©The Author(s) 2015.
World J Orthop. Mar 18, 2015; 6(2): 202-210
Published online Mar 18, 2015. doi: 10.5312/wjo.v6.i2.202
Published online Mar 18, 2015. doi: 10.5312/wjo.v6.i2.202
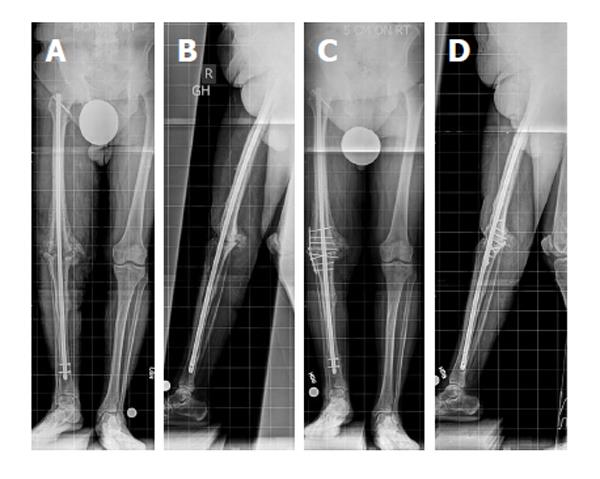
Figure 1 Radiographs of the knee.
Anteroposterior (A) and lateral (B) view radiographs of the knee show nonunion of a knee arthrodesis with a long intramedullary nail, without evidence of implant failure or loosening. The intramedullary (IM) nail diameter has a good diaphyseal canal fit but poor canal fit at the arthrodesis site and surrounding metaphysis, which decreases bending and rotational stability provided by the IM nail in this region. Decreased stability increases motion at the arthrodesis site, which can impede bony healing. Anteroposterior (C) and lateral (D) view radiographs of the knee after supplemental plate fixation around the existing knee fusion nail and bone grafting of the nonunion site. Supplemental plate fixation provides additional stability at the nonunion site, which promotes bony healing and union of the knee arthrodesis. Bicortical screw fixation is achieved by aiming slightly posterior to the IM nail. Note the motion at the distal interlocking screws is now visible; however, the knee arthrodesis site has progressive consolidation (reprinted with permission from the Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore).
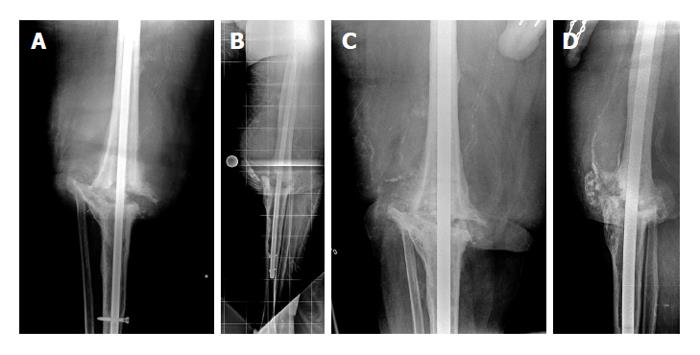
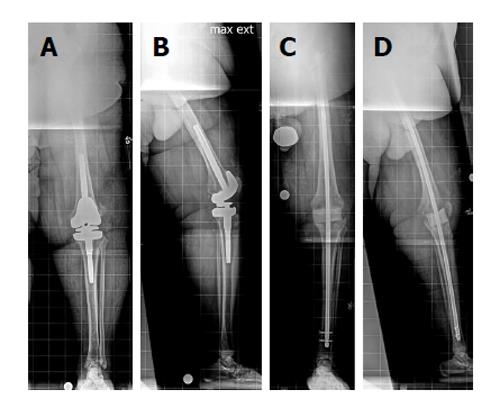
Figure 2 Anteroposterior and lateral view radiographs of the knee.
Anteroposterior (A) and lateral (B) view radiographs of the knee show a nonunion of a knee arthrodesis following insertion of an antegrade knee arthrodesis rod with inadequate tibial length. In this case, the intramedullary (IM) nail is shorter than what is typically used in such cases. The distal end of the nail should be 2 cm above the ankle joint. Also, this IM nail diameter is too small to provide a good canal fit. The IM diameter is measured, and exchange nailing is planned. Anteroposterior (C) and lateral (D) view radiographs of the knee after exchange nailing and bone grafting of the nonunion site. Exchange nailing to a larger diameter rod improves canal fit, thus providing additional stability to the nonunion site. The IM nail length was also increased so that the distal end of the nail was 2 cm above the ankle joint. Increasing both the length and the diameter improves the biomechanical stability of the nail and decreases motion at the nonunion site, thus promoting bony healing (reprinted with permission from the Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore).
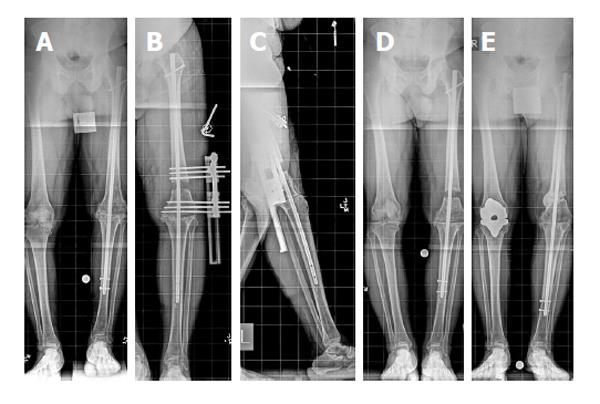
Figure 3 Knee arthrodesis.
A: Anteroposterior view full length standing radiograph shows that the left limb has a 3-cm limb length discrepancy. Note the lift that is used under the left limb; B: Anteroposterior view full length standing radiograph shows the distal femoral osteotomy and lengthening over the existing knee fusion nail. Note that the distal interlocking screws are removed from the nail; C: Full length lateral view radiograph shows that the pins of the external fixator have been placed away from the intramedullary nail; D: Postoperative anteroposterior view full length standing radiograph shows that interlocking screws have been placed and the external fixator has been removed. Note the resolution of the limb length discrepancy; E: Anteroposterior view full length standing radiograph obtained 2 years after lengthening (reprinted with permission from the Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore).
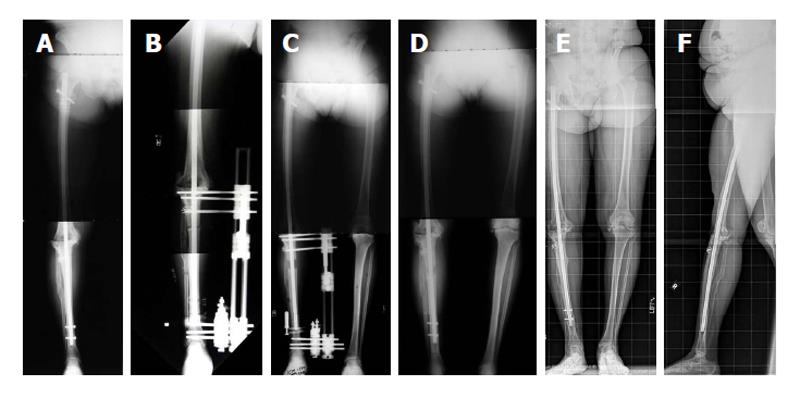
Figure 4 Sixty-four-year-old woman underwent total knee arthroplasty of the right knee and developed a chronic recurrent infection with loss of anterior soft tissue.
The infection was treated and the knee was fused, but she developed limb length discrepancy (LLD) and nonunion of the right knee. She underwent resection of the nonunion, implantation of bone graft and bone morphogenetic protein-2, and gradual lengthening for the LLD. Proximal tibial and fibular osteotomies were performed, and external fixation was applied to the tibia. The antibiotic cement-coated rod was not removed. A: Preoperative anteroposterior view full length standing radiograph obtained at the time of nonunion and prior to lengthening; B: Anteroposterior view radiograph obtained during the distraction stage of treatment. Note that the distal fibula was captured with an anteromedial to anterolateral half-pin; C: Anteroposterior view full length standing radiograph obtained after the distraction stage of treatment was completed; D: Anteroposterior view full length standing radiograph obtained after external fixation removal and insertion of interlocking screws; E and F: Anteroposterior (E) and lateral (F) view full length standing radiographs obtained 12 mo after external fixation was removed. Note the complete and total regenerate healing at the level of the proximal tibia (reprinted with permission from the Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore).
Figure 5 Temporary knee fusion is accomplished by inserting both an antibiotic cement-coated intramedullary knee fusion nail.
Anteroposterior (A) and lateral (B) view radiographs of the left leg in a 71-year-old patient with an infected revision total knee arthroplasty. The patient was morbidly obese. A knee joint gap greater than 5 cm was expected after removal of the infected implants. Knee flexion contracture was also present (B). Temporary knee fusion was planned. Anteroposterior (C) and lateral (D) view radiographs of the left leg obtained postoperatively show the temporary knee fusion, including a long, antibiotic cement-coated intramedullary nail and a static antibiotic cement-coated spacer to fill the knee joint gap (reprinted with permission from the Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore).
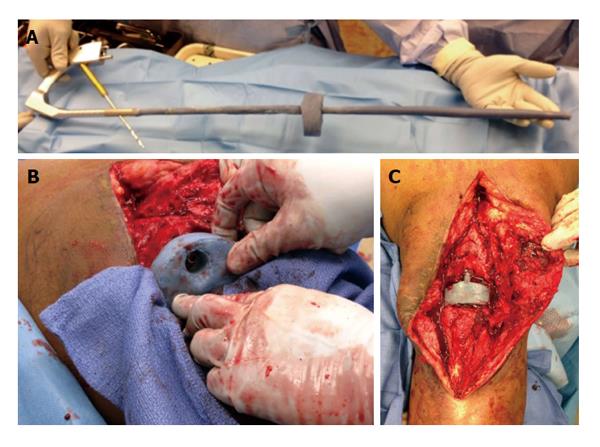
Figure 6 Intraoperative photographs of a temporary arthrodesis for an infected total knee arthroplasty.
A: Photograph shows the long, antibiotic cement-coated intramedullary fusion nail and antibiotic cement-coated spacer prior to insertion. The static antibiotic cement-coated spacer was made with a hole placed centrally that was large enough to accommodate the antibiotic cement-coated nail; B: The nail was inserted to the level of the distal femur, was guided through the central hole in the static spacer, and was guided into the tibia. As the nail was inserted into the tibia, the tibia was held in proper alignment and rotation. When the nail reached the midshaft of the tibia, axial load was applied to the lower extremity to prevent distraction from occurring at the knee; C: The knee wound following spacer insertion and locking of the rod (reprinted with permission from the Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore).
- Citation: Wood JH, Conway JD. Advanced concepts in knee arthrodesis. World J Orthop 2015; 6(2): 202-210
- URL: https://www.wjgnet.com/2218-5836/full/v6/i2/202.htm
- DOI: https://dx.doi.org/10.5312/wjo.v6.i2.202