Published online Feb 18, 2020. doi: 10.5312/wjo.v11.i2.129
Peer-review started: May 20, 2019
First decision: July 31, 2019
Revised: November 8, 2019
Accepted: November 25, 2019
Article in press: November 25, 2019
Published online: February 18, 2020
Processing time: 279 Days and 2 Hours
Cleft foot is a very rare congenital anomaly, which is characterized by central rays deficiency of the foot. It is also known as split foot or ectrodactyly of the foot, and it is very often combined with splitting of the hands. The defect develops due to insufficient activity of the median apical ectodermal ridge, which leads to an increase in cell death or a decrease in cell proliferation. Due to the rarity of the pathology, there are few papers on the surgical treatment of this congenital foot disease, and publications to date concern the treatment of children.
We present a clinical case of congenital splitting of the feet and hands in a 31-year-old woman and a long-term result of foot treatment using the minimal arrangement of the Ilizarov apparatus. The patient had paternal inheritance of the trait. After the surgical treatment, cosmetic view and functional condition of the foot were improved and persisted two years after intervention. There were no complications in the treatment process.
The possibility of dosed control and stable fixation of the foot rays made it possible to create favorable conditions for the healing of the central wound and the closure of the segment splitting without complications. The long-term outcome of the treatment of foot congenital splitting using the proposed Ilizarov apparatus arrangement has shown its effectiveness. Our approach should be considered as an option of treatment in similar cases.
Core tip: We present a clinical case of rare congenital anomaly of feet and hands in a 31-year-old woman and a long-term result of foot treatment using the minimalist construct of the Ilizarov external fixator. The treatment approach made it possible to create favorable conditions for healing of the central wound and closure of segment splitting without complications. The long-term outcome of our treatment of the congenital foot anomaly has shown its effectiveness and can be considered in similar cases.
- Citation: Leonchuk SS, Neretin AS, Blanchard AJ. Cleft foot: A case report and review of literature. World J Orthop 2020; 11(2): 129-136
- URL: https://www.wjgnet.com/2218-5836/full/v11/i2/129.htm
- DOI: https://dx.doi.org/10.5312/wjo.v11.i2.129
Cleft foot is a very rare congenital anomaly, which is characterized by central rays deficiency of the foot: From shortening of the central toe to the absence of several rays of the foot. It is also known as split foot or ectrodactyly of foot, and it is very often combined with splitting of the hands. The first report of this anomaly was from South Africa in 1770[1]. The prevalence of the disease is 1 case per 90000 newborns and 1 case per 120000 in the population[2,3], and according to some data, 1 case per 1000000 live newborns[4]. It may be isolated or may be a part of a syndrome of deformity, and it is more common as bilateral[5]. The defect develops due to insufficient activity of the median apical ectodermal ridge, which leads to an increase in cell death or a decrease in cell proliferation[6]. Cleft foot (or hand) is usually inherited as an autosomal dominant type with reduced penetrance, although there are reports of sporadic, autosomal recessive and X-related forms[7,8]. To the present date, seven types of this anomaly have been described. Chromosomal rearrangement leads to the association of ectrodactyly with other disorders. Today, there are more than 50 syndromes that are associated with congenital splitting of the feet/hands. There are possible combinations of this malformation with anencephaly, cleft lip and palate, clinodactyly, scoliosis, nonperforation of the anus, anonychia, cataract and deafness[9].
Surgical reconstruction in splitting of the hands includes the closure of the cleft, the release of syndactyly, correction of the adduction of the first finger and the removal of transverse or deformed bones[9,10]. Surgical treatment of ectrodactyly of the feet is discussed to date[11]. Due to the rarity of the pathology, there are few publications about surgical treatment of this congenital foot disease; moreover, available literature concerns the treatment of children[12-18]. We present a clinical case of congenital splitting of the feet and hands in an adult patient and a long-term result of applying the minimum arrangement of the Ilizarov apparatus to correct this foot defect.
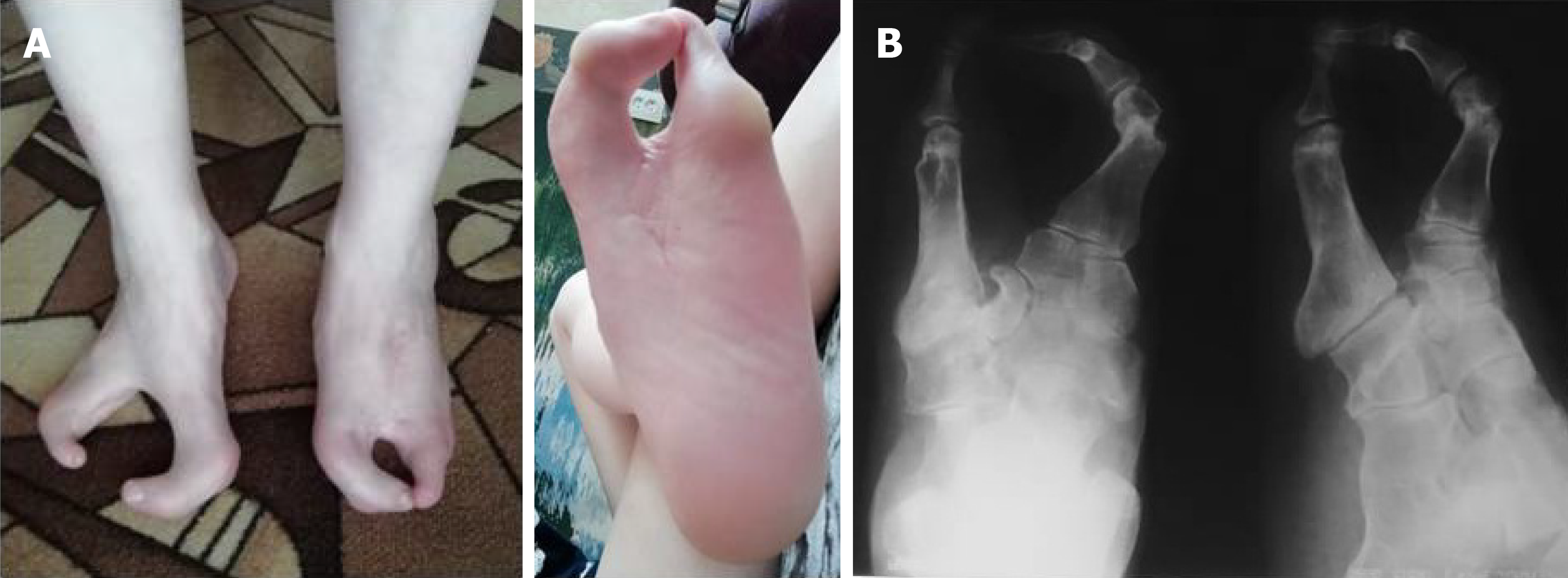
A female patient, 31-years-old, was admitted to the Ilizarov Center with complaints of painful calluses on the feet, difficulty in selecting shoes, a pronounced limitation of the function of the hands and a cosmetic defect of the lower (Figure 1) and upper extremities (Figure 2).
The patient is a resident of the countryside. There are no demographic and origin features. From the anamnesis, it is noted that her grandfather, father, brother and paternal uncles also have a similar anomaly in the development of hands and feet. Her aunt and grandmother have no such problems.
The patient had not been treated surgically; she was denied medical care and offered only amputation of the fingers at other facilities.
The patient wore overly wide shoes. The range of motion in elbow, wrist, hip, knee and ankle joints was full. The feet were strongly spread and represented by two rays (deep cleft with absence of central foot rays) (Figure 1). The patient had pronounced limitation of function and severe cosmetic defect of hands (each segment was represented by three rays with absence of fingers 1-4) (Figure 2). She could hold large non-heavy things, and her palm-finger grasp was preserved.
Blood analysis and urine analysis were normal. Electrocardiogram, chest x-ray and arterial blood gas were also normal.
The feet were represented by two rays (V type according to Blauth W. and Borisch N.C. classification[2], II type according to Abraham E et al[18]) (Figure 1). The hands were represented by three metacarpals with transverse bone in base of cleft and absence of fingers 1-4 (Figure 2).
Congenital anomaly, ectrodactyly of the feet (V type according to Blauth W. and Borisch N.C. classification, II type according to Abraham E et al[18]) and ectrodactyly of the hands.
Surgical treatment was divided into several stages. To start surgical treatment from the feet was the patient’s desire because the anomaly of the feet caused her more inconvenience. At the first stage, we performed surgical treatment on the left foot using a small arrangement of the Ilizarov apparatus (Figure 3). The patient noted more discomfort with the left foot than with the right foot.
First, open access was performed on the left foot, rudiment of central foot ray was removed and resectional wedge-shaped osteotomy of cuboid and cuneiform bones was performed to bring the rays together (Figure 3A). In the midfoot area, two olivial wires were pushed towards each other. Through the metatarsal bones, two olivial wires were also passed towards each other. Each pair of olivial wires was fixed in the semi-ring of the original Ilizarov apparatus. The supports were interconnected by straight rods. Then corrective osteotomy of both metatarsal bones was performed (Figure 3A) with fixation of each ray by two wires, which were fixed on the rods. Correction of the foot rays position was made by tensioning the wires in the supports (Figure 3B). After that, we performed suturing of the central space and Z-shaped skin plasty to close the foot defect. Patient started walking by gradually increasing weight-bearing on the left foot beginning on the 3rd d after surgery. Dressings after surgery were performed daily for 3 d and then weekly. The patient was discharged for outpatient treatment at the place of residence after 2 wk. The period of fixation of the left foot by the Ilizarov apparatus was 59 d.
The treatment approach made it possible to create favorable conditions for healing of the central wound and closure of segment splitting without complications. Two years after surgery, the result of the treatment on the left foot was maintained, and the patient was satisfied. According to the patient, the support on the foot improved (Figure 4). For family reasons, the patient was forced to take a long pause between the stages of treatment of the feet. Currently, we plan to perform a similar surgical treatment on the right foot.
Cleft hand/foot deformity is a rare congenital anomaly. Severity of hand/foot splitting varies[5]. Prenatal diagnosis of cleft hand/foot malformations can be established from the first trimester[5,19]. A number of publications devoted to this disease describe only pathogenesis and diagnostics of this pathology[3-5,7,8,19].
Surgical treatment strategies of this disorder are debatable. Due to the rarity of the pathology, there are few publications on the surgical treatment of ectrodactyly of the foot, and all of them describe the experience of children’s treatment[12-18]. There are no publications about surgical treatment of adults with this congenital malformation of feet. Some authors recommend that children do not undergo surgery if the feet are well-supporting and it is possible to wear normal shoes[11]. Other colleagues insist that the surgical treatment of this splitting should be carried out before the age of 1 year[12,13]. The aim of treatment of patients with this congenital anomaly is to improve foot function and cosmetic view[14]. In children, operative treatment is aimed at closing the central foot defect with possible osteotomy/resection of the segment bones and fixation of the forefoot by wires or screws and even transplanting fingers into the defect zone[12-17,20] or amputation[18] (Table 1).
| Authors | Number of patients/feet | Surgery, technique | Results |
| Sumiya et al[12] | 8/16 | Reconstruction of five toes: Closing of defect; creation of third toe by double pedicle flaps from the cleft area; separating third and fourth toes to create five toes by using free skin grafts from the skin defects | Excellent results in terms of both the function and the aesthetics |
| Wood et al[13] | 9/15 | Triangular flaps, in addition metatarsal osteotomies, intermetatarsal ligament reconstruction, fixation by Kirschner wires | The feet maintained good cosmetic and function |
| Choudry et al[14] | 3/5 | Removal of central wedge of skin; excision of central metatarsal; lateral release of the adductors and capsule of hallux metatarsophalangeal joint; osteotomy of fifth metatarsal; fixation by Kirschner wire; soft tissue syndactylization | All patients were happy with the cosmetic results |
| Tani et al[15] | 21/32 | Simple closure, silicone block insertion, application of a double-pedicled flap | Only 1 patient of 14 with long-term follow-up complained of pain following walking |
| Talusan et al[16] | 1/2 | Suture-button construct | Positive result |
| Lejman et al[17] | 3/5 | Wedge resection of the metatarsals with screw fixation and skin syndactyly | All patients were satisfied |
| Abraham et al[18] | 16/32 | Soft-tissue syndactylism, partial hallux valgus correction; soft-tissue syndactylism with first-ray osteotomy; first-ray amputation | 23 of the 24 procedures performed gave a satisfactory result |
| Sunagawa et al[20] | 1/1 | Microvascular toe transfer from a contralateral side that was amputated | Longitudinal growth of the grafted toe was symmetric, compared to the recipient toes, and the appearance of the treated foot was quite natural |
However, the adult’s foot is more rigid than a child’s segment, and it is difficult for such patients to use regular shoes or an orthosis. Often, patients with abnormal development of the distal lower extremities have impaired segment function and gait.
Surgical reconstruction in splitting of hands includes the closure of the cleft, the release of syndactyly, correction of the adduction of the first finger and the removal of transverse or deformed bones[9,10]. The Snow-Littler and Miura procedures are the most common surgical techniques to close the cleft of hand and widen the thumb-index finger web space[21,22].
According to the surgical scheme (classification) of Abraham E et al[18], the recommended treatment of I type split foot (deficiency of the second or third ray to the metatarsal area) is to create syndactyly between the existing rays and partial correction of valgus deformity of the first ray if necessary. In type II (deep cleft to the tarsal part with the extension of the forefoot), syndactyly with osteotomy of the first ray is shown. With type III, when completely missing from the first to the third or fourth ray, the operation is not required. The authors recommend performing an amputation of the first foot ray after reaching the age of 5 years.
There are a number of publications in the literature on the use of external fixation to create favorable conditions for the healing of central wounds/defects of the soft tissues of the forefoot in the setting of diabetes and vascular disorders. Strauss et al[23] described the successful use of an external mini-fixator in the forefoot with the central wound of forefoot in the presence of diabetes and peripheral vascular diseases. Oznur et al[24] showed a positive result in the treatment of a defect in the forefoot after resection in the presence of diabetes using the Ilizarov apparatus. In our case of foot congenital splitting in an adult patient, we applied the minimal arrangement of the Ilizarov apparatus to create favorable conditions for healing the wound without tension and with stable fixation of the achieved result, which was described for the first time.
The possibility of dosed control and stable fixation of the foot rays made it possible to create favorable conditions for the healing of the central wound and the closure of the segment splitting without complications. The long-term outcome of the treatment of foot congenital splitting using the proposed Ilizarov apparatus arrangement has shown its effectiveness. Our approach should be considered as an option of treatment in similar cases.
| 1. | Hartsinck G. Beschryving van Guiana of de wilde Just iin Zuid America. Vol 2. Amsterdam: Gerrit Teilenburg; 1770. |
| 2. | Blauth W, Borisch NC. Cleft feet. Proposals for a new classification based on roentgenographic morphology. Clin Orthop Relat Res. 1990;258:41-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (2)] |
| 3. | Basel D, Kilpatrick MW, Tsipouras P. The expanding panorama of split hand foot malformation. Am J Med Genet A. 2006;140:1359-1365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Fusco C, Nittis P, Alfaiz AA, Pellico MT, Augello B, Malerba N, Zelante L, Reymond A, Merla G. A New Split Hand/Foot Malformation with Long Bone Deficiency Familial Case. J Pediatr Genet. 2017;6:98-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Durmaz MS, Demirtaş H, Hattapoğlu S, Kara T, Göya C, Adin ME. Bilateral cleft foot: Radiographic and prenatal ultrasound features of two siblings with a review of literature. Medicina (Kaunas). 2016;52:257-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Gane BD, Natarajan P. Split-hand/feet malformation: A rare syndrome. J Family Med Prim Care. 2016;5:168-169. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Elliott AM, Evans JA, Chudley AE. Split hand foot malformation (SHFM). Clin Genet. 2005;68:501-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Shamseldin HE, Faden MA, Alashram W, Alkuraya FS. Identification of a novel DLX5 mutation in a family with autosomal recessive split hand and foot malformation. J Med Genet. 2012;49:16-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 71] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 9. | Baba AN, Bhat YJ, Ahmed SM, Nazir A. Unilateral cleft hand with cleft foot. Int J Health Sci (Qassim). 2009;3:243-246. [PubMed] |
| 10. | Upton J, Taghinia AH. Correction of the typical cleft hand. J Hand Surg Am. 2010;35:480-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Herring JA. Disorders of the foot. In: Herring JA ed. Tachdjian’s pediatric orthopaedics: from the Texas Scottish Rite Hospital for children. Vol 2. 5th ed. Philadelphia: WB Saunders; 2014: 761-883. |
| 12. | Sumiya N, Onizuka T. Seven years' survey of our new cleft foot repair. Plast Reconstr Surg. 1980;65:447-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 11] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Wood VE, Peppers TA, Shook J. Cleft-foot closure: a simplified technique and review of the literature. J Pediatr Orthop. 1997;17:501-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Choudry Q, Kumar R, Turner PG. Congenital cleft foot deformity. Foot Ankle Surg. 2010;16:e85-e87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Tani Y, Ikuta Y, Ishida O. Surgical treatment of the cleft foot. Plast Reconstr Surg. 2000;105:1997-2002. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Talusan PG, Telles C, Perez JL, Reach JS. Treatment of cleft foot deformity with a suture-button construct in the pediatric foot: a case report. Foot Ankle Int. 2013;34:1299-1304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Lejman T, Michno P. [Surgical treatment of congenital cleft foot]. Chir Narzadow Ruchu Ortop Pol. 1998;63:475-478. [PubMed] |
| 18. | Abraham E, Waxman B, Shirali S, Durkin M. Congenital cleft-foot deformity treatment. J Pediatr Orthop. 1999;19:404-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | González-Ballano I, Savirón-Cornudella R, Alastuey-Aisa M, Garrido-Fernández P, Lerma-Puertas D. [Split hand-foot: sonographic detection at 12 weeks]. Ginecol Obstet Mex. 2014;82:490-495. [PubMed] |
| 20. | Sunagawa T, Kimori K, Ikuta Y, Ishida O, Tani Y. Microvascular toe transfer for cleft-foot plasty: eight-year follow-up. J Reconstr Microsurg. 2002;18:83-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 21. | Beck JD, Chang B, Jones NF. Over 20-year follow-up of Miura reconstruction of cleft hand. Hand (N Y). 2015;10:319-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 22. | Rider MA, Grindel SI, Tonkin MA, Wood VE. An experience of the Snow-Littler procedure. J Hand Surg Br. 2000;25:376-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Strauss MB, Bryant BJ, Hart JD. Forefoot narrowing with external fixation for problem cleft wounds. Foot Ankle Int. 2002;23:433-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 24. | Oznur A, Tokgözoğlu M. Closure of central defects of the forefoot with external fixation: a case report. J Foot Ankle Surg. 2004;43:56-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: Russia
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Malik S S-Editor: Wang J L-Editor: Filipodia E-Editor: Liu MY