©The Author(s) 2025.
World J Orthop. Nov 18, 2025; 16(11): 110276
Published online Nov 18, 2025. doi: 10.5312/wjo.v16.i11.110276
Published online Nov 18, 2025. doi: 10.5312/wjo.v16.i11.110276
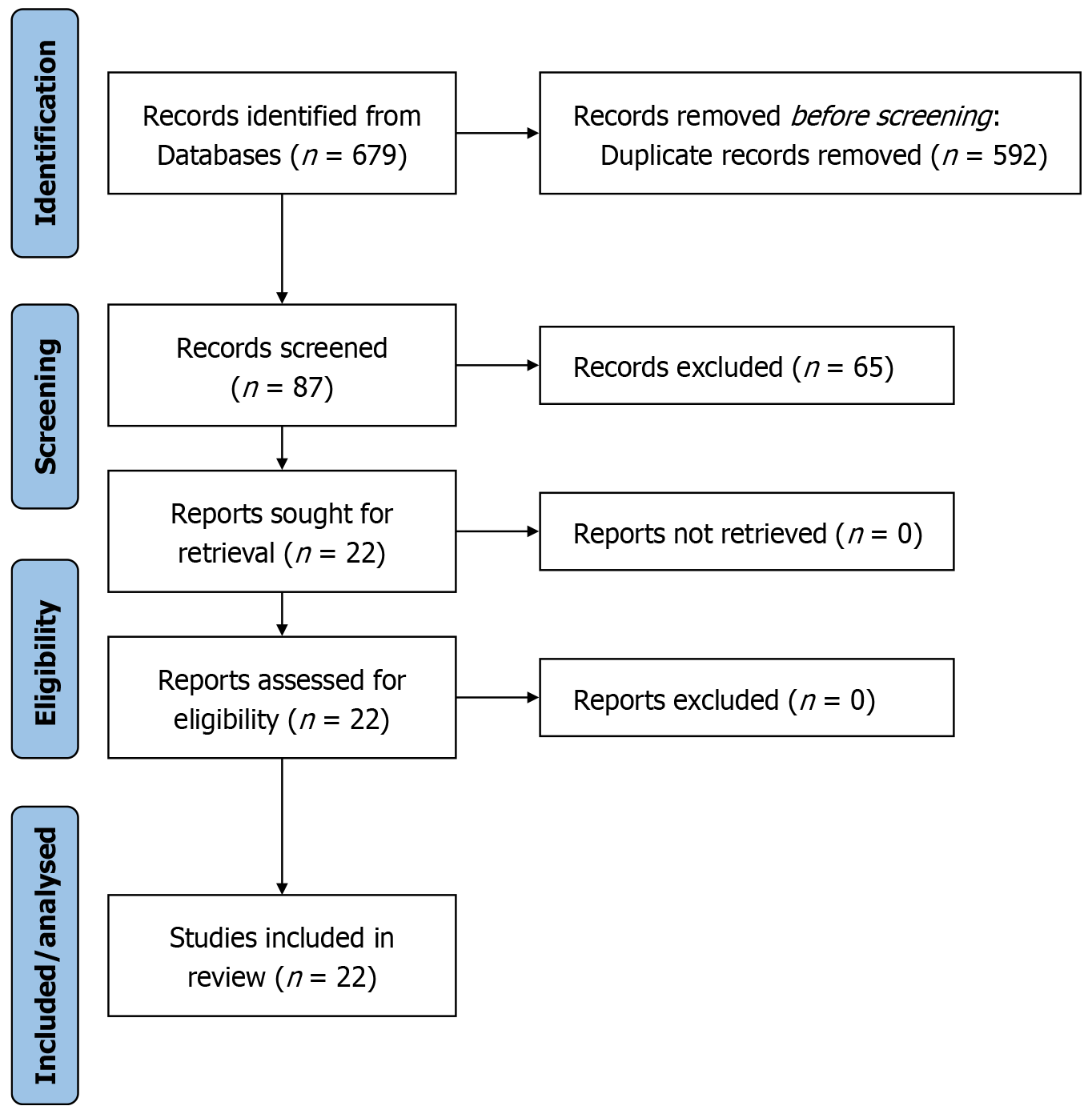
Figure 1
PRISMA flow diagram.
Figure 2 Comparative outcomes of robot-assisted vs comparator pedicle screw placement techniques.
A: Comparative accuracy of pedicle screw placement (grade A) across studies for robot-assisted (RA) vs comparator techniques. RA consistently achieved higher grade A placement rates compared to fluoroscopy-guided, freehand, or navigation-assisted approaches; B: Operative time comparisons (in minutes) between RA and comparator techniques across studies. Each pair of bars represents the mean operative times for RA and comparator groups within the same study, highlighting the trend toward slightly longer RA times due to the learning curve and robotic setup, although in some studies RA times were shorter; C: Comparison of facet joint violation (FJV) rates across studies. Each pair of bars represents the FJV rates for RA and comparator groups within each study, illustrating the consistent reduction in FJV rates with RA techniques; D: Revision rates (in%) of RA vs comparator techniques across studies. Each pair of bars represents the revision rates for RA and comparator groups within the same study. RA: Robot-assisted; FJV: Facet joint violation.
Figure 3 Forest plots of robot-assisted vs conventional lumbar interbody fusion outcomes.
A: Forest plot of screw placement accuracy (grade A) comparing robot-assisted and conventional lumbar interbody fusion techniques. Each horizontal line represents the 95% confidence interval (CI) of the odds ratio (OR) for perfect pedicle screw placement (grade A) in robot-assisted vs conventional techniques for individual studies. The black marker indicates the pooled OR estimated using a random-effects model. An OR > 1 favors robot-assisted techniques. Substantial heterogeneity was observed (I2 = 78.2%); B: Forest plot of standardized mean differences (SMD) in estimated blood loss between robot-assisted and conventional lumbar procedures. Each study presents the SMD in estimated blood loss (mL) between the robot-assisted and fluoroscopy-guided groups, with 95%CIs. A negative SMD favors the robot-assisted approach. The pooled estimate was calculated using a random-effects model; C: Forest plot of SMD in operative time between robot-assisted and conventional lumbar procedures. Each study presents the SMD in operative time (minutes), with 95%CIs. A random-effects model was used to estimate the pooled effect. An SMD of 0 indicates no difference between groups.
- Citation: Ardila CM, Ángel-Estrada S, González-Arroyave D. Robot-assisted vs conventional lumbar interbody fusion: A systematic review and meta-analysis of perioperative, radiographic, and clinical outcomes. World J Orthop 2025; 16(11): 110276
- URL: https://www.wjgnet.com/2218-5836/full/v16/i11/110276.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i11.110276