©The Author(s) 2025.
World J Orthop. Nov 18, 2025; 16(11): 112307
Published online Nov 18, 2025. doi: 10.5312/wjo.v16.i11.112307
Published online Nov 18, 2025. doi: 10.5312/wjo.v16.i11.112307
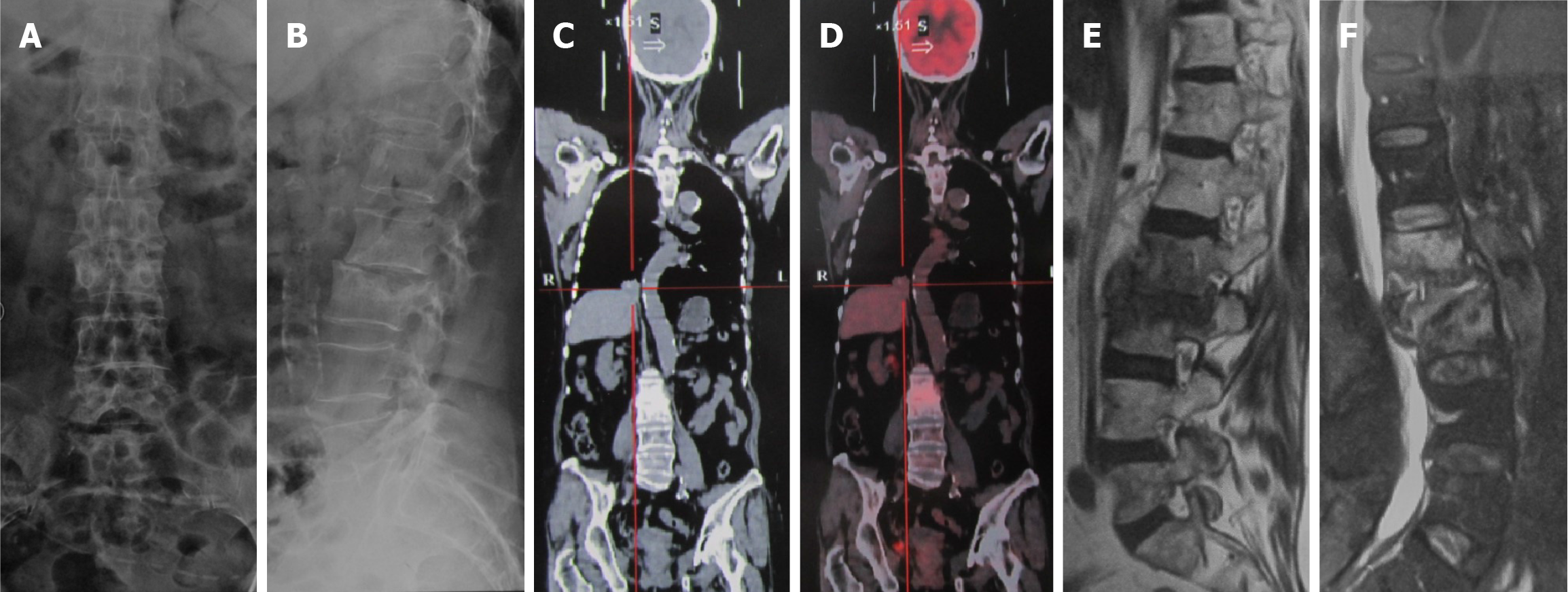
Figure 1 Imaging examinations before surgery.
A and B: Visible destruction of the L2 and L3 vertebral bodies, with narrowing of the L2/L3 space; C and D: Positron emission tomography/computed tomography suggest bone metastasis of lung cancer to the L2 and L3 vertebrae; E and F: Magnetic resonance imaging indicates increased signals in the L2 and L3 vertebral bodies and intervertebral space.
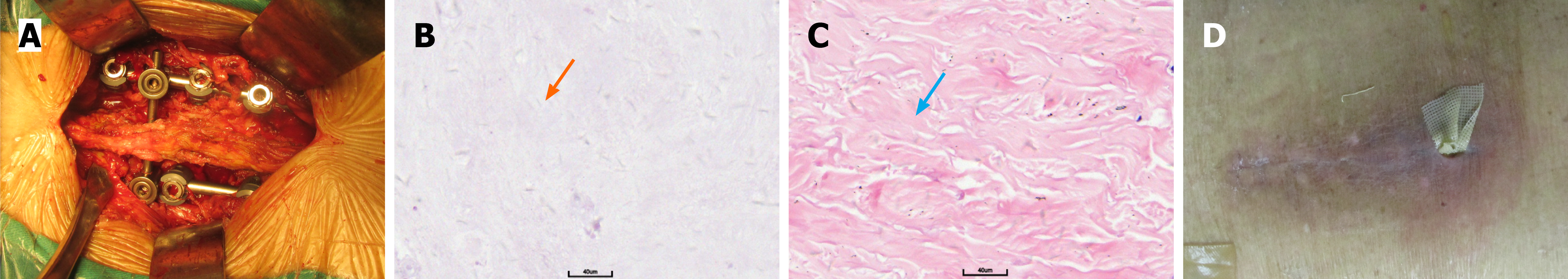
Figure 2 Intraoperative details and postoperative pathology.
A: Internal fixation during surgery; B: Postoperative case with intervertebral bone tissue, fibrous tissue, and necrotic tissue. The orange arrow points to the site of the lesion; C: Postoperative case with obvious proliferation of dermal sclerosis fibrous scar tissue accompanied by necrosis, suggesting chronic radiation dermatitis. The blue arrow points to the site of the pathology; D: Lower end of the incision was not healing, accompanied by inflammatory exudate.
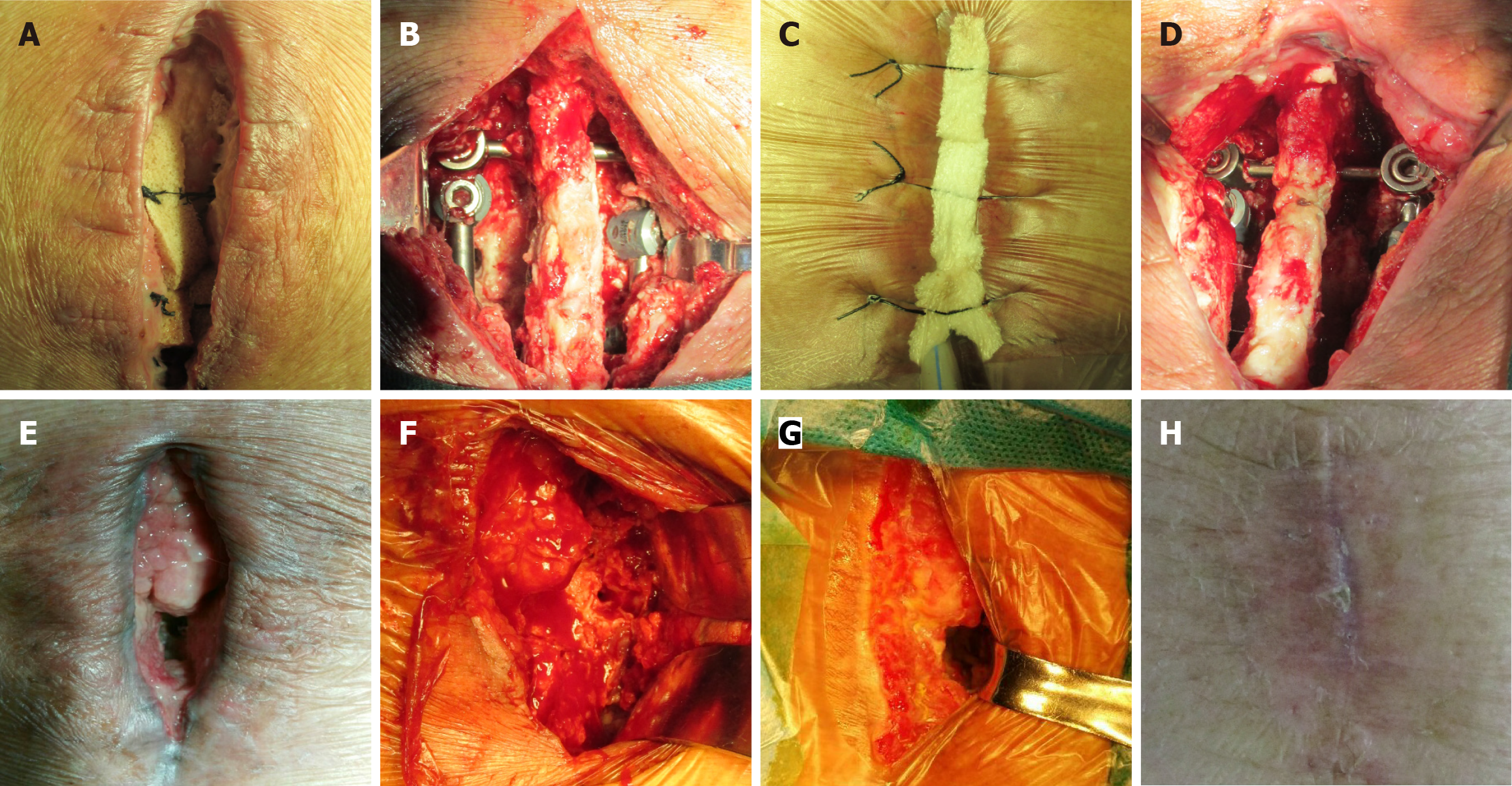
Figure 3 The treatment process for vacuum sealing drainage of the lumbar incision post-radiotherapy.
A: Initial vacuum sealing drainage (VSD); B: Fresh wound after initial VSD surgery with residual necrotic tissue; C: Sixth application of VSD; D: Fresh wound (5 weeks post-surgery); E: Healing on the left side after the eighth application of VSD, but the right side remained unhealed (7 weeks post-surgery); F: Removal of the right internal fixation (8 weeks post-surgery); G: 11th application of VSD (9 weeks post-surgery); H: Wound healing after 12th application of VSD.
- Citation: Pan JL, Xing H, Li Y, Chang ZQ. Successful treatment of a non-healing lumbar incision post-radiotherapy using vacuum sealing drainage: A case report. World J Orthop 2025; 16(11): 112307
- URL: https://www.wjgnet.com/2218-5836/full/v16/i11/112307.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i11.112307