Peer-review started: June 16, 2016
First decision: July 11, 2016
Revised: September 12, 2016
Accepted: November 16, 2016
Article in press: November 17, 2016
Published online: January 26, 2017
Processing time: 221 Days and 12.4 Hours
A 56-year-old man experienced an aborted sudden death followed by an arrhythmic storm. Angiography revealed a non-severe lesion on the left circumflex artery that was treated medically but an arrhythmic storm recurred. A repeat angiogram was comparable but optical coherence tomography imaging revealed a ruptured plaque with intraluminal thrombosis. Percutaneous coronary intervention was performed and no arrhythmia recurred.
Core tip: A 56-year-old man presented to a community hospital after an aborted sudden death. After initial resuscitation, he presented an arrhythmic storm with multiple episodes of ventricular fibrillation refractory to intravenous amiodarone. Coronary angiogram showed a nonobstructive intermediate lesion in the mid left circumflex artery. Because of repeated ventricular fibrillation episodes, an optical coherence tomography (OCT) was performed and revealed a ruptured thin-cap fibroatheroma with an intraluminal thrombosis at the level of the intermediate lesion. This case suggests that performing OCT to detect vulnerable culprit lesion of less than severe angiographic severity when an ischemic event is likely, such as an aborted sudden death or arrhythmic storm, may be of diagnostic value and alter therapeutic decisions.
- Citation: Couture EL, Bérubé S, Daneault B. Optical coherence tomography to identify the cause of an arrhythmic storm: A case report. World J Cardiol 2017; 9(1): 71-75
- URL: https://www.wjgnet.com/1949-8462/full/v9/i1/71.htm
- DOI: https://dx.doi.org/10.4330/wjc.v9.i1.71
Triggers for arrhythmic storms are found in a minority of them. Careful assessment is required as some causes are reversible such as myocardial ischemia. We report the first case of an arrhythmic storm where the trigger was revealed by optical coherence tomography.
A 56-year-old man known for smoking presented to a community hospital after an aborted sudden death. A witness immediately began cardiopulmonary resuscitation and the patient received 7 shocks from an automated external defibrillator prior to emergency arrival. Repeated electrocardiograms and a head CT-scan were normal. Five ventricular fibrillation (VF) episodes recurred and were treated with defibrillation and intravenous amiodarone. Given the refractory arrhythmia, the patient was transferred to our center to exclude myocardial ischemia.
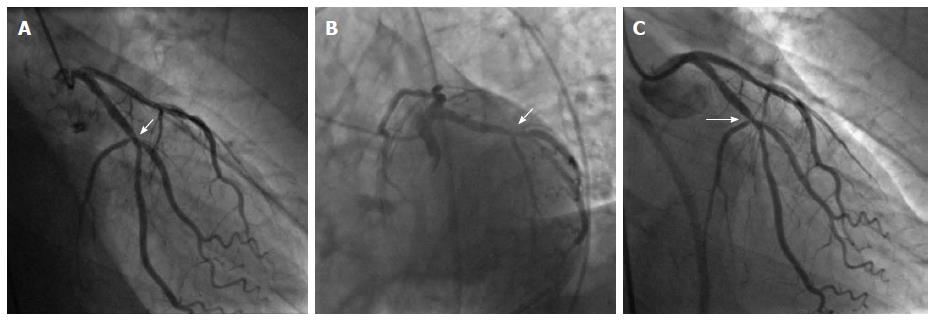
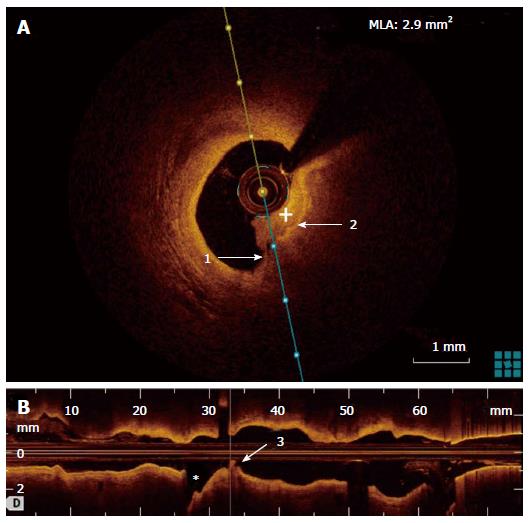
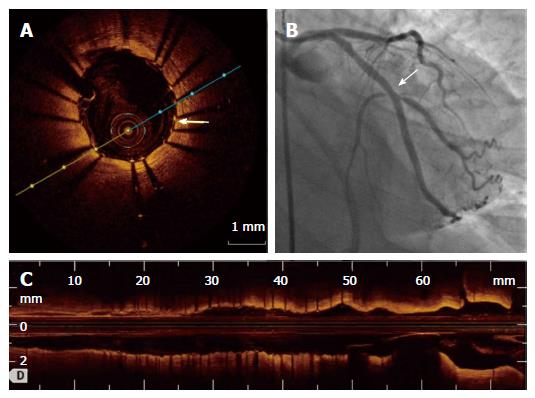
Angiogram showed an intermediate lesion (50% stenosis) on the left circumflex artery (LCX) with a TIMI grade 3 flow (Figure 1A and B). The LCX lesion was therefore not judged as the culprit and he was admitted to the intensive care unit (ICU) with a plan to performed cardiovascular magnetic resonance after therapeutic hypothermia. Initial ICU laboratories revealed a hs-TnT of 732 ng/mL as well as normal electrolytes. A transthoracic echocardiogram demonstrated diffuse hypokinesis with a left ventricular ejection fraction of 35%. Within 24 h, 10 episodes of VF recurred and were treated with defibrillation and intravenous xylocaine. Between VF episodes, electrocardiogram transiently revealed inferior and posterior ST-elevation. Emergent angiogram was repeated and was unchanged from the day prior (Figure 1C). Optical coherence tomography (OCT) imaging study was performed in the LCX. OCT revealed a ruptured thin-cap lipid-rich plaque with intraluminal thrombosis (Figure 2). Minimal lumen area was 2.9 mm2. Because of the unstable characteristics of the plaque and clinical presentation, percutaneous coronary intervention (PCI) with a drug-eluting stent was performed (Figure 3B). Adequate stent expansion and strut apposition was confirmed by OCT (Figure 3A and C). After PCI, no arrhythmia recurred and the patient was discharged home 8 d after admission without neurological deficits and without an implantable cardioverter-defibrillator. Ten months later, he is asymptomatic with no recurrent cardiovascular event.
Although coronary artery disease and especially acute coronary occlusion represent the most common cause of sudden cardiac arrest (SCD), diagnosis and treatment of the underlying mechanism remains a challenge[1]. In this case, because of the initial normal ECGs and the coronary angiogram showing a non-obstructive lesion, it was judged that this lesion did not cause active resting ischemia and therefore, was not the cause of the arrhythmia. Subsequent VF recurrences and transient ST-elevation in leads corresponding to the LCX prompted a repeat angiogram and the use of intravascular imaging. The unstable plaque characteristics revealed by OCT lead us to treat the lesion with PCI and the subsequent evolution proved that the arrhythmia’s trigger had been effectively treated.
This case is interesting for a multitude of factors. It highlights the limitation of post-resuscitation ECG for the selection of patients who could benefit from immediate coronary angiography. When initial post-resuscitation ECGs do not demonstrate ST-segment elevation or presumably new left bundle branch block, it remains controversial to proceed to immediate coronary angiography. However, as demonstrated recently in SCD survivors, a culprit lesion (defined as > 90% coronary stenosis) was found in 19% of patients presenting with no ECG signs indicating myocardial ischemia[2]. In this case, transient ST-elevation was only documented once despite continuous ECG monitoring and 22 VF episodes.
It also suggests that immediate angiography may have a central role in the management algorithm of SCD. Among initial survivors of SCD caused by VF or pulseless VT, it has been suggested that early coronary angiography was associated with higher rate of survival to discharge and favorable neurological outcome[3]. These observations are however retrospective and need to be validated in adequate trials.
Another important aspect of this case is the normal flow found in the culprit artery. In the PAMI trials, 16% of patients had TIMI 3 flow before PCI indicating spontaneous reperfusion[4]. Therefore, plaque rupture must be seen as a dynamic event as flow could be transiently occluded by thrombus with spontaneous fibrinolysis or by transient vasospasm. In this case, we supposed the arrhythmic storm was caused by multiple transient occlusive coronary spasms triggered by the plaque rupture. This phenomenon increases the difficulty in identifying ischemic causes of SCD and culprit lesion when ECGs are normal. This case demonstrated the additive value of OCT to further stratify intermediate non-obstructive lesion when an ischemic event is likely. Intravascular ultrasound (IVUS) also have been reported to revealed culprit lesion in SCD[5]. In a study of 12 survivors of SCD and high probability of coronary artery disease who underwent cardiac catheterization, 4 of them showed non-obstructive lesion a (< 50% stenosis and TIMI 3 flow) but all had intraluminal thrombosis revealed by intravascular ultrasound. However, none of the previous reports were accompanied by a such an arrhythmic storm[5,6]. Moreover, to rule out plaque rupture in survivors of SCD with non-obstructive intermediate lesion, OCT own a potential advantage over IVUS given its higher spatial resolution. Other modality such as near infrared spectroscopy could be of value in the future[7,8].
The optimal treatment of unstable plaque with adequate residual lumen area is however uncertain. Prior reports suggest that medical management could be adequate in these circumstances[9]. However, in our case, PCI clearly was of additional value to medical therapy. With the evolution of drug eluting stents and especially bioresorbable vascular scaffold, these technologies may impact the treatment of vulnerable lesions in the future. Large trials will be needed to evaluate the optimal diagnostic modalities and treatments for these unstable lesions.
In conclusion, this case suggests that performing OCT to detect vulnerable culprit lesion of less than severe angiographic severity when an ischemic event is likely, such as an aborted sudden death or arrhythmic storm, may be of diagnostic value and alter therapeutic decisions.
A 56-year-old man known for smoking presented to a community hospital after an aborted sudden death.
Arrhythmic storm (ventricular fibrillation) episodes refractory to intravenous amiodarone.
Ischemic secondary to acute coronary syndrome, electrolytes abnormalities, primary cardiomyopathy.
Electrolytes were all normal at intensive care unit arrival, but hs-TnT was elevated.
Coronary angiogram showed a nonobstructive intermediate lesion in the mid left circumflex artery. Optical coherence tomography (OCT) revealed ruptured thin-cap fibroatheroma with an intraluminal thrombosis at the level of an angiographic intermediate lesion in the mid left circumflex artery.
Acute coronary syndrome with a plaque rupture.
Percutaneous coronary intervention with a drug-eluting stent.
Very few cases of sudden death caused by a plaque rupture only detected with intravascular imaging have been described but never with a so dramatic presentation as in this case.
OCT is an intravascular imaging modality that uses light to capture micrometer-resolution, three-dimensional images from within optical scattering media (e.g., coronary artery). Spatial resolution is between 2-10 μm and his penetration varied between 1-10 mm.
This case suggests that performing optical coherence tomography to detect vulnerable culprit lesion of less than severe angiographic severity when an ischemic event is likely, such as an aborted sudden death or arrhythmic storm, may be of diagnostic value and alter therapeutic decisions.
The paper is well written.
| 1. | Zipes DP, Camm AJ, Borggrefe M, Buxton AE, Chaitman B, Fromer M, Gregoratos G, Klein G, Moss AJ, Myerburg RJ. ACC/AHA/ESC 2006 Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (writing committee to develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006;114:e385-e484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 922] [Cited by in RCA: 816] [Article Influence: 40.8] [Reference Citation Analysis (0)] |
| 2. | Stær-Jensen H, Nakstad ER, Fossum E, Mangschau A, Eritsland J, Drægni T, Jacobsen D, Sunde K, Andersen GØ. Post-Resuscitation ECG for Selection of Patients for Immediate Coronary Angiography in Out-of-Hospital Cardiac Arrest. Circ Cardiovasc Interv. 2015;8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 64] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 3. | Vyas A, Chan PS, Cram P, Nallamothu BK, McNally B, Girotra S. Early Coronary Angiography and Survival After Out-of-Hospital Cardiac Arrest. Circ Cardiovasc Interv. 2015;8:pii: e002321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 79] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 4. | Stone GW, Cox D, Garcia E, Brodie BR, Morice MC, Griffin J, Mattos L, Lansky AJ, O’Neill WW, Grines CL. Normal flow (TIMI-3) before mechanical reperfusion therapy is an independent determinant of survival in acute myocardial infarction: analysis from the primary angioplasty in myocardial infarction trials. Circulation. 2001;104:636-641. [PubMed] |
| 5. | Quintanilla J, Avila C, Meraz M, Jerjes-Sanchez C, de la Peña-Almaguer E, Diaz-Cid A, Sanchez L, Trevino AR, Perez LC. The role of a multimodality imaging approach in diagnosis and stratification of aborted sudden cardiac death. Can J Cardiol. 2015;31:103.e9-103.e11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Sánchez-Recalde A, Merino JL, Moreno R, Jiménez-Valero S, Galeote G, Calvo L, López de Sá E, López-Sendón JL. Clinical implications of intracoronary findings beyond coronary angiograms in patients with sudden death and high probability of coronary artery disease. Rev Esp Cardiol. 2011;64:819-823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Madder RD, Goldstein JA, Madden SP, Puri R, Wolski K, Hendricks M, Sum ST, Kini A, Sharma S, Rizik D. Detection by near-infrared spectroscopy of large lipid core plaques at culprit sites in patients with acute ST-segment elevation myocardial infarction. JACC Cardiovasc Interv. 2013;6:838-846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 160] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 8. | Madder RD, Husaini M, Davis AT, VanOosterhout S, Khan M, Wohns D, McNamara RF, Wolschleger K, Gribar J, Collins JS. Large lipid-rich coronary plaques detected by near-infrared spectroscopy at non-stented sites in the target artery identify patients likely to experience future major adverse cardiovascular events. Eur Heart J Cardiovasc Imaging. 2016;17:393-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 76] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 9. | Hong MK, Mintz GS, Lee CW, Suh IW, Hwang ES, Jeong YH, Park DW, Kim YH, Han KH, Cheong SS. Serial intravascular ultrasound evidence of both plaque stabilization and lesion progression in patients with ruptured coronary plaques: effects of statin therapy on ruptured coronary plaque. Atherosclerosis. 2007;191:107-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 28] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: Canada
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Chang ST, De Ponti R, Teragawa H, Ueda H S- Editor: Qiu S L- Editor: A E- Editor: Wu HL