Published online May 18, 2019. doi: 10.5312/wjo.v10.i5.219
Peer-review started: January 22, 2019
First decision: April 11, 2019
Revised: April 30, 2019
Accepted: May 14, 2019
Article in press: May 14, 2019
Published online: May 18, 2019
Processing time: 117 Days and 10.4 Hours
The purpose of open reduction and internal fixation of acetabulum posterior wall fractures is to restore anatomical structure and stability of the hip joint, in order to start weight bearing as soon as possible and prevent hip arthrosis; restoration of the anatomy should preserve function of the joint as well. Although “special shaped precontoured plates” have been developed in recent years for surgical treatment of this region, studies comparing the traditional plates with the newly designed precontoured plates are lacking.
To evaluate the biomechanical properties of precontoured anatomic buttress and conventional curved reconstruction plates (CCRPs) for posterior wall acetabulum fracture treatment.
Twelve pelvis models were created for testing plate treatment of fracture in the posterior wall of the acetabulum. These 12 pelvis models were used to create 24 hemipelvis models (experimental) by cutting from the sagittal plane and passing over the center of gravity, after which the posterior wall acetabular fractures (of similar type and size) were created. In these experimental models, the right acetabulum was fixed with a 5-hole CCRP, while the left was fixed with a precontoured anatomic buttress plate (PABP). Samples were placed through the test device and were subjected to static load testing, with a constant testing velocity of 2 mm/min until the load reached 2.3 kN or the acetabular fixation failed. Dynamic tests were also performed with sinusoidal wave load, with a maximal load of 2.3 kN and a load ratio of 0.1.
The average stiffness values were 460.83 ± 95.47 N/mm for the PABP and 291.99 ± 118.58 N/mm for the 5-hole CCRP. The precontoured anatomic acetabulum buttress plates had significantly higher rigidity than the CCRPs (P = 0.022). There was a statistically significant difference between the unloaded and 2.3 kN-loaded values of AL (posterosuperior fracture line vertical to the ground surface) and CL (posteroinferior fracture line vertical to the ground surface) parameters for both the PABPs and the 5-hole CCRPs (P = 0.036 and P = 0.045, respectively). According to the static tests, the amount of total displacement was significantly less in the PABPs than in the CCRPs. Comparative analysis of the displacement in the BL (posterior wall fracture line horizontal to the ground) parameter yielded no statistically significant differences between the PABP and the 5-hole CCRPs (P = 0.261).
PABP provides more stable fixation in acetabulum posterior wall fractures than 5-hole CCRP, allowing for proximal or distal fracture line screw application without reshaping.
Core tip: The results of this biomechanical study demonstrated that application of precontoured anatomic acetabular buttress plates in posterior wall fractures of the acetabulum provide more stable fixation than 5-hole conventional curved reconstruction plates. For the precontoured anatomic acetabular buttress plate, its features of anatomic contour, low profile, avoidance of joint penetration by locking screws, and allowance of placement of more screws through both the proximal and distal parts of a fracture pattern as needed represent marked advantages over the traditional plate.
- Citation: Altun G, Saka G, Demir T, Elibol FKE, Polat MO. Precontoured buttress plate vs reconstruction plate for acetabulum posterior wall fractures: A biomechanical study. World J Orthop 2019; 10(5): 219-227
- URL: https://www.wjgnet.com/2218-5836/full/v10/i5/219.htm
- DOI: https://dx.doi.org/10.5312/wjo.v10.i5.219
Almost one-fourth to one-third of all fractures of the acetabulum are posterior wall fractures[1]. Furthermore, most of these posterior wall fractures are comminuted and associated with an impaction injury of the articular surface. The Kocher-Langenbeck approach is appropriate for reduction and fixation of posterior acetabular wall fractures, and the traditional fixation methods generally involve reconstruction plates and/or screws.
Over the past decade, few surgical approaches and techniques to repair these fractures have been advanced, and most patients have had good clinical outcomes after anatomic reduction and rigid internal fixation[1-3]. Even nowadays, experienced surgeons report post-operative rates of osteoarthritis of 20%–60% following acetabular fracture fixation[1,4]. Because of the complex structure of the posterior acetabulum, providing anatomical alignment intra-operatively is sometimes difficult for surgeons. Use of conventional curved reconstruction plates (CCRPs) cause prolongation in the duration of surgery since intra-operative reshaping is required for adaptation to the posterior acetabular surface; moreover, ideal anatomical adaptation cannot always be provided.
Application of two reconstruction plates to obtain better fixation via the buttress effect creates additional risk due to the greater amount of screws used for penetration of the articular surface, which may lead to the development of osteoarthritis[5,6]. This conundrum makes the precontoured anatomic buttress plates (PABPs) attractive to surgeons, in spite of the fact that little information is available in the literature about the mechanical properties of these anatomical buttress plates.
The purpose of this study was, therefore, to evaluate the stiffness and rigidity of a PABP fixation model for fixation of posterior wall acetabular fractures and to compare with a CCRP model.
Twelve pelvis models were created, each with fractures made in the same manner through the posterior wall of the acetabulum, to serve as the biomechanical test material for this study. The simulated fracture line of the posterior wall was designed in a similar way and rendered on the basis of the work of Olson et al[7]. Two different types of fixation materials (CCRP and PABP) were used for fixation of the fractures created in these experimental models. Each of the fixated pelvis models were then embedded in a polyurethane block and an alignment tool was used to position the pelvis in an anatomical standing position. Hemipelvis models were then created by cutting each of the pelvis models from the sagittal plane and passing over the center of gravity.
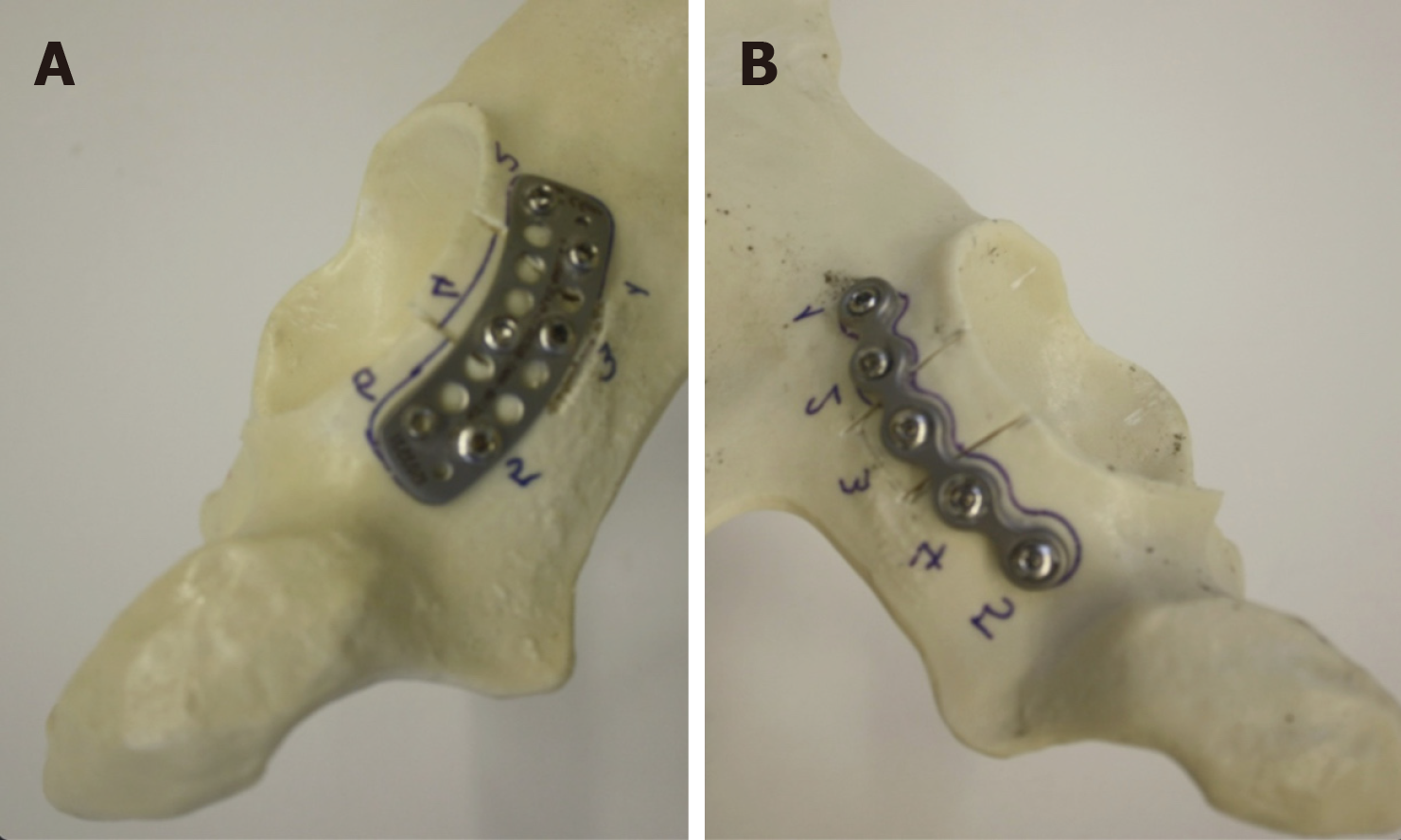
The right hemipelvis models were fixed by application of a 5-hole, 3.5-mm CCRP. In each model, the fracture fragment was fixed with a screw that was applied through the third hole of the plate, after which one non-locking screw and three locking screws were applied to the proximal and distal parts of the fracture line to complete the reconstruction. For experimental purpose, each hole of the plates on these models was numbered and all of the screws applied were of the same length and diameter (Figure 1A-B).
The left hemipelvis models were fixed by application of a PABP. In each model, the fracture fragment was fixed with two non-locking screws that were applied to the superior and inferior parts respectively, then four locking screws were applied to the proximal and distal parts of the fracture fragment. For experimental purpose, each hole of the plates on these models was numbered and all of the screws applied were of the same length and diameter (Figure 1A-B).
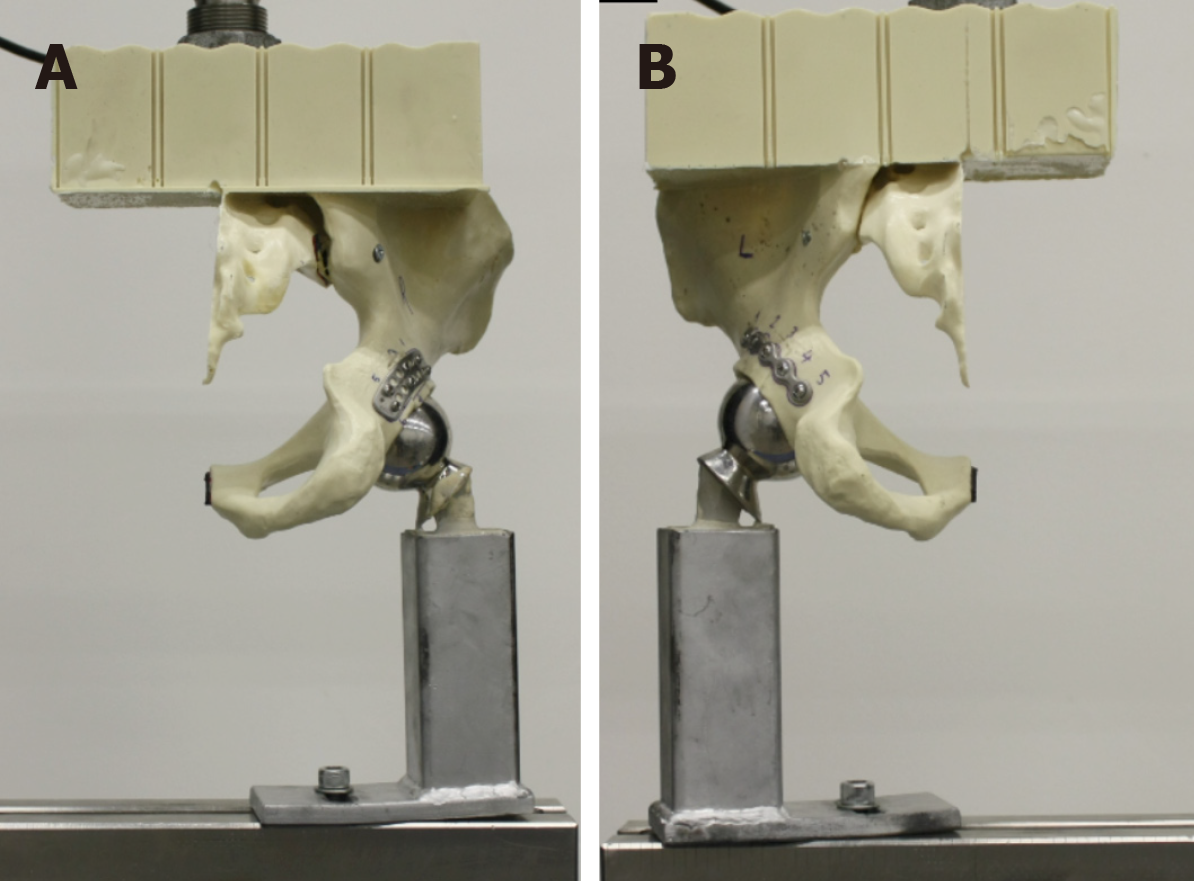
The embedding of the pelvis model in a polyurethane block allowed for us to simulate actual loading conditions and to apply force in the right direction. The embedded samples were placed into the Instron 3300 Universal Testing System (Instron, High Wycombe, United Kingdom) and subjected to axial load according to the anatomical reference position (Figure 2A-B). The samples were then subjected to static loading test, with 2 mm/min constant velocity until load reached 2.3 kN; this maximum load was selected from ISO 7206-4 as the maximum load for a single primer stem, and this value was accepted as the highest load. Load vs displacement values were recorded during the static tests. A high-resolution camera was used, with automatic shot to capture sample data during loading (per-second images taken continuously).
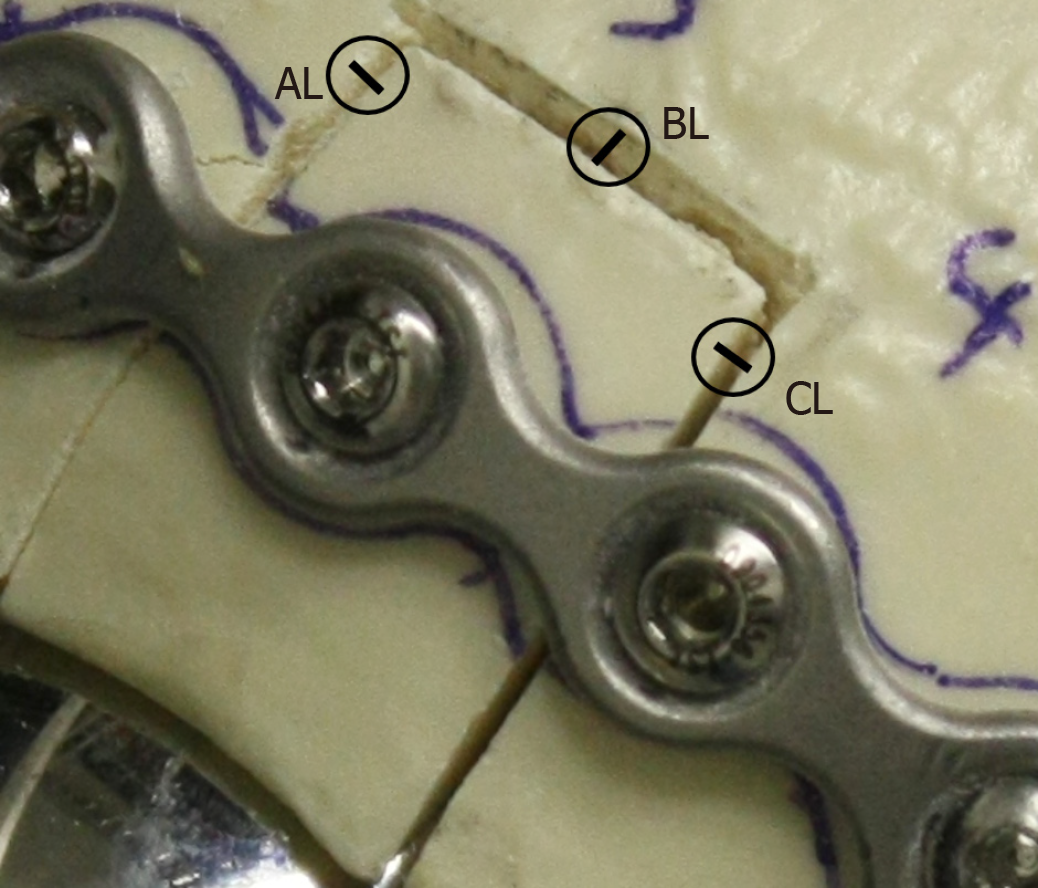
Some parameters determined on the photographs were measured by using the computer-assisted program before and after the 2.3 kN load, and then assessed by statistical comparative analyses (Figure 3). Dynamic tests were performed with sinusoidal wave load, with a maximal load of 2.3 kN and a load ratio of 0.1. In the case of a sample not breaking in the test, it was then subjected to 10 Hz for up to 1000 cycles. Photographs of the samples were taken two times, for measurements of before and after sample loading.
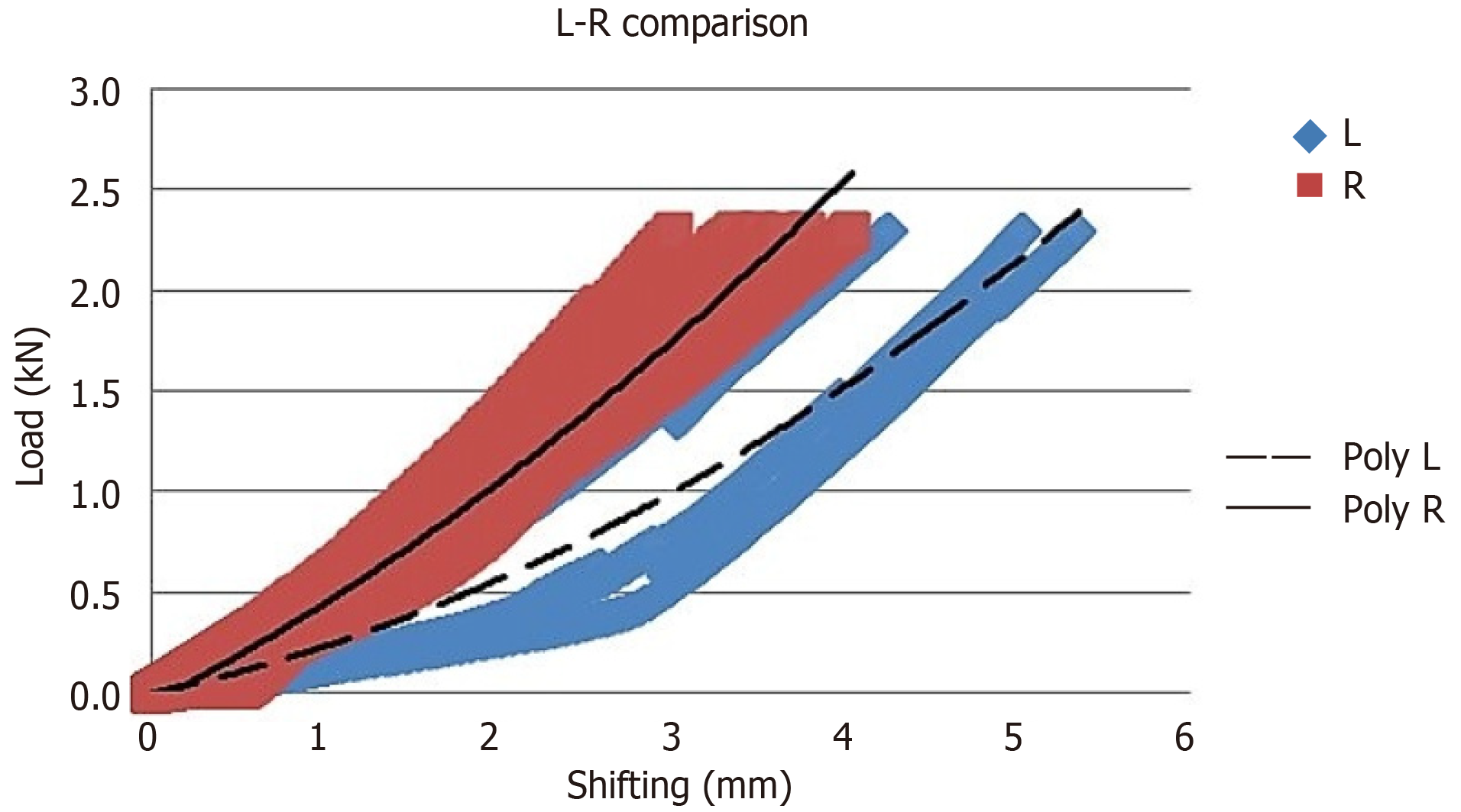
For static tests performed with a 5-hole 3.5-mm CCRP and a PABP, averages were taken for the two groups and a load-shifting distribution graph was generated (Figure 4). Rigidity was calculated for the two different plate types, according to the load-displacement distribution graph.
The SPSS statistical software package for Windows (version 11.5; SPSS Inc., Chicago, IL, United States) was used for the statistical analyses. The Shapiro-Wilk test was used to determine if the distributions of continuous variables were normal. The non-parametric Mann-Whitney U test was used to determine which group differed from the other groups significantly according to P value, with the threshold for significance set at 0.05.
The average stiffness values were determined to be 460.83 ± 95.47 N/mm for the PABP group and 291.99 ± 118.58 N/mm for the CCRP group. Rigidity of the PABPs was found to be significantly higher than that of the CCRPs (P = 0.022) (Table 1). There were statistically significant differences between the unloaded and 2.3 kN-loaded values of AL (posterosuperior fracture line vertical to the ground surface) and CL (posteroinferior fracture line vertical to the ground surface) parameters (Figure 3) for both the PABP group and CCRP group (P= 0.036 and P = 0.045, respectively). According to the static tests, the amount of total displacement was significantly less in the PABP group than in the CCRP group (Table 2). Statistical comparison of displacement in the BL (posterior wall fracture line horizontal to the ground) parameter (Figure 3) yielded no statistically significance difference between the PABP and CCRP groups (P = 0.261).
| PABP | CCRP | ||
| R1 | 345.26 | L1 | 400.17 |
| R2 | 542.77 | L2 | 172.49 |
| R3 | 570.23 | L3 | 445.06 |
| R4 | 504.47 | L4 | 196.14 |
| R5 | 353.87 | L5 | 196.05 |
| R6 | 448.36 | L6 | 342.02 |
| Mean | 460.83 | Mean | 291.99 |
| STD | 95.44 | STD | 118.58 |
| Plate | Amount of load-displacement values | |||||||
| CCRP | L1 | L2 | L3 | L4 | L5 | L6 | Mean | STD |
| AL | 0.22 | 0.46 | 0.09 | 0.05 | 0.12 | 0.08 | 0.17 | 0.16 |
| BL | 0.15 | 0.92 | 0.21 | 0.42 | 0.59 | 0.09 | 0.40 | 0.32 |
| CL | 0.41 | 0.16 | 0.11 | 0.35 | 0.12 | 0.09 | 0.21 | 0.14 |
| PABP | R1 | R2 | R3 | R4 | R5 | R6 | Mean | STD |
| AL | 0.00 | 0.16 | 0.05 | 0.04 | 0.05 | 0.04 | 0.06 | 0.05 |
| BL | 0.33 | 0.01 | 0.01 | 0.17 | 0.31 | 0.27 | 0.18 | 0.12 |
| CL | 0.03 | 0.05 | 0.08 | 0.01 | 0.41 | 0.08 | 0.11 | 0.15 |
The purpose of open reduction and internal fixation of acetabulum posterior wall fractures is to restore anatomical structure and stability of the hip joint, in order to start weight bearing as soon as possible and prevent hip arthrosis; restoration of the anatomy should also preserve function of the joint. However, post-traumatic osteoarthrosis of the hip joint has been reported in association with as many as 20% of fractures of the acetabulum posterior wall following treatment with open reduction and internal fixation[1,8,9].
Abnormal contact stress caused by unsatisfactory joint fixation is one of the crucial factors underlying development of post-traumatic arthritis. Because of the risk of arthritis and the high complication rates of surgical fixation, the option of total hip arthroplasty is preferred for acetabular fractures in older patients as an alternative to surgery[10]. CCRPs and PABPs, with or without inter-fragmentary screws, are the most common fixation methods practiced as treatment for posterior acetabular wall fractures. Biomechanical studies have indicated that the inter-fragmentary lag screws confer additional strength to the CCRP fixation[11,12].
Technological advances in implant technology over the recent past years have included the development of “special shaped precontoured plates” for surgical treatment of this region. However, only a few studies have been published that compare the biomechanical stability of different fixation methods[1,13-15]. Application of reconstruction plates following primary fixation with inter-fragmentary lag screw(s) is the treatment method used most commonly and safely. Liu et al[16] previously demonstrated that anatomical plates have higher accuracy than conventional ones, which is helpful for fracture reduction and reducing the operation’s difficulty. In our study, the experimental model in which fixation was applied with PABP and inter-fragmentary screws provided a rigid and reliable fixation, with average 1 mm displacement at an axial load of 2.3 kN.
A paramount issue related to fixation methods is the direction of the locking screws, which is directly associated with the direction of the screw holes. Although we encountered joint penetration in some screws during application of screws into the CCRP for two of the hemipelvis models in our study, joint penetration was not encountered in any screws during the application of the PABP in the hemipelvis samples. Due to design features of the plate itself, locking screws in a PABP have such advantages as inhibiting joint penetration and providing a safer fixation in the proximal and distal parts of a fracture fragment, with use of a greater amount of screws being possible as needed. In addition, the multiple-screw choice for the PABP allows for a greater number of compression screws to be placed into the acetabular fragment, through the plate. There is no need to place any extra screw beyond the plate. Due to this feature, the PABP can provide a safer fixation than the CCRP.
Application of a buttress influences the posterior wall of the acetabulum with a reconstruction plate, and inter-fragmentary screw is the most commonly used fixation method for surgical treatment of posterior wall fractures of the acetabulum. The PABP fixated models in our study had an average displacement of less than 1 mm with a load of 2.3 kN in static and dynamic tests. This feature will both impact comminution favorably and prevent development of degenerative arthrosis due to near-complete joint adaptation. The consequences of malreduction of joint congruency and insufficiency of surgical fixation are the reasons for poor results of acetabular fracture surgery[1,5]. Thus, the choice of fixation method applied in this condition and knowledge of the biomechanical properties of the methods are crucial.
Among the biomechanical studies in the literature to date, Sawaguchi et al[17] reported on fixation of the anterior column with a plate or lag screw and of the posterior column with one of three different plates; no differences were found between the various modalities. Mehin et al[18] suggested that the locking plate is as strong as the conventional plate plus inter-fragmentary lag screw for fixing transverse acetabular fractures. Simonian et al[19] evaluated the stability of different types of fixation methods for the T-type acetabular fracture and found that the differences in displacements were not statistically significant. Goulet et al[20] reported in 1994 that when concentric comminuted and transverse comminuted posterior wall fractures of the acetabulum were simulated separately, the stiffness of a reconstruction plate and screws was significantly higher than that achieved with screws alone. Still other studies have mentioned that, for treatment of posterior wall fractures, fixation with combined fixation materials was more reliable and stable due to the single reconstruction plates[21,22]. In our study, displacement of the single PABP was lower and rigidity was higher than for the CCRP.
It is important that our experimental-based study be discussed in the light of its limitations and strengths. Firstly, our biomechanical study was not performed with Sawbones® models or cadaveric specimens. Although, these pelvic models do not represent the heterogeneity of real bone, the homogeneity of the synthetic models (between each other) provides an advantage over the real specimens for more direct comparison without the potential confounding factors, such as age- or sex-related differences. Secondly, the range of patterns of acetabulum posterior wall fractures is wide but the instability of a fracture and the intra-articular component of a fragment remain the major features of the posterior wall fracture type. As such, we focused on an instable and intra-articular fracture pattern for the creation of our simulated fracture figure. Finally, the screw numbers applied to the two groups of plates were not equal; the CCRP group has 5 screws/model and the PABP group had 6 screws/model. Yet this limitation of the study also underlies the PABP feature that increases the stability of the fracture pattern.
In conclusion, the results of this experimental study showed that application of PABP for posterior wall fractures of the acetabulum provides a more stable fixation than CCRP. The features of anatomic contour, low profile, avoidance of joint penetration of locking screws, and allowance for a greater amount of screws through the proximal and distal parts of the fracture pattern as needed are the marked advantages of PABPs. Although biomechanical and experimental data have shown this, further clinical studies are needed to support the findings.
The purpose of open reduction and internal fixation of acetabulum posterior wall fractures is to restore anatomical structure and stability of the hip joint, in order to start weight bearing as soon as possible and prevent hip arthrosis; restoration of the anatomy should preserve function of the joint as well.
Although “special shaped precontoured plates” have been developed in recent years for surgical treatment of this region, studies comparing the traditional plates with the newly designed precontoured plates are lacking.
The main objective of this study was to evaluate the biomechanical properties of precontoured anatomic buttress and conventional curved reconstruction plates (CCRPs) for posterior wall acetabulum fracture treatment, particularly to determine if one provides more stable fixation.
Hemipelvis models (experimental; divided at the sagittal plane and passing over the center of gravity) with similar posterior wall acetabular fractures were fixed with a 5-hole CCRP (right pelvis model) or a precontoured anatomic buttress plate (left pelvis model). These fixated hemipelvis samples were subjected to static load testing (constant testing velocity of 2 mm/min, applied until the load reached 2.3 kN or the acetabular fixation failed) and dynamic testing (sinusoidal wave load, with a maximal load of 2.3 kN and a load ratio of 0.1).
Rigidity of the precontoured anatomic acetabulum buttress plates was significantly higher than that of the CCRPs (P = 0.022).
The findings of this study support the use of anatomic buttress plates for posterior acetabular wall fractures’ surgical treatment. In this surgical treatment, the CCRP is insufficient for safe stability because of its need for anatomic adaptation, lower screw number allowance, and lack of a buttress effect. The precontoured anatomic acetabulum buttress plate is safer, according to its matching the anatomy of the posterior acetabular region and ability to use more screws. In practice, surgeons usually use two reconstruction plates to achieve stable fixation, doubling the surgical time; the use of a single precontoured anatomic acetabulum buttress plate will lessen the surgical time.
For posterior acetabular wall fractures, only fixing the fragment may not always be the best solution. Because the pelvic girdle is exposed to substantial force, according to its anatomic location, stable fixation with multiple screws is needed. Future research efforts must be made from the perspective of clinical practice, to provide biomechanical data from real-life experiences. We also caution that, in clinical practice, this type of fracture does not usually occur in isolation, and is generally accompanied by fracture in other parts of the pelvic girdle (i.e., sacroiliac), and for best results each single fracture pattern must be considered.
| 1. | Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78:1632-1645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 886] [Cited by in RCA: 923] [Article Influence: 31.8] [Reference Citation Analysis (0)] |
| 2. | Ebraheim NA, Patil V, Liu J, Sanford CG, Haman SP. Reconstruction of comminuted posterior wall fractures using the buttress technique: a review of 32 fractures. Int Orthop. 2007;31:671-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Kumar A, Shah NA, Kershaw SA, Clayson AD. Operative management of acetabular fractures. A review of 73 fractures. Injury. 2005;36:605-612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 61] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Kreder HJ, Rozen N, Borkhoff CM, Laflamme YG, McKee MD, Schemitsch EH, Stephen DJ. Determinants of functional outcome after simple and complex acetabular fractures involving the posterior wall. J Bone Joint Surg Br. 2006;88:776-782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 166] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 5. | Russell GV, Nork SE, Chip Routt ML. Perioperative complications associated with operative treatment of acetabular fractures. J Trauma. 2001;51:1098-1103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Ebraheim NA, Savolaine ER, Hoeflinger MJ, Jackson WT. Radiological diagnosis of screw penetration of the hip joint in acetabular fracture reconstruction. J Orthop Trauma. 1989;3:196-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Olson SA, Bay BK, Chapman MW, Sharkey NA. Biomechanical consequences of fracture and repair of the posterior wall of the acetabulum. J Bone Joint Surg Am. 1995;77:1184-1192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 80] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Baumgaertner MR. Fractures of the posterior wall of the acetabulum. J Am Acad Orthop Surg. 1999;7:54-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 99] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 9. | Letournel E, Judet R. Fractures of the acetabulum. Posterior wall fractures. 2nd ed. New York: Springer-Verlag 1993; 67-88. [DOI] [Full Text] |
| 10. | Tissingh EK, Johnson A, Queally JM, Carrothers AD. Fix and replace: An emerging paradigm for treating acetabular fractures in older patients. World J Orthop. 2017;8:218-220. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Chang JK, Gill SS, Zura RD, Krause WR, Wang GJ. Comparative strength of three methods of fixation of transverse acetabular fractures. Clin Orthop Relat Res. 2001;433-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 48] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Shazar N, Brumback RJ, Novak VP, Belkoff SM. Biomechanical evaluation of transverse acetabular fracture fixation. Clin Orthop Relat Res. 1998;215-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Su K, Liu S, Wu T, Yin Y, Zhang R, Li S, Zhang Y. Posterior column acetabular fracture fixation using a W-shaped angular plate: A biomechanical analysis. PLoS One. 2017;12:e0187886. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (2)] |
| 14. | Zhang Y, Tang Y, Wang P, Zhao X, Xu S, Zhang C. Biomechanical comparison of different stabilization constructs for unstable posterior wall fractures of acetabulum. A cadaveric study. PLoS One. 2013;8:e82993. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Fulkerson E, Egol KA, Kubiak EN, Liporace F, Kummer FJ, Koval KJ. Fixation of diaphyseal fractures with a segmental defect: a biomechanical comparison of locked and conventional plating techniques. J Trauma. 2006;60:830-835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 136] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 16. | Liu Q, Zhang K, Zhuang Y, Tao K, Fu Y. A morphological study of anatomical plates for acetabular posterior column. Int J Comput Assist Radiol Surg. 2014;9:725-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Sawaguchi T, Brown TD, Rubash HE, Mears DC. Stability of acetabular fractures after internal fixation. A cadaveric study. Acta Orthop Scand. 1984;55:601-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 35] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Mehin R, Jones B, Zhu Q, Broekhuyse H. A biomechanical study of conventional acetabular internal fracture fixation versus locking plate fixation. Can J Surg. 2009;52:221-228. [PubMed] |
| 19. | Simonian PT, Routt ML, Harrington RM, Tencer AF. The acetabular T-type fracture. A biomechanical evaluation of internal fixation. Clin Orthop Relat Res. 1995;234-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 20. | Goulet JA, Rouleau JP, Mason DJ, Goldstein SA. Comminuted fractures of the posterior wall of the acetabulum. A biomechanical evaluation of fixation methods. J Bone Joint Surg Am. 1994;76:1457-1463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 60] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 21. | Liu XM, Pan CW, Wang GD, Cai XH, Chen L, Meng CF, Huang JC. Finite element analysis of the stability of combined plate internal fixation in posterior wall fractures of acetabulum. Int J Clin Exp Med. 2015;8:13393-13397. [PubMed] |
| 22. | Wu X. A biomechanical comparison of different fixation techniques for fractures of the acetabular posterior wall. Int Orthop. 2018;42:673-679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: Turkey
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Liu J S-Editor: Dou Y L-Editor: A E-Editor: Wu YXJ