Published online Aug 26, 2015. doi: 10.4330/wjc.v7.i8.476
Peer-review started: December 1, 2014
First decision: December 26, 2014
Revised: February 9, 2015
Accepted: June 15, 2015
Article in press: June 16, 2015
Published online: August 26, 2015
Processing time: 270 Days and 17.9 Hours
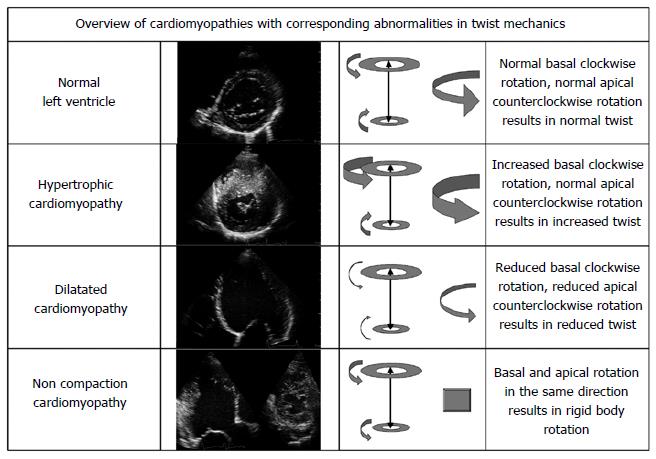
Left ventricular twist is an essential part of left ventricular function. Nevertheless, knowledge is limited in “the cardiology community” as it comes to twist mechanics. Fortunately the development of speckle tracking echocardiography, allowing accurate, reproducible and rapid bedside assessment of left ventricular twist, has boosted the interest in this important mechanical aspect of left ventricular deformation. Although the fundamental physiological role of left ventricular twist is undisputable, the clinical relevance of assessment of left ventricular twist in cardiomyopathies still needs to be established. The fact remains; analysis of left ventricular twist mechanics has already provided substantial pathophysiological understanding on a comprehensive variety of cardiomyopathies. It has become clear that increased left ventricular twist in for example hypertrophic cardiomyopathy may be an early sign of subendocardial (microvascular) dysfunction. Furthermore, decreased left ventricular twist may be caused by left ventricular dilatation or an extensive myocardial scar. Finally, the detection of left ventricular rigid body rotation in noncompaction cardiomyopathy may provide an indispensible method to objectively confirm this difficult diagnosis. All this endorses the value of left ventricular twist in the field of cardiomyopathies and may further encourage the implementation of left ventricular twist parameters in the “diagnostic toolbox” for cardiomyopathies.
Core tip: Left ventricular twist is an essential part of left ventricular function. Nevertheless, knowledge is limited in “the cardiology community” as it comes to twist mechanics. It has become clear that increased left ventricular twist in for example hypertrophic cardiomyopathy may be an early sign of subendocardial (microvascular) dysfunction. Furthermore, decreased left ventricular twist may be caused by left ventricular dilatation or an extensive myocardial scar. Finally, the detection of left ventricular rigid body rotation in noncompaction cardiomyopathy may provide an indispensible method to objectively confirm this difficult diagnosis. All this endorses the value of left ventricular twist in the field of cardiomyopathies and may further encourage the implementation of left ventricular twist parameters in the “diagnostic toolbox” for cardiomyopathies.
- Citation: Kauer F, Geleijnse ML, Dalen BMV. Role of left ventricular twist mechanics in cardiomyopathies, dance of the helices. World J Cardiol 2015; 7(8): 476-482
- URL: https://www.wjgnet.com/1949-8462/full/v7/i8/476.htm
- DOI: https://dx.doi.org/10.4330/wjc.v7.i8.476
As early as the 16th century Leonardo da Vinci[1,2] wrote about the twisting deformation of the heart and Richard Lower compared the myocardial contraction with “the wringing of a linen cloth to squeeze out the water” in his observations of myocardial contraction in 1669[3,4]. A complex spiral architecture is the mechanical basis for this wringing motion[5,6]. The left ventricle comprises of obliquely orientated multiple layers of cardiomyocytes, transforming from a subendocardially located (smaller-radius) right-handed helix to a subepicardial (larger-radius) left-handed helix.
This helix generates a torsional motion pattern caused by rotation in a clockwise direction (as seen from the apex) at the level of the mitral valve (basal level) and counter clockwise rotation of the apex (apical level). This twisting deformation performs a fundamental part in the mechanical efficiency of the heart resulting in a 60% ejection fraction with only 15% fibre shortening[7]. Furthermore, left ventricular untwisting is essential in actively aiding diastolic filling[8]. The physiology of left ventricular twist and changes of left ventricular twist in different cardiomyopathies are reviewed in this paper.
By his first description of left ventricular twist, Leonardo da Vinci[1,2] has been a constant inspiration for scientists in their pursuit to comprehend the functioning of the human heart. Nevertheless, reliable quantitative measurement of left ventricular twist in a non-invasive manner has not been possible until recently.
Speckle tracking echocardiography is based on automated tracking of a specific portion of myocardial tissue being visualized by a pattern of gray values, a speckle pattern, on an ultrasound image. These gray values are the result of the analysis of the reflection of ultrasound interfering with the myocardial tissue. Therefore, movement of speckle patterns represent motion of myocardial tissue[9].
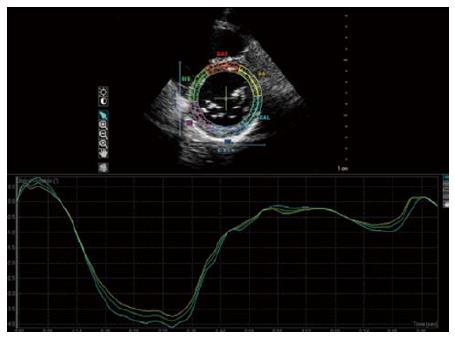
In case a of suitably high frame rate, the pattern of speckles is conserved from frame to frame[10]. By following a specific pattern of speckles, the motion of the corresponding myocardial segment can be tracked, thus allowing to quantify deformation of the myocardium and, as a function of time, deformation rate (Figure 1). Several validation studies[11,12] showed good correlation between left ventricular twist assessment by commercially available speckle tracking software and magnetic resonance imaging. Also, speckle tracking derived left ventricular twist has been shown to be feasible and reproducible, and may thereby be used as a method to follow-up patients[13].
After the first description of left ventricular twist by Da Vinci, it lasted until the late 1960s before a more detailed description of twist was provided by Streeter et al[5] in a study of post-mortem canine hearts. Generally, myofibre position changes gradually from +60 degrees (circumferential axis as a reference) subendocardially to -60 degrees at the subepicardium. The counter coiled helix of subepi - and subendocardial fibres generates twist. The direction of basal and apical rotation is dominated by the larger - radius fibres at the subepicardium, caused by their longer arm of movement[14]. The significance of the direction of fibres has been demonstrated in patient studies as well[15]. Left ventricular twist showed a linear relation with sphericity index (as a measure of change in left ventricle fibre orientation, because in more spherically shaped hearts fibres are supposed to be oriented more horizontally) in patients with a dilated cardiomyopathy, supporting the hypothesis on twist mechanics and the influence of the direction of fibres on the twisting left ventricular deformation[14].
The influence of aging on twist was studied by several groups[16-19]. In all these studies, aging appeared to be related to an increase of left ventricular twist. As the function of the fibres at the subendocardium deteriorates when getting older, even in normal hearts[20,21], the reduction of the opposing rotational forces of the subendocardium will result in an increase of apical rotation by the already dominant subepicardial fibres and consequently in an increase of left ventricular twist. This increase of left ventricular twist appears to be a part of “physiological cardiac aging”. One may hypothesize that this increase of twist contributes to the conservation of left ventricular stroke volume with ageing.
Untwisting begins after left ventricular twist reaches its peak, usually shortly before end-systole. Systolic twisting leads to storage of potential energy in the compressed coil of twisted fibres of the left ventricular wall[19]. During isovolemic relaxation this coil springs open and releases this energy. Fibres at the subepicardium that are still depolarized and are at that time - in contrast to systole - not overruled by active contraction of the fibres located at the subepicardium, might dynamically reinforce this role of untwisting in diastole[19,22]. It was shown by magnetic resonance imaging that there is an important dissociation of time of untwist and filling, approximately 40% of the untwist takes place during isovolumic relaxation[23]. Furthermore, the extent of the diastolic intraventricular pressure gradient is strongly related to untwisting. Even more so, untwist precedes the development of this pressure gradient, thereby potentially being an important indicator of suction during early diastole[24,25].
Left ventricular twist in patients with hypertrophic cardiomyopathy is moderately increased, in particular the left ventricular basal rotation[26-29]. This augmented rotation at mitral valve level is probably caused by reduced counteraction of the subendocardial fibres, due to subendocardial ischemia caused by endocardial microvascular insufficiency and increased oxygen demand[30,31]. This is supported by the phenomenon of increased rotation being most pronounced in the hypertrophic segments[26]. A larger difference in radius between the subepicardium and subendocardium will increase the arm of effect on the already dominant fibres of the subepicardium and consequently will increase rotation at mitral valve level (basal rotation)[26].
There is a significant relation between the pattern of hypertrophy on apical rotation and twist. If the septum has a sigmoid curvature, rotation of the apex is more pronounced than in reverse septal curvature hearts. Outflow tract obstruction is more common in patients in whom the septum has a sigmoid curvature. The resulting intraventricular forces from these outflow tract gradients can lead to microvascular insufficiency and thereby to more (sub)endocardial ischemia. Subsequently, this lack of oxygen might cause impairment of the countereffect of contraction of the subendocardially located myocardial fibres on left ventricular twist.
The necessity to objectively demonstrate diastolic dysfunction in hypertrophic cardiomyopathy has caused an ongoing pursuit for a non invasive and load independent technique for quantifying the severity of diastolic dysfunction. For instance Takeuchi et al[32] examined the effect of left ventricular hypertrophy in hypertensive patients on untwisting of the left ventricle. In moderate to severe hypertrophy, untwisting was reduced and delayed as compared to healthy individuals, supposedly resulting in decreased function of left ventricular diastole. In hypertrophic cardiomyopathy[33] and also in aortic stenosis[34] the untwisting rate, being the mean untwisting velocity during the isovolumic relaxation phase, is decreased and as a result untwisting is delayed[27]. In hypertrophic cardiomyopathy this was most obvious in the affected segments[27,29]. Also, compromised elastic characteristics lead to suboptimal transformation of the potential kinetic energy stored in the twisted heart. Peak diastolic untwisting velocity is reduced in hypertrophic cardiomyopathy whereas it is augmented in aortic stenosis. In aortic stenosis twist is increased more severe. Release of the relatively high amount of potential energy results in increased untwisting, possibly compensating for otherwise diastolic dysfunction[27,35]. In hypertrophic cardiomyopathy twist is just discreetly increased, weakening this effect[27,33].
Twist in non-ischaemic dilated left ventricles is known to be reduced. The abnormal shape of the left ventricle in dilated cardiomyopathy may cause a change in fibre orientation. This fibre orientation is of importance in left ventricular twist as described earlier. This influence was found as an independent linear relation between left ventricular sphericity index and peak systolic twist. The more dilated the left ventricle, the more decreased the left ventricular twist. Actually, also in patients with dilated cardiomyopathy and comparable left ventricular ejection fraction, sphericity index was still significantly related to left ventricular twist[15]. Nonetheless, derangement of myocardial fibre architecture is not the only cause for decreased left ventricular twist in patients with non-ischaemic dilated cardiomyopathy as fibrosis appeared to play a role in decreased left ventricular twist.
The extent of myocardial fibrosis in dilated cardiomyopathy has been evaluated by cardiac magnetic resonance imaging with late gadolinium enhancement. Fibrosis proved to be related to twist[36]. Reduction of twist indicated more extensive cardiac fibrosis.
As explained earlier, very rapid left ventricular untwisting is known to play a prominent part in fast filling in early diastole. However, in dilated hearts untwisting is delayed, leading to an apex-to-base-rotation delay. This will interfere with early diastolic suction and might harm filling of the left ventricle in dilated cardiomyopathy[27,37,38].
Noncompaction cardiomyopathy is still subject to debate because of the shortcoming on consensus on its pathogenesis, diagnosis and treatment[39-41].
In the final embryonic development of the heart the myocardial tissue is transformed in a compact myocardium together with the formation of epicardial and endocardial fibre as oppositely wound helices[6,42]. As noncompaction cardiomyopathy is supposed to be caused by intrauterine arrest of cardiac embryogenesis during this transformation[43], distorted left ventricular twist features may be expected, even more than in the situation of reduced systolic function and a normally compacted myocardium. This was recognised in clinical studies[44-48] where noncompaction cardiomyopathy patients displayed a twist pattern with basal and apical rotation in the same direction, resulting in almost full absence of left ventricular twist. This rotation pattern is known as left ventricular rigid body rotation[44,49]. Rigid body rotation demonstrated, in a relative large study, to have a good predictive value for the diagnosis of noncompaction cardiomyopathy[47]. Even more interesting, all familial noncompaction cardiomyopathy patients showed rigid body rotation. The fact that noncompaction cardiomyopathy diagnosis is most definite in these patients underscores the good sensitivity of rigid body rotation in diagnosing noncompaction cardiomyopathy.
The clinical importance of left ventricular rigid body rotation was shown in more recent studies, where rigid body rotation was found in a majority of noncompaction cardiomyopathy patients as well[50,51], but the patients with rigid body rotation and noncompaction cardiomyopathy proved to have a lower NYHA functional status as compared to the patients without rigid body rotation[48].
An optical device attached to the apex was used in a canine model to study the early effects of myocardial ischemia[52]. Ischemia was inflicted by occluding the anterior descending coronary artery. Early after induction of ischemia, there was a paradoxical increase of apical rotation. This finding was ascribed to secluded ischemia of the subendocardium, resulting in a declined counteractive effect of the fibres located at the subendocardium[27,52].
Also, Moen et al[53] used speckle-tracking echocardiography on eight anesthetized pigs to define regional myocardial function in anterior wall ischemia. They discovered left ventricular twist remained normal until there was extensive impairment of perfusion of the left anterior descending artery.
Sun et al[54] induced a myocardial infarction in 7 pigs, leading to decreased twist, specifically in the area perfused by the occluded coronary artery[27,54]. Hence, it was suggested that twist might be used to assess wall motion abnormalities in order to localize cardiac ischemia. Conversely, in a clinical study using dobutamine stress echo in 125 patients with myocardial infarction or ischemia, the influence of myocardial infarction on left ventricular twist proved to be related to size rather than localisation of infarction. In addition, stress-induced myocardial ischemia did not influence left ventricular twist[55]. Other studies on anterior myocardial infarction patients showed a decreased apical rotation in the infarcted left ventricle however with a preserved left ventricular basal rotation[56,57].
When left ventricular myocardial infarction was complicated by left ventricular aneurysm formation, rotation of the apex was lost or even reversed, consequently losing left ventricular twist. Restorative surgery as a treatment of this problem is rather complex: the aim is to reconstruct a near normal ventricular chamber after aneurysm formation and thus reducing left ventricular volume and improving ejection fraction[58]. Setser et al[59] did not see a significant improvement in their patients left ventricular twist after traditional left ventricular reconstruction. Much more interesting however; when an improved restoration technique was used, where residual myocardium around the defect was re-approached endeavouring to redirect fibre orientation displaced by infarct scar toward a more physiological gross disposition, left ventricular twist did improve in all patients[60]. This encouraging concept of fibre orientation based surgical reparative surgery, could expand the potential of repairing the failing heart.
Left ventricular twist is an essential part of left ventricular function. Nevertheless, knowledge is limited in “the cardiology community” as it comes to twist mechanics.
Fortunately, evolution of echocardiography, permitting speckle tracking to precisely assess left ventricular twist, has boosted the awareness of this fundamental feature of cardiac mechanics. The vital role of twist in the physiology of the heart is undisputable. Nevertheless, the significance of twist assessment in daily clinical practice in patients with a cardiomyopathy still has to be established[27]. On the other hand, twist analysis has contributed substantially to the understanding of pathophysiology in a diversity of cardiomyopathies (Figure 2). Increased twist in for example hypertrophic cardiomyopathy may be an early sign of subendocardial (microvascular) dysfunction. Furthermore, decreased twist might be initiated by left ventricular dilatation or an extensive myocardial scar. Finally, the detection of rigid body rotation in noncompaction cardiomyopathy could serve as an indispensible method to accurately diagnose this challenging entity. All this highlights the importance of left ventricular twist in the field of cardiomyopathies and may further encourage the implementation of left ventricular twist parameters in the “diagnostic toolbox” for cardiomyopathies[27].
| 1. | Keele KD. Leonardo da Vinci’s elements of the science of man. New York, USA: Academic Press 1983; . |
| 2. | Da Vinci L. Quoted by Evans l. Starling’s Principles of Human Physiology. London, UK: J.A. Churchill 1936; 706. |
| 3. | Lower R. Tractus de corde. Early Science in Oxford. Oxford, London, UK: Sawsons, Pall Mall 1968; 1169. |
| 4. | Geleijnse ML, van Dalen BM. Let’s twist. Eur J Echocardiogr. 2009;10:46-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Streeter DD, Spotnitz HM, Patel DP, Ross J, Sonnenblick EH. Fiber orientation in the canine left ventricle during diastole and systole. Circ Res. 1969;24:339-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1057] [Cited by in RCA: 984] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 6. | Greenbaum RA, Ho SY, Gibson DG, Becker AE, Anderson RH. Left ventricular fibre architecture in man. Br Heart J. 1981;45:248-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 760] [Cited by in RCA: 785] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 7. | Sallin EA. Fiber orientation and ejection fraction in the human left ventricle. Biophys J. 1969;9:954-964. [PubMed] |
| 8. | Notomi Y, Martin-Miklovic MG, Oryszak SJ, Shiota T, Deserranno D, Popovic ZB, Garcia MJ, Greenberg NL, Thomas JD. Enhanced ventricular untwisting during exercise: a mechanistic manifestation of elastic recoil described by Doppler tissue imaging. Circulation. 2006;113:2524-2533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 300] [Cited by in RCA: 285] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 9. | D’hooge J. Principles and Different Techniques for Speckle Tracking, in Myocardial Imaging: Tissue Doppler and Speckle Tracking. Marwick TH, Yu CM, Sun JP, editors. Oxford, UK: Blackwell Publishing Ltd 2007; . [DOI] [Full Text] |
| 10. | Ramamurthy BS, Trahey GE. Potential and limitations of angle-independent flow detection algorithms using radio-frequency and detected echo signals. Ultrason Imaging. 1991;13:252-268. [PubMed] [DOI] [Full Text] |
| 11. | Notomi Y, Lysyansky P, Setser RM, Shiota T, Popović ZB, Martin-Miklovic MG, Weaver JA, Oryszak SJ, Greenberg NL, White RD. Measurement of ventricular torsion by two-dimensional ultrasound speckle tracking imaging. J Am Coll Cardiol. 2005;45:2034-2041. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 566] [Cited by in RCA: 547] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 12. | Helle-Valle T, Crosby J, Edvardsen T, Lyseggen E, Amundsen BH, Smith HJ, Rosen BD, Lima JA, Torp H, Ihlen H. New noninvasive method for assessment of left ventricular rotation: speckle tracking echocardiography. Circulation. 2005;112:3149-3156. [PubMed] |
| 13. | van Dalen BM, Soliman OI, Vletter WB, Kauer F, van der Zwaan HB, ten Cate FJ, Geleijnse ML. Feasibility and reproducibility of left ventricular rotation parameters measured by speckle tracking echocardiography. Eur J Echocardiogr. 2009;10:669-676. [PubMed] |
| 14. | Taber LA, Yang M, Podszus WW. Mechanics of ventricular torsion. J Biomech. 1996;29:745-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 167] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 15. | van Dalen BM, Kauer F, Vletter WB, Soliman OI, van der Zwaan HB, Ten Cate FJ, Geleijnse ML. Influence of cardiac shape on left ventricular twist. J Appl Physiol (1985). 2010;108:146-151. [PubMed] |
| 16. | Nakai H, Takeuchi M, Nishikage T, Kokumai M, Otani S, Lang RM. Effect of aging on twist-displacement loop by 2-dimensional speckle tracking imaging. J Am Soc Echocardiogr. 2006;19:880-885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 57] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 17. | Takeuchi M, Nakai H, Kokumai M, Nishikage T, Otani S, Lang RM. Age-related changes in left ventricular twist assessed by two-dimensional speckle-tracking imaging. J Am Soc Echocardiogr. 2006;19:1077-1084. [PubMed] |
| 18. | van Dalen BM, Soliman OI, Vletter WB, ten Cate FJ, Geleijnse ML. Age-related changes in the biomechanics of left ventricular twist measured by speckle tracking echocardiography. Am J Physiol Heart Circ Physiol. 2008;295:H1705-H1711. [PubMed] |
| 19. | van Dalen BM, Soliman OI, Kauer F, Vletter WB, Zwaan HB, Cate FJ, Geleijnse ML. Alterations in left ventricular untwisting with ageing. Circ J. 2010;74:101-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Lumens J, Delhaas T, Arts T, Cowan BR, Young AA. Impaired subendocardial contractile myofiber function in asymptomatic aged humans, as detected using MRI. Am J Physiol Heart Circ Physiol. 2006;291:H1573-H1579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 127] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 21. | Nikitin NP, Witte KK, Thackray SD, de Silva R, Clark AL, Cleland JG. Longitudinal ventricular function: normal values of atrioventricular annular and myocardial velocities measured with quantitative two-dimensional color Doppler tissue imaging. J Am Soc Echocardiogr. 2003;16:906-921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 193] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 22. | Ashikaga H, Criscione JC, Omens JH, Covell JW, Ingels NB. Transmural left ventricular mechanics underlying torsional recoil during relaxation. Am J Physiol Heart Circ Physiol. 2004;286:H640-H647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 114] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 23. | Rademakers FE, Buchalter MB, Rogers WJ, Zerhouni EA, Weisfeldt ML, Weiss JL, Shapiro EP. Dissociation between left ventricular untwisting and filling. Accentuation by catecholamines. Circulation. 1992;85:1572-1581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 231] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 24. | Notomi Y, Popovic ZB, Yamada H, Wallick DW, Martin MG, Oryszak SJ, Shiota T, Greenberg NL, Thomas JD. Ventricular untwisting: a temporal link between left ventricular relaxation and suction. Am J Physiol Heart Circ Physiol. 2008;294:H505-H513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 232] [Cited by in RCA: 240] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 25. | van Dalen BM, Soliman OI, Vletter WB, ten Cate FJ, Geleijnse ML. Insights into left ventricular function from the time course of regional and global rotation by speckle tracking echocardiography. Echocardiography. 2009;26:371-377. [PubMed] |
| 26. | Kauer F, van Dalen BM, Soliman OI, van der Zwaan HB, Vletter WB, Schinkel AF, ten Cate FJ, Geleijnse ML. Regional left ventricular rotation and back-rotation in patients with reverse septal curvature hypertrophic cardiomyopathy. Eur Heart J Cardiovasc Imaging. 2013;14:435-442. [PubMed] |
| 27. | van Dalen BM, Geleijnse ML. Left Ventricular Twist in Cardiomyopathy, Cardiomyopathies. Milei J, editor. InTech. Oxford, UK: Blackwell Publishing Ltd 2013; . [DOI] [Full Text] |
| 28. | Young AA, Kramer CM, Ferrari VA, Axel L, Reichek N. Three-dimensional left ventricular deformation in hypertrophic cardiomyopathy. Circulation. 1994;90:854-867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 308] [Cited by in RCA: 278] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 29. | van Dalen BM, Kauer F, Soliman OI, Vletter WB, Michels M, ten Cate FJ, Geleijnse ML. Influence of the pattern of hypertrophy on left ventricular twist in hypertrophic cardiomyopathy. Heart. 2009;95:657-661. [PubMed] |
| 30. | Cecchi F, Olivotto I, Gistri R, Lorenzoni R, Chiriatti G, Camici PG. Coronary microvascular dysfunction and prognosis in hypertrophic cardiomyopathy. N Engl J Med. 2003;349:1027-1035. [PubMed] [DOI] [Full Text] |
| 31. | Soliman OI, Geleijnse ML, Michels M, Dijkmans PA, Nemes A, van Dalen BM, Vletter WB, Serruys PW, ten Cate FJ. Effect of successful alcohol septal ablation on microvascular function in patients with obstructive hypertrophic cardiomyopathy. Am J Cardiol. 2008;101:1321-1327. [PubMed] |
| 32. | Takeuchi M, Borden WB, Nakai H, Nishikage T, Kokumai M, Nagakura T, Otani S, Lang RM. Reduced and delayed untwisting of the left ventricle in patients with hypertension and left ventricular hypertrophy: a study using two-dimensional speckle tracking imaging. Eur Heart J. 2007;28:2756-2762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 143] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 33. | van Dalen BM, Kauer F, Michels M, Soliman OI, Vletter WB, van der Zwaan HB, ten Cate FJ, Geleijnse ML. Delayed left ventricular untwisting in hypertrophic cardiomyopathy. J Am Soc Echocardiogr. 2009;22:1320-1326. [PubMed] |
| 34. | van Dalen BM, Tzikas A, Soliman OI, Heuvelman HJ, Vletter WB, Ten Cate FJ, Geleijnse ML. Assessment of subendocardial contractile function in aortic stenosis: a study using speckle tracking echocardiography. Echocardiography. 2013;30:293-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 35. | van Dalen BM, Tzikas A, Soliman OI, Kauer F, Heuvelman HJ, Vletter WB, ten Cate FJ, Geleijnse ML. Left ventricular twist and untwist in aortic stenosis. Int J Cardiol. 2011;148:319-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 36. | Karaahmet T, Gürel E, Tigen K, Güler A, Dündar C, Fotbolcu H, Basaran Y. The effect of myocardial fibrosis on left ventricular torsion and twist in patients with non-ischemic dilated cardiomyopathy. Cardiol J. 2013;20:276-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 37. | van Dalen BM, Soliman OI, Vletter WB, ten Cate FJ, Geleijnse ML. Left ventricular untwisting in restrictive and pseudorestrictive left ventricular filling: novel insights into diastology. Echocardiography. 2010;27:269-274. [PubMed] |
| 38. | Kim HK, Chang SA, Ahn HS, Shin DH, Kim JH, Lee SP, Kim YJ, Cho GY, Sohn DW, Oh BH. Load independence of two-dimensional speckle-tracking-derived left ventricular twist and apex-to-base rotation delay in nonischemic dilated cardiomyopathy: implications for left ventricular dyssynchrony assessment. J Am Soc Echocardiogr. 2012;25:652-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 39. | Ritter M, Oechslin E, Sütsch G, Attenhofer C, Schneider J, Jenni R. Isolated noncompaction of the myocardium in adults. Mayo Clin Proc. 1997;72:26-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 507] [Cited by in RCA: 468] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 40. | Maron BJ, Towbin JA, Thiene G, Antzelevitch C, Corrado D, Arnett D, Moss AJ, Seidman CE, Young JB. Contemporary definitions and classification of the cardiomyopathies: an American Heart Association Scientific Statement from the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; and Council on Epidemiology and Prevention. Circulation. 2006;113:1807-1816. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2284] [Cited by in RCA: 2288] [Article Influence: 114.4] [Reference Citation Analysis (0)] |
| 41. | Sen-Chowdhry S, McKenna WJ. Left ventricular noncompaction and cardiomyopathy: cause, contributor, or epiphenomenon? Curr Opin Cardiol. 2008;23:171-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 68] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 42. | Sanchez-Quintana D, Garcia-Martinez V, Climent V, Hurle JM. Morphological changes in the normal pattern of ventricular myoarchitecture in the developing human heart. Anat Rec. 1995;243:483-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 55] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 43. | Jenni R, Oechslin EN, van der Loo B. Isolated ventricular non-compaction of the myocardium in adults. Heart. 2007;93:11-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 208] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 44. | van Dalen BM, Caliskan K, Soliman OI, Nemes A, Vletter WB, Ten Cate FJ, Geleijnse ML. Left ventricular solid body rotation in non-compaction cardiomyopathy: a potential new objective and quantitative functional diagnostic criterion? Eur J Heart Fail. 2008;10:1088-1093. [PubMed] |
| 45. | Bellavia D, Michelena HI, Martinez M, Pellikka PA, Bruce CJ, Connolly HM, Villarraga HR, Veress G, Oh JK, Miller FA. Speckle myocardial imaging modalities for early detection of myocardial impairment in isolated left ventricular non-compaction. Heart. 2010;96:440-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 68] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 46. | Udink ten Cate FE, Schmidt BE, Lagies R, Brockmeier K, Sreeram N. Reversed apical rotation and paradoxical increased left ventricular torsion in children with left ventricular non-compaction. Int J Cardiol. 2010;145:558-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 47. | van Dalen BM, Caliskan K, Soliman OI, Kauer F, van der Zwaan HB, Vletter WB, van Vark LC, Ten Cate FJ, Geleijnse ML. Diagnostic value of rigid body rotation in noncompaction cardiomyopathy. J Am Soc Echocardiogr. 2011;24:548-555. [PubMed] |
| 48. | Peters F, Khandheria BK, Libhaber E, Maharaj N, Dos Santos C, Matioda H, Essop MR. Left ventricular twist in left ventricular noncompaction. Eur Heart J Cardiovasc Imaging. 2014;15:48-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 49. | Nemes A, Kalapos A, Domsik P, Forster T. Identification of left ventricular “rigid body rotation” by three-dimensional speckle-tracking echocardiography in a patient with noncompaction of the left ventricle: a case from the MAGYAR-Path Study. Echocardiography. 2012;29:E237-E240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 50. | Rüssel IK, Götte MJ. New insights in LV torsion for the selection of cardiac resynchronisation therapy candidates. Neth Heart J. 2011;19:386-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 51. | Nemes A, Havasi K, Forster T. “Rigid body rotation” of the left ventricle in hypoplastic right-heart syndrome: a case from the three-dimensional speckle-tracking echocardiographic MAGYAR-Path Study. Cardiol Young. 2015;25:768-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 52. | Kroeker CA, Tyberg JV, Beyar R. Effects of ischemia on left ventricular apex rotation. An experimental study in anesthetized dogs. Circulation. 1995;92:3539-3548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 90] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 53. | Moen CA, Salminen PR, Grong K, Matre K. Left ventricular strain, rotation, and torsion as markers of acute myocardial ischemia. Am J Physiol Heart Circ Physiol. 2011;300:H2142-H2154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 54. | Sun JP, Niu J, Chou D, Chuang HH, Wang K, Drinko J, Borowski A, Stewart WJ, Thomas JD. Alterations of regional myocardial function in a swine model of myocardial infarction assessed by echocardiographic 2-dimensional strain imaging. J Am Soc Echocardiogr. 2007;20:498-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 55. | Bansal M, Leano RL, Marwick TH. Clinical assessment of left ventricular systolic torsion: effects of myocardial infarction and ischemia. J Am Soc Echocardiogr. 2008;21:887-894. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 60] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 56. | Takeuchi M, Nishikage T, Nakai H, Kokumai M, Otani S, Lang RM. The assessment of left ventricular twist in anterior wall myocardial infarction using two-dimensional speckle tracking imaging. J Am Soc Echocardiogr. 2007;20:36-44. [PubMed] |
| 57. | Nagel E, Stuber M, Lakatos M, Scheidegger MB, Boesiger P, Hess OM. Cardiac rotation and relaxation after anterolateral myocardial infarction. Coron Artery Dis. 2000;11:261-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 68] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 58. | Cirillo M, Arpesella G. Rewind the heart: a novel technique to reset heart fibers’ orientation in surgery for ischemic cardiomyopathy. Med Hypotheses. 2008;70:848-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 59. | Setser RM, Smedira NG, Lieber ML, Sabo ED, White RD. Left ventricular torsional mechanics after left ventricular reconstruction surgery for ischemic cardiomyopathy. J Thorac Cardiovasc Surg. 2007;134:888-896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 60. | Cirillo M, Campana M, Brunelli F, Tomba MD, Mhagna Z, Messina A, Villa E, Troise G. ‘Let’s twist again’: surgically induced renewal of left ventricular torsion in ischemic cardiomyopathy. J Cardiovasc Med (Hagerstown). 2010;11:34-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: De Ponti R, Peteiro J, Sakabe K, Teragawa H S- Editor: Tian YL L- Editor: A E- Editor: Wu HL