Published online Nov 18, 2020. doi: 10.5312/wjo.v11.i11.499
Peer-review started: April 21, 2020
First decision: June 15, 2020
Revised: August 25, 2020
Accepted: September 22, 2020
Article in press: September 22, 2020
Published online: November 18, 2020
Processing time: 207 Days and 2.1 Hours
The morbidity and burden of knee osteoarthritis affecting millions of lives worldwide has created a constant pursuit in finding the ideal treatment for knee osteoarthritis. There has been a paradigm shift in the surgical treatment of osteoarthritis ever since the initial description of Volkmann’s tibial osteotomy. This review focuses on one such recent procedure, the proximal fibular osteotomy (PFO) for medial compartment knee osteoarthritis. This review encompasses the history, evidence, risk factors, outcomes and technical considerations of PFO.
To understand the evidence and its techniques, and whether this could be an alternative solution to the problem of knee osteoarthritis in the developing world.
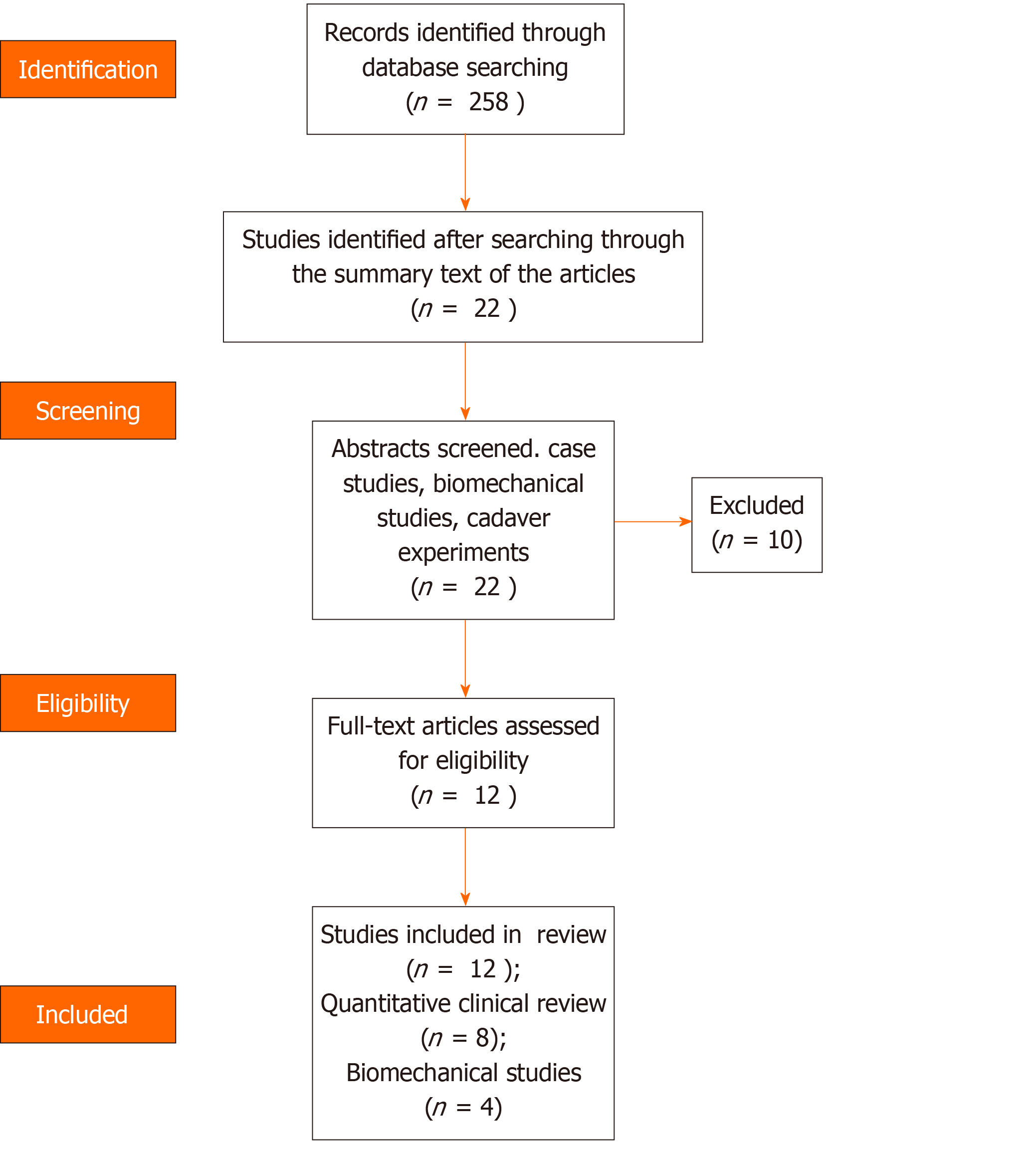
The phrases “proximal fibular osteotomy” and “knee osteoarthritis” were searched (date of search December 20, 2019) on PubMed to identify articles evaluating the biomechanical and clinical outcomes of PFO in patients with knee osteoarthritis. A total of 258 were retrieved. After reviewing the summary of the texts, 22 articles written in English were marked for abstract review. Articles that were case studies or cadaver experiments were excluded. The abstracts of the remaining articles were read, and only those that focused on the history, outcomes of case studies and technical considerations of PFO were included in the review. A total of 12 articles were included in this review.
At least six studies reported improvement in the visual analogue scale(VAS) from the average preoperative VAS score [6.32, 95% confidence interval (CI) = (4.05, 8.59)] to average postoperative VAS score [1.23, 95%CI: (-1.20, 3.71)], which was statistically significant. Similarly, the American Knee Society Score (KSS) functional score improved from an average preoperative KSS functional score [43.11, 95%CI: (37.83, 48.38)] to postoperative KSS functional score [66.145, 95%CI: (61.94, 70.35)], which was statistically significant. The femorotibial angle improved by around 7º, and the hip knee ankle angle improved by around 6º.
With the existing data, it seems that PFO is a viable option for treating medial joint osteoarthritis in selected patients. Long term outcome studies and progression of disease pathology are some of the important parameters that need to be addressed by use of multicenter randomized controlled trials.
Core Tip: The treatment of knee osteoarthritis with total knee arthroplasty is still a luxury and far-fetched for most patients from developing countries. The burden caused by the morbidity of knee osteoarthritis is more in Asian countries than in western countries, hence a treatment modality that could address this specific population subgroup within their financial hold is needed.
- Citation: Ashraf M, Purudappa PP, Sakthivelnathan V, Sambandam S, Mounsamy V. Proximal fibular osteotomy: Systematic review on its outcomes. World J Orthop 2020; 11(11): 499-506
- URL: https://www.wjgnet.com/2218-5836/full/v11/i11/499.htm
- DOI: https://dx.doi.org/10.5312/wjo.v11.i11.499
An unassisted bipedal gait is a complex series of movements that results in a progression of the body. This is perhaps one of the most fundamental functions of the human race on which humanity has thrived. This complex series of movements is crippled in persons with osteoarthritis, thereby affecting their livelihood significantly. The prevalence of knee osteoarthritis reported in 1997 by the Framingham study group was at 15.6%[1]. Since then, this rate has nearly doubled (28.7%) in countries like India[2]. Treatment options include various nonsurgical and surgical management strategies; total knee arthroplasty (TKA) is the treatment of choice in end stage knee osteoarthritis. It is estimated that by 2030, the demand for TKA is projected to grow at a staggering 673%, reaching 3.4 million surgeries between the years 2005-2030[3].
The procedure, although highly effective, incurs a significant expenditure to both the hospital and the patient[4]. In most developed countries, with bundled payments, insurance coverage of costs, meticulous data collection and sample analysis by way of maintaining arthroplasty registries, TKA has been deemed a successful operation for treatment of osteoarthritis. On the contrary, the treatment of knee osteoarthritis with TKA is still a luxury and far-fetched for most patients from developing countries. The burden caused by the morbidity of knee osteoarthritis is more in Asian countries than in western countries, hence a treatment modality that could address this specific population subgroup within their financial hold is needed. Hence, this review on proximal fibular osteotomy (PFO) was undertaken to understand the evidence and its techniques, and whether this could be an alternative solution to the problem of knee osteoarthritis in the developing world.
The phrases “proximal fibular osteotomy” and “knee osteoarthritis” were searched (date of search December 20, 2019) on PubMed to identify articles evaluating the biomechanical and clinical outcomes of PFO in patients with knee osteoarthritis. A total of 258 were retrieved. After reviewing the summary of the texts, 22 articles written in English were marked for abstract review. Articles that were case studies or cadaver experiments were excluded. The abstracts of the remaining articles were read, and only those that focused on the history, outcomes of case studies and technical considerations of PFO were included in the review. A total of 12 articles were included in this review (Figure 1).
Two investigators independently performed the quality assessment using the Coleman Methodology criteria, which has a maximum score of 100%. The average Coleman Methodology Score was 63.
In this review, there were eight clinical studies and four biomechanical studies on PFO. All of the reported studies were published after 2014. All of the clinical studies were from Asian countries (seven from China and one from Indonesia). The total number of knees analyzed in the clinical studies was 535 (Table 1). The PFO was done in these studies for all grades of symptomatic knee osteoarthritis. In two out of seven studies (including 203 knees), the authors did not document the grade of osteoarthritis in their patients undergoing PFO. Whereas, in the remaining 280 knees, the Kellegren-Lawrence grade of osteoarthritis was grade I (61 knees), grade 2 (97 knees), grade 3 (60 knees), and grade 4 (62 knees). The complications were listed only in three studies, there were twelve superficial peroneal nerve palsy and two common peroneal nerve palsy. However, all of these nerve palsies were transient and were recovered in an average time of 11.6 mo (range: 3 to 15 mo). The functional outcomes were assessed using the American Knee Society Score (KSS), Oxford Knee Score, Japanese Orthopaedic Association Knee Score, and Hospital for Special Surgery Score. The reported outcomes in all eight studies showed significant improvement of postoperative values as compared to preoperative values.
| No. | Ref. | Country | Year | Cases, n | Grade of osteoarthritis | Outcome score | Follow up period | Complications | Modified Colemans methodological quality assessment score |
| 1 | Yang et al[6] | China | 2015 | 156 | Not mentioned | KSS | 49 | CPN palsy = 2 nos; SPN palsy = 2 nos; All resolved | 76 |
| 2 | Zou et al[7] | China | 2017 | 92 | Grade 1, 2-30; grade 3, 4-10 | JOA | 25 | NVI = 1; Fracture = 1; Recurrent deformity = 1 | 68 |
| 3 | Wang et al[8] | China | 2017 | 47 | Not mentioned | KSS | 12 | Not available | 63 |
| 4 | Lu et al[9] | China | 2018 | 31 | Ahlback grade 1 | HSS | 24 | SPN palsy = 1 | 53 |
| 5 | Liu et al[10] | China | 2018 | 111 | Grade 2 = 17; Grade = 47; Grade = 47 | KSS | 12 | Not available | 68 |
| 6 | Nie et al[11] | China | 2018 | 16 | Grade 2 = 3; Grade 3 = 16 | HSS | 12 | Not available | 63 |
| 7 | Qin et al[12] | China | 2018 | 67 | KL score more than 2 with varus deformity | HSS | 36 | SPN palsy = 8 | 71 |
| 8 | Utomo et al[13] | Indonesia | 2018 | 15 | All cases were grade 4 | OKS | Immediate postoperative period only | Not available | 51 |
Among the biomechanical studies (Table 2), there were two cadaveric studies and three clinical studies. Unlike the clinical studies in this review, the demographics of the origin of these biomechanical studies did not belong to one particular region. All of the studies uniformly demonstrated medial compartment unloading following PFO.
| No. | Ref. | Country | Year | Type of study | Cases, n | Medial compartment unloading | Remarks |
| 1 | Yazdi et al[14] | Iran | 2015 | Cadaveric study | 6 | Yes | Increase in pressure of lateral compartment |
| 2 | Huang et al[15] | China | 2017 | Clinical study with gait analysis | 1 | Yes | Reduction in knee pain due to increasing femoral valgus, femoral external rotation and distal translation of knee |
| 3 | Baldini et al[16] | United States | 2018 | Cadaveric study | 10 | Yes | A decrease in lateral compartment as well as ankle joint pressure was noted |
| 4 | Nie et al[11] | China | 2018 | Clinical study with gait analysis and dynamic musculoskeletal analysis | 29 patient vs 20 controls | Yes | Decreased knee adduction moment was observed |
| 5 | Wang et al[17] | China | 2019 | Retrospective study with radiographic analysis | 560 knees | Yes | Reduction in knee adduction moments and rebalance the biceps-proximal fibula-peroneus longus complex |
Demographics and preoperative variables of the patients studied: A total of eight studies were included for the pooled sample quantitative analysis. The largest study to date by Yang et al[6] included 156 patients on whom the PFO was performed, but only 110 patients were available for follow-up to obtain postoperative data. After excluding patients with incomplete data sets, we had 450 patients available for quantitative analysis. The age of the patients was reported by all eight studies, and the average age of the patients undergoing PFO was 60.76 (range 58.45 to 63.96). Body mass index (BMI) was reported by three studies, and average BMI was 25.30 (range 24.20 to 27.38). Follow-up duration was mentioned by seven studies, and the average duration of follow-up was 21.9 mo (range 6.0 to 49.1 mo).
Outcome measures studied: Pain was assessed using the visual analog scale (VAS) score and was reported preoperatively in seven studies and postoperatively in six studies. There was no uniformity in the type of clinical outcome scores used in various studies. The KSS clinical outcome measure was used by three studies, the KSS functional score was reported by two studies, the Oxford Score was used in one study, the Japanese Knee Score was used in one study, and the Hospital for Special Surgery Score was used for one study. Femorotibial angle was used as a radiological outcome by three studies, and the hip knee ankle angle was used by two studies.
At least six studies reported improvement in VAS from the average preoperative VAS score [6.32, 95% confidence interval (CI): 4.05, 8.59] to average postoperative VAS score (1.23, 95%CI: -1.20, 3.71), which was statistically significant. Similarly, the KSS functional score improved from an average preoperative KSS functional score (43.11, 95%CI: 37.83, 48.38) to postoperative KSS functional score (66.145, 95%CI: 61.94, 70.35), which was statistically significant. The femorotibial angle improved by around 7 º, and the hip knee ankle angle improved by around 6 º. Complications were reported by three studies with a mean complication of 8 (range 1 to 8).
For this part of the analysis, we stratified postoperative outcome as “good” if there was less than 30% improvement in the preoperative outcome score and “excellent” if there was more than 30% increase in the reported outcome score. Outcomes from six studies were categorized as good, and outcomes from two studies were categorized as excellent. There was no statistical difference between the two groups in any of the preoperative variables including age, BMI, preoperative functional score, or VAS scores. Patients with excellent outcomes tended to have longer follow-up (27.5 mo) compared to patients with good outcomes (19.6 mo). However, this difference was not statistically significant but shows a trend that the outcome continues to get better with continuing follow-up up to two years. We also noted that higher complications occurred in patients with good outcomes (3 complications) compared to patients with excellent outcomes (0 complications). This further signifies the need for good surgical technique thereby avoiding early complications, which could affect the outcome up to two years.
When analyzing studies reporting more complications, none of the preoperative variables were noted to significantly differ between studies with less than 10% or more than 10% complications. However, it is difficult to interpret because complications were only reported by three studies.
The technique of osteotomy in knee osteoarthritis was first reported by Volkmann in 1875, wherein he had described a simple high tibial osteotomy (HTO) for surgical management of knee osteoarthritis. According to Wardle et al[18], combined tibial and fibular osteotomy was observed in Royal Southern Hospital, Liverpool in the year 1928. The reason for combining a fibular osteotomy was that it facilitates better union rates following the procedure. Over the years the tibial osteotomy procedure has been the workhorse procedure of choice in younger patients with osteoarthritis. The danger of nerve injuries following a combined tibia and fibula osteotomy was described by Preston et al[19].
Conversion to total knee arthroplasty following PFO was observed in four cases reported by Yang et al[6] after one year follow-up. Lu et al[9] reported no conversion to total knee arthroplasty following PFO in their study. The other authors did not mention conversion to total knee arthroplasty.
It was noted by Lu et al[9] that the disease progression had stopped when PFO was used in conjunction with medial meniscectomy. The authors felt that this could have happened as the medial meniscectomy addressing the theory of meniscal subluxation leading to osteoarthritis[20].
A statistically significant decrease in operative time, bleeding, and complication rates were observed when PFO was compared with HTO[7]. Also, in this study it was noted that there were improved clinical outcome scores in comparison with that of the HTO group.
The exact mechanism by which a PFO works is believed to be based on the principle of nonuniform settlement (discussed below). As reported by Wang et al[17], it is stated that the lateral support provided to the osteoporotic tibia by the fibula–soft tissue complex may lead to non-uniform settlement and degeneration of the plateau bilaterally, which may cause the load from the normal distribution to shift farther medially to the medial plateau, consequently leading to knee Varus and aggravating the progression of medial compartment osteoarthritis of the knee joint. A PFO thereby nullifies the effect of lateral support provided by the fibula and leads to unloading of the medial compartment of the knee.
The settlement phenomenon was studied radiographically using objective measurements by Dong et al[21]. Furthermore, they had also described that the proximal fibula had more bone density when compared with the proximal tibia by quantitative computed tomography bone scan.
Following a PFO, biomechanical cadaveric studies demonstrated that the medial compartment was unloaded. Meanwhile, gait analysis studies have shown a reduced knee adduction moment, increasing femoral valgus, femoral external rotation, and distal translation of knee. The factors that have been identified to be associated with outcome of PFO are the following[10,12] (Table 3): (1) Medial joint space; (2) Condyle plateau angle; (3) Hip knee ankle angle; (4) Settlement value; (5) Preoperative functional score; and (6) Patient BMI. Of which (1)-(4) are radiographic parameters, and (5) and (6) are clinical parameters.
| Radiological parameters | Clinical parameters |
| Medial joint space | Preoperative functional score |
| CP angle | Body mass index |
| HKA angle | |
| Settlement value |
Under epidural anesthesia, the pneumatic tourniquet was used for hemostasis, and the fibular posterolateral approach was performed in the supine position. The subcutaneous tissues were exposed, the intermuscular space between the peroneus longus and brevis and soleus muscle were found, curved forceps were used for layer separation until the proximal fibula, and then the subperiosteal dissection was performed. Two broad osteotomes were used to protect the soft tissues along the fibular medial surface. A 2 cm long fibula 6-10 cm away from the fibular head was cut off using a micro-oscillating saw and then washed thoroughly with 0.9% sodium chloride solution. The broken end was sealed by bone wax to reduce bleeding and pain. Combined with arthroscopic debridement, the synovial soft tissues and cartilage face were cleaned, loose bodies were removed, the meniscus was repaired and shaped, the lateral patellar retinaculum was released, and osteophytes were removed. The negative pressure drainage tube was placed and then removed within 24 h. The pneumatic pump was used to prevent lower limb venous thrombosis, and lower limb functional exercise was guided.
Peroneal nerve palsy is the most reported complication following PFO. Rupp et al[22] described the danger zones while performing fibular osteotomy. The neurovascular structures at primary risk in the proximal third region are the common peroneal nerve, superficial peroneal nerve, deep peroneal nerve, and anterior tibial artery. In the middle third region, primary risk is to peroneal artery and superficial peroneal nerve. This anatomical consideration forms the basis of selecting a 2 cm long fibula roughly 6-10 cm away from fibular head.
The certain characteristics of the case studies included in this review that are to be noted are: (1) Almost all of the case studies have an Asian background; and (2) The level of evidence is low. Ever since the initial descriptions and reports of proximal fibular osteotomy for medial joint knee osteoarthritis had surfaced, it has been faced with less enthusiasm as is evident by the number of published studies when compared with the voluminous data that exist in literature regarding total knee arthroplasty. However, with the existing data, it seems that PFO is a viable option for treating medial joint osteoarthritis in selected patients. Long term outcome studies and progression of disease pathology are some of the important parameters that need to be addressed by use of multicenter randomized controlled trials. Of particular note, the reason why studies on PFO from the developed countries remains sparse is rather intriguing. The rationale and technique of PFO seems to be promising but at a nascent stage according to the available literature.
A systematic review of articles pertaining to proximal fibular osteotomy (PFO).
To better understand the effects of PFO in treating medial compartmental arthritis.
To conduct a systematic review and Coleman’s methodological assessment.
To evaluate using systematic review using PRISMA guidelines and methodological quality of studies using Coleman’s scoring.
Short term and midterm outcomes have demonstrated clinically and statistically significant reduction in pain and functional outcomes.
The results obtained are rather encouraging and PFO may be a viable option in selected patients.
Further long term outcomes and randomized controlled trials are to be conducted to shed light on this treatment strategy.
| 1. | Felson DT, Zhang Y, Hannan MT, Naimark A, Weissman B, Aliabadi P, Levy D. Risk factors for incident radiographic knee osteoarthritis in the elderly: the Framingham Study. Arthritis Rheum. 1997;40:728-733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 495] [Cited by in RCA: 500] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 2. | Pal CP, Singh P, Chaturvedi S, Pruthi KK, Vij A. Epidemiology of knee osteoarthritis in India and related factors. Indian J Orthop. 2016;50:518-522. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 116] [Cited by in RCA: 152] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 3. | Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2079] [Cited by in RCA: 3320] [Article Influence: 174.7] [Reference Citation Analysis (0)] |
| 4. | Bumpass DB, Nunley RM. Assessing the value of a total joint replacement. Curr Rev Musculoskelet Med. 2012;5:274-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 68] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 5. | Fransen M, Bridgett L, March L, Hoy D, Penserga E, Brooks P. The epidemiology of osteoarthritis in Asia. Int J Rheum Dis. 2011;14:113-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 217] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 6. | Yang ZY, Chen W, Li CX, Wang J, Shao DC, Hou ZY, Gao SJ, Wang F, Li JD, Hao JD, Chen BC, Zhang YZ. Medial Compartment Decompression by Fibular Osteotomy to Treat Medial Compartment Knee Osteoarthritis: A Pilot Study. Orthopedics. 2015;38:e1110-e1114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 69] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 7. | Zou G, Lan W, Zeng Y, Xie J, Chen S, Qiu Y. Early clinical effect of proximal fibular osteotomy on knee osteoarthritis. Biomed Res. 2017;28:9291-9294. |
| 8. | Wang X, Wei L, Lv Z, Zhao B, Duan Z, Wu W, Zhang B, Wei X. Proximal fibular osteotomy: a new surgery for pain relief and improvement of joint function in patients with knee osteoarthritis. J Int Med Res. 2017;45:282-289. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 61] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 9. | Lu ZK, Huang C, Wang F, Miao S, Zeng L, He S, Ye S, Chen W. Combination of proximal fibulectomy with arthroscopic partial meniscectomy for medial compartment osteoarthritis accompanied by medial meniscal tear. J Clin Diagn Res. 2018;12:1-3. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Liu B, Chen W, Zhang Q, Yan X, Zhang F, Dong T, Yang G, Zhang Y. Proximal fibular osteotomy to treat medial compartment knee osteoarthritis: Preoperational factors for short-term prognosis. PLoS One. 2018;13:e0197980. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 11. | Nie Y, Ma J, Huang Z, Xu B, Tang S, Shen B, Kraus VB, Pei F. Upper partial fibulectomy improves knee biomechanics and function and decreases knee pain of osteoarthritis: A pilot and biomechanical study. J Biomech. 2018;71:22-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 12. | Qin D, Chen W, Wang J, Lv H, Ma W, Dong T, Zhang Y. Mechanism and influencing factors of proximal fibular osteotomy for treatment of medial compartment knee osteoarthritis: A prospective study. J Int Med Res. 2018;46:3114-3123. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (1)] |
| 13. | Utomo DN, Mahyudin F, Wijaya AM, Widhiyanto L. Proximal fibula osteotomy as an alternative to TKA and HTO in late-stage varus type of knee osteoarthritis. J Orthop. 2018;15:858-861. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | Yazdi H, Mallakzadeh M, Mohtajeb M, Farshidfar SS, Baghery A, Givehchian B. The effect of partial fibulectomy on contact pressure of the knee: a cadaveric study. Eur J Orthop Surg Traumatol. 2014;24:1285-1289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 15. | Huang W, Lin Z, Zeng X, Ma L, Chen L, Xia H, Zhang Y. Kinematic Characteristics of an Osteotomy of the Proximal Aspect of the Fibula During Walking: A Case Report. JBJS Case Connect. 2017;7:e43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (3)] |
| 16. | Baldini T, Roberts J, Hao J, Hunt K, Dayton M, Hogan C. Medial Compartment Decompression by Proximal Fibular Osteotomy: A Biomechanical Cadaver Study. Orthopedics. 2018;41:e496-e501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 17. | Wang J, Lv HZ, Chen W, Fan MK, Li M, Zhang YZ. Anatomical Adaptation of Fibula and its Mechanism of Proximal Partial Fibulectomy Associated with Medial Compartment Knee Osteoarthritis. Orthop Surg. 2019;11:204-211. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (3)] |
| 18. | Wardle EN. Osteotomy of the tibia and fibula in the treatment of chronic osteoarthritis of the knee. Postgrad Med J. 1964;40:536-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Preston CF, Fulkerson EW, Meislin R, Di Cesare PE. Osteotomy about the knee: applications, techniques, and results. J Knee Surg. 2005;18:258-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 20. | Gale DR, Chaisson CE, Totterman SM, Schwartz RK, Gale ME, Felson D. Meniscal subluxation: association with osteoarthritis and joint space narrowing. Osteoarthritis Cartilage. 1999;7:526-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 290] [Cited by in RCA: 303] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 21. | Dong T, Chen W, Zhang F, Yin B, Tian Y, Zhang Y. Radiographic measures of settlement phenomenon in patients with medial compartment knee osteoarthritis. Clin Rheumatol. 2016;35:1573-1578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 45] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 22. | Rupp RE, Podeszwa D, Ebraheim NA. Danger zones associated with fibular osteotomy. J Orthop Trauma. 1994;8:54-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Halabchi F S-Editor: Gao CC L-Editor: Filipodia P-Editor: Xing YX