Published online Oct 18, 2022. doi: 10.5312/wjo.v13.i10.940
Peer-review started: October 4, 2021
First decision: January 11, 2022
Revised: March 28, 2022
Accepted: October 11, 2022
Article in press: October 11, 2022
Published online: October 18, 2022
Processing time: 377 Days and 12.9 Hours
Humeral shaft fractures are relatively common in adults. Rotational malalignment is reported as one complication but severe rotational deformity of the humerus is extremely rare. To our knowledge, only three cases of symptomatic humeral malrotation have been reported. There are sparse literature reports of humeral reconstruction correction.
We present a case of extreme rotational deformity of the humerus (180°) after humeral shaft fracture. The patient complained of pain and difficulties with activities of daily living. In addition, she found the deformity cosmetically unacceptable. Therefore, she was searching for surgical correction. Neurolysis of the radial nerve followed by derotational osteotomy of the humerus and internal fixation were performed. Postoperatively, the patient demonstrated transient iatrogenic radial nerve palsy which recovered completely during postoperative follow-up. The Disabilities of the Arm, Shoulder, and Hand score improved from 55 preoperatively to 16 at the final 2-year follow-up.
Single-stage radial neurolysis, derotational osteotomy and stable fixation is a feasible option to improve anatomic and functional problems of severely malrotated humeral shaft fractures.
Core Tip: We present a case of extreme rotational deformity of the humerus (180°) after humeral shaft fracture. The patient complained about pain and difficulties with activities of daily living. A neurolysis of the radial nerve followed by derotational osteotomy of the humerus and internal fixation were performed. Postoperatively, the patient demonstrated transient iatrogenic radial nerve palsy which had complete recovery at 2 years postoperatively. The Disabilities of the Arm, Shoulder, and Hand score improved from a preoperative 55 to a final 16 at the final 2-year follow-up.
- Citation: Wenning KE, Schildhauer TA, Jones CB, Hoffmann MF. Derotational osteotomy and internal fixation of a 180° malrotated humerus: A case report. World J Orthop 2022; 13(10): 940-948
- URL: https://www.wjgnet.com/2218-5836/full/v13/i10/940.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i10.940
Humeral shaft fractures are relatively common, accounting for approximately 1%-5% of all fractures and 20% of humeral fractures in adults[1-2]. These fractures have been historically regarded as benign fractures; as such, most are managed nonoperatively with functional bracing. The assumption of benign nature is based on the robust blood supply of the humerus, its limited weight-bearing characteristics and the technical ease of splint application[3-4].
Upper extremity function is primarily dependent on the hand’s ability to reach a desired point in space. Most studies of malalignment have focused on angulation[5-6]. Rotational malalignment has been reported as a possible complication of humeral shaft fractures, but considered normally tolerated and to not necessitate a surgical intervention. Nevertheless, extreme rotational deformity following humeral shaft fractures can occur and the recommended treatment for these entities has been rarely touched upon in the literature.
Herein, we describe a case of a 180° rotational deformity that developed after a midshaft humeral fracture that had been clinically addressed by nonoperative treatment which had resulted in shortening of the humerus, limited range of motion (ROM) of the shoulder, and flexion contracture of the elbow.
The patient complained of resting pain exacerbated with activities and severe limitations in activities of daily living. Furthermore, the cosmetic deformity was repulsive to her.
In 2009, the right-hand-dominant patient had sustained a traumatic left humeral shaft fracture which was treated nonoperatively. In 2019 at age 27, she was referred to our institution with severe malrotation of her left humerus associated with shortening of the upper arm and limited ROM of the shoulder and elbow. The patient complained about consistent pain which increases during activities and severe limitations of activities of daily living. Furthermore, the cosmetic deformity was repulsive to her.
There is no history of past illness.
Personal and family history are not known.
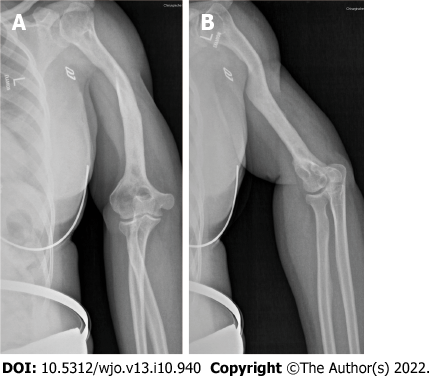
Physical examination detected a rotational deformity of the left upper arm of 180°. In supine position, the palm of her left hand and her olecranon were facing up (Figure 1). The Patient’s left arm was 5 cm shorter than her right (51 cm vs 56 cm). She complained of tenderness over the whole upper arm and movement-dependent pain in the shoulder region. No neurological deficits were diagnosed. Shoulder ROM was presented with only 80° of abduction (Table 1). The elbow demonstrated a flexion contracture of 85°. The patient’s forearm was fixed in neutral with total loss of pronation and supination. Wrist ROM was about normal.
| Preoperative | Postoperative | |
| Shoulder | ||
| Flexion/anteversion | 80° | 140° |
| Extension/retroversion | 20° | 25° |
| External rotation | 30° | 30° |
| Internal rotation | 60° | 60° |
| Abduction | 80° | 80° |
| Adduction | 10° | 20° |
| Elbow | ||
| Flexion | 85° | 90° |
| Extension | 0° | 0° |
| Pronation | 0° | 80° |
| Supination | 0° | 80° |
| Wrist | ||
| Flexion | 50° | 50° |
| Extension | 50° | 50° |
| Radial deviation | 20° | 20° |
| Ulnar deviation | 30° | 30° |
Laboratory examinations were unnecessary.
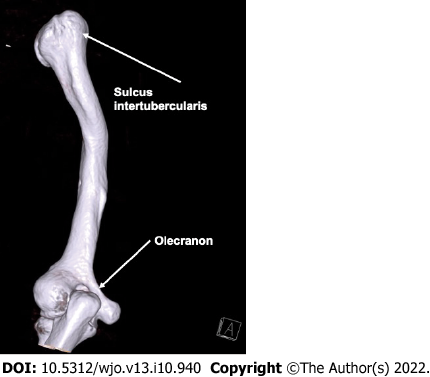
Radiographic imaging of the left shoulder and humerus demonstrated a malunited humeral shaft fracture with extensive remodeling and consolidated fracture site (Figure 2A). In addition, the shoulder displayed classic signs of post-traumatic osteoarthritis (Figure 2B). Preoperative three-dimensional computed tomography (3D CT) imaging confirmed a 180° malrotation of the humerus (Figure 3).
The patient demonstrated with rotational deformity of the left upper arm of 180°. Imaging of the left shoulder and upper arm revealed a malunited humeral fracture with extensive remodeling and fracture site consolidation.
Preoperatively, different surgical options were discussed with the patient and her family. The patient gave informed consent for a single staged procedure with complete radial nerve neurolysis followed by corrective osteotomy and internal fixation via plate fixation.
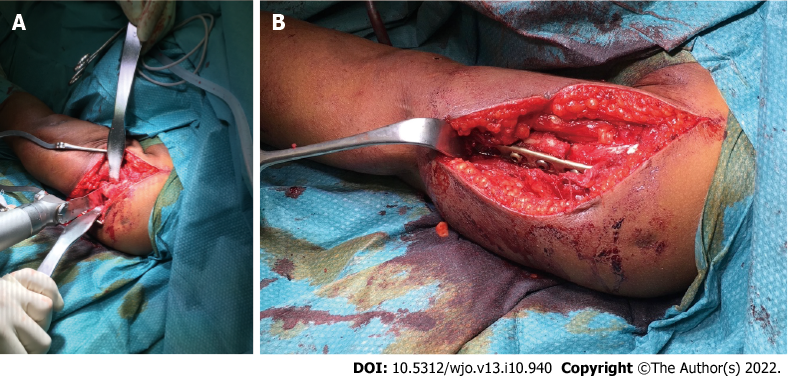
Ten years after the initial injury, the patient finally underwent derotational osteotomy with internal fixation of the left humerus and radial nerve exploration. Surgery was performed in the supine position under brachial plexus blocking and general anesthesia. Proximal humerus and the humeral shaft were exposed through a deltopectoral approach with extension distally anteriorly, following the anatomic muscles of the upper arm. Through the same anterior extensile incision, the radial nerve was exposed and released from the posterior aspect of the deltoid, through the lateral intermuscular septum, to the distal the arm in order not to lessen tension during the humeral derotation. A transverse osteotomy at the level of the consolidated fracture was performed carefully with a micro-oscillating saw and using instruments to protect surrounding and posterior soft tissues (Figure 4A). Subsequently, the entire distal humerus was rotated 180° demonstrating no tension to the radial nerve under direct visualization. Finally, internal fixation was performed utilizing an (3.5 mm or 4.5 mm) eight-hole dynamic compression plate [Limited Contact Dynamic Compression Plate System (LC-DCP); DePuySynthes, Warsaw, IN, United States] (Figures 4B and 5). Postoperatively, normal vascularity was noted, and soft compartments were noted, but a secondary or iatrogenic partial radial nerve palsy with weak wrist and digit extension and decreased light touch sensation in the radial nerve distribution. This injury was related to devascularization from dissection and manipulation of the nerve and less likely from the preoperative brachial plexus regional block. Secondary to the known intact and not impinged radial nerve at the end of the procedure, the patient and surgeons agreed to treat this transient radial nerve palsy with observation and did not re-explore the dissection.
The osteotomy zone was immobilized utilizing a Gilchrist-bandage for 4 wk postoperatively. Physical therapy with shoulder mobilization was initiated immediately after surgery. Shoulder and elbow ROM gradually increased and full ROM was allowed after 6 wk. Additionally, the weakened wrist muscles were immobilized in a functional splint and daily passive exercises were performed to maintain full ROM and to avoid contractures.
Initially, the skin incision had healed uneventfully and no signs of superficial or deep surgical site infection were noted. However, approximately 4 mo postoperatively, the patient presented with a deep surgical site infection with involvement of the osteosynthesis material and a non-consolidated osteotomy zone (an infected nonunion with fixation failure). Since the patient was healthy without comorbidities, she wanted to continue with therapy and avoid recurrence of the deformity. Therefore, a single stage revision was reviewed with the patient. Operative treatment consisted of plate removal with thorough excisional debridement, recanalization of the humerus, followed by re-osteosynthesis as a single staged procedure. Aerococcus viridans bacteria were detected in the deep intraoperative tissue cultures. Therefore, an antimicrobial therapy with clindamycin was initiated and continued for 6 wk.
After revision surgery, the patient did not present for follow-up appointments. We assumed that she was satisfied with the operative outcome and had resolution of the infection and preoperative functional difficulties. Approximately 2 years after initial surgery, we contacted the patient and scheduled an appointment. She reported a high level of satisfaction, resolution of infection, diminishment of pain, and a complete return to daily activities and caring of her two toddlers. Physical exam demonstrated complete healing of the soft tissues and resolution of the infection and imaging demonstrated consolidation of the osteotomy zone (Figure 6). The patient only complained of pain in her left upper arm and shoulder when carrying heavy objects or after a strenuous day with constant use of her arm. She demonstrated increased shoulder ROM: flexion/extension 140-0-25°, abduction/ adduction 80-0-20° and improved elbow ROM: flexion/extension 0-0-90°, with free supination and pronation. Compared to preoperative function, she demonstrated a marked improvement in all areas of arm motion. She did not have full shoulder ROM secondary to the preoperative, degenerative changes of her left shoulder (Figure 7). The patient described gradual improvement in the radial function within 3-4 mo of the initial surgery with complete recovery of the transient radial nerve palsy at the time of the follow-up examination. The patient completed the follow up Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire comparing the pre- and post-operative scores. The DASH score improved from a preoperative score of 55 to 16 at the final follow-up.
Although rotational malalignment is recognized as a possible complication of humeral shaft fractures in adults, extreme rotational deformities are extremely rare. Accordingly, the literature regarding this topic is sparse. To our knowledge, only three cases have been reported[7,8] and there are only a few papers regarding upper limb correction in general, with most focusing on non-traumatic and pediatric indications[9,10]. In contrast, deformity correction and bone lengthening of the lower extremities are standard techniques with an increasing number of reports appearing in the literature. External fixators (unilateral, multiaxial, or circular) are utilized. Bulky techniques, like Ilizarov external fixation or Taylor-Spatial-Frame are still practiced and offered as reliable treatment options[11,12]. For upper limb treatment, circular fixation techniques like the Ilizarov external fixator and Taylor-Spatial-Frame pose problems of discomfort because of the limited distance to the thorax. Additionally, proximal or midshaft humeral fractures provide only limited bone stock for proximal fixation for all external fixation systems.
In our patient, the indications for operative intervention were the cosmetically unacceptable condition of a 180° malrotated arm as well as the inability to perform routine daily activities. She also reported limited ROM and severe pain of her left arm during shoulder movement. More extensive deformity corrections are usually performed as staged or continuous procedures utilizing external fixation to preserve neural structures and blood supply[13]. In our case, we decided against surgical correction by an external fixator for several reasons. On the one hand, the patient declined treatment with an Ilizarov fixator, citing the extensive follow-up care associated with it. Additionally, we needed a quick solution because it was unclear how long the patient would be in the area and available for follow-up and stepwise correction.
Although the patient’s left arm already presented with a shorter length preoperatively, this condition did not bother our patient. Due to the decision just to perform a rotational correction and no lengthening of the arm, we chose derotational osteotomy, and exposure and release of the radial nerve by internal fixation. We assumed that exposing the nerve would reduce the risk for radial nerve injury. Nevertheless, the patient experienced radial nerve palsy postoperatively. Because of the good visualization of the radial nerve, we were able to rule out disruption or compression. There are reports of radial nerve injuries after deformity correction of the upper limb with different fixation systems[11,14] as well as after closed reduction of severe rotational deformity of the humerus[8]. Data on iatrogenic radial nerve injuries for open procedures vary between 6%-32%[15,16].
Regarding treatment, no clear consensus exists regarding if and when the nerve should be surgically explored[17]. Some authors recommend early exploration in cases of secondary nerve palsy[18], others advocate observation for a 4-to-6-mo period[19,20]. According to the literature, secondary radial nerve palsy has a good overall recovery rate of 93%[21]. In our case, the “wait and see” strategy was sufficient as the patient achieved complete neurological recovery. An increasing improvement in the radial nerve palsy was observed already after 4 mo. Two years after the initial surgery, the neurologic deficit had completely recovered, but the exact time point remains unclear because of the discontinued follow-up visits.
Different treatment options for surgical site infections and infected nonunions during a single or staged procedure have been discussed[22,23]. Due to the fact that our patient presented with infection 4 mo postoperatively, nonunion with secondary infection was assumed. Wu et al[24] reported a preference for single-stage treatment to address infected nonunions with Ilizarov fixation. Since our patient was healthy without comorbidities, we respected her request to continue with the initial therapy in order to avoid external fixation or recurrence of the deformity. Therefore, thorough debridement and hardware exchange were performed as a single-stage revision. Olszewski et al[22] reported their support of such an approach, based upon their data showing that 78% of patients healed after an index procedure and were able to avoid external fixation.
Bae et al[25] also described a case of severe malrotation of the humerus after humeral shaft fracture. Similar to our treatment, those authors described the performance of a derotation osteotomy of the left humerus with internal fixation and exposure of the radial nerve. They also reported a good postoperative result without neurological deficits.
In our case, the patient benefited greatly from the surgical procedure. Her preoperative DASH score was quite high (at 55) and had improved significantly after the deformity correction (to 16). Her 180° malrotated left upper arm represented a cosmetic problem, serving as a mental burden and significantly impairing her functional activities of daily living. Therefore, our treatment aimed for correction of the deformity, improvement of function, pain reduction, and achievement of the desired cosmetic result. These goals were achieved with very good results. The humeral malrotation has been entirely corrected and the overall deformity was reduced. Above all, shoulder ROM (especially shoulder flexion: 80° vs 140°) and pronation/supination of the elbow (0° vs 80°) increased significantly due to a more anatomic position of the humeral head articular surface. Some limitations persisted due to pre-existing degenerative changes. Furthermore, the flexion contracture of the elbow could not be resolved because of the long existing malalignment of the upper limb.
The patient noticed relevant pain relief from “severe” (preoperative) to “no” or “mild” pain postoperatively. At the 2-year follow-up appointment, she was very satisfied with the result of the operation. She indicated that she occasionally has pain in her left arm while carrying heavy objects. Ultimately, she stated that she is now living a normal life with her children without limitations in her everyday activities.
Our case complements the sparse literature of extreme malrotation deformity of the humerus and illustrates that corrective osteotomy with internal fixation may be a feasible treatment approach to avoid uncomfortable circular external fixation and to reach good postoperative results. It is a valid method that improved outcomes following deformity correction. We admit that a stepwise procedure utilizing a fixator (e.g., a Taylor-Spatial frame) would have offered the option of additional lengthening.
Malalignment after humeral shaft fractures often includes a malrotation component. Extensive rotational correction is rare and the literature is sparse. Common procedures for extensive alignment correction utilizing circular external fixations cause a great amount of discomfort, especially when utilized on the proximal or midshaft humerus. Acute rotational correction of 180° is feasible and can lead to good clinical results when performed carefully.
| 1. | Gallusser N, Barimani B, Vauclair F. Humeral shaft fractures. EFORT Open Rev. 2021;6:24-34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 54] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 2. | Brinker MR, O'Connor DP. The incidence of fractures and dislocations referred for orthopaedic services in a capitated population. J Bone Joint Surg Am. 2004;86:290-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 92] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 3. | Rämö L, Sumrein BO, Lepola V, Lähdeoja T, Ranstam J, Paavola M, Järvinen T, Taimela S; FISH Investigators. Effect of Surgery vs Functional Bracing on Functional Outcome Among Patients With Closed Displaced Humeral Shaft Fractures: The FISH Randomized Clinical Trial. JAMA. 2020;323:1792-1801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 84] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 4. | Garnavos C. Humeral Shaft Fractures. Rockwood Green’s Fract Adults Philadelphia Wolters Kluwer. 2020; 1: 1231-1291. |
| 5. | Arora R, Fichadia U, Hartwig E, Kannikeswaran N. Pediatric upper-extremity fractures. Pediatr Ann. 2014;43:196-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Robinson CM, Wylie JR, Ray AG, Dempster NJ, Olabi B, Seah KT, Akhtar MA. Proximal humeral fractures with a severe varus deformity treated by fixation with a locking plate. J Bone Joint Surg Br. 2010;92:672-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 42] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 7. | Hawi N, Razaeian S, Krettek C, Meller R, Liodakis E. [Torsional malalignment of the humerus]. Unfallchirurg. 2018;121:199-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (1)] |
| 8. | Chan D, Petricciuolo F, Maffulli N. Fracture of the humeral diaphysis with extreme rotation. Acta Orthop Belg. 1991;57:427-429. |
| 9. | Farr S, Mindler G, Ganger R, Girsch W. Bone Lengthening in the Pediatric Upper Extremity. J Bone Joint Surg Am. 2016;98:1490-1503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Tellisi N, Ilizarov S, Fragomen AT, Rozbruch SR. Humeral lengthening and deformity correction in Ollier's disease: distraction osteogenesis with a multiaxial correction frame. J Pediatr Orthop B. 2008;17:152-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Hosny GA. Humeral lengthening and deformity correction. J Child Orthop. 2016;10:585-592. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 12. | Malkova TA, Borzunov DY. International recognition of the Ilizarov bone reconstruction techniques: Current practice and research (dedicated to 100th birthday of G. A. Ilizarov). World J Orthop. 2021;12:515-533. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (3)] |
| 13. | Goodier WD, Calder PR. External fixation for the correction of adult post-traumatic deformities. Injury. 2019;50 Suppl 1:S36-S44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Malot R, Park KW, Song SH, Kwon HN, Song HR. Role of hybrid monolateral fixators in managing humeral length and deformity correction. Acta Orthop. 2013;84:280-285. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | Hak DJ. Radial nerve palsy associated with humeral shaft fractures. Orthopedics. 2009;32:111. [RCA] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Bumbasirević M, Lesić A, Bumbasirević V, Cobeljić G, Milosević I, Atkinson HD. The management of humeral shaft fractures with associated radial nerve palsy: a review of 117 cases. Arch Orthop Trauma Surg. 2010;130:519-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 54] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 17. | Schwab TR, Stillhard PF, Schibli S, Furrer M, Sommer C. Radial nerve palsy in humeral shaft fractures with internal fixation: analysis of management and outcome. Eur J Trauma Emerg Surg. 2018;44:235-243. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 85] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 18. | Kwasny O, Maier R, Kutscha-Lissberg F, Scharf W. [Treatment procedure in humeral shaft fractures with primary or secondary radial nerve damage]. Unfallchirurgie. 1992;18:168-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Liu GY, Zhang CY, Wu HW. Comparison of initial nonoperative and operative management of radial nerve palsy associated with acute humeral shaft fractures. Orthopedics. 2012;35:702-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 20. | Wang JP, Shen WJ, Chen WM, Huang CK, Shen YS, Chen TH. Iatrogenic radial nerve palsy after operative management of humeral shaft fractures. J Trauma. 2009;66:800-803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 62] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 21. | Korompilias AV, Lykissas MG, Kostas-Agnantis IP, Vekris MD, Soucacos PN, Beris AE. Approach to radial nerve palsy caused by humerus shaft fracture: is primary exploration necessary? Injury. 2013;44:323-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 59] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 22. | Olszewski D, Streubel PN, Stucken C, Ricci WM, Hoffmann MF, Jones CB, Sietsema DL, Tornetta P 3rd. Fate of Patients With a "Surprise" Positive Culture After Nonunion Surgery. J Orthop Trauma. 2016;30:e19-e23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 49] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 23. | Nasser AAH, Fenton P, Bose D. Single stage versus two-stage orthoplastic management of bone infection. Injury. 2022;53:984-991. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 24. | Wu CC. Single-stage surgical treatment of infected nonunion of the distal tibia. J Orthop Trauma. 2011;25:156-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 25. | Bae H, Widmann RF, Hotchkiss RN. Extreme rotational malunion of the humerus. A case report. J Bone Joint Surg Am. 2001;83:424-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Germany
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Abulsoud MI, Egypt; Abulsoud MI, Egypt; Muthu S, India S-Editor: Wu YXJ L-Editor: Filipodia P-Editor: Wu YXJ