©The Author(s) 2025.
World J Orthop. Jan 18, 2025; 16(1): 102120
Published online Jan 18, 2025. doi: 10.5312/wjo.v16.i1.102120
Published online Jan 18, 2025. doi: 10.5312/wjo.v16.i1.102120
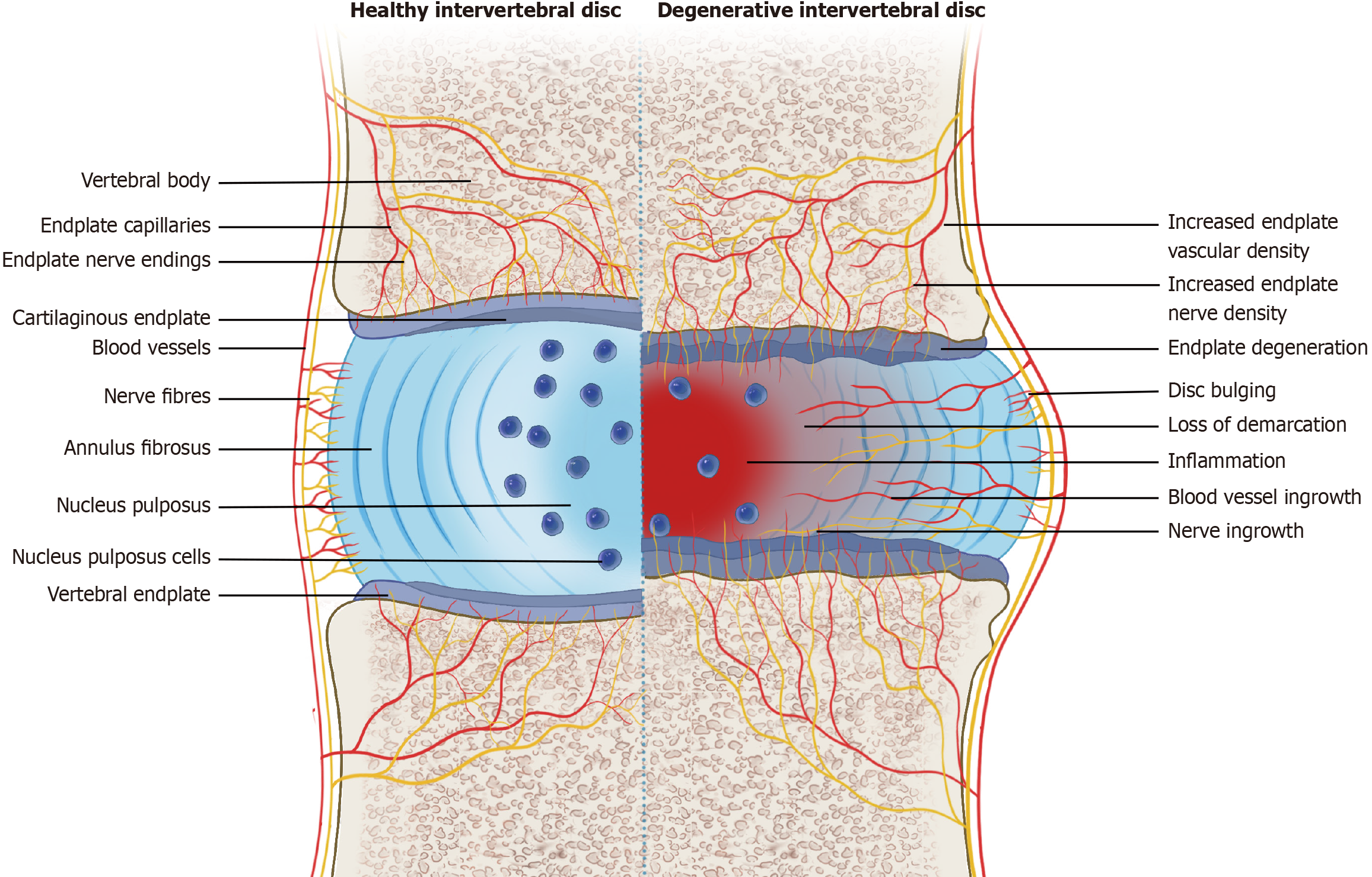
Figure 1 Schematic of a healthy disc and a degenerative disc.
A healthy disc is composed of the annulus fibrosus, nucleus pulposus, and cartilaginous endplates (left side). Nerve fibers and blood vessels are distributed only in the outer layer of the annulus fibrosus and in the vertebral endplate. A degenerative disc shows loss of border between the annulus fibrosus and nucleus pulposus, reduction of nucleus pulposus cells, and ingrowth of blood vessels and nerve fibers into the inner layer of degenerative disc (right side). There are significantly increased nerve fibers and blood vessels in the vertebral endplate.
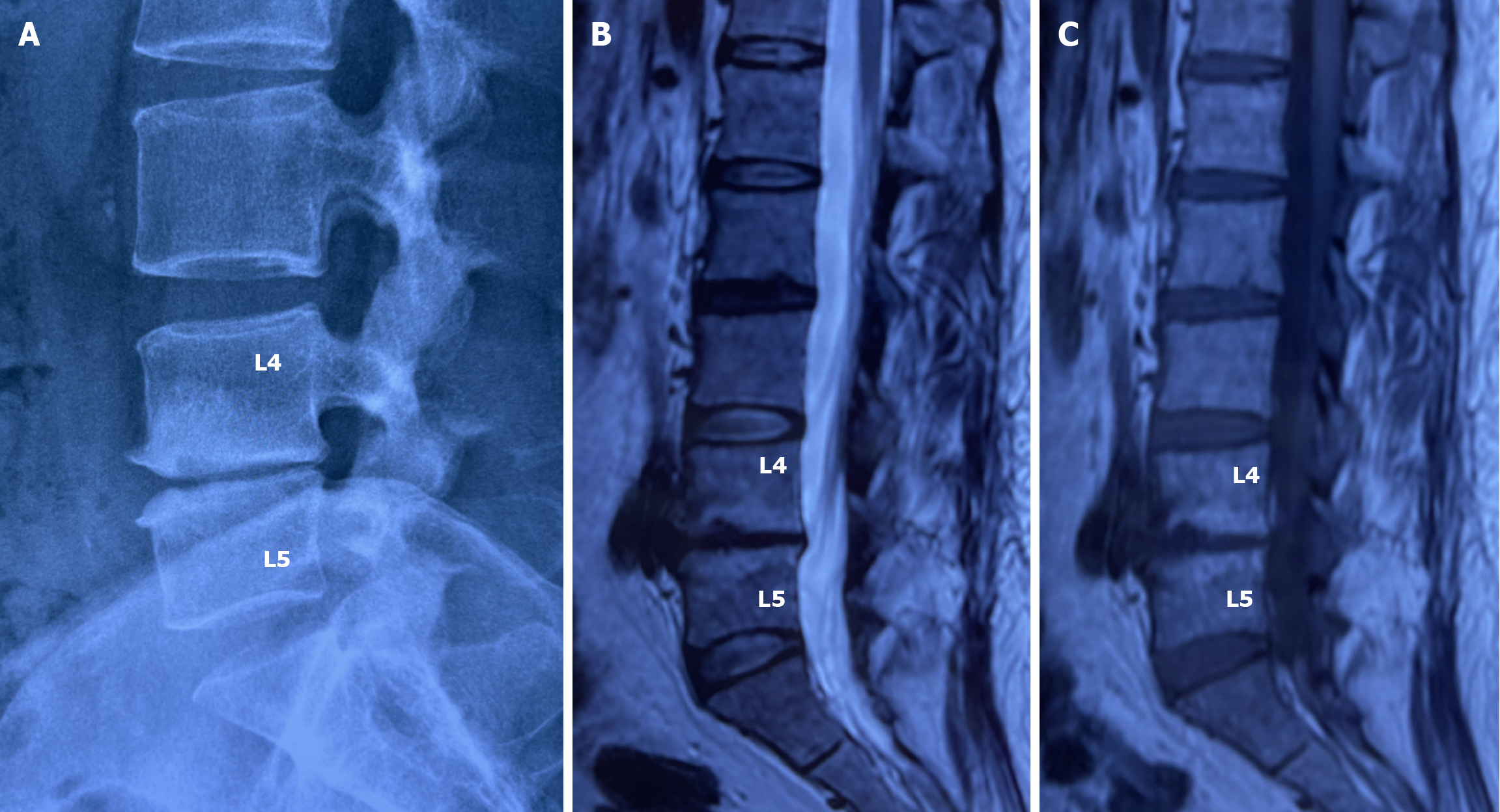
Figure 2 The relationship between severe disc degeneration and Modic changes in the endplates.
A: Lateral radiograph of the lumbar spine showed significant narrowing of the L4/5 intervertebral space, osteophyte formation at the edges of the vertebral bodies, and sclerosis of the upper and lower endplates; B and C: T2-weighted and T1-weighted magnetic resonance imaging revealed bone marrow hypersignal in the upper and lower endplates of the L4/5 disc, respectively, indicating Modic changes type 2 in the vertebral endplates (bone marrow fatty degeneration).
Figure 3 Painful intervertebral discs are always structurally ruptured.
A: Lumbar T2-weighted magnetic resonance imaging showed disc degeneration at L3/4 and L4/5 Levels (black disc), with a high-signal zone (arrow) behind each annulus fibrosus; B: Discography showed that both discs were painful discs (pain reproduction during injection of contrast agent), and the two-dimensional reconstruction of the CT scan after discography showed that the contrast agent leaked into the spinal canal from behind the L3/4 and4/5 intervertebral discs, indicating a tear in the posterior annulus fibrosus of these two intervertebral discs.
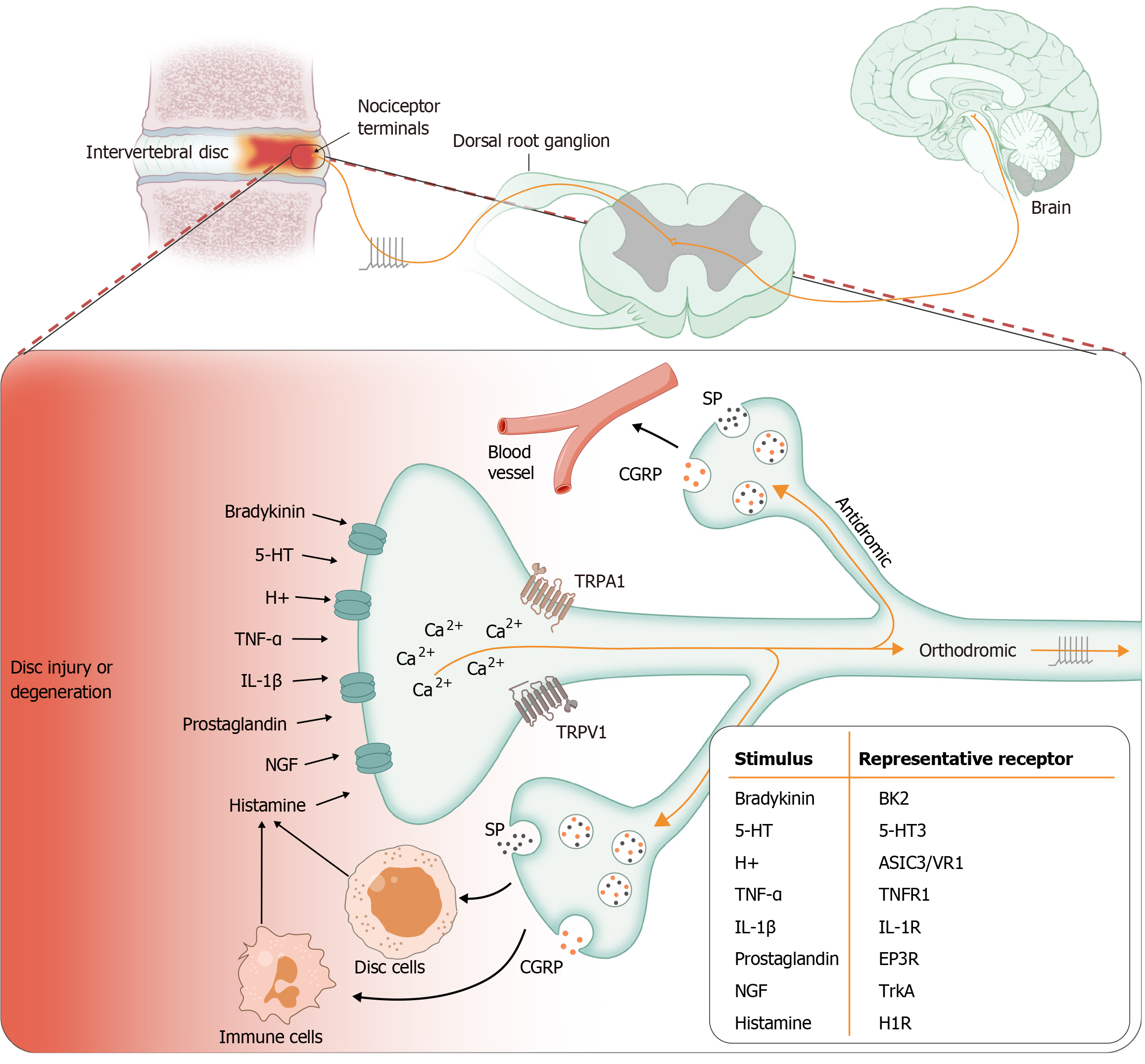
Figure 4 Schematic of the major relationship between disc degeneration and neurogenic inflammation.
Intervertebral disc injury or degeneration produces a large number of inflammatory mediators, including histamine, 5-HT, bradykinin, tumor necrosis factor-α (TNF-α), interleukin-1β (IL-1β), nerve growth factor (NGF), H+, and prostaglandins. Each of these mediators sensitizes (lowers threshold) or stimulates the terminals of nociceptors by interacting with cell surface receptors expressed by the neurons innervating disc. Activation of nociceptors not only triggers an orthodromic action potential that transmits afferent information to the dorsal horn of the spinal cord but also invades local collaterals and terminals (antidromic activity) unaffected by the original insult, thus initiating the process of neurogenic inflammation. This is an efferent function of nociceptors in which neuropeptides, particularly substance P (SP) and calcitonin gene-related peptides (CGRP), are released from the peripheral terminals to induce vasodilation and plasma extravasation as well as the activation of non-neuronal cells, including disc cells and immune cells. These cells in turn release inflammatory mediators that aggravate the inflammatory response of the disc. TrkA: Tyrosine receptor kinase A.
- Citation: Peng BG, Li YC, Yang L. Role of neurogenic inflammation in intervertebral disc degeneration. World J Orthop 2025; 16(1): 102120
- URL: https://www.wjgnet.com/2218-5836/full/v16/i1/102120.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i1.102120