Published online Jul 18, 2021. doi: 10.5312/wjo.v12.i7.456
Peer-review started: March 23, 2021
First decision: May 3, 2021
Revised: May 6, 2021
Accepted: June 4, 2021
Article in press: June 4, 2021
Published online: July 18, 2021
Processing time: 113 Days and 15.1 Hours
Fractures of femur proximal extremity (FFPE) are the most common fragility fractures requiring hospitalization, with a high risk of mortality, low independence in the activities of daily living and severe consequences on health-related quality of life. Timing for surgery has a key role in the management of elderly patients with FFPE as recommended by the Australian and New Zealand guidelines and the National Institute for Health and Care Excellence guidelines. Early surgery (within 48 h from hospital admission) allows significant benefits in terms of lower rates of postoperative complications and risk of death and can provide better functional outcomes. Therefore, time for surgery could be considered as a comorbidity marker. The choice between conservative or surgical approach surprisingly seems to be still not strongly supported by available literature, but it seems that both 30 d and 1 year risk of mortality is higher with the conservative treatment rather than with surgery. In light of these considerations, the optimization of FFPE management care is mandatory to improve functional outcomes and to reduce sanitary costs. Albeit it is widely accepted that transdisciplinary approach to patients suffering from FFPE is mandatory to optimize both short-term and long-term outcomes, the feasibility of a comprehensive approach in clinical practice is still a challenge. In particular, the large variability of figures involved could be considered both a resource and an additional disadvantage taking into account the difficulty to coordinate multidis
Core Tip: Optimization of fractures of femur proximal extremity management care is mandatory in order to improve functional outcomes and reduce sanitary costs. Albeit it is widely accepted that the transdisciplinary approach to patients suffering from fractures of femur proximal extremity is mandatory to optimize both short-term and long-term outcomes, the feasibility of a comprehensive approach in practice is still a challenge. Therefore, by the present study, we portray the potential benefits of transdisciplinary management of patients with fractures of femur proximal extremity, highlighting feasibility and limitations of this approach.
- Citation: de Sire A, Invernizzi M, Baricich A, Lippi L, Ammendolia A, Grassi FA, Leigheb M. Optimization of transdisciplinary management of elderly with femur proximal extremity fracture: A patient-tailored plan from orthopaedics to rehabilitation. World J Orthop 2021; 12(7): 456-466
- URL: https://www.wjgnet.com/2218-5836/full/v12/i7/456.htm
- DOI: https://dx.doi.org/10.5312/wjo.v12.i7.456
Fractures of femur proximal extremity (FFPE) are the most common fragility fractures requiring hospitalization[1], with a high risk of mortality[2], low independence in the activities of daily living[3] and severe consequences on health-related quality of life[4].
FPE fracture patients are expected to increase worldwide due to the aging popula
Aging is considered an independent, non-modifiable risk factor for fragility fracture, with over 90% of FFPE occurring in patients aged more than 65 years suffering from pre-existing medical comorbidities[10]. Disability related to hip fractures is responsible for major health care expenditures resulting from both medical care and assistance that should be associated with the sanitary costs due to surgical procedures and hospitalization[11-13]. Furthermore, a recent systematic review by Downey et al[14] reported that hospitalization costs for hip fracture patients during the first year might be estimated as £14000 (€15900/$18750) per patient.
Taken together, all these findings highlight that the optimization of hip fracture management care is mandatory in order to improve functional outcomes and to reduce sanitary costs. To date, it is widely accepted that the transdisciplinary approach to patients suffering from hip fractures is mandatory in the correct management of this condition to optimize both short-term and long-term outcomes[15]. More in detail, the Australian and New Zealand Guidelines[16] and the National Institute for Health and Care Excellence (NICE) guidelines[17] support a coordinated multidisciplinary approach covering care in all settings, from the ambulance to the discharge destin
Therefore, an adequate coordination of different figures including orthopaedic surgeons, physical and rehabilitation physicians, geriatric physicians, physical therapists and caregivers should be planned for hip fracture patients.
The aim of the present article was to summarize current evidence supporting transdisciplinary management of patients with fracture of the proximal extremity of femur, highlighting the benefits, feasibility and limitations of this approach.
It is widely accepted that timing for surgery has a key role in FFPE management[18-20], as also affirmed by the NICE guidelines[17] that recommended that an early surgery (within the first day or next day from the admission) improved functional outcomes in older patients with FFPE.
In this scenario, a recent meta-analysis performed by Simunovic et al[21] assessed the effects of surgery performed within the 72 h controlling for comorbidities, reporting significant benefits in terms of risk of death and lower rates of postoperative complications. Despite previous large studies suggesting that time for surgery could be considered as a comorbidity marker[22,23], higher rate of mortality and compli
Albeit the early surgical approach is supported by high level of evidence according to both Australian and New Zealand[16] and NICE guidelines[17], the choice between conservative or surgical approach surprisingly seems to not be strongly supported by available literature. In particular, a Cochrane systematic review by Handoll et al[26] reported several biases in studies supporting surgical management, and the limited available evidence did not show significant differences between conservative and surgical management.
A recent systematic review and meta-analysis[27] assessed randomized controlled trials comparing conservative and surgical treatment. The authors included seven observational studies with a total of 1189 patients reporting that both 30 d and 1 year mortalities were higher in the conservative group rather than the surgical group (odds ratio (OR): 3.95, 95% confidence interval (CI): 1.43-10.96; OR: 3.84, 95%CI: 1.57- 9.41). Unfortunately, functional outcomes and health-related quality of life were not assessed by these studies.
Altogether, these findings suggest that early surgical approach should be considered in elderly patients suffering from FFPE, taking into account the need for a transdisciplinary integrated management of these patients.
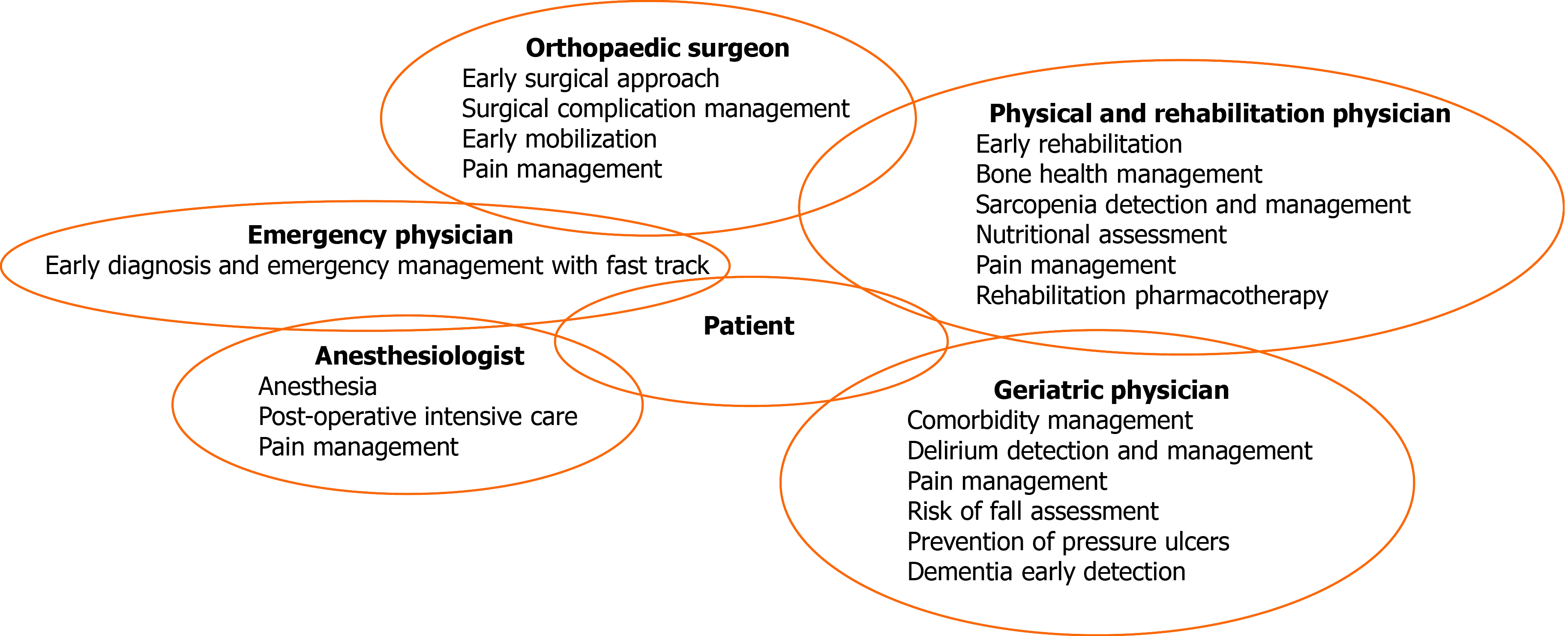
A transdisciplinary management of FFPE patients started from a model of a “fracture liaison service” that might reduce the osteoporosis treatment gap, improving functional outcomes in these patients[28-30]. Figure 1 describes a model of a transdisciplinary management of patients with FFPE.
Lin et al[31] recently performed a meta-analysis assessing the effects of comprehensive geriatric care. They reported a consistent decrease of overall mortality (OR: 0.71; 95%CI: 0.53-0.95), whereas independence in activities of daily living significantly improved (standardized mean difference: 0.29; 95%CI: 0.12-0.47). Despite reports that hospital-based transdisciplinary rehabilitation could be more expensive than usual care, the sanitary costs may be offset by the benefits in terms of reduced length of stay and independence at discharge[32].
Furthermore, interdisciplinary management might play a key role also in the screening for common co-occurring conditions, such as delirium or pain[33]. In particular, delirium is very common after hip fractures, with a prevalence between 13.5% to 33.0%[34] and was shown to negatively affect clinical and functional outcomes[35,36]. Unfortunately, the clinical manifestations are heterogeneous, ranging from a hyperactive delirium, characterized by irritability, pressured speech and uneasiness to a hypoactive delirium, characterized by quiet mobility reduction, special-temporal disorientation, carelessness and trouble to answer simple questions[37]. A transdisciplinary screening for delirium should be provided across the FFPE management to avoid detrimental consequences on functional outcomes, complications and even mortality[10]. Unfortunately, routine assessment remains uncommon with approximately 39% of hip fracture patients suffering from delirium at discharge and 32% at 1 mo after fracture[36].
Taking into account that pain is a major risk factor for delirium, adequate management is mandatory to reduce delirium onset[10,38]. NICE guidelines[17] recommend analgesia administration within the first 30 min from hospital admission. Paracetamol should be considered as first-line in the management of the elderly with FFPE. However, frequent analgesia targets were not reached by paracetamol administration only. Therefore, oral opioids should be considered even if intravenous opioids provide faster relief[39]. Recently, peripheral nerve blocks have been introduced in managing pain and minimizing the side effects and sedation related to opioid drugs[40,41]. In addition, continuous blocks can be included after surgical intervention for postoperative analgesia, with potentially positive effects in terms of pain, confusional state and probably in time to the first mobilization[42].
In this context, an early rehabilitation might reduce pain in FFPE patients and should be adequately planned particularly in elderly patients.
Rehabilitation is recommended by the main Osteoporosis Guidelines available in the literature in patients with osteoporotic FFPE[43]. The main goals of the rehabilitation management are reducing pain, improving physical function, independence in activities of daily living and health-related quality of life[44]. Oldmeadow et al[45] reported potential benefits of walking 24 h or 48 h from surgery compared to delayed assisted ambulation after 3 d or 4 d from surgery. Moreover, a higher rate of discharge to home (26.3%) was recorded compared to the delayed ambulation group (2.4%). In a single-blinded cohort study, Overgaard et al[46] assessed progressive strength training shortly (17.5 ± 5.7 d) after FFPE surgery in outpatients, with positive effects in terms of pain and functional outcome measurements.
In this context, rehabilitation plays a key role in the comprehensive management of FFPE patients, taking into account the positive effects of exercise in the recovery of functional status[47] and for balance and prevention of risk of falling, which is a major determinant of refracture occurrence[48].
During the transdisciplinary management of FFPE patients, caregivers should be included across the whole pathway[49,50]. As a matter of fact, functional impairment resulting from FFPE in elderly patients require long-term care in different settings. Albeit the transition from hospital to home should be conducted by health professionals[51], in outpatient settings, caregivers should be informed and trained with health education programs in order to optimize patient management at home[52-54].
In this scenario, long-term management of FFPE patients should include osteoporosis and sarcopenia screening[17]. In light of this consideration, dual-energy x-ray absorptiometry should be performed to provide data of the baseline condition and treatment monitoring, whereas bone densitometry exams are not mandatory to start anabolic/antiresorptive treatment. However, promising studies showed that ultrasound assessment might be used for osteoporosis diagnosis[55,56].
Despite bone health playing a key role in patients suffering from FFPE, the optimal management of patients with fragility fractures is still evolving, with new pharmacological therapeutic strategies including sequential therapies aimed at optimizing bone formation or inhibit bone resorption[57].
Bisphosphonates are still the osteoporosis drug most commonly prescribed, characterized by antiresorptive action induced by osteoclast function inhibition[57,58]. However, denosumab, a fully human IgG2 monoclonal antibody preventing the development of osteoclasts by RANK inhibition, has been introduced as effective therapy for osteoporosis in the last decade[58,59]. In contrast, an anabolic drug such as teriparatide might stimulate bone formation and could be used in FFPE patients for a limited period of time (anabolic window)[60].
Several exercise modalities have been proposed as nonpharmacological treatments to prevent bone loss, increase bone mineral density and reduce fall risk[61]. In particular, balance training, weight-bearing, strength training, progressive resistance exercise and Tai Chi seem to be effective in both osteoporosis prevention and treatment. Moreover, these exercise trainings were encouraged by national and international recommendations[62]. Exercise therapy should be tailored to patients’ characteristics, focusing on back extensors and hip muscles due to the widely noted osteogenic effects of physical exercise and the improvement in terms of balance control[63,64].
Moreover, besides osteoporosis management, physicians should focus on sarcopenia, taking into account the strict relation among muscle strength, function impairment and risk of fall. More in detail, sarcopenia is considered a multifactorial common condition sharing several pathophysiological mechanisms with osteoporotic hip fracture patients[47].
A recent meta-analysis including more than 10000 older patients reported that sarcopenic patients have a higher risk of falls compared to non-sarcopenic ones (pooled OR: 1.52, 95%CI: 1.32-1.77, I2= 39.1%)[65]. However, risk of fall is not the only mechanism linking sarcopenia and FFPE. Indeed, sarcopenia and osteoporosis share several underlying pathogenic factors, including cellular biomolecular pathways involving muscle-derived cytokines (myokines) influencing bone density, growth and repair[66].
Moreover, albeit aging is the most common risk factor for sarcopenia, malnutrition has been widely recognised to be strictly related to sarcopenia onset. In this context, previous studies reported a malnutrition prevalence in hip fracture patients ranging from 40% to 80% of hospitalized patients[67,68]. Furthermore, it has been reported that malnutrition may be considered a risk factor for FFPE, and it is a strong predictor of poor functional recovery[10,67]. In this scenario, oral nutrition supplementation has been proposed to reduce minor postoperative complications after FFPE, with promising results even in overall length of stay[69-71]. Nevertheless, a recent systematic review reported several methodological flaws on trials supporting oral supplementation, underlining that nutritional interventions were supported by only weak evidence[69]. In addition, nutrient supplementation without exercise seems ineffective in muscle strength improvement or physical frailty[72,73].
On the other hand, it has been reported that micronutrients might play a key role in the musculoskeletal system, promoting muscle anabolism and functioning in older people[74,75]. Therefore, combined nutrition and physical exercise might be crucial to treat complex and multifactorial conditions affecting the musculoskeletal system, including sarcopenia in hip fracture patients[76,77].
Taking into account these findings, our group has recently performed a pilot randomized controlled trial[47] to assess the effects of a transdisciplinary rehabilitative and nutritional approach, showing promising results in terms of strength and physical function in sarcopenic hip fracture patients. Moreover, a further analysis in a subgroup of this population suggested that serum myostatin levels might be considered as promising biomarkers of sarcopenia in hip fracture patients undergoing rehabilitation after orthopaedic surgery[78].
In this scenario, the “rehabilitation pharmacotherapy” has been recently introduced to characterize medical management based on optimization of functional outcomes and minimization of adverse effects on nutritional status[79].
Thus, these findings suggested that a comprehensive long-term patient-tailored rehabilitative approach should be planned for the elderly with FFPE to optimize physical exercise, nutritional intake, bone health and medical drugs to promote complete functional recovery of frail patients.
However, despite the large amount of literature supporting a transdisciplinary approach in the elderly suffering from FFPE, the feasibility in most hospital settings still remains difficult. We retain that this approach might optimize the integration among hospital care management, rehabilitative outcomes and ensure continuity of care at discharge[80,81].
Dementia is a cognitive disorder characterized by intellectual function impairment affecting both function and social performance[82,83]. Recent studies[84,85] reported that approximately 19% of patients with FFPE meet diagnostic criteria for dementia. In addition, considering that age represents one of the most common risk factors for dementia, the number of hip fracture patients with dementia is expected to increase worldwide. To date, previous evidence showed that FFPE older patients with dementia were admitted to long-term care more frequently, and the mortality rate was significantly higher in these patients[86]. In this scenario, targeted interventions are needed to optimize a multidisciplinary management of hip fracture patients with dementia. In particular, structured and familiarised routines, orientation to environ
Despite physical and cognitive rehabilitation were considered as effective therapies to improve functional and performance outcomes in elderly, a gap in the current literature in terms of effectiveness in patients with dementia has been shown[88]. Similarly, a recent Cochrane systematic review[89] reported very low-quality evidence supporting geriatrician-led recovery and enhanced rehabilitation strategies in the functional recovery of elderly patients with dementia after FFPE surgery.
Therefore, the optimization of rehabilitative pathways in these particular patients might be considered a challenge. However, multidisciplinary management should be tailored to the patients in order to overpass cognitive impairment limitations to optimize functional outcomes of patients with dementia. Unfortunately, albeit the optimal rehabilitation and care model is still uncertain, an early detention in addition to dementia-focused treatment might be considered in the future, taking into account the potential role of assistive technologies and caregivers in the recovery pathway of these patients.
Furthermore, in light of these considerations, fragility fracture prevention should be emphasized to improve long-term management of patients with dementia. In contrast, it has been reported that dementia could be strictly linked to osteoporosis[90]. However, bone health management could be frequently underestimated in the elderly with cognitive impairment due to the short life expectancy of these patients[91]. On the other hand, a growing number of papers underlined poor compliance with osteoporosis drugs, especially in patients with dementia or elderly with polypharmacotherapy[92].
Therefore, given the high sanitary burden and the social consequences of fragility fracture recurrence, osteoporosis management should be emphasized considering subcutaneous denosumab or annual zoledronic acid infusions characterized by a lower discontinuation rate and earlier onset of efficacy in fracture reduction[93], with possible implications in long-term outcomes of patients after fragility fractures with dementia.
Albeit the aim of the present article was to underline the key role of transdisciplinary management of patients with FFPE, some limitations should be taken into account before drawing conclusions.
First, in the clinical scenario, FFPEs are composed by a wide variability of anatomic presentations including head fractures, femur neck fractures, intertrochanteric fractures, subtrochanteric fractures and proximal femur shaft fractures. In the era of precision medicine, we are aware that a specific stratification should be provided to clearly present data of FFPE, given the strict linking among anatomic presentation, surgical intervention, bone health and rehabilitation. Unfortunately, the present editorial did not distinguish FFPEs; however, this intrinsic limitation reflects the high number of studies in the literature considering FFPE as a single pathology, resulting in a wrong generalization of study results probably affected by the type of fracture, with crucial implication in terms of evidence supporting a patient-tailored therapeutic plan.
Furthermore, it should be noticed that the high heterogeneity of key topics discussed in the present study did not allow a systematic review to be performed. In light of these considerations, a narrative analytical technique has been performed to highlight the gaps in the current literature and to guide future research and clinicians in a tailored transdisciplinary management of FFPE.
Taken together, the optimization of FFPE patient management should be considered as crucial to avoid the detrimental consequences on functional outcomes and the assistance and healthcare burden related to fragility fractures. Albeit the current literature supports a transdisciplinary care of elderly patients suffering from FFPE, global challenges still exist to implement these findings in the common clinical practice. The main limitation in terms of generalization of organization models might be found in the large heterogeneity of settings, healthcare models, community opportunities and specializations involved in the complex management of these patients. It would be optimal to be able to organize the care of these patients in multidisciplinary hospital wards of orthogeriatrics. However, this editorial was meant to describe the need to define a tailored transdisciplinary management that could be performed in the common clinical practice to reduce functional and social consequences of patients with FFPE. Further studies are warranted to define feasible organization models supported by clear evidence to manage FFPE patients across the whole health care pathway, in both inpatient and outpatient settings.
| 1. | Tarantino U, Capone A, Planta M, D'Arienzo M, Letizia Mauro G, Impagliazzo A, Formica A, Pallotta F, Patella V, Spinarelli A, Pazzaglia U, Zarattini G, Roselli M, Montanari G, Sessa G, Privitera M, Verdoia C, Corradini C, Feola M, Padolino A, Saturnino L, Scialdoni A, Rao C, Iolascon G, Brandi ML, Piscitelli P. The incidence of hip, forearm, humeral, ankle, and vertebral fragility fractures in Italy: results from a 3-year multicenter study. Arthritis Res Ther. 2010;12:R226. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 73] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 2. | Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331:1374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 970] [Cited by in RCA: 1040] [Article Influence: 49.5] [Reference Citation Analysis (0)] |
| 3. | Magaziner J, Fredman L, Hawkes W, Hebel JR, Zimmerman S, Orwig DL, Wehren L. Changes in functional status attributable to hip fracture: a comparison of hip fracture patients to community-dwelling aged. Am J Epidemiol. 2003;157:1023-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 205] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 4. | Cree M, Carriere KC, Soskolne CL, Suarez-Almazor M. Functional dependence after hip fracture. Am J Phys Med Rehabil. 2001;80:736-743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 49] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Piscitelli P, Brandi M, Cawston H, Gauthier A, Kanis JA, Compston J, Borgström F, Cooper C, McCloskey E. Epidemiological burden of postmenopausal osteoporosis in Italy from 2010 to 2020: estimations from a disease model. Calcif Tissue Int. 2014;95:419-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Toro G, Calabrò G, Toro A, de Sire A, Iolascon G. Locking plate fixation of distal femoral fractures is a challenging technique: a retrospective review. Clin Cases Miner Bone Metab. 2015;12:55-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Cooper C, Cole ZA, Holroyd CR, Earl SC, Harvey NC, Dennison EM, Melton LJ, Cummings SR, Kanis JA; IOF CSA Working Group on Fracture Epidemiology. Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int. 2011;22:1277-1288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 729] [Cited by in RCA: 703] [Article Influence: 46.9] [Reference Citation Analysis (0)] |
| 8. | Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl DA, Cooper C; IOF Working Group on Epidemiology and Quality of Life. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int. 2012;23:2239-2256. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1083] [Cited by in RCA: 1049] [Article Influence: 74.9] [Reference Citation Analysis (0)] |
| 9. | Cooper C, Campion G, Melton LJ 3rd. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2:285-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1996] [Cited by in RCA: 1987] [Article Influence: 58.4] [Reference Citation Analysis (0)] |
| 10. | Carpintero P, Caeiro JR, Carpintero R, Morales A, Silva S, Mesa M. Complications of hip fractures: A review. World J Orthop. 2014;5:402-411. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 183] [Cited by in RCA: 248] [Article Influence: 20.7] [Reference Citation Analysis (6)] |
| 11. | Huddleston JM, Whitford KJ. Medical care of elderly patients with hip fractures. Mayo Clin Proc. 2001;76:295-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 53] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 12. | Cummings SR, Rubin SM, Black D. The future of hip fractures in the United States. Numbers, costs, and potential effects of postmenopausal estrogen. Clin Orthop Relat Res. 1990;163-166. [PubMed] |
| 13. | Dy CJ, McCollister KE, Lubarsky DA, Lane JM. An economic evaluation of a systems-based strategy to expedite surgical treatment of hip fractures. J Bone Joint Surg Am. 2011;93:1326-1334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 79] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 14. | Downey C, Kelly M, Quinlan JF. Changing trends in the mortality rate at 1-year post hip fracture - a systematic review. World J Orthop. 2019;10:166-175. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 159] [Cited by in RCA: 292] [Article Influence: 41.7] [Reference Citation Analysis (10)] |
| 15. | Pioli G, Bendini C, Pignedoli P, Giusti A, Marsh D. Orthogeriatric co-management - managing frailty as well as fragility. Injury. 2018;49:1398-1402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 58] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 16. | Mak J, Wong E, Cameron I; Australian and New Zealand Society for Geriatric Medicine. Australian and New Zealand Society for Geriatric Medicine. Position statement--orthogeriatric care. Australas J Ageing. 2011;30:162-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | National Clinical Guideline Centre (UK). The Management of Hip Fracture in Adults [Internet]. London: Royal College of Physicians (UK); 2011. [PubMed] |
| 18. | Pogliacomi F, Schiavi P, Calderazzi F, Leigheb M, Domenichini M, Pedrazzini A, Ceccarelli F, Vaienti E. Is there a relation between clinical scores and serum ion levels after MoM-THA? Acta Biomed. 2020;91:e2020014. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 19. | Pellegrini A, Tacci F, Leigheb M, Costantino C, Pedrazzini A, Pedrazzi G, Vaienti E, Ceccarelli F, Pogliacomi F. Injuries of the trochanteric region: can analysis of radiographic indices help in prediction of recurrent osteoporotic hip fractures? Acta Biomed. 2017;88:43-49. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 20. | Xie J, Feng X, Ma J, Kang P, Shen B, Yang J, Zhou Z, Pei F. Is postoperative cell salvage necessary in total hip or knee replacement? Int J Surg. 2015;21:135-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 21. | Simunovic N, Devereaux PJ, Sprague S, Guyatt GH, Schemitsch E, Debeer J, Bhandari M. Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ. 2010;182:1609-1616. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 711] [Cited by in RCA: 689] [Article Influence: 43.1] [Reference Citation Analysis (0)] |
| 22. | Grimes JP, Gregory PM, Noveck H, Butler MS, Carson JL. The effects of time-to-surgery on mortality and morbidity in patients following hip fracture. Am J Med. 2002;112:702-709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 244] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 23. | Vidán MT, Sánchez E, Gracia Y, Marañón E, Vaquero J, Serra JA. Causes and effects of surgical delay in patients with hip fracture: a cohort study. Ann Intern Med. 2011;155:226-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 180] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 24. | Orosz GM, Magaziner J, Hannan EL, Morrison RS, Koval K, Gilbert M, McLaughlin M, Halm EA, Wang JJ, Litke A, Silberzweig SB, Siu AL. Association of timing of surgery for hip fracture and patient outcomes. JAMA. 2004;291:1738-1743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 418] [Cited by in RCA: 443] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 25. | HIP ATTACK Investigators. Accelerated surgery versus standard care in hip fracture (HIP ATTACK): an international, randomised, controlled trial. Lancet. 2020;395:698-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 241] [Article Influence: 40.2] [Reference Citation Analysis (0)] |
| 26. | Handoll HH, Parker MJ. Conservative versus operative treatment for hip fractures in adults. Cochrane Database Syst Rev. 2008;CD000337. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 74] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 27. | van de Ree CLP, De Jongh MAC, Peeters CMM, de Munter L, Roukema JA, Gosens T. Hip Fractures in Elderly People: Surgery or No Surgery? Geriatr Orthop Surg Rehabil. 2017;8:173-180. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 69] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 28. | Bachmann S, Finger C, Huss A, Egger M, Stuck AE, Clough-Gorr KM. Inpatient rehabilitation specifically designed for geriatric patients: systematic review and meta-analysis of randomised controlled trials. BMJ. 2010;340:c1718. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 389] [Cited by in RCA: 346] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 29. | Grigoryan KV, Javedan H, Rudolph JL. Orthogeriatric care models and outcomes in hip fracture patients: a systematic review and meta-analysis. J Orthop Trauma. 2014;28:e49-55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 498] [Cited by in RCA: 449] [Article Influence: 37.4] [Reference Citation Analysis (0)] |
| 30. | Kim YS, Lee HM, Kim JP, Bae EW, Oh CW, Kim JW. Proximal femoral insufficiency fracture after interlocking intramedullary nailing for atypical femoral fracture. Minerva Ortop Traumatol. 2020;71:78-85. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 31. | Lin SN, Su SF, Yeh WT. Meta-analysis: Effectiveness of Comprehensive Geriatric Care for Elderly Following Hip Fracture Surgery. West J Nurs Res. 2020;42:293-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 32. | National Institute for Health and Care Excellence. Hip Fracture: Management. London: National Institute for Health and Care Excellence, 2017. |
| 33. | Martocchia A, Curto M, Comite F, Scaccianoce S, Girardi P, Ferracuti S, Nicoletti F, Falaschi P; Orthogeriatric Group. The Prevention and Treatment of Delirium in Elderly Patients Following Hip Fracture Surgery. Recent Pat CNS Drug Discov. 2015;10:55-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 34. | Dolan MM, Hawkes WG, Zimmerman SI, Morrison RS, Gruber-Baldini AL, Hebel JR, Magaziner J. Delirium on hospital admission in aged hip fracture patients: prediction of mortality and 2-year functional outcomes. J Gerontol A Biol Sci Med Sci. 2000;55:M527-M534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 157] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 35. | Magaziner J, Simonsick EM, Kashner TM, Hebel JR, Kenzora JE. Predictors of functional recovery one year following hospital discharge for hip fracture: a prospective study. J Gerontol. 1990;45:M101-M107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 563] [Cited by in RCA: 546] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 36. | Marcantonio ER, Flacker JM, Michaels M, Resnick NM. Delirium is independently associated with poor functional recovery after hip fracture. J Am Geriatr Soc. 2000;48:618-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 479] [Cited by in RCA: 476] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 37. | Lipowski ZJ. Delirium in the elderly patient. N Engl J Med. 1989;320:578-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 353] [Cited by in RCA: 294] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 38. | Hsu JR, Mir H, Wally MK, Seymour RB; Orthopaedic Trauma Association Musculoskeletal Pain Task Force. Clinical Practice Guidelines for Pain Management in Acute Musculoskeletal Injury. J Orthop Trauma. 2019;33:e158-e182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 99] [Cited by in RCA: 192] [Article Influence: 27.4] [Reference Citation Analysis (0)] |
| 39. | Titler MG, Herr K, Schilling ML, Marsh JL, Xie XJ, Ardery G, Clarke WR, Everett LQ. Acute pain treatment for older adults hospitalized with hip fracture: current nursing practices and perceived barriers. Appl Nurs Res. 2003;16:211-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 57] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 40. | Haslam L, Lansdown A, Lee J, van der Vyver M. Survey of Current Practices: Peripheral Nerve Block Utilization by ED Physicians for Treatment of Pain in the Hip Fracture Patient Population. Can Geriatr J. 2013;16:16-21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 41. | Gottlieb M, Long B. Peripheral nerve block for hip fracture. Acad Emerg Med. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 42. | Guay J, Kopp S. Peripheral nerve blocks for hip fractures in adults. Cochrane Database Syst Rev. 2020;11:CD001159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 64] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 43. | Iolascon G, de Sire A, Curci C, Paoletta M, Liguori S, Calafiore D, Gimigliano F, Moretti A. Osteoporosis guidelines from a rehabilitation perspective: systematic analysis and quality appraisal using AGREE II. Eur J Phys Rehabil Med. 2021;57:273-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 44. | Tugni C, Sansoni J, Vanacore N, Valente D, Galeoto G. Rehabilitation effects in patients with total hip replacement: a systematic review and meta-analysis. Minerva Ortop Traumatol. 2019;70:205-218. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 45. | Oldmeadow LB, Edwards ER, Kimmel LA, Kipen E, Robertson VJ, Bailey MJ. No rest for the wounded: early ambulation after hip surgery accelerates recovery. ANZ J Surg. 2006;76:607-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 193] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 46. | Overgaard J, Kristensen MT. Feasibility of progressive strength training shortly after hip fracture surgery. World J Orthop. 2013;4:248-258. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 28] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 47. | Invernizzi M, de Sire A, D'Andrea F, Carrera D, Renò F, Migliaccio S, Iolascon G, Cisari C. Effects of essential amino acid supplementation and rehabilitation on functioning in hip fracture patients: a pilot randomized controlled trial. Aging Clin Exp Res. 2019;31:1517-1524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 52] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 48. | Iolascon G, de Sire A, Calafiore D, Benedetti MG, Cisari C, Letizia Mauro G, Migliaccio S, Nuti R, Resmini G, Gonnelli S, Moretti A. Multifactorial Assessment of Risk of Falling in 753 Post-Menopausal Women: A Multicenter Cross-Sectional Study by the Italian Group for the Study of Metabolic Bone Diseases. Clin Interv Aging. 2020;15:1077-1084. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 49. | Nahm ES, Resnick B, Orwig D, Magaziner J, Degrezia M. Exploration of informal caregiving following hip fracture. Geriatr Nurs. 2010;31:254-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 60] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 50. | Louie SWS, Poon MY, Yu SY, Chan WL, Au KM, Wong KM. Effectiveness of a patient/carer in an empowerment programme for people with hip fractures. IJTR. 2012;19:673-681. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 51. | Di Castro D, Passarani R, Romanini E, Magaletti M, Berardi A, Servadio A, Mollica R, Tofani M, Valente D, Galeoto G. Validity and reliability of the psychometric properties of the 12-item Berg Balance Scale (BBS-12) in the Italian population with hip or knee prosthesis: a cross sectional study. Minerva Ortop Traumatol. 2020;71:104-110. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 52. | Lin PC, Lu CM. Psychosocial factors affecting hip fracture elder's burden of care in Taiwan. Orthop Nurs. 2007;26:155-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 53. | Siddiqui MQ, Sim L, Koh J, Fook-Chong S, Tan C, Howe TS. Stress levels amongst caregivers of patients with osteoporotic hip fractures - a prospective cohort study. Ann Acad Med Singap. 2010;39:38-42. [PubMed] |
| 54. | Biver E, Pepe J, de Sire A, Chevalley T, Ferrari S. Associations between radius low-frequency axial ultrasound velocity and bone fragility in elderly men and women. Osteoporos Int. 2019;30:411-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 55. | Diez-Perez A, Brandi ML, Al-Daghri N, Branco JC, Bruyère O, Cavalli L, Cooper C, Cortet B, Dawson-Hughes B, Dimai HP, Gonnelli S, Hadji P, Halbout P, Kaufman JM, Kurth A, Locquet M, Maggi S, Matijevic R, Reginster JY, Rizzoli R, Thierry T. Radiofrequency echographic multi-spectrometry for the in-vivo assessment of bone strength: state of the art-outcomes of an expert consensus meeting organized by the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO). Aging Clin Exp Res. 2019;31:1375-1389. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 70] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 56. | Iolascon G, Moretti A, Toro G, Gimigliano F, Liguori S, Paoletta M. Pharmacological Therapy of Osteoporosis: What's New? Clin Interv Aging. 2020;15:485-491. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 64] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 57. | Lewiecki EM. Bisphosphonates for the treatment of osteoporosis: insights for clinicians. Ther Adv Chronic Dis. 2010;1:115-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 79] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 58. | Moretti A, de Sire A, Curci C, Toro G, Gimigliano F, Iolascon G. Effectiveness of denosumab on back pain-related disability and quality-of-life in patients with vertebral fragility fractures. Curr Med Res Opin. 2019;35:151-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 59. | Deeks ED. Denosumab: A Review in Postmenopausal Osteoporosis. Drugs Aging. 2018;35:163-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 136] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 60. | Tarantino U, Iolascon G, Cianferotti L, Masi L, Marcucci G, Giusti F, Marini F, Parri S, Feola M, Rao C, Piccirilli E, Zanetti EB, Cittadini N, Alvaro R, Moretti A, Calafiore D, Toro G, Gimigliano F, Resmini G, Brandi ML. Clinical guidelines for the prevention and treatment of osteoporosis: summary statements and recommendations from the Italian Society for Orthopaedics and Traumatology. J Orthop Traumatol. 2017;18:3-36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 132] [Cited by in RCA: 136] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 61. | Benedetti MG, Furlini G, Zati A, Letizia Mauro G. The Effectiveness of Physical Exercise on Bone Density in Osteoporotic Patients. Biomed Res Int. 2018;2018:4840531. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 210] [Cited by in RCA: 254] [Article Influence: 31.8] [Reference Citation Analysis (0)] |
| 62. | IOF. International Osteoporosis Foundation (IOF) Exercise recommendations. [cited 15 July 2021]. Available from: https://www.iofbonehealth.org/exercise-recommendations. |
| 63. | Hong AR, Kim SW. Effects of Resistance Exercise on Bone Health. Endocrinol Metab (Seoul). 2018;33:435-444. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 132] [Cited by in RCA: 159] [Article Influence: 19.9] [Reference Citation Analysis (15)] |
| 64. | Oral A, Küçükdeveci AA, Varela E, Ilieva EM, Valero R, Berteanu M, Christodoulou N. Osteoporosis. The role of physical and rehabilitation medicine physicians. The European perspective based on the best evidence. A paper by the UEMS-PRM Section Professional Practice Committee. Eur J Phys Rehabil Med. 2013;49:565-577. [PubMed] |
| 65. | Zhang X, Huang P, Dou Q, Wang C, Zhang W, Yang Y, Wang J, Xie X, Zhou J, Zeng Y. Falls among older adults with sarcopenia dwelling in nursing home or community: A meta-analysis. Clin Nutr. 2020;39:33-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 141] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 66. | White TA, LeBrasseur NK. Myostatin and sarcopenia: opportunities and challenges - a mini-review. Gerontology. 2014;60:289-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 143] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 67. | Pioli G, Barone A, Giusti A, Oliveri M, Pizzonia M, Razzano M, Palummeri E. Predictors of mortality after hip fracture: results from 1-year follow-up. Aging Clin Exp Res. 2006;18:381-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 100] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 68. | Fiatarone Singh MA. Exercise, nutrition and managing hip fracture in older persons. Curr Opin Clin Nutr Metab Care. 2014;17:12-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 69. | Avenell A, Handoll HH. Nutritional supplementation for hip fracture aftercare in older people. Cochrane Database Syst Rev. 2005;CD001880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 70. | Anbar R, Beloosesky Y, Cohen J, Madar Z, Weiss A, Theilla M, Koren Hakim T, Frishman S, Singer P. Tight calorie control in geriatric patients following hip fracture decreases complications: a randomized, controlled study. Clin Nutr. 2014;33:23-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 69] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 71. | Delmi M, Rapin CH, Bengoa JM, Delmas PD, Vasey H, Bonjour JP. Dietary supplementation in elderly patients with fractured neck of the femur. Lancet. 1990;335:1013-1016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 608] [Cited by in RCA: 521] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 72. | Fiatarone MA, O'Neill EF, Ryan ND, Clements KM, Solares GR, Nelson ME, Roberts SB, Kehayias JJ, Lipsitz LA, Evans WJ. Exercise training and nutritional supplementation for physical frailty in very elderly people. N Engl J Med. 1994;330:1769-1775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1938] [Cited by in RCA: 1740] [Article Influence: 54.4] [Reference Citation Analysis (0)] |
| 73. | Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet. 2019;393:2636-2646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1036] [Cited by in RCA: 2682] [Article Influence: 383.1] [Reference Citation Analysis (0)] |
| 74. | Kramer IF, Blokhuis TJ, Verdijk LB, van Loon LJC, Poeze M. Perioperative nutritional supplementation and skeletal muscle mass in older hip-fracture patients. Nutr Rev. 2019;77:254-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 75. | Malafarina V, Uriz-Otano F, Malafarina C, Martinez JA, Zulet MA. Effectiveness of nutritional supplementation on sarcopenia and recovery in hip fracture patients. A multi-centre randomized trial. Maturitas. 2017;101:42-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 91] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 76. | Roberts KC, Brox WT. AAOS Clinical Practice Guideline: Management of Hip Fractures in the Elderly. J Am Acad Orthop Surg. 2015;23:138-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 113] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 77. | Artaza-Artabe I, Sáez-López P, Sánchez-Hernández N, Fernández-Gutierrez N, Malafarina V. The relationship between nutrition and frailty: Effects of protein intake, nutritional supplementation, vitamin D and exercise on muscle metabolism in the elderly. A systematic review. Maturitas. 2016;93:89-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 192] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 78. | de Sire A, Baricich A, Renò F, Cisari C, Fusco N, Invernizzi M. Myostatin as a potential biomarker to monitor sarcopenia in hip fracture patients undergoing a multidisciplinary rehabilitation and nutritional treatment: a preliminary study. Aging Clin Exp Res. 2020;32:959-962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 42] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 79. | Kose E, Wakabayashi H. Rehabilitation pharmacotherapy: A scoping review. Geriatr Gerontol Int. 2020;20:655-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 80. | Young J. The development of intermediate care services in England. Arch Gerontol Geriatr. 2009;49:S21-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 81. | Lenzi J, Mongardi M, Rucci P, Di Ruscio E, Vizioli M, Randazzo C, Toschi E, Carradori T, Fantini MP. Sociodemographic, clinical and organisational factors associated with delayed hospital discharges: a cross-sectional study. BMC Health Serv Res. 2014;14:128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 82. | Lieberman D, Friger M, Lieberman D. Inpatient rehabilitation outcome after hip fracture surgery in elderly patients: a prospective cohort study of 946 patients. Arch Phys Med Rehabil. 2006;87:167-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 65] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 83. | McGilton KS, Davis A, Mahomed N, Flannery J, Jaglal S, Cott C, Naglie G, Rochon E. An inpatient rehabilitation model of care targeting patients with cognitive impairment. BMC Geriatr. 2012;12:21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 84. | Seitz DP, Adunuri N, Gill SS, Rochon PA. Prevalence of dementia and cognitive impairment among older adults with hip fractures. J Am Med Dir Assoc. 2011;12:556-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 176] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 85. | Adunsky A, Lusky A, Arad M, Heruti RJ. A comparative study of rehabilitation outcomes of elderly hip fracture patients: the advantage of a comprehensive orthogeriatric approach. J Gerontol A Biol Sci Med Sci. 2003;58:542-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 75] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 86. | Seitz DP, Gill SS, Gruneir A, Austin PC, Anderson GM, Bell CM, Rochon PA. Effects of dementia on postoperative outcomes of older adults with hip fractures: a population-based study. J Am Med Dir Assoc. 2014;15:334-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 97] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 87. | Strömberg L, Ohlén G, Nordin C, Lindgren U, Svensson O. Postoperative mental impairment in hip fracture patients. A randomized study of reorientation measures in 223 patients. Acta Orthop Scand. 1999;70:250-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 88. | Hall AJ, Lang IA, Endacott R, Hall A, Goodwin VA. Physiotherapy interventions for people with dementia and a hip fracture-a scoping review of the literature. Physiotherapy. 2017;103:361-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 89. | Smith TO, Gilbert AW, Sreekanta A, Sahota O, Griffin XL, Cross JL, Fox C, Lamb SE. Enhanced rehabilitation and care models for adults with dementia following hip fracture surgery. Cochrane Database Syst Rev. 2020;2:CD010569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 90. | Downey CL, Young A, Burton EF, Graham SM, Macfarlane RJ, Tsapakis EM, Tsiridis E. Dementia and osteoporosis in a geriatric population: Is there a common link? World J Orthop. 2017;8:412-423. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 30] [Cited by in RCA: 36] [Article Influence: 4.0] [Reference Citation Analysis (1)] |
| 91. | Mughal N, Inderjeeth AJ, Inderjeeth CA. Osteoporosis in patients with dementia is associated with high morbidity and mortality: Findings from a single orthogeriatric unit. Aust J Gen Pract. 2019;48:53-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 92. | Yun H, Curtis JR, Guo L, Kilgore M, Muntner P, Saag K, Matthews R, Morrisey M, Wright NC, Becker DJ, Delzell E. Patterns and predictors of osteoporosis medication discontinuation and switching among Medicare beneficiaries. BMC Musculoskelet Disord. 2014;15:112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 93. | Inderjeeth CA, Chan K, Kwan K, Lai M. Time to onset of efficacy in fracture reduction with current anti-osteoporosis treatments. J Bone Miner Metab. 2012;30:493-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Iida H, Liu J S-Editor: Zhang H L-Editor: Filipodia P-Editor: Xing YX