Published online Oct 18, 2021. doi: 10.5312/wjo.v12.i10.791
Peer-review started: April 4, 2021
First decision: June 7, 2021
Revised: July 21, 2021
Accepted: August 4, 2021
Article in press: August 4, 2021
Published online: October 18, 2021
Processing time: 193 Days and 1.9 Hours
There appears to be a close relationship between deformities at the knee joint and at the hindfoot in patients with knee osteoarthritis (OA). Despite this intrinsic link, there is a dearth of studies investigating alterations in hindfoot alignment following total knee arthroplasty (TKA) in patients with knee OA.
To evaluate changes in alignment of the hindfoot following TKA, foot and ankle clinical outcomes in terms of subjective clinical scoring tools following surgical intervention, and to analyse the level of evidence (LOE) and quality of evidence (QOE) of the included studies.
MEDLINE, EMBASE and Cochrane Library databases were systematically reviewed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Studies reporting changes in the postoperative alignment of the hindfoot following TKA were included. The level and QOE were recorded and assessed.
Eleven studies with a total of 1142 patients (1358 knees) met the inclusion/ exclusion criteria. Six studies were of LOE II and 5 studies were of LOE III. Patients with preoperative varus knee deformity and valgus hindfoot deformity demonstrated improvement in hindfoot alignment post TKA. Patients with preoperative varus knee deformity and varus hindfoot deformity demonstrated no improvement in hindfoot alignment following TKA. Twelve different radiographic parameters were used to measure the alignment of the hindfoot across the included studies, with the tibio-calcaneal angle most frequently utilised (27.3%).
This systematic review demonstrated that the hindfoot may display compen
Core Tip: This current systematic review has found that correction of deformities at the knee joint following total knee arthroplasty typically resulted in improved changes in the alignment of the hindfoot. However, the poor quality of evidence together with the marked heterogeneity between the included studies, underscores the need for further higher quality studies.
- Citation: Butler JJ, Mercer NP, Hurley ET, Azam MT, Kennedy JG. Alignment of the hindfoot following total knee arthroplasty: A systematic review. World J Orthop 2021; 12(10): 791-801
- URL: https://www.wjgnet.com/2218-5836/full/v12/i10/791.htm
- DOI: https://dx.doi.org/10.5312/wjo.v12.i10.791
Osteoarthritis (OA) of the knee is one of the leading causes of pain in the older population, affecting 30% of adults over the age of 60 years old[1]. Although the etiology and pathogenesis of knee OA remains unclear, knee malalignment is a significant risk factor for knee OA. Even minor changes in knee alignment can lead to abnormal load distribution across the articular surface of the knee joint, leading to degeneration of the joint capsule and further progression of OA[2,3]. Replacement procedures, such as total knee arthroplasty (TKA), aim to restore neutral mechanical alignment of the lower extremity.
The alignment of the lower extremity is frequently evaluated by extrapolating the femoral-tibial angle (FTA) and the mechanical axis from standing, full-length, plain radiographs[4,5]. However, the FTA and mechanical axis provide an incomplete picture of the alignment of the lower limb as they exclude assessment of the hindfoot axis. There are a variety of reports demonstrating a relationship between varus or valgus deformities at the knee joint and hindfoot malalignment in patients with knee OA[6-16]. In fact, hindfoot malalignment has been shown to improve following TKA in patients with knee OA[6-10,12-16]. This suggests that knee OA leads to compensatory changes in the hindfoot or, hindfoot deformities may predispose the knee to osteoarthritic change. As a result, pre and post-operative radiological imaging of the hindfoot, via Cobey views or otherwise, is crucial in the management of knee OA[17].
Despite the intrinsic link between deformities at the knee joint and the hindfoot in knee OA, there appears to be scant literature extensively investigating the relationship between these 2 pathologies. There also seems to be no consensus regarding the optimal imaging method for hindfoot alignment. The purpose of this systematic review was to evaluate changes in hindfoot alignment and foot and ankle clinical outcomes in terms of subjective clinical scoring tools following TKA.
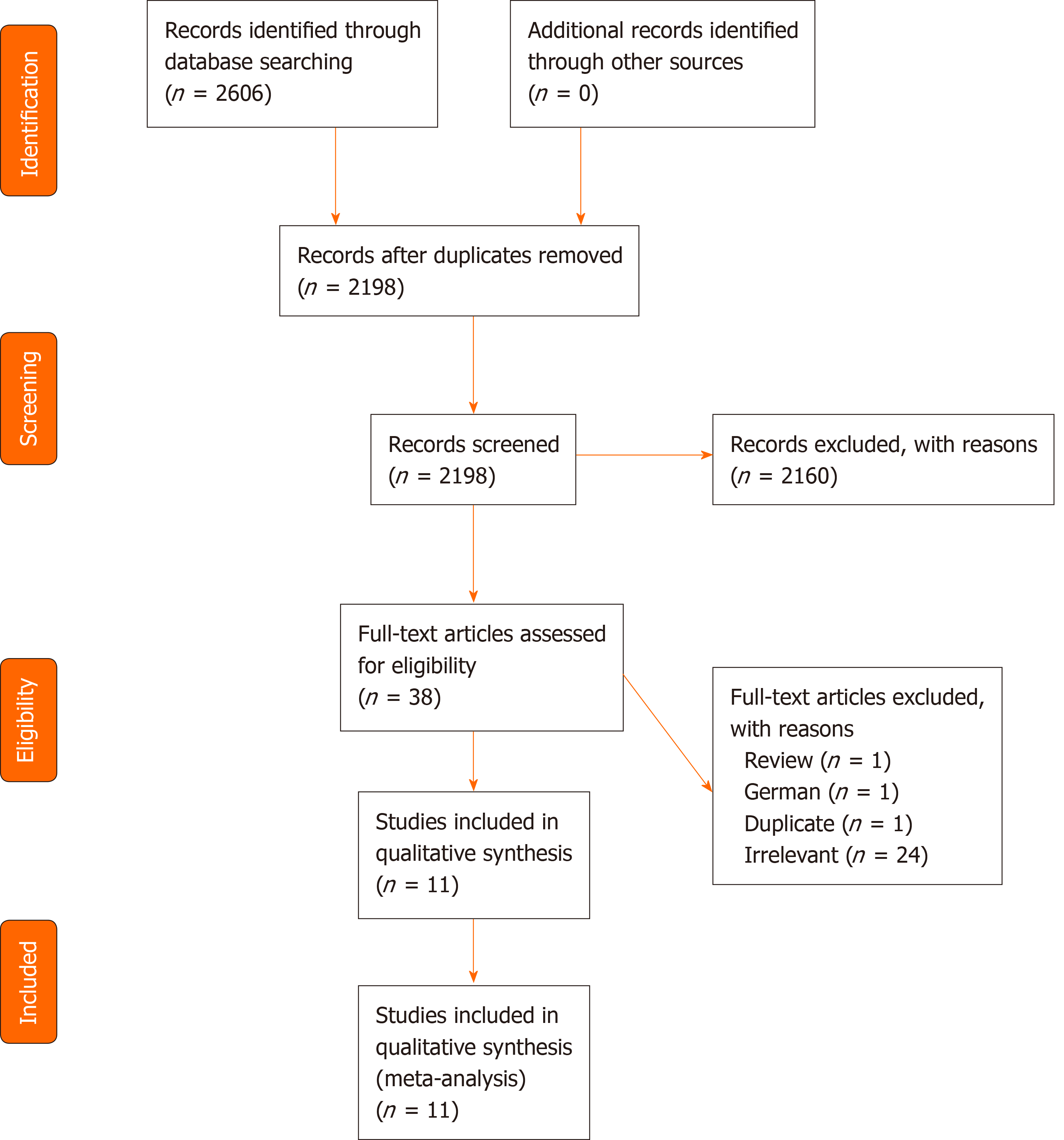
During October 2019, a systematic review of the MEDLINE, EMBASE and Cochrane Library databases was performed based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (Figure 1) guidelines. The following search terms were used: [(Hindfoot OR foot OR ankle) AND (alignment OR malalignment OR misalignment OR position OR kinematics OR axis OR anatomy) AND (knee replacement OR TKR OR knee arthroplasty OR TKA)]. The inclusion and exclusion criteria are shown in Table 1. Following retrieval of the data, the titles, abstracts and full text articles were screened by two independent reviewers of all searched studies by applying the aforementioned criteria. A senior author was consulted to arbitrate any disagreements that arose.
| Inclusion criteria | Exclusion criteria |
| Clinical studies related to changes in the hindfoot following TKA | Less than 10 patients |
| Published in a peer review journal | Case reports |
| Written in English | Cadaveric studies |
| Full text version available | Animal studies |
| Review articles | |
| In vivo studies |
The level of evidence (LOE) was assessed using the criteria published by the Journal of Bone & Joint Surgery. The methodological quality of evidence (QOE) was assessed using the Modified Coleman Methodology Score (MCMS)[18]. Two independent reviewers determined the MCMS for each study. If any discrepancy existed, the senior author evaluated the available data and a consensus was reached. Excellent studies had a score between 85 to 100 points, good studies scored between 70 to 84 points, fair studies had a score between 55 to 69 points and poor studies scored less than 55 points.
Two independent reviewers independently extracted and assessed the data from each study. Patient demographic data and postoperative follow up times were gathered. Radiographic parameters used to evaluate the alignment of the hindfoot, lower extremity and ankle joint were also collected. Data on postoperative clinical outcomes in terms of subjective clinical scoring tools were evaluated.
All other statistical analyses were performed using SAS software version 9.3 (SAS Institute, Inc., Cary, NC, United States). Descriptive statistics were calculated for all continuous and categorical variables. Continuous variables were reported as weighted mean and estimated standard deviation, whereas categorical variables were reported as frequencies with percentages. A value of P < 0.05 was considered statistically significant.
The search generated 2606 studies. Of these, 11 met the inclusion and exclusion criteria of this systematic review (Table 1). The studies were published between 2004 and 2019.
From the 11 studies, 1142 patients (1358 knees) with a weighted mean age of 69.1 ± 3.6 years (range, 63.4-74.7), had radiographic imaging of the hindfoot following TKA. The weighted mean postoperative follow-up time was 10.9 ± 9.4 mo (range, 0.75–31.3) (Table 2).
| Ref. | LOE | Patients, n (%) | Knees, n (%) | Age (yr) | Sex (M/F) | Follow-up (mo) | MCMS |
| Chandler and Moskal[6], 2004 | 2 | 86 | 86 | N/R | N/R | 3 | 48 |
| Cho et al[7], 2017 | 2 | 117 | 195 | 69.1 | 8/187 | 24 | 66 |
| Hara et al[8], 2015 | 3 | 100 | 100 | 74.3 | 14/86 | 0.75 | 48 |
| Jeong et al[9], 2018 | 2 | 331 | 375 | 68.3 | 23/308 | 6 | 60 |
| Kim et al[10], 2018 | 3 | 55 | 65 | 69.3 | N/R | 31.3 | 71 |
| Levinger et al[11], 2012 | 2 | 19 | 26 | 67.5 | 13/6 | 12 | 46 |
| Mansur et al[12], 2019 | 2 | 72 | 72 | N/R | 23/49 | 3 | 44 |
| Mullaji and Shetty[13], 2011 | 2 | 125 | 165 | 66.1 | 24/101 | 12 | 51 |
| Okamoto et al[14], 2017 | 3 | 75 | 80 | 72.5 | 8/67 | 24 | 48 |
| Palanisami et al[15], 2020 | 3 | 91 | 121 | 63.4 | 29/62 | 12 | 58 |
| Takenaka et al[16], 2016 | 3 | 71 | 73 | 74.7 | 17/56 | 12 | 48 |
Six studies were LOE II and 5 studies were LOE III. The mean MCMS of all included studies was 53.5 ± 8.5 of 100 points. No studies were classified as excellent quality using the MCMS. There was 1 study of good quality, 3 studies of fair quality and 7 studies of poor quality. 8 studies had a large patient cohort (n > 60).
The radiologic assessment data are listed in Table 3. Twelve different radiographic parameters were used to evaluate the alignment of the hindfoot. The most commonly utilised radiographic tool was the tibio-calcaneal angle (TCA) in 3 studies (27.3%)[6,7,13]. Other radiographic parameters utilised included the varus-valgus angle (VVA) in 2 studies (18.2%)[8,16], hindfoot alignment view angle (HAVA) in 1 study[10], calcaneal pitch and naviculocuboid overlap in 1 study (9.1%)[14], tibia-hindfoot angle and varus-valgus index (VVI) in 1 study (9.1%)[15], foot posture index in 1 study (9.1%)[11], the hindfoot alignment angle (HA), hindfoot alignment ratio (HR) and hindfoot alignment distance (HD) in 1 study (9.1%)[9], and the intersection of the load axis of the leg and the calcaneus axis in 1 study (9.1%)[12].
| Radiographic Assessment | AOFAS | ||||||||
| Ref. | Patients, n (%) | Knees, n (%) | Knee deformity | Hindfoot | Ankle | Lower limb alignment | Pre-op | Post-op | Postoperative outcomes |
| Chandler and Moskal[6], 2004 | 86 | 86 | Both valgus and varus | TCA: Pre-op = 0.4°; Post-op = -0.1° | FTA: Pre-op = 3.6°; Post-op = 6.6° | Both valgus and varus hindfoot alignment improved post TKA | |||
| Valgus hindfoot alignment remained in valgus alignment post TKA | |||||||||
| Varus hindfoot alignment remained in varus alignment post TKA | |||||||||
| Cho et al[7], 2017 | 117 | 195 | Varus only | TCA: Pre-op = 5.2° valgus; Post-op = 2.1° valgus | Mechanical alignment angle: Pre-op = 10.8° varus; Post-op = 1.8° varus | Valgus hindfoot alignment improved post TKA | |||
| Severe varus knee deformities had best improvement in hindfoot alignment post TKA | |||||||||
| Hara et al[8], 2015 | 100 | 100 | Varus only | VVA: Pre-op = 78.8°; Post-op = 76.7° | FTA: Pre-op = 186.7°; Post-op = 174.4° | Varus hindfoot alignment with varus knee deformity remained in varus alignment post TKA | |||
| Valgus hindfoot alignment with varus knee deformity improved post TKA | |||||||||
| Jeong et al[9], 2018 | 331 | 375 | Varus only | HA: Pre-op = 13.5°; Post-op = 5.8°. HR: Pre-op = 0.2°; Post-op = 0.3°. HD: Pre-op = 11.0°; Post-op = 5.2° | TT: Pre-op = 0.4°; Post-op = 0.1°. GD: Pre-op = 6.5°; Post-op = 0.2°. TAS: Pre-op = 92.0°; Post-op = 92.0°. TLS: Pre-op = 81.8°; Post-op = 81.3° | Mechanical axis: Pre-op = 11.1° varus; Post-op = 0.3° varus | Valgus hindfoot alignment improved post TKA | ||
| Subtalar joint became more varus post TKA | |||||||||
| Kim et al[10], 2018 | 55 | 65 | Varus only | HAVA: Pre-op = 6.1°; Post-op = 5.7° | TT: Pre-op = 1.9°; Post-op = 1.7°. TAS: Pre-op = 85.9°; Post-op = 84.9°. MCS: Pre-op = 2.4 mm; Post-op = 2.6 mm. MTTJS: Pre-op = 2.8°; Post-op = 2.3°. FTGA: Pre-op = 85.6°; Post-op = 86.5° | Mechanical axis deviation angle: Pre-op = 10.0°; Post-op = 1.9° | 95.2 | 91.5 | Valgus hindfoot alignment slightly improved post TKA |
| Newly developed ankle pain post TKA was associated with larger degrees of residual varus knee deformity | |||||||||
| Levinger et al[11], 2012 | 19 | 26 | Varus only | FPI: Pre-op = 2.9°; Post-op = 2.7° | FTA: Pre-op = -1.2°; Post-op = 4.9° | Increased range of motion of the rearfoot in the frontal plane post TKA | |||
| No change in static foot pressure post TKA | |||||||||
| Mansur et al[12], 2019 | 72 | 72 | Both varus and valgus | Intersection of the load axis of the leg and the calcaneus axis: Pre-op = -3.8°; Post-op = -4.4° | FTA: Pre-op = ? | 74.3 | 89.4 | Varus hindfoot alignment with varus knee deformity remained in varus alignment post TKA | |
| Varus hindfoot alignment with valgus knee deformity, valgus hindfoot alignment with valgus knee deformity and valgus hindfoot alignment with varus knee deformity all improved post TKA | |||||||||
| Mullaji and Shetty[13], 2011 | 125 | 165 | Both varus and valgus | TCA: Pre-op = 188°; Post-op = 185.5° | CMAD: Pre-op = 34.3 mm; Post-op = 0.0 mm. GMAD: Pre-op = 31.0 mm; Post-op = -6.0 mm | Valgus hindfoot alignment with varus knee deformity improved post TKA | |||
| 87% of patients had persistent valgus hindfoot alignment post TKA | |||||||||
| Okamoto et al[14], 2017 | 75 | 80 | Varus only | Calcaneal pitch: Pre-op = 14.9°. Naviculocuboid overlap: Pre-op = 84.7°; Post-op = 65.7° | TT: Pre-op = 13.1°; Post-op = 4.4°. TI: Pre-op = 9.9°; Post-op = 0.8° | Mechanical axis: Pre-op = 5.0°; Post-op = 0.7° | 46.6 | 60.2 | Valgus hindfoot alignment with severe varus knee deformity did not improve post TKA |
| Valgus hindfoot alignment with moderate varus knee deformity improved post TKA | |||||||||
| Palanisami et al[15], 2020 | 91 | 121 | Varus only | TH: Pre-op = 9.9°; Post-op = 4.7°. VVI: Pre-op = -0.29; Post-op = -0.04 | FTMA: Pre-op = 162.0°; Post-op = 178.8° | 59.2 | 88.7 | Valgus hindfoot alignment with varus knee deformity improved post TKA | |
| TKA restores foot loading pattern medially | |||||||||
| Takenaka et al[16], 2016 | 71 | 73 | Varus only | VVA: Preop = 78.2; Post-op = 76.0 | FTA: Pre-op = 184.8; Post-op = 173.9 | Valgus hindfoot alignment with varus knee deformity improved post TKA | |||
| Varus hindfoot alignment with varus knee deformity did not improve post TKA | |||||||||
Six radiographic parameters were used to measure the alignment of the lower extremity, the most common of which was the FTA in 4 studies (36.4%)[6,8,11,12]. Other radiographic tools used included mechanical axis in 2 studies (18.2%)[9,14], mechanical axis deviation angle in 1 study (9.1%)[10], mechanical alignment angle in 1 study (9.1%)[7], conventional mechanical axis deviation in 1 study (9.1%)[13], femorotibial mechanical angle in 1 study (9.1%)[15].
Only 3 studies (27.3%) recorded the alignment of the ankle joint, with the talar tilt (TT) utilised in 3 studies (27.3%)[9,10,14], the tibial anterior surface angle (TAS) used in 2 studies (18.2%)[9,10], the ground talar dome angle of foot (GD) and lateral surface angle of distal tibia used in 1 study each (9.1%)[9], the TAS, distal medial clear space (DMCS), and medial tibiotalar joint space (MTTJS) and frontal tibial ground angle (FTGA) were utilised in 1 study each (9.1%)[10].
Ten studies evaluated changes in hindfoot alignment following TKA for patients with varus deformity of the knee joint[7-16]. Nine of these studies demonstrated improvement of hindfoot valgus alignment following TKA[7-10,12-16]. Chandler and Moskal[6], Cho et al[7] and Mullaji and Shetty[13] showed a mean postoperative improvement in TCA of 3.1°, 3.1° and 2.0° respectively. Hara et al[8] and Takenaka et al[16] highlighted a mean postoperative improvement in VVA of 3.1° and 3.4° respectively. Jeong et al[9] demonstrated a mean postoperative improvement in HA, HR and HD of 7.7°, 0.1° and 5.8° respectively. Kim et al[10] illustrated a mean postoperative improvement in HAVA of 1.4°. Mansur et al[12] demonstrated a mean postoperative improvement of hindfoot alignment of 3.6. Okamoto et al[14] illustrated a mean postoperative improvement in naviculocuboid overlap of 19.0°. Palanisami et al[15] highlighted a mean postoperative improvement in VVI of 0.25.
Okamoto et al[14] noted that a cohort of patients with severe varus knee deformity did not show correction of hindfoot malalignment following TKA[14]. Conversely, Cho et al[7] showed that patients with severe varus knee deformity had the greatest overall improvement in hindfoot alignment. Patients with a severe varus knee deformity displayed a mean change in HA of 4.0° ± 3.0° in contrast to patients with a less severe varus knee deformity who displayed a mean change in HA of 1.8° ± 2.5°[7].
Three studies highlighted that patients with preoperative hindfoot varus malali
Two studies investigated alterations in hindfoot alignment following TKA in patients with valgus deformity at the knee joint[12,13]. Both studies recorded improvements in postoperative hindfoot varus alignment. Mansur et al[12] reported an increase in mean hindfoot alignment axis of 7.5, while Mullaji and Shetty[13] recorded a mean decrease in TCA of 1.5°. Also, Mullaji and Shetty[13] reported an improvement in postoperative hindfoot valgus alignment, as evident by a decrease in mean hindfoot alignment axis of 3.3.
Three studies reported changes in ankle joint alignment following TKA for knee OA[9,10,14]. There was a decrease in the TT postoperatively in 2 studies, indicating a varus shift in the TT[9,14], with no significant change reported in 1 study[14]. The GD shifted towards a valgus alignment in 1 study[9]. The TLS changed significantly in 1 study[9]. The TAS, DMCS, MTTJS and FTGA showed no statistically significant change following TKA.
Clinical outcomes were evaluated using the American Orthopaedic Foot and Ankle Society (AOFAS) score in 4 studies[10,12,14,15]. The weighted mean preoperative AOFAS score improved from 66.1 ± 18.1 to 82.0 ± 12.9 postoperatively at a mean of 17.6 mo of follow-up. One study reported that patients with newly developed ankle pain or who experienced an aggravation of existing pain after TKA had significantly larger degrees of residual varus knee than patients without ankle pain before and after TKA or those with ankle pain before surgery that did not change during the follow-up period[10]. One study demonstrated that patients with severe preoperative varus deformity at the knee had no statistically significant improvement in AOFAS score following TKA
This current systematic review has found that correction of deformities at the knee joint following TKA typically resulted in improved changes in the alignment of the hindfoot. However, the poor QOE together with the marked heterogeneity between the included studies, underscores the need for further higher quality studies.
All studies reported that preoperative varus or valgus knee deformity was associated with malalignment of the hindfoot. Typically varus knee OA was accompanied by a valgus hindfoot deformity. Furthermore, the findings of this current review highlights that patients who undergo TKA for a varus osteoarthritic knee with pre-existing valgus hindfoot deformity may display improvements in hindfoot alignment postoperatively. This suggests that these patients may have a residual capacity to compensate for the corrected lower limb malalignment. Interestingly, Cho et al[7] reported improvement in hindfoot alignment at 6 wk post TKA but little to no improvement at 2 years postoperatively, suggesting that compensatory changes in hindfoot alignment predominantly occur during the early postoperative period. This lack of improvement in hindfoot alignment at the 2 year follow up point may indicate that following the early postoperative period, there may be no further hindfoot alignment compensation as the knee joint alignment has now been corrected following TKA. However, Takenaka et al[16] recorded improvement in hindfoot alignment at 3 wk post TKA with further improvement noted 1 year post TKA. The discrepancy between these 2 studies highlights that further research is warranted to understand the complex lower limb biomechanical alterations that occur in sequential postoperative time points following TKA.
This current study demonstrated that patients with co-existing varus knee deformities and varus hindfoot malalignment showed no improvement in hindfoot alignment post TKA[8,12,16]. There are several reasons that could explain this resistance to change in varus hindfoot deformity. Firstly, varus feet cause nonparallel alignment of the midtarsal axes, which in turn leads to the foot displaying rigid stability so as to support the body’s weight[8]. This may reduce the ability of the preoperative varus hindfoot to change alignment following TKA of a varus osteoarthritic knee. Varus hindfoot is often associated with a rigid or non-correctible hindfoot alignment, either from increase calcaneal pitch or mechanical changes from neuromuscular changes that are not reversible. Charcot Marie Tooth is commonly associated with a varus hindfoot but this is typically not compensated for by knee realignment. In contrast, many valgus hindfoot alignments are correctible and flexible adapting to better alignment in the femoral tibia joint by re-establishing improved hindfoot alignment.
The ability to achieve a neutral alignment is essential if knee re-alignment is to have any measurable impact on hindfoot alignment. Tarsal coalition in valgus hindfeet and CMT and other neurological conditions associated with varus hindfeet will prevent re-establishing normal hindfoot alignment. In addition, advanced post-traumatic osteoarthritis (PTOA) of the ankle or subtalar joint will also prevent neutral alignment of the hindfoot[9]. The ability to change alignment of the hindfoot is critical in survivorship of the knee implant as persistent varus hindfoot deformity post TKA may lead to asymmetric wear, osteolysis and failure of the implant[19].
There were conflicting reports regarding the severity of knee joint deformity and postoperative outcomes. Okamoto et al[14] demonstrated that patients with severe varus knee deformity presented with postoperative hindfoot pain and valgus alignment[14]. This may in part be explained by the advanced stage of PTOA in the hindfoot and the advanced stage of knee varus malalignment from delayed operative intervention. Restriction in motion preventing restoration of neutral hindfoot alignment would be expected in the advanced stages of PTOA where peri articular osteophytes and soft tissue cicatrization would prevent choparts and ankle joint motion. In contrast, Cho et al[7] showed that patients who underwent surgical intervention for severe varus knee deformity had the best postoperative outcomes but his cohort was younger and had less advanced ankle arthritic change[7]. Further studies are required to determine the correlation between severity of knee deformity and post TKA outcomes, but it does seem that earlier intervention in knee OA is helpful in addressing knee pain but also has downstream effects on hindfoot biomechanical alignment and consequent health of the ankle joint.
This current systematic review has demonstrated that there is marked heterogeneity in the assessment of the alignment of the hindfoot. Twelve different radiographic parameters were utilised across the 11 studies, with the TCA being the most commonly utilised metric in 3 studies[6,7,13]. The lack of consensus regarding what radiographic parameter to utilise to evaluate the alignment of the hindfoot underpins the need for a standardised imaging protocol of the limb following knee arthroplasty. In addition, only 2 studies reported radiographic data at 2 or more sequential operative time points[7,16]. Assessing the alignment of the hindfoot at regular intervals postoperatively may be necessary to determine the time at which correction of hindfoot malalignment occurs and could possibly predict the time at which a surgical realignment of the hindfoot is required to protect the longevity of the knee implant (Table 4).
| Hindfoot radiographic parameters | Studies, n (%) |
| TCA | 3 (27.3) |
| VVA | 2 (18.2) |
| HAVA | 1 (9.1) |
| Intersection of the load axis of the leg and the calcaneus axis | 1 (9.1) |
| TH | 1 (9.1) |
| Calcaneal pitch | 1 (9.1) |
| Naviculocuboid overlap | 1 (9.1) |
| FPI | 1 (9.1) |
| HA | 1 (9.1) |
| HR | 1 (9.1) |
| HD | 1 (9.1) |
This current systematic review found that only 4 studies reported pre and postoperative clinical scoring systems, with the AOFAS score utilised in all 4 studies[10,12,14,15]. AOFAS scores tended to increase post TKA, suggesting that correction of lower limb malalignment resulted in improved functional and pain outcomes in the foot and ankle. Interestingly, 1 study demonstrated that patients presenting with new or aggravated pre-existing foot and ankle pain following TKA had a residual varus deformity at the knee joint[10]. Furthermore, Okamoto et al[14] reported that patients with severe varus deformity at the knee joint had no statistically significant improvement in AOFAS score, possibly due to loss of residual capacity for compensation in the hindfoot[14]. However, these outcomes should be assessed with caution due to a lack of a validated scoring tool for the foot and ankle following TKA.
This systematic review has several inherent limitations and/or potential biases. The criterion was limited to MEDLINE, EMBASE and Cochrane Library Database articles published exclusively in English. A further limitation was the marked heterogeneity between studies, in terms of both patient selection and pre and post-operative radiographic assessment. As a result, cross-sectional comparison amongst studies could not be analysed. Another limitation with this review is the poor QOE of the included studies. Lastly, the data was not extracted blindly, but was extracted by two independent reviewers and later confirmed by the lead author.
In conclusion, this systematic review demonstrated that the hindfoot typically displays compensatory changes in alignment following TKA in patients with knee osteoarthritis. However, the marked heterogeneity between the included studies and poor QOE limits any meaningful cross sectional comparisons between studies. Further, well designed studies, are necessary to determine the changes and outcomes of hindfoot alignment following TKA.
There are a variety of reports demonstrating a relationship between deformities at the knee joint and hindfoot malalignment in patients with knee osteoarthritis (OA).
The relationship between knee joint deformities and alterations in hindfoot alignment following total knee arthroplasty (TKA) has not been fully investigated to date.
To evaluate changes in alignment of the hindfoot following TKA and foot and ankle clinical outcomes in terms of subjective clinical scoring tools following surgical intervention.
MEDLINE, EMBASE and Cochrane Library databases were systematically reviewed. Studies reporting changes in the postoperative alignment of the hindfoot following TKA were included.
Eleven studies with a total of 1142 patients (1358 knees) were included. Patients with preoperative varus knee deformity and valgus hindfoot deformity demonstrated improvement in hindfoot alignment post TKA. Patients with preoperative varus knee deformity and varus hindfoot deformity demonstrated no improvement in hindfoot alignment following TKA. Twelve different radiographic parameters were used to measure the alignment of the hindfoot, with the tibio-calcaneal angle most frequently utilised (27.3%).
The hindfoot may display compensatory changes in alignment following TKA in patients with knee OA. However, the marked heterogeneity between the included studies and poor quality of evidence confounds the generation of robust conclusions from this review.
Further, higher quality studies are required to determine the changes and outcomes of hindfoot alignment following TKA.
| 1. | Felson DT, Naimark A, Anderson J, Kazis L, Castelli W, Meenan RF. The prevalence of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum. 1987;30:914-918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1034] [Cited by in RCA: 1063] [Article Influence: 27.3] [Reference Citation Analysis (0)] |
| 2. | Tanamas S, Hanna FS, Cicuttini FM, Wluka AE, Berry P, Urquhart DM. Does knee malalignment increase the risk of development and progression of knee osteoarthritis? Arthritis Rheum. 2009;61:459-467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 229] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 3. | Teichtahl A, Wluka A, Cicuttini FM. Abnormal biomechanics: a precursor or result of knee osteoarthritis? Br J Sports Med. 2003;37:289-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Abdel MP, Oussedik S, Parratte S, Lustig S, Haddad FS. Coronal alignment in total knee replacement: historical review, contemporary analysis, and future direction. Bone Joint J. 2014;96-B:857-862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 156] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 5. | Kamath J, Danda RS, Jayasheelan N, Singh R. An Innovative Method of Assessing the Mechanical Axis Deviation in the Lower Limb in Standing Position. J Clin Diagn Res. 2016;10:RC11-RC13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Chandler JT, Moskal JT. Evaluation of knee and hindfoot alignment before and after total knee arthroplasty: a prospective analysis. J Arthroplasty. 2004;19:211-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 75] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 7. | Cho WS, Cho HS, Byun SE. Changes in hindfoot alignment after total knee arthroplasty in knee osteoarthritic patients with varus deformity. Knee Surg Sports Traumatol Arthrosc. 2017;25:3596-3604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 8. | Hara Y, Ikoma K, Arai Y, Ohashi S, Maki M, Kubo T. Alteration of hindfoot alignment after total knee arthroplasty using a novel hindfoot alignment view. J Arthroplasty. 2015;30:126-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 39] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 9. | Jeong BO, Kim TY, Baek JH, Jung H, Song SH. Following the correction of varus deformity of the knee through total knee arthroplasty, significant compensatory changes occur not only at the ankle and subtalar joint, but also at the foot. Knee Surg Sports Traumatol Arthrosc. 2018;26:3230-3237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 41] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 10. | Kim CW, Gwak HC, Kim JH, Lee CR, Kim JG, Oh M, Park JH. Radiologic Factors Affecting Ankle Pain Before and After Total Knee Arthroplasty for the Varus Osteoarthritic Knee. J Foot Ankle Surg. 2018;57:865-869. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 11. | Levinger P, Menz HB, Morrow AD, Bartlett JR, Feller JA, Fotoohabadi MR, Bergman NR. Dynamic foot function changes following total knee replacement surgery. Knee. 2012;19:880-885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Mansur H, Rocha FA, Garcia PBL, de Alencar FHU, Guilme P, de Castro IM. Alteration of Hindfoot Axis After Total Knee Arthroplasty. J Arthroplasty. 2019;34:2376-2382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Mullaji A, Shetty GM. Persistent hindfoot valgus causes lateral deviation of weightbearing axis after total knee arthroplasty. Clin Orthop Relat Res. 2011;469:1154-1160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 74] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 14. | Okamoto Y, Otsuki S, Jotoku T, Nakajima M, Neo M. Clinical usefulness of hindfoot assessment for total knee arthroplasty: persistent post-operative hindfoot pain and alignment in pre-existing severe knee deformity. Knee Surg Sports Traumatol Arthrosc. 2017;25:2632-2639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 15. | Palanisami DR, Rajasekaran RB, Reddy PK, Natesan R, Sethuraman A, Rajasekaran S. Foot loading pattern and hind foot alignment are corrected in varus knees following total knee arthroplasty: a pedobarographic analysis. Knee Surg Sports Traumatol Arthrosc. 2020;28:1861-1867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Takenaka T, Ikoma K, Ohashi S, Arai Y, Hara Y, Ueshima K, Sawada K, Shirai T, Fujiwara H, Kubo T. Hindfoot alignment at one year after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2016;24:2442-2446. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 17. | Cobey JC. Posterior roentgenogram of the foot. Clin Orthop Relat Res. 1976;202-207. [PubMed] |
| 18. | Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports. 2000;10:2-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 647] [Cited by in RCA: 786] [Article Influence: 30.2] [Reference Citation Analysis (0)] |
| 19. | Meding JB, Keating EM, Ritter MA, Faris PM, Berend ME, Malinzak RA. The planovalgus foot: a harbinger of failure of posterior cruciate-retaining total knee replacement. J Bone Joint Surg Am. 2005;87 Suppl 2:59-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Garcia-Mansilla I, Yi S S-Editor: Fan JR L-Editor: A P-Editor: Xing YX