters associated with the reparability of rotator cuff tears[5]. Pre-operative evaluations have been shown to facilitate better treatment outcomes and lower re-tear rates after complete rotator cuff repair[1,2]. In cases where complete repair is not feasible, alternative salvage techniques with superior results to partial rotator cuff repair should be considered[8].
Accordingly, we developed a novel scoring system for predicting the reparability of large or massive rotator cuff tears. The objective of the present study was to determine the accuracy of our novel pre-operative scoring system in predicting the probability of the reparability of large or massive rotator cuff tears. We hypothesized that higher rotator cuff reparability scores predict rotator cuff repair failure.
The present retrospective cohort study collected data from January 1, 2013 to December 31, 2019 after the Queen Savang Vadhana Memorial Hospital's Research Ethics Committee gave its approval to the study protocol. All patients with large or massive rotator cuff injuries identified by magnetic resonance imaging (MRI) prior to surgery and verified during surgery by arthroscopy were included in the current study. Rotator cuff tears were classified using the Snyder classification and modified Millstein[9,10].
The term "complete supraspinatus tendon tears" was used to describe large rotator cuff tears. At least two tendons must be involved for a rotator cuff injury to be considered massive. The current study excluded patients with recurrent rotator cuff injuries or surgical contraindications.
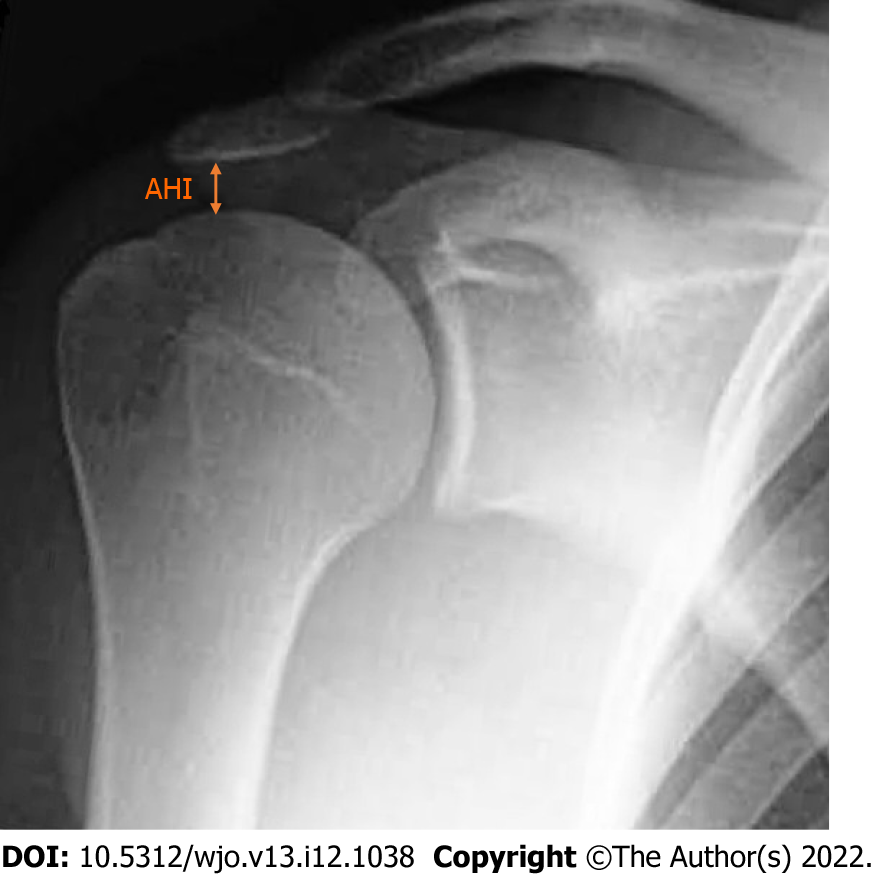
Our rotator cuff reparability scoring system consisted of three factors: age ≥ 65 years, AHI ≤ 6 mm, and AP tear size ≥ 22 mm[2]. AHI was used to assess superior humeral head migration and was measured as the distance between the inferior border of the acromion and the superior aspect of the humeral head on AP plain radiography[11] (Figure 1). AP tear size was determined using T2-weighted MRI in the sagittal oblique view as the largest straight distance from anterior to posterior tendon edge[12]. No measurements were performed for frayed tissues at the tendon edge (Figure 2). Two independent observers measured both imaging parameters twice.
Arthroscopic repair was performed by three fellowship-trained sports medicine surgeons. General anesthesia was used to sedate the patients, who were then placed in a beach chair position. If an acromial spur was identified, acromioplasty was performed. Arthroscopic capsular release and manipulation under anesthesia were performed in cases of adhesive capsulitis. After confirming the size of the tear using an arthroscopic probe, tendon adhesions were released and mobilized to cover as much of the native footprint as feasible. The interval sliding technique was used where necessary. Where feasible, double-row rotator cuff repair or trans-osseous equivalent repair could improve tendon healing, lower the risk of re-rupture, and improve functional outcomes compared to single-row repair[13-15]. Single-row or partial repair was performed in cases where double-row repair was not possible.
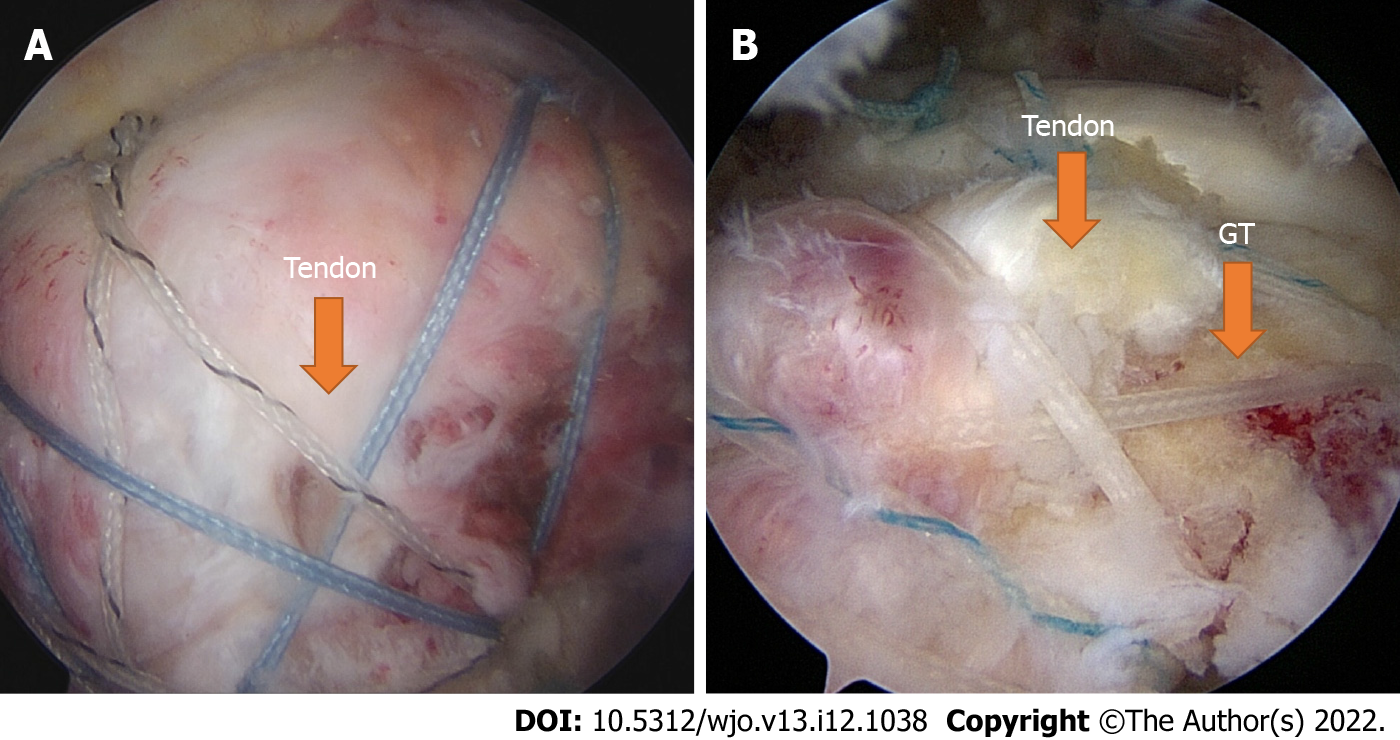
Partial repair was defined as having less than 50% of the anatomical footprint covered by tendon. Complete repair was defined as 50% tendon coverage or greater[7,11] (Figure 3A and B). On the first post-operative day, passive range-of-motion exercises were permitted for all patients. Patients were provided an arm sling for 6 wk post-operatively. In the third or fourth post-operative week, progressive active-assisted passive motion exercises were initiated for muscle strengthening.
Statistical analyses were performed using SPSS version 26. Each risk factor score's sensitivity, specificity, positive and negative predictive value, and positive and negative probability ratio were assessed. The optimal cut-off score and values of area under the curve (AUC) were determined using receiver operating characteristics (ROC) curves. Intra-observer and inter-observer reliabilities were calculated using Kappa analysis and the intra-class correlation coefficient for categorical and continuous data, respectively.
Eighty patients (mean age, 61 years; range, 25–84 years; 41 females and 39 males) met the study inclusion criteria. A total of 64 massive rotator cuff tears (82.5%) and 14 Large rotator cuff tears (17.5%) were identified by MRI and confirmed by arthroscopic examination.
AP distance and AHI had intra-observer reliability values of 83.8 and 84.6 %, respectively. The inter-observer reliability values for AP distance and AHI were 81.2 and 81.6 %, respectively. Both outcomes were rated as good to excellent. Sixty-six patients underwent complete arthroscopic rotator cuff repair. Partial arthroscopic rotator cuff repairs were performed in 14 patients. All 24 patients who had no risk factors for rotator cuff surgery failure had complete arthroscopic repair of their rotator cuffs. Only two of the 33 patients with one risk factor underwent partial repair. Seven patients with two risk factors underwent partial repair, while ten patients with two risk factors underwent complete repair. One of the six patients with all three risk factors underwent complete repair. The numbers of patients undergoing complete or partial repair according to number of risk factors for rotator cuff repair failure are shown in Table 1.
| No. of risk factors | Partial repair | Complete repair | Total |
| 3 | 5 | 1 | 6 |
| 2 | 7 | 10 | 17 |
| 1 | 2 | 31 | 33 |
| 0 | 0 | 24 | 24 |
| Total | 14 | 66 | 80 |
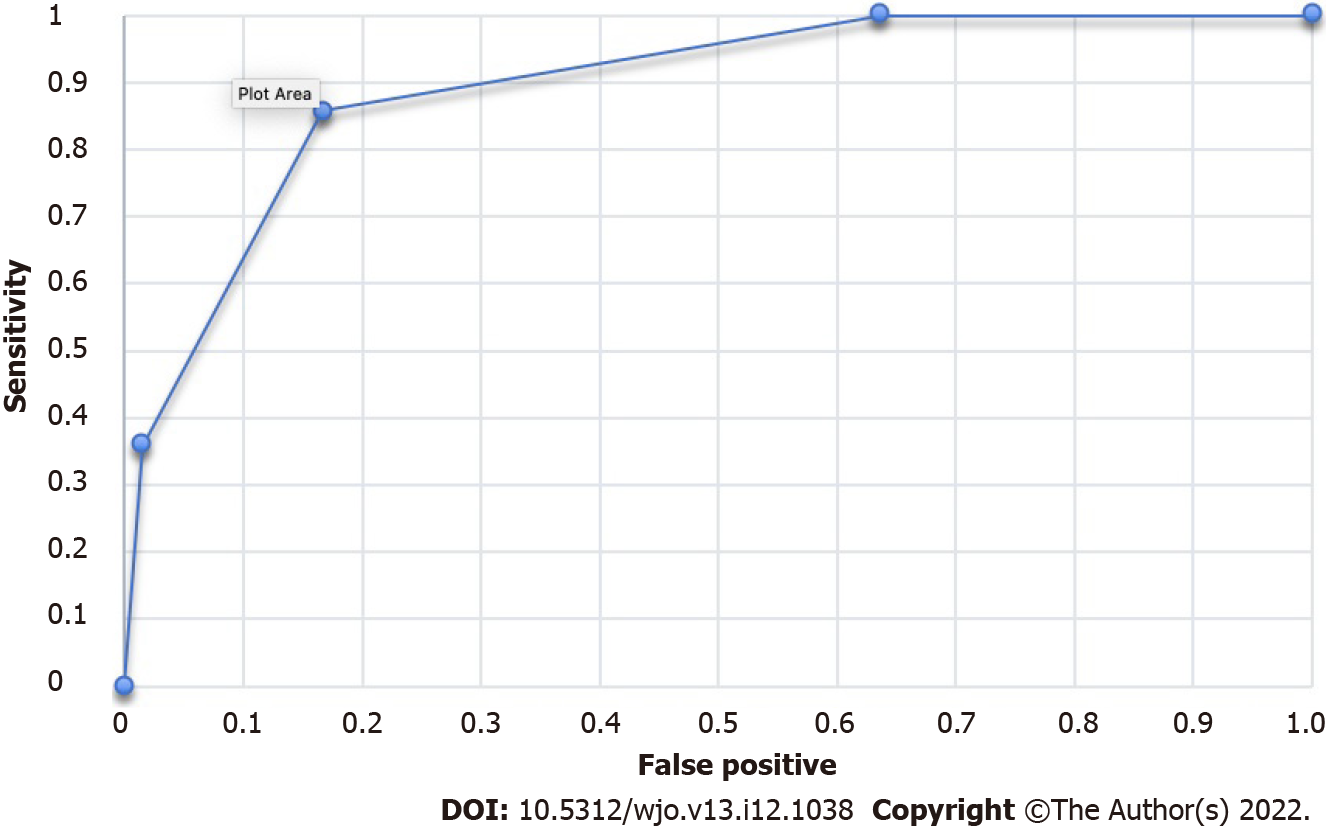
For each rotator cuff reparability score, sensitivity, specificity, positive and negative predictive value, as well as positive and negative likelihood ratios, were investigated (Table 2). The AUC of ROC curve was 0.894 (Figure 4). Two was the optimal cut-off score for rotator cuff reparability, with a sensitivity of 85.71% and a specificity of 83.33%.
| Rotator cuff reparability score | Sensitivity | Specificity | PPV | NPV | Positive likelihood ratio | Negative likelihood ratio |
| 1 | 100% | 36.36% | 25% | NA | 1.57 | 0 |
| 2 | 85.71% | 83.33% | 52.17% | 96.49% | 5.14 | 0.17 |
| 3 | 35.71% | 98.47% | 83.33% | 87.84% | 23.57 | 0.65 |
Arthroscopic rotator cuff repair is currently the standard treatment for rotator cuff tears. However, arthroscopic surgery is technically challenging in cases of large or massive rotator cuff tears. Previous studies have demonstrated that complete rotator cuff repair leads to superior functional results compared to partial rotator cuff repair[1,2,16,17]. Shon et al[3] suggested that arthroscopic partial repair may result in initial clinical improvements at two-year follow-up; however, over half of the study participants were dissatisfied with surgical outcomes which had worsened over time[3]. Heuberer et al[1] conducted a 45-mo follow-up study and demonstrated that partial rotator cuff repair was associated with higher re-rupture rates compared to complete rotator cuff repair.
Many salvage procedures have recently been developed for irreparable rotator cuff tears. However, there is a lack of studies comparing partial rotator cuff repair with other salvage procedures. A recent prospective cohort study comparing a latissimus dorsi muscle transfer with a partial rotator cuff repair in irreparable posterosuperior rotator cuff tears showed higher the University of California-Los Angeles (UCLA) shoulder scale, forward flexion, and shoulder strength in the muscle transfer group[8]. A cost-effective study by Makhni et al[18] revealed that arthroscopic rotator cuff repair may be a more cost-effective initial treatment for massive rotator cuff tears compared with primary reverse total shoulder arthroplasty. However, reverse total shoulder arthroplasty had superior outcomes in cases of rotator cuff repair failure or re-tear. The results of the study by Makhni et al[18] demonstrate the importance of comprehensive evaluation of the reparability of rotator cuff tears. Salvage procedures including superior capsular reconstruction, subacromial spacer, tendon transfer, and reverse total shoulder arthroplasty, are recommended in cases of irreparable rotator cuff tears after their utility in significantly improving functional outcomes was confirmed[19,20]. To our knowledge, no comparative studies of partial rotator cuff repair and salvage procedures have been reported to date. Accordingly, the assessment of rotator cuff reparability is clinically challenging, particularly in cases of large or massive rotator cuff tears. However, many factors have been reported to be associated with rotator cuff tear reparability and have utility in predicting treatment outcomes pre-operatively[1-3,17].
Rotator cuff injuries are a phenomenon of natural aging[21]. The majority of rotator cuff injuries are asymptomatic. However, 30% – 40% of patients with asymptomatic tears developed symptoms in the subsequent 2 to 5 years[22-23]. Larger rotator cuff tears are typically associated with degeneration and fatty infiltration[21,24]. Moreover, increasing age, particularly ≥ 65 years, has been shown to significantly correlate with rotator cuff tear irreparability[5-6].
Rotator cuff tears cause an imbalance between the forces acting on the glenohumeral joint, which can result in the humeral head superior migration, [25] which is one of the earliest signs of rotator cuff tear arthropathy[26]. The humeral head superior migration, as measured by the AHI or inferior glenohumeral distance, is an important factor in predicting the reparability and clinical outcomes of rotator cuff tears[4-7,27]. Previous studies have reported that an AHI ≤ 6 mm is associated with rotator cuff tear irreparability[4-5].
Tear size is another significant factor, which many studies reported as a main predicting factor of reparability[4-7,11,21]. Previous studies have determined rotator cuff tear size using different imaging modalities and in coronal and sagittal oblique views. Our previous study reported that both mediolateral tear size ≥ 36 mm and AP tear size ≥ 22 were associated with rotator cuff tear irreparability. This result corroborates a previous study by Di Benedetto et al[4]; however, their multiple logistic regression model demonstrated that only AP tear size was significantly correlated with rotator cuff tear irreparability.
A previous retrospective study reported the development of a quantitative scoring system for large-to-massive rotator cuff tears[6]. Their scoring system, which included AP tear size, mediolateral tear size, muscle atrophy, and fatty infiltration, had a sensitivity of 73.5% and a specificity of 96.2%. However, this study included only pre-operative MRI factors and not clinical and radiographic factors.
Our previous study analyzed all pre-operative clinical and radiographic factors to estimate the reparability of large and massive rotator cuff tears[5], demonstrating that age, AHI, and AP tear size were correlated with rotator cuff reparability. As all three factors had similar odd ratios, we weighted them equally to develop the present three-point scoring system.
In this study, the AUC for our rotator cuff reparability score was 0.894, indicating good accuracy. A score of two, which had a sensitivity of 85.71% and a specificity of 83.33%, was found to be the optimal cut-off rotator cuff reparability score. Accordingly, rotator cuff tears are most likely to be irreparable in patients with a score rotator cuff reparability of two or three. We recommend pre-operative consideration of backup procedures in such cases.
This study had several limitations. First, the retrospective nature of the present study may have introduced selection or information into the study analysis. Second, there was a wide range of participant ages which may have affected tissue quality and the likelihood of traumatic rotator cuff tears. Third, the small sample size and small number of patients in the partial repair group may have influenced the study results. Finally, clinical outcomes and follow-up were not assessed in the present study. Further studies are required to validate the clinical utility of our rotator cuff reparability score in improving clinical outcomes and provided satisfactory results after long-term follow-up.
A score of two is the optimal rotator cuff reparability score for predicting the reparability of large or massive rotator cuff tears. Patients with a pre-operative rotator cuff reparability score of two or greater are likely to have irreparable rotator cuff tears.
It is challenging to predict the reparability of a large and massive rotator cuff injury before surgery. Age, tendon retraction, tendon tear size, fatty infiltration, muscle atrophy, and superior humeral head migration are factors that influence whether or not large or massive rotator cuff tears can be repaired.
The better result and lower recurrent rate of complete rotator cuff repair, make the pre-operative evaluation much more important. If a complete repair is not possible, alternative salvage techniques with better results than partial rotator cuff repair should be considered.
The aim of the current study was to determine the accuracy of the rotator cuff reparability score.
This was a retrospective cohort diagnostic study including all patients with large and massive rotator cuff tears between January 2013 and December 2019. All patients underwent an arthroscopic rotator cuff repair and were classified as having either complete or partial rotator cuff repair. The sensitivity, specificity, positive and negative predictive value, and positive and negative likelihood ratio were assessed. The receiver operating characteristic curve was analyzed to define the optimal cut-off level for the reparability of the rotator cuff tear.
Eighty patients were recruited for this study. The intra- and inter-observer reliabilities were good to excellent. The number of patients with 0, 1, 2, and 3 positive factors were 24, 33, 17, and 6 respectively. The complete repair was done in all patients without any positive factors. Two of 32 patients with one positive factor and seven of 17 patients with two positive factors were partially repaired. Only one of six patients with three positive factors was completely repaired. The area under the curve was 0.894. The optimal cut-off point was two with the sensitivity of 85.71% and the specificity of 83.33%.
The optimal cut-off point for predicting the reparability of a large or massive rotator cuff tear is a rotator cuff reparability score of two. If the pre-operative score is two or more, the rotator cuff tear is likely to be irreparable.
Further studies are required to validate the clinical utility of our rotator cuff reparability score in improving clinical outcomes and provide satisfactory results after long-term follow-up.
The authors appreciate very much the support of the Biostatistics Excellence Center, Research Affairs, Faculty of Medicine, Chulalongkorn University for statistical consultation. The authors also acknowledge the Thai Orthopedic Society for Sports Medicine for academic support.
| 1. | Heuberer PR, Kölblinger R, Buchleitner S, Pauzenberger L, Laky B, Auffarth A, Moroder P, Salem S, Kriegleder B, Anderl W. Arthroscopic management of massive rotator cuff tears: an evaluation of debridement, complete, and partial repair with and without force couple restoration. Knee Surg Sports Traumatol Arthrosc. 2016;24:3828-3837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 67] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 2. | Lee YS, Jeong JY, Park CD, Kang SG, Yoo JC. Evaluation of the Risk Factors for a Rotator Cuff Retear After Repair Surgery. Am J Sports Med. 2017;45:1755-1761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 168] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 3. | Shon MS, Koh KH, Lim TK, Kim WJ, Kim KC, Yoo JC. Arthroscopic Partial Repair of Irreparable Rotator Cuff Tears: Preoperative Factors Associated With Outcome Deterioration Over 2 Years. Am J Sports Med. 2015;43:1965-1975. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 89] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 4. | Di Benedetto P, Beltrame A, Cicuto C, Battistella C, Gisonni R, Cainero V, Causero A. Rotator cuff tears reparability index based on pre-operative MRI: our experience. Acta Biomed. 2019;90:36-46. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 5. | Kuptniratsaikul V, Laohathaimongkol T, Umprai V, Yeekian C, Prasathaporn N. Pre-operative factors correlated with arthroscopic reparability of large-to-massive rotator cuff tears. BMC Musculoskelet Disord. 2019;20:111. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 6. | Kim SJ, Park JS, Lee KH, Lee BG. The development of a quantitative scoring system to predict whether a large-to-massive rotator cuff tear can be arthroscopically repaired. Bone Joint J. 2016;98-B:1656-1661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Dwyer T, Razmjou H, Henry P, Gosselin-Fournier S, Holtby R. Association between pre-operative magnetic resonance imaging and reparability of large and massive rotator cuff tears. Knee Surg Sports Traumatol Arthrosc. 2015;23:415-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 62] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 8. | Paribelli G, Boschi S, Randelli P, Compagnoni R, Leonardi F, Cassarino AM. Clinical outcome of latissimus dorsi tendon transfer and partial cuff repair in irreparable postero-superior rotator cuff tear. Musculoskelet Surg. 2015;99:127-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Millstein ES, Snyder SJ. Arthroscopic evaluation and management of rotator cuff tears. Orthop Clin North Am. 2003;34:507-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 31] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Aliprandi A, Messina C, Arrigoni P, Bandirali M, Di Leo G, Longo S, Magnani S, Mattiuz C, Randelli F, Sdao S, Sardanelli F, Sconfienza LM, Randelli P. Reporting rotator cuff tears on magnetic resonance arthrography using the Snyder's arthroscopic classification. World J Radiol. 2017;9:126-133. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Koh KH, Lim TK, Park YE, Lee SW, Park WH, Yoo JC. Preoperative factors affecting footprint coverage in rotator cuff repair. Am J Sports Med. 2014;42:869-876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Davidson JF, Burkhart SS, Richards DP, Campbell SE. Use of preoperative magnetic resonance imaging to predict rotator cuff tear pattern and method of repair. Arthroscopy. 2005;21:1428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 36] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Prasathaporn N, Kuptniratsaikul S, Kongrukgreatiyos K. Single-row repair versus double-row repair of full-thickness rotator cuff tears. Arthroscopy. 2011;27:978-985. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 55] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 14. | Zhang Q, Ge H, Zhou J, Yuan C, Chen K, Cheng B. Single-row or double-row fixation technique for full-thickness rotator cuff tears: a meta-analysis. PLoS One. 2013;8:e68515. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Xu C, Zhao J, Li D. Meta-analysis comparing single-row and double-row repair techniques in the arthroscopic treatment of rotator cuff tears. J Shoulder Elbow Surg. 2014;23:182-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 75] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 16. | Holtby R, Razmjou H. Relationship between clinical and surgical findings and reparability of large and massive rotator cuff tears: a longitudinal study. BMC Musculoskelet Disord. 2014;15:180. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 17. | Jenssen KK, Lundgreen K, Madsen JE, Kvakestad R, Dimmen S. Prognostic Factors for Functional Outcome After Rotator Cuff Repair: A Prospective Cohort Study With 2-Year Follow-up. Am J Sports Med. 2018;46:3463-3470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 18. | Makhni EC, Swart E, Steinhaus ME, Mather RC 3rd, Levine WN, Bach BR Jr, Romeo AA, Verma NN. Cost-Effectiveness of Reverse Total Shoulder Arthroplasty Versus Arthroscopic Rotator Cuff Repair for Symptomatic Large and Massive Rotator Cuff Tears. Arthroscopy. 2016;32:1771-1780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 59] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 19. | Catapano M, de Sa D, Ekhtiari S, Lin A, Bedi A, Lesniak BP. Arthroscopic Superior Capsular Reconstruction for Massive, Irreparable Rotator Cuff Tears: A Systematic Review of Modern Literature. Arthroscopy. 2019;35:1243-1253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 62] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 20. | Dickerson P, Pill SG, Longstaffe R, Shanley E, Thigpen CA, Kissenberth MJ. Systematic review of reversing pseudoparalysis of the shoulder due to massive, irreparable rotator cuff tears. J Shoulder Elbow Surg. 2020;29:S87-S91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 21. | Keener JD, Patterson BM, Orvets N, Chamberlain AM. Degenerative Rotator Cuff Tears: Refining Surgical Indications Based on Natural History Data. J Am Acad Orthop Surg. 2019;27:156-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 89] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 22. | Keener JD, Galatz LM, Teefey SA, Middleton WD, Steger-May K, Stobbs-Cucchi G, Patton R, Yamaguchi K. A prospective evaluation of survivorship of asymptomatic degenerative rotator cuff tears. J Bone Joint Surg Am. 2015;97:89-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 175] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 23. | Moosmayer S, Tariq R, Stiris M, Smith HJ. The natural history of asymptomatic rotator cuff tears: a three-year follow-up of fifty cases. J Bone Joint Surg Am. 2013;95:1249-1255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 143] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 24. | Gumina S, Carbone S, Campagna V, Candela V, Sacchetti FM, Giannicola G. The impact of aging on rotator cuff tear size. Musculoskelet Surg. 2013;97 Suppl 1:69-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 61] [Article Influence: 4.7] [Reference Citation Analysis (1)] |
| 25. | Nam D, Maak TG, Raphael BS, Kepler CK, Cross MB, Warren RF. Rotator cuff tear arthropathy: evaluation, diagnosis, and treatment: AAOS exhibit selection. J Bone Joint Surg Am. 2012;94:e34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 45] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 26. | Hamada K, Yamanaka K, Uchiyama Y, Mikasa T, Mikasa M. A radiographic classification of massive rotator cuff tear arthritis. Clin Orthop Relat Res. 2011;469:2452-2460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 202] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 27. | Vad VB, Warren RF, Altchek DW, O'Brien SJ, Rose HA, Wickiewicz TL. Negative prognostic factors in managing massive rotator cuff tears. Clin J Sport Med. 2002;12:151-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 36] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Thailand
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ghannam WM, Egypt; Oommen AT, India S-Editor: Liu GL L-Editor: Ma JY - MedE P-Editor: Liu GL