INTRODUCTION
Illicit drug abuse, including intravenous drug abuse (IVDA), is increasing in the Middle East Gulf region[1,2]. The existence of many transit port services in the Middle East Gulf States (Saudi Arabia, United Arab Emirates (UAE), Oman, Bahrain, Kuwait and Qatar) has contributed to smuggling of substance abuse drugs in the region[1,2]. The Middle East and Gulf, traditionally transit markets, are also increasingly becoming consumer markets in view of their geographical location and the young population of the region (60% below 15 years). As a direct consequence, this may have led to increasing correlates of drug abuse such as overdose, dependence, psychosis, suicide, road traffic accidents, cutaneous complications, thrombophlebitis of veins, myocardial infarction, pulmonary embolism, infective endocarditis (IE) specifically tricuspid valve endocarditis (TVE), pneumonia, pulmonary tuberculosis, septicemia, transmission of blood-borne infections (human immune deficiency virus (HIV)/hepatitis) and have also impacted on increased mortality due to overdose[2]. However, there is a paucity of data with respect to the incidence of tricuspid valve endocarditis in this region, probably due to underdiagnosis or underreporting. In addition, there is a lack of epidemiological studies documenting the burden of disease in terms of prevalence and related morbidity and mortality due to drug abuse in this region. This review article summarizes the epidemiology of illicit drug abuse in the Middle East Gulf Region (Figure 1) in relation to the diagnosis and treatment of TVE.
Figure 1 Map of Middle East Gulf States.
UAE: United arab emirates.
EPIDEMIOLOGY AND BURDEN OF ILLICIT DRUG ABUSE IN THE MIDDLE EAST GULF REGION
The commonly abused illicit substances can be broadly grouped as stimulants (amphetamines/methamphetamines/crystal meth/speed/captagon tablets/khat /3,4-methylenedioxy-N-methylamphetamine/ecstasy, lysergic acid diethylamide, cocaine/crack and cannabis/marijuana/ganja/hashish/bhang), hypnotics (barbiturates and methaqualones) and opiates (morphine, heroin/smack/brown sugar, opium, methadone). Among these, the most commonly injected drug is heroin[1]. However, morphine, amphetamines/methamphetamines, and cocaine are also common[1].
Globally, the United Nations Office on Drugs and Crime (UNODC), estimates that there were about 149-271 million people aged 15-64 years (3.3%-6.1%) who used an illicit drug at least once in 2009[1]. A large systematic review which included UNODC data reported 125-203 million people to be cannabis users, 15-39 million were opioid, amphetamine or cocaine users, and 11-21 million IVDAs[2]. The highest levels of use were in North America, Western Europe and Oceania. The Middle East data suggested that 6-12 million (2.4%-4.8%) were cannabis users, 2-3 million were opioid users (0.8%-1.4%), 0.4-4 million were amphetamine users (0.2%-1.7%) and 0.04-0.6 million were cocaine users[2]. Opioid use, including heroin, had an estimated 12 to 21 million users globally. The highest rates of opioid use was reported in the Middle Eastern regions, where up to 1.4% of the population aged 15 to 64 had tried the drug at least once in 2009[2].
Data from the Eastern Mediterranean Regional Office of the World Health Organization suggest a prevalence of illicit drug use disorders at the rate of 3500 per 100000 population and that of injecting drug use to be 172 per 100000 population[3]. A report from UAE estimated that about 40% of all illegal drugs in the world are sold in the Gulf region[4]. The same report noted that the mean age of new drug abusers has dropped from 17-18 years to 10 years[4]. Most of the illicit drugs destined for African and European countries transited via the Gulf States, with significant leakage to the Gulf States[4]. In a report from Oman, quoting the Ministry of Health, 1521 drug misuse-related cases were reported in the period 2006-2011 and the most common mode of misuse was IVDA (66%)[5].
In 2002, a report from Al-Amiri Hospital in Kuwait estimated the presence of 18000-20000 drug users in this small Gulf State, the equivalent of 1% its total population[6]. Unemployment, excess disposable income, boredom and frustration were cited as important factors for the youth to take up drugs. In addition, drug dealers easily get couriers among the thousands of expatriate laborers entering Kuwait[6]. Another survey conducted among university students in Kuwait revealed that the total lifetime prevalence of illicit drug use was 14.4% and the most frequently used illicit substance was marijuana (11%)[7]. On multivariate logistic regression analysis, drug use was significantly associated with age, poor academic performance, high family income, being an only child in the family, divorced parents and graduation from a private high school[7].
TRICUSPID VALVE ENDOCARDITIS PATHOGENESIS
Right sided endocarditis accounts for 5%-10% of all IE and predominantly affects the tricuspid valve (TV)[8-10]. TVE commonly occur among IVDAs[11,12]. The cause for the increased prevalence of TVE in IVDAs is multifactorial. Frontera et al[10] suggested possible mechanisms which include: (1) recurrent episodes of particulate matter bombardment (drug solutions may contain particulate matter like talc) leading to damage of TV; (2) TV intimal damage, vasospasm (cocaine induced) and thrombus formation due to injected drugs; (3) increased right sided cardiac turbulence secondary to drug-induced pulmonary hypertension (buprenorphine); (4) increased expression of matrix molecules on the TV which are capable of binding microorganisms in IVDAs; (5) injection of large “bacterial loads” from contaminated drug solutions causing IE; and (6) IVDA-related “immune dysregulation” with or without coexistent HIV infection. In addition, poor injection hygiene (e.g., lack of skin cleaning before injecting), injecting with unsterile needles, multiple needle sharing and injecting contaminated drug solutions which tends to introduce high bacterial loads.
WORLDWIDE INCIDENCE OF TVE
Among the published reports, the overall incidence of IE among IVDAs ranges from 1.5-20 per 1000 drug user per year[10]. In the United States, the incidence is estimated at 1.5 to 3.3 cases per 1000 person-years[12]. From the Western series, acute infection is responsible for 60% of all hospital admissions among IVDAs. Among these acute infections, TVE is implicated in 5%-15% of these cases[12,13]. It is also estimated that the incidence of IE in IVDAs is 2%-5% per year and is responsible for 5% to 10% of the overall death rate[14]. In the large multinational International Collaboration on Endocarditis-Prospective Cohort Study (ICE-PCS) evaluating 2781 patients with IE, 10% of the patients were IVDAs[15].
INCIDENCE OF TVE IN THE MIDDLE EAST
There are few published reports of IE from Middle East Gulf States. Among these studies, IVDA is reported in only 1 study. Even although the Middle East region has the highest prevalence of IVDA among all countries in the world[2], the incidence of TVE and IVDA is reported to be very low. This may be due to either underdiagnosis or underreporting. In a study from Oman published in 2003 and involving 90 patients with IE, there were no patients with TVE or with a history of IVDA[16]. This was similar to studies from Yemen (72 patients) and Kuwait (60 patients), with no involvement of TV or history of IVDA[17,18]. However, between 2006 and 2011, 7 cases of TVE with 3 of them reporting active IVDA were reported from Oman (personal communication). In a study from Saudi Arabia among 83 patients with IE, 4 cases of native TV involvement and 1 case of prosthetic TV involvement were reported, but with no mention of IVDA[19]. In a second study from Saudi Arabia, out of 47 cases of endocarditis, TV was affected in 3 patients (6.4%), pulmonic valve in 2 patients and both pulmonic valve and TV in 1 patient (2.1%). In addition, 2 (4.3%) patients gave a history of IVDA[20]. A study from Lebanon also reported 7% (6/91) of patients with IE had TVE and no IVDA[21].
CLINICAL MANIFESTATIONS
The majority of IVDAs with TVE are young, between 20-40 years of age, and predominantly men (male:female ratio, 4 to 6:1)[12]. The most common presenting manifestations of TVE are persistent fever, bacteremia and multiple pulmonary emboli[9,11]. Respiratory symptoms are more common in TVE than left sided endocarditis. Dyspnea, pleuritic chest pain, cough and hemoptysis are the most common symptoms. Patients can present with metastatic abscesses in lungs that may lead to repeated episodes of dyspnea with hypoxemia and may mimic pulmonary embolism. However, left sided endocarditis in IVDAs is not uncommon and when any peripheral emboli or stroke occur, either left sided endocarditis or paradoxical embolism should be strongly suspected in patients with IVDA[11]. It is important to note that history and physical examination are not diagnostic of TVE in patients with IVDA. There is an absence of underlying heart disease in two-thirds of the patients. Symptoms and signs may be nonspecific. In about 65% of IVDAs with TVE, heart murmurs are not appreciated[11]. This is in view of normal or mildly elevated right ventricular pressures resulting in a low velocity less turbulent tricuspid regurgitation (TR) jet[11]. Generally, respiratory findings dominate the clinical, chest X-ray and computed tomography (CT) scan features. They can even mimic other respiratory infections like pulmonary tuberculosis[22].
DIAGNOSIS
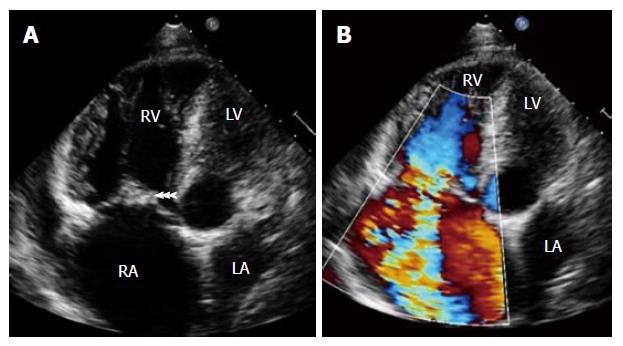
The two most important diagnostic features of TVE in patients with IVDA are echocardiographic evidence of vegetation (Figure 2A) and the presence of septic embolic phenomena[11]. In addition, moderate to severe tricuspid regurgitation may be present (Figure 2B). In IVDAs with IE, TV is commonly involved in about 60%-80% of cases, with reported mortality of 5%-10%[9]. In a study of 105 IVDAs with IE, 86% were right sided and 14% were left sided[11]. In IVDAs, both sides of the heart are usually involved simultaneously in 5% to 10% of cases[13]. TV vegetations generally grow to a larger size (> 2 cm) due to low pressure in right heart chambers and thus may mimic fungal endocarditis[11]. Vegetations may embolize and can be seen in the right ventricle or pulmonary artery or entrapped in the tricuspid chordal apparatus[11,22]. Transthoracic echocardiography (TTE) plays an important role in the diagnosis of TVE. Many IVDAs are young and generally have good echo windows, resulting in good high resolution images[11]. In addition, as the TV is relatively nearer to the transducer, excellent images can be obtained by TTE. TEE is indicated in patients with poor echo window or in those with initial negative TTE in whom there is high index of suspicion of TVE[11]. The diagnostic yield of TTE is comparable with that of TEE in IVDAs[23].
Figure 2 Transthoracic echocardiography showing (A) large vegetation attached to tricuspid valve leaflets (arrowheads) in a patient with intravenous drug abuse and septic pulmonary emboli.
Note hugely dilated right atrium and right ventricle and (B) severe tricuspid regurgitation. RA: Right atrium; RV: Right ventricle; LA: Left atrium; LV: Left ventricle.
Duke’s criteria have been predominantly applied for left sided endocarditis and have not been studied specifically in TVE. However, the two major criteria of typical echocardiographic features of TVE along with positive blood cultures with a typical organism should be regarded as diagnostic of TVE[11]. Blood culture is positive in a high proportion of TVE. When the culture is negative, it is usually due to prior antibiotic use or due to rare organisms such as Bartonella and HACEK organisms. The predominant organism of TVE in IVDAs is Staphylococcus aureus (60%-90%)[9-15]. Other organisms causing TVE are pseudomonas aeruginosa, other gram-negative bacilli, poly-microbial infections, fungi and group B streptococci[9-15]. In a study, the incidence of IE was 17% among all staphylococcal bacteremia patients and 46% among IVDAs[13]. In another study, 24% of IVDAs developed methicillin resistant staphylococcus aureus, of whom 41% developed IE[24]. Thus, in IVDAs, if patients develop staphylococcal bacteremia, nearly 50% of them go on to develop TVE. In another study among IVDAs presenting with fever to emergency departments, negative predictors of TVE were lack of skin infection, tachycardia, hyponatremia, pneumonia on chest radiograph, history of endocarditis, thrombocytopenia and heart murmur. The best criteria combination of lack of skin infection, tachycardia and cardiac murmur had a sensitivity and negative predictive value of 100%[25].
COMPLICATIONS
Septic pulmonary embolism in patients with TVE occurs in 75% to 100% of patients[26]. It may cause pulmonary infarction, pulmonary abscesses, bilateral pneumothoraces, mycotic aneurysms of pulmonary arteries, pleural effusions and empyema[9,11]. The chest X-ray may show pulmonary infiltrates or opacities in about 56% of radiographs at presentation[11]. Typical chest manifestations on CT scan due to emboli are pulmonary infiltrates, obstruction, nodules or wedge shaped opacities with or without cavitations and abscesses suggesting septic emboli, which are seen in 80% of such patients[9-14]. The use of large proximal veins (femoral veins) in IVDAs may result in life-threatening septic deep venous thrombosis and pulmonary embolism[27].
Right heart failure is common due to acute pulmonary hypertension or severe TR or TV obstruction[9,11]. Large vegetations can cause tethering of the septal and lateral valve leaflets, causing the TV to remain open throughout systole and leading to severe TR. In addition, prolapse, perforation, right ventricular dilation and flail leaflet due to disruption can all lead to severe TR. Large vegetations can even protrude through patent foramen ovale into the left atrium[28]. Paravalvar abscess formation occurs infrequently. Hypoxemia and paradoxical embolism can occur due to right to left shunting through a patent foramen ovale[11].
MANAGEMENT AND PROGNOSIS
Uncomplicated TVE is successfully treated medically in 80% of patients, with only 20% needing surgical intervention[12,29]. The reason why TVE responds well to medical therapy is that right sided heart involvement, even when severe, often allows time for medical treatment because of the greater tolerance for TR and pulmonary embolization[29]. Hence, it is recommended to wait before surgical intervention if possible until sepsis resolves with antibiotic treatment[29]. Right sided involvement, younger age and lack of pre-existing heart disease or other underlying diseases have been thought to explain the better prognosis of Staphylococcus aureus endocarditis among IVDAs than in the general population.
In methicillin-sensitive staphylococcal aureus native-valve endocarditis, beta-lactamase-resistant penicillins, like flucloxacillin, oxacillin or glycopeptides (teicoplanin or vancomycin), combined with gentamycin (for 2 wk) is recommended[9]. In uncomplicated TVE, medical treatment should be continued for 4-6 wk[12]. However, IVDAs pose a unique challenge in the treatment as they are poor or non-compliant to medication and follow-up, get early self-discharge from hospital and may go back to injecting drugs again once discharged from hospital. This naturally leads to high rates of relapse and re-infection[30]. Given the low likelihood of adherence to a 4 wk course of antimicrobials among IVDAs, shorter courses of therapy, with a combination of β-lactam with or without an aminoglycoside (for 2 wk) have become an accepted standard[12,30]. However, in a few centers in highly selected IVDA IE patients, with appropriate counseling and monitoring, it was possible to treat with outpatient parenteral antibiotic therapy using peripherally inserted central catheter lines[31]. Poly-microbial endocarditis is more frequent in IVDA, which may need long-term suppressive therapy, specifically if fungal endocarditis is present[32]. The most important organisms in poly-microbial IE in IVDAs are: Staphylococcus aureus, Streptococcus pneumonia and Pseudomonas aeruginosa, as well as mixed cultures of Candida spp. and bacteria[33].
The European Society for Cardiology guidelines made some recommendations for operative indications for TVE in the active stage. These recommendations are: (1) refractory right heart failure secondary to severe persistent TR; (2) IE caused by organisms which are difficult to eradicate (e.g., persistent fungi) or bacteremia for at least 7 d despite adequate antibiotic therapy; and (3) TV vegetations > 20 mm which persist after recurrent pulmonary emboli with or without concomitant right heart failure[9]. Surgical options include vegetectomy, valvulectomy, valve repair/reconstruction with annuloplasty ring or replacement (either mechanical or bioprosthesis valves)[29,34]. A few authors opine that in IVDAs, vegetectomy and valve repair is preferred, avoiding artificial material and thus preventing prosthetic valve endocarditis[29,35,36]. If a valve replacement is done, some authors prefer a bioprosthesis valve as it could be better in terms of prognosis than a mechanical valve[36-38]. However, in a few studies, both mechanical and bioprosthesis valves have been successfully implanted in IVDAs with a similar 15 year survival (47.8% for mechanical vs 46.7% for bioprosthesis valves) and re-operation free survival (53% for mechanical vs 52% for bioprosthesis valves)[39,40].
Prognosis in TVE is generally good and in-hospital mortality is less than 10%[9-14]. Vegetation length > 20 mm and fungal etiology were found to be the main predictors of death in right sided IE in IVDAs[41,42]. In the ICE-PCS registry, 22% of TVE patients needed surgery and in-hospital mortality was 6%[15]. In patients with IE and HIV infection, there was higher total mortality at 2 mo, specifically in those with a CD4 count below 200 per microl[43,44]. In addition, any left sided involvement and age greater than 35 years are independently associated with mortality[45-47]. In a study, IVDAs with IE admitted to intensive care unit had very high mortality (27%), mainly due to sepsis and septic embolization[48]. In patients with repeated IVDA and endocarditis, the prognosis is poor and few authors are of the opinion that these patients should be offered valve replacement only once. If they develop a second episode of endocarditis, they should not be offered another valve replacement surgery[49,50].
CONCLUSION
In conclusion, recent reports indicate increasing trends in IVDA in the Middle East region. However, there is lack of reports about TVE, probably due to underdiagnosis or underreporting. TVE can mimic other respiratory diseases and may mislead in obtaining early diagnosis. A high index of suspicion of TVE is essential in patients with IVDA. In addition to already prevailing regulations and strict laws against drug trafficking in the Middle East Gulf region, programs to increase public awareness about the harmful effects of drug abuse are essential. Furthermore, a de-addiction drive among the youth in this region, anti-drug campaigns and the establishment of more rehabilitation centers are the need of the hour for eradicating this menace.
P- Reviewer: Castillo R S- Editor: Zhai HH L- Editor: Roemmele A E- Editor: Wang CH