Published online Aug 26, 2025. doi: 10.4330/wjc.v17.i8.107437
Revised: May 22, 2025
Accepted: August 1, 2025
Published online: August 26, 2025
Processing time: 150 Days and 1.6 Hours
Mesenchymal stem cells (MSCs) possess unique properties such as immunomodulation, paracrine actions, multilineage differentiation, and self-renewal. Therefore, MSC-based cell therapy is an innovative approach to treating various degenera
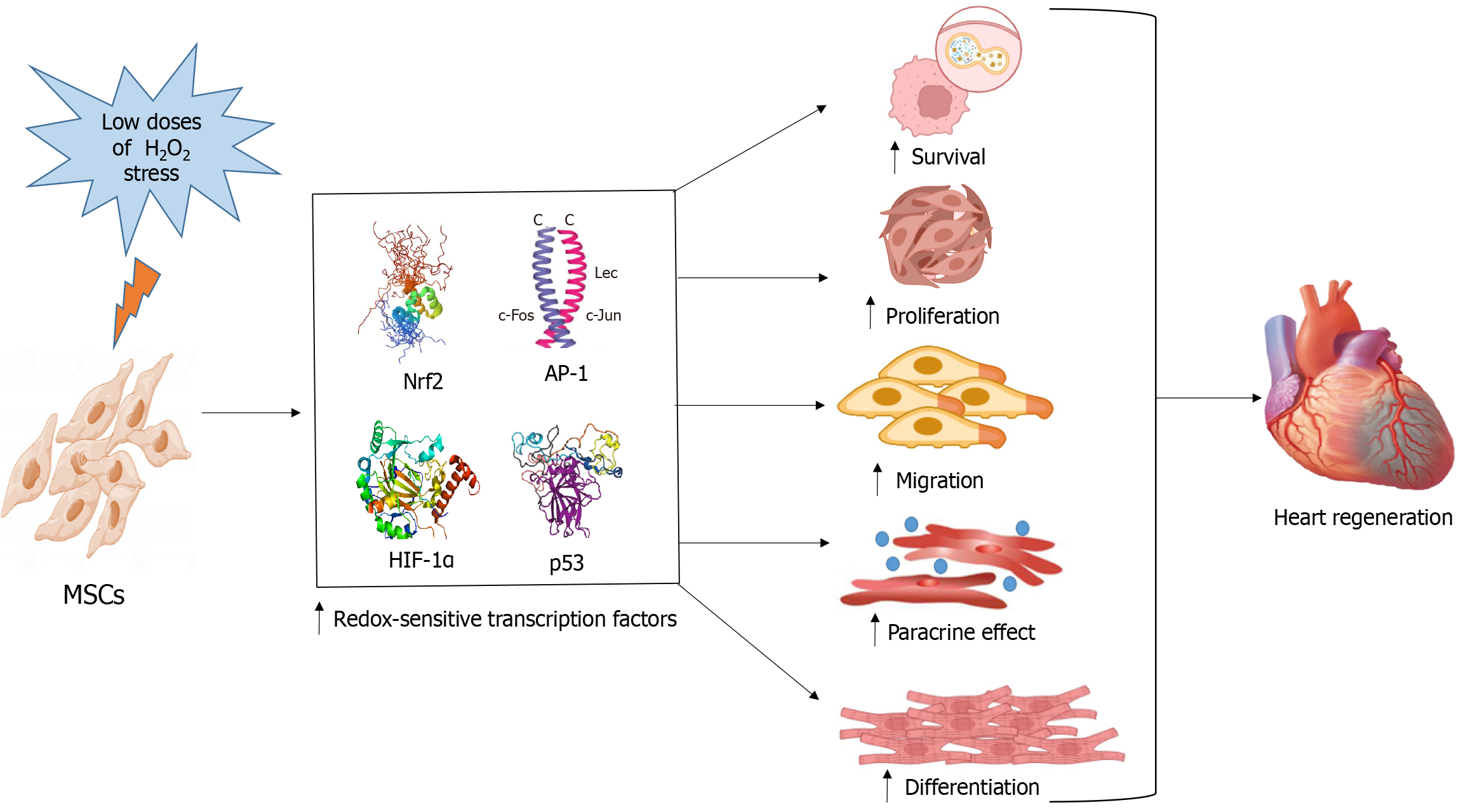
Core Tip: Hydrogen peroxide (H2O2) preconditioning is reported to increase protective mechanisms in mesenchymal stem cells and enhance their ability to regenerate in damaged hearts. However, its molecular mechanism remains under-explored. This review highlights the studies on the protective biological functions and regulatory mechanisms associated with H2O2 preconditioning in heart regeneration. Moreover, the role of the H2O2-activated redox-sensitive transcription factors and their associated pathways in cell survival, proliferation, migration, paracrine effect, and cardiac differentiation is discussed. The molecular insights provided in this review will possibly help in the development of cardiovascular regenerative therapy.
- Citation: Siraj A, Haneef K. Role of hydrogen peroxide preconditioning in mesenchymal stem cell-mediated heart regeneration: Molecular insights. World J Cardiol 2025; 17(8): 107437
- URL: https://www.wjgnet.com/1949-8462/full/v17/i8/107437.htm
- DOI: https://dx.doi.org/10.4330/wjc.v17.i8.107437
Redox imbalance, which is caused by a compromised antioxidant system or an overabundance of reactive oxygen species (ROS), is a major factor in cardiovascular disorders such as myocardial infarction (MI), ischemia-reperfusion damage, end-stage heart failure, and cardiomyopathy[1]. Heart transplantation remains the most effective treatment for heart failure because existing treatments have limited efficacy and cannot restore the heart's normal functions. However, this procedure is limited due to donor organ unavailability, immunological rejection, long-term complications, and higher expenses[2].
Mesenchymal stem cell (MSC) therapy has shown promise as an alternative method for restoring heart function in individuals with cardiovascular disorders[3]. MSCs are adult stem cells that can self-renew and differentiate into several lineages. These cells are found in bone marrow, adipose tissue, umbilical cord, and several other tissues and organs[4]. Studies have demonstrated that transplanted MSCs can differentiate into vascular cells and cardiomyocytes in heart models[5]. Since stem cell self-renewal and differentiation are dependent upon the redox balance of the tissue, stem cells cannot survive in inflamed tissue for long periods due to the hostile microenvironment[6].
Preconditioning is a technique that refers to the brief exposure of cells to mild stressors to get them ready for the harsh environment that they may experience in the diseased tissue[7]. Numerous preconditioning methods, such as chemical agents, hypoxia, gene modification, pharmacological agents, and physical factors have been investigated to increase the overall effectiveness of MSC transplantation[8]. It has been reported that pretreatment of MSCs with a controlled stressor can improve their proliferative, secretory, migratory, and differentiated properties[9]. Numerous studies have demon
MSCs are increasingly being used in regenerative medicine to develop cell treatments. MSCs have demonstrated remar
Hypoxic preconditioning is a method where cells are exposed to moderate hypoxia for a shorter period of time which results in increased resistance to severe ischemic conditions[15]. Preconditioning techniques regulate a range of biological processes by either activating or suppressing chemical signals and signal transduction pathways[9]. Hypoxic preconditioned MSCs (HP-MSCs) release a wide range of substances with anti-apoptotic, pro-angiogenic, trophic, immunomodulatory, or immunosuppressive properties[16]. A number of studies have demonstrated the therapeutic potential of HP-MSCs in heart regeneration[9,17,18]. It has been reported that HP-MSCs following transplantation provide cardioprotective benefits in terms of increased neovascularization and reduced fibrosis[19]. According to research, controlled hypoxia is reported to improve cardiovascular health and oxygen supply by increasing blood vessel density, myocardial contractility, and erythropoietin (EPO) production[20]. Moreover, hypoxia is reported to enhance EVs loaded with miRNAs such as miR-210 to heal MI[21].
A number of physical preconditioning methods such as shear stress, stretch, compression, and electrical or magnetic fields have shown promising results in the field of regenerative medicine[22]. These methods are reported to enhance MSCs’ ability to regenerate damaged tissues[7,23]. It has been reported that shear stress improves MSC alignment and stimulates the phosphatidylinositol 3-kinase (PI3K)/protein kinase B (Akt)/endothelial nitric oxide (NO) synthase path
Biological and pharmacological preconditioning agents have been shown to enhance MSC survival, proliferation, di
For efficient utilization of MSCs in heart regeneration, their survival must be increased by triggering adaptive cellular responses. A number of research studies support the narration that H2O2 preconditioning induces cell survival in MSCs by upregulating various signaling pathways such as Janus kinase/signal transducer and activator of the transcription, Akt, Nrf1, Nrf2, p38 MAPK, PI3K/Akt, Notch1, and Wnt11[34,42-44]. In 2020, Garrido Pascual[45] reported that preconditioning with 0.25 mmol H2O2 for 1 hour regulates the effects of oxidative stress in transplanted MSCs by increasing the expression of the transcription factor Nrf2 and antioxidant enzymes catalase (CAT), superoxide dismutase (SOD), heme oxygenase-1 (HO-1), and glutathione peroxidase (GPx)-1. Moreover, these preconditioned MSCs are reported to increase cell survival by reducing the secretion of pro-inflammatory molecules cyclooxygenase-2 and interleukin (IL)-1β and by increasing adenosine triphosphate production. Sadidi et al[46] in 2009 have also reported increased survival and growth of preconditioned MSCs via the PI3K/Akt signaling pathway. According to the research by Nouri et al[34] in 2019, MSCs pretreated with 20 μM H2O2 for 12 hours exhibited enhanced cell survival in the ischemic heart via the hypoxia-inducible factor-1α (HIF-1α) and PI3K/Akt pathways.
Adequate cell count is a key factor that boosts MSCs’ capability to repair and regenerate damaged tissues[47]. MSCs’ functional characteristics such as proliferation, adhesion, and migration are reported to be enhanced by H2O2 preconditioning[41]. In 2012, Zhang et al[48] reported that preconditioning of MSCs with a low concentration of H2O2 stimulates cell migration and proliferation via IL-6 secretion. Moreover, H2O2 treated cells have been shown to modulate the production of phase II antioxidant enzymes via the PI3K/Akt and p38 MAPK pathways, thus promoting proliferation[44]. Similar proliferation results of preconditioned stem cells have been reported in a in vitro study of 2019 by Castro et al[49], who stated that the cryopreserved H2O2 preconditioned stem cells show improved bioactivity against oxidative stress through increased adhesion and cell cycle progression, suggesting a greater ability for proliferation.
Cell migration plays a key role in various physiological processes including tissue regeneration and repair. A number of studies[34] have reported that H2O2 preconditioning enhances MSCs’ migration to ischemic myocardium following trans
Preconditioning enhances MSCs' therapeutic potential by stimulating the release of paracrine chemicals through a variety of signaling pathways. A study has been carried out by Pankajakshan et al[52] has shown the H2O2 preconditioned MSCs release key paracrine factors involved in heart regeneration, such as VEGF, FGF-2, IGF-1, and IL-6. These soluble factors support heart regeneration via angiogenesis, cell survival, and immunomodulation[52]. A possible method to boost MSC-mediated tissue regeneration was suggested by a study, where MSCs were preconditioned with H2O2. These preconditioned MSCs showed higher proliferation and decreased inflammation rate through paracrine effects[53]. Furthermore, the research conducted by Pendergrass et al[54] described that H2O2 preconditioned cardiac progenitor cells stimulate neoangiogenesis in the peri-infarct region of an ischemia-reperfusion injury model. Another investigation revealed that H2O2 preconditioned MSCs stimulate the production of IL-6, which in turn enhances neovascularization and decreases cardiac fibrosis[48]. Moreover, H2O2 preconditioned cardiac progenitor cells show reduced fibrosis and enhanced angio
H2O2 has been shown to act as signaling molecules that affect several biological pathways. Recently, it has been demonstrated that the key cardiovascular pathways, Notch1 and Wnt11, are activated in H2O2 preconditioned MSCs[55]. Notch1 signaling activation is reported to improve MSC based therapies for cardiac repair and regeneration[56]. A study conducted by Boopathy et al[42] reported that H2O2 mediated oxidative stress activates Notch1 signaling, which promotes cardiogenic gene expression in bone marrow derived MSCs. Exogenous H2O2 at low concentrations shows higher expression of cardiogenic TFs, cytokines, and a number of stem cells derived beating cardiomyocytes[57]. It is well-documented that H2O2 preconditioning enhances various cell protective mechanisms, survival, proliferation, migration, paracrine effects, and differentiation, by activating intracellular signaling pathways (Figure 1 and Table 1)[34,41-45,48-50,54,58-61]. However, there is still a large gap that needs to be filled with a thorough investigation of the underlying mechanisms of H2O2 preconditioning in heart regeneration.
| Cells | Cellular mechanism(s) | Redox sensitive transcription factor(s) | Pathway(s) | Major findings | Ref. |
| Adipose-derived stem cells (hASCs) | Survival | Nrf2 | - | Increased: Antioxidant response; reduced: Inflammation; bioenergetic adaptation; nuclear factor-kappa B modulation | Garrido Pascual[45] |
| Cardiomyocytes | Survival | Nrf2 | - | Increased: Mitochondrial membrane potential; reduced: Oxidative stress, apoptosis in cardiomyocytes | Dreger et al[58] |
| Cardiomyocytes | Proliferation and survival | Nrf1 and Nrf2 | P38 MAPK and phosphatidylinositol 3-kinase/Akt | Increased: Phase II enzymes and Bcl2; reduced: Oxidative stress, apoptosis, and caspase-3; resistance to oxidative stress in ischemia-reperfusion injury | Angeloni et al[44] |
| Zebrafish cardiomyocytes | Proliferation and survival | P53 | - | Increased: Proliferation and redox homeostasis; reduced: Reactive oxygen species levels and scar formation | Ye et al[59] |
| Human Wharton's jelly-derived MSCs | Proliferation, survival, and migration | Hypoxia-inducible factor-1α | Akt | Increased: Resistance to oxidative stress and cell viability; reduced: Apoptosis | Nouri et al[34] |
| Human MSCs | Survival | - | - | Increased: Adhesion | O'Leary[43] |
| Mice myocytes | Survival | Catalase | - | Regulate calcium handling and improve ventricular diastolic dysfunction; preserve sarcoplasmic reticulum calcium ATPase activity | Qin et al[60] |
| Wharton's Jelly-derived MSCs | Survival, migration, paracrine effect, and differentiation | - | - | Increased: Neovascularization and interleukin-6; reduced: Fibrosis | Zhang et al[48] |
| HASCs | Proliferation, paracrine effects, and migration | - | - | Increased: Insulin-like growth factor-1, PFKFB4, pyruvate dehydrogenase kinase isoenzyme 1, resistance to oxidative stress, glycolysis; reduced: Oxidative phosphorylation | Castro et al[49] |
| Human decidua basalis mesenchymal stem/stromal cells | Proliferation, migration, and survival | - | - | Increased: Colony formation, adhesion, migration, wound-healing, tube formation, and oxidative stress resilience | Khatlani et al[41] |
| Zebrafish heart lines | Migration, and differentiation | - | MAPK and extracellular signal-regulated kinases 1/2 | Increased: Duox and NADPH oxidase 2; reduced: Dusp6 | Han et al[50] |
| Cardiac progenitor cells | Paracrine effect, differentiation, survival | - | - | Increased: Angiogenesis, endothelial cell density, survival, and cardiac function post-I/R injury; reduced: Fibrosis, apoptosis | Pendergrass et al[54] |
| Mouse cardiac myocytes | Survival and paracrine effect | - | AMP-activated protein kinase and Akt | Increased: Myocyte contractility; selective activation of nitric oxide synthase isoforms | Sartoretto et al[61] |
| Bone marrow-derived MSCs | Differentiation | - | Notch1 | Increased: Flt1, vWF, PECAM1, NK2 homeobox 5, αMHC, Notch1, Wnt11, cardiac repair and regeneration | Boopathy et al[42] |
Mammalian cells continuously produce ROS as byproducts of electron transport activities. At physiological levels, ROS serves a crucial role in redox signaling through various post-translational modifications. However, increased ROS production causes molecular damage, a condition known as oxidative distress. Therefore, maintaining the redox balance is crucial for normal cell functioning[62]. H2O2, a ROS and an essential redox signaling agent, is produced by several metabolic activities in mammalian cells[63]. It is an intracellular messenger that regulates a number of physiological processes by reversible oxidation of the thiol side chain of cysteine residues of the effector proteins, thereby modulating the downstream gene expression and cell behaviors[57]. Heart development is regulated by a network of TFs such as Nkx2.5, GATA-4, Mef2c, and Tbx5[13]. Cardiac TFs might not be directly targeted by ROS, but their regulation can be controlled by redox sensitive TFs[57]. According to earlier research[64], oxidative stress caused by low-concentration H2O2 supplementation to culture media activates redox sensitive TFs, including Nrf2, activator protein-1 (AP-1), p53[65], and HIF-1α[34]. These TFs control the intracellular signaling pathways involved in the development/regeneration of the heart[58,59,66,67]. However, the precise role of redox sensitive TFs in heart repair is not fully understood yet. Therefore, it is now essential to uncover their molecular mechanism to target specific biological pathways to ensure improved survival, proliferation, and differentiation of cells in ischemic myocardium, thus increasing the outcome of cardiovascular rege
The basic leucine zipper transcription factor Nrf2 is encoded by the human NFE2 L2 gene. In normal conditions, Nrf2 resides in the cytoplasm because it assembles with kelch-like ECH-associated protein 1 (Keap1). Keap1 is the main negative regulator of Nrf2 that constantly ubiquitylates and degrades Nrf2. Deubiquitination, which is caused by the disruption of the Keap1-Cul3 E3 Ligase complex, releases and accumulates Nrf2 in the nucleus. In the nucleus, Nrf2 interacts with Maf proteins and binds to the antioxidant-response elements (ARE). This interaction promotes the trans
Nrf2's complex transcriptional, translational, and post-translational network regulation allows it to coordinate adaptive responses to different types of stress. It has been proposed that Nrf2 acts as a mediator of protective responses since it is activated in response to moderate concentrations of various stressors and conditions[69]. In the process of tissue re
The transcription factor AP-1 is produced by various dimeric combinations of Fos and Jun families. The synthesis of new Jun and Fos family proteins is triggered by ROS and is dependent on pre-existing TFs[77]. AP-1 is reported to control the signal transduction pathways that lead to cell growth and transformation[78]. Moreover, AP-1 activity is noticeably increased in the presence of antioxidants such as pyrrolidine dithiocarbamate and butylated hydroxyanisole[79]. In response to a variety of stimuli, such as growth hormones, cytokines, oxidative stress, and other environmental signals, AP-1 attaches to the TPA response element in target genes' promoter regions and regulates the transcription of stress responses, apoptosis, differentiation, and cell proliferation[80].
In 2013, a study conducted by Windak et al[81], reported that c-Jun and c-Fos play critical role in the induction of cardiac fetal genes. c-Jun has been shown to shield the heart against pathologic remodeling and maintain the correct arrangement of the cytoskeleton and sarcomeric structure in cardiomyocytes. Moreover, deletion of c-Jun in cardiomyo
AP-1 production is stimulated by various stimuli such as UV light, ionizing radiation, or H2O2[84]. In 2006, Kikuta et al[85] reported that 100 μM H2O2 for 25 hours activates AP-1 by MAPKs, which phosphorylate AP-1 components and increase their transcriptional activity. In earlier studies, it was reported that H2O2 treatment increases AP-1 DNA binding, Jun nuclear kinase activity, and the levels of c-Fos and c-Jun mRNA[86]. AP-1 is reported to regulate the expression of certain antioxidant enzymes and proteins, as well as transforming growth factor-1 beta (TGF-1β)[87], cyclin D1[88], and many cytokines genes, which help in cell cycle progression. Moreover, AP-1 is reported to regulate cellular functions necessary for heart repair, thus playing a crucial role in cardiac regeneration. A recent study in 2020 by Beisaw et al[66], demonstrated that AP-1 regulates the expression of metabolism and cell cycle progression related genes during the process of heart regeneration as well as facilitates the expression of genes necessary for cardiomyocyte regeneration by regulating chromatin accessibility. According to Zuppo et al[89], cardiomyocyte proliferation is hampered when AP-1 expression is reduced, highlighting its crucial function in cell proliferation.
The transcription factor HIF-1α is essential for coordinating cellular reactions to hypoxia or low oxygen supply[90]. Under normoxic conditions, prolyl hydroxylase domain (PHD) enzymes hydroxylate HIF-1α at particular proline residues. This post-translational alteration helps the von Hippel-Lindau E3 ubiquitin ligase complex to ubiquinate and degrade HIF-1α by proteasomal destruction[91]. Hypoxic preconditioning has been shown to increase the expression of HIF-1α through inhibition of PHDs. Similarly, ROS is also reported to stabilize HIF-1α by inhibiting PHD enzymes[92].
HIF-1α is reported to regulate angiogenesis, metabolism, and survival pathways, thus preserving cellular homeostasis in stressful situations[90]. Moeinabadi-Bidgoli et al[7] in 2021 reported that HIF-1α stimulates the production of SDF-1/CXCR4/CXCR7 signaling molecules, which play a crucial role in cell migration. Moreover, it enhances cell survival and proliferation through PI3K/Akt signaling[7]. In 2015, a study conducted by Zimna and Kurpisz[93], demonstrated that HIF-1α increases vessel formation by stimulating VEGF production. Moreover, HIF-1α at low oxygen levels, stimulates the expression of genes that produce glycolytic enzymes and pyruvate dehydrogenase, thus regulating metabolic repro
Preconditioning with a non-cytotoxic dose of H2O2 is reported to increase cell tolerance in stem cells. Chang et al[97] in 2008 reported that HIF-1α inhibition can reverse the H2O2 preconditioning mediated increased tolerance. Sun et al[98] in 2020 reported that HIF-1α overexpressing MSCs enhance cardiac functions and angiogenesis by increasing MSCs’ adhesion, migration, and paracrine effect. These results have suggested that HIF-1α is an important mediator in stem cell preconditioning for cardiac cell therapy. Similar results were reported by Cerrada et al[51]’s study which demonstrated that HIF-1α engineered MSCs enhance the expression of cell adhesion, migration, and paracrine factors genes. These genetically modified MSCs promote cardiac function in terms of angiogenesis, neovascularization, and heart regene
The tumor suppressor protein p53 plays a crucial role in the regulation of the cell cycle, DNA repair, apoptosis, and senescence. P53 is reported to activate NCF2/p67phox, a component of NADPH oxidase 2, which produces ROS[99]. However, it can also inhibit ROS accumulation in low-stress settings[100]. It has been established that p53 regulates several antioxidant enzymes, such as SOD2, GPx1[101], CAT[102], Grx[103], Prxs, and Sestrins[104]. Aubrey et al[105] in 2017 reported that p53 prevents apoptosis in mild stress situations by upregulation of anti-apoptotic genes like Bcl-2 and the downregulation of pro-apoptotic genes like PUMA and NOXA. This process enables cells to endure stress and bounce back[105]. In addition, p53 regulates DNA repair and antioxidant responses, which are essential for tissue regeneration and homeostasis[106]. Under stress conditions, p53 preserves energy balance by regulating metabolic processes including glycolysis and oxidative phosphorylation, which in turn improves cell survival and proliferation[107]. Moreover, p53 is reported to stimulate the production of growth factors like VEGF[108] and TGF-β[109] as well as cytokines (IL-6 and IL-8)[110] which in turn regulate inflammation, angiogenesis, and tissue regeneration. Furthermore, p53 controls the expre
P53 signaling is reported to play an important role in heart development as well as essential to maintaining normal heart architecture and functions[112]. It has been reported that a low concentration of H2O2 induces the expression of p53, which in turn activates the oxidative stress combating genes such as NADPH, and glutathione (GSH) synthesis and nucleotide production genes[61]. In 2021, Goshovska et al[113] demonstrated that GSH deficiency is associated with myocardium damage during cardiac ischemia-reperfusion. Whereas, higher expression of GSH provides cardioprotection by regulating NO, AMPK, and peroxisome proliferator-activated receptor-α signaling[113]. Ye et al[59] in 2020 reported that H2O2 acts as an essential signaling molecule for zebrafish heart regeneration. Moreover, the expression of p53 isoform Δ133p53 I has been shown to increase by low-level ROS. It has been reported that Δ133p53 I, by interacting with full-length p53, promotes cell survival by enhancing the expression of antioxidant genes including GPx1a, Sestrin1, Sestrin2, aldh4, SOD1, and SOD2[59]. These p53 target genes are reported to maintain redox homeostasis within the regenerating tissue[114].
In this review, we present an overview of the protective cellular mechanisms stimulated in H2O2 preconditioned MSCs while covering the role of H2O2-activated redox sensitive TFs in heart regeneration. Cells continuously produce ROS to maintain normal physiological functions. However, increased ROS production causes molecular damage, a condition known as oxidative distress. H2O2, a ROS, acts as an intracellular messenger that regulates several physiological processes. H2O2 preconditioned MSCs have the potential to regulate biological processes related to heart regeneration such as survival, proliferation, migration, paracrine activities, and differentiation. As highlighted in this review, H2O2 might not directly regulate heart regeneration, but oxidative stress caused by a low concentration of H2O2 activates redox sensitive TFs such as Nrf2, AP-1, p53, and HIF-1α, which in turn control the intracellular signaling pathways involved in the development/regeneration of the heart. Combining H2O2 preconditioning with other induction factors may further promote stem cell-mediated heart regeneration. For this reason, it could be a major player in new therapies involving the use of stem cells for the heart diseases. In addition to heart regeneration, H2O2 preconditioned MSCs have also been found to be promising in increasing in vivo cell survival, wound healing, and regeneration of several tissues. These results indicate a broader translational perspective for H2O2 preconditioning in the field of regenerative medicine. However, in the future, it is critical to optimize H2O2 concentration and treatment time to enhance its regenerative effects and prevent oxidative damage.
| 1. | Moris D, Spartalis M, Spartalis E, Karachaliou GS, Karaolanis GI, Tsourouflis G, Tsilimigras DI, Tzatzaki E, Theocharis S. The role of reactive oxygen species in the pathophysiology of cardiovascular diseases and the clinical significance of myocardial redox. Ann Transl Med. 2017;5:326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 213] [Article Influence: 23.7] [Reference Citation Analysis (0)] |
| 2. | Kim IC, Youn JC, Kobashigawa JA. The Past, Present and Future of Heart Transplantation. Korean Circ J. 2018;48:565-590. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 110] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 3. | Clavellina D, Balkan W, Hare JM. Stem cell therapy for acute myocardial infarction: Mesenchymal Stem Cells and induced Pluripotent Stem Cells. Expert Opin Biol Ther. 2023;23:951-967. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 4. | Akbar N, Razzaq SS, Salim A, Haneef K. Mesenchymal Stem Cell-Derived Exosomes and Their MicroRNAs in Heart Repair and Regeneration. J Cardiovasc Transl Res. 2024;17:505-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 5. | Guo Y, Yu Y, Hu S, Chen Y, Shen Z. The therapeutic potential of mesenchymal stem cells for cardiovascular diseases. Cell Death Dis. 2020;11:349. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 212] [Article Influence: 35.3] [Reference Citation Analysis (0)] |
| 6. | Wang K, Zhang T, Dong Q, Nice EC, Huang C, Wei Y. Redox homeostasis: the linchpin in stem cell self-renewal and differentiation. Cell Death Dis. 2013;4:e537. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 192] [Cited by in RCA: 224] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 7. | Moeinabadi-Bidgoli K, Babajani A, Yazdanpanah G, Farhadihosseinabadi B, Jamshidi E, Bahrami S, Niknejad H. Translational insights into stem cell preconditioning: From molecular mechanisms to preclinical applications. Biomed Pharmacother. 2021;142:112026. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 49] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 8. | Hu C, Li L. Preconditioning influences mesenchymal stem cell properties in vitro and in vivo. J Cell Mol Med. 2018;22:1428-1442. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 304] [Cited by in RCA: 325] [Article Influence: 40.6] [Reference Citation Analysis (0)] |
| 9. | Haneef K, Salim A, Hashim Z, Ilyas A, Syed B, Ahmed A, Zarina S. Chemical Hypoxic Preconditioning Improves Survival and Proliferation of Mesenchymal Stem Cells. Appl Biochem Biotechnol. 2024;196:3719-3730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 10. | Jackson MJ, Stretton C, McArdle A. Hydrogen peroxide as a signal for skeletal muscle adaptations to exercise: What do concentrations tell us about potential mechanisms? Redox Biol. 2020;35:101484. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 11. | Hossain MA, Bhattacharjee S, Armin SM, Qian P, Xin W, Li HY, Burritt DJ, Fujita M, Tran LS. Hydrogen peroxide priming modulates abiotic oxidative stress tolerance: insights from ROS detoxification and scavenging. Front Plant Sci. 2015;6:420. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 467] [Cited by in RCA: 395] [Article Influence: 35.9] [Reference Citation Analysis (0)] |
| 12. | Qazi RE, Khan I, Haneef K, Malick TS, Naeem N, Ahmad W, Salim A, Mohsin S. Combination of mesenchymal stem cells and three-dimensional collagen scaffold preserves ventricular remodeling in rat myocardial infarction model. World J Stem Cells. 2022;14:633-657. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Razzaq SS, Khan I, Naeem N, Salim A, Begum S, Haneef K. Overexpression of GATA binding protein 4 and myocyte enhancer factor 2C induces differentiation of mesenchymal stem cells into cardiac-like cells. World J Stem Cells. 2022;14:700-713. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | Gnecchi M, Zhang Z, Ni A, Dzau VJ. Paracrine mechanisms in adult stem cell signaling and therapy. Circ Res. 2008;103:1204-1219. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1645] [Cited by in RCA: 1568] [Article Influence: 87.1] [Reference Citation Analysis (0)] |
| 15. | Sharp FR, Ran R, Lu A, Tang Y, Strauss KI, Glass T, Ardizzone T, Bernaudin M. Hypoxic preconditioning protects against ischemic brain injury. NeuroRx. 2004;1:26-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 187] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 16. | Hao D, He C, Ma B, Lankford L, Reynaga L, Farmer DL, Guo F, Wang A. Hypoxic Preconditioning Enhances Survival and Proangiogenic Capacity of Human First Trimester Chorionic Villus-Derived Mesenchymal Stem Cells for Fetal Tissue Engineering. Stem Cells Int. 2019;2019:9695239. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 17. | Chacko SM, Ahmed S, Selvendiran K, Kuppusamy ML, Khan M, Kuppusamy P. Hypoxic preconditioning induces the expression of prosurvival and proangiogenic markers in mesenchymal stem cells. Am J Physiol Cell Physiol. 2010;299:C1562-C1570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 155] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 18. | Song H, Li B, Guo R, He S, Peng Z, Qu J, Zhao Y, Zhai X, Yin W, Yang K, Fan X, Zhang J, Tan J, Liu Y, Xie J, Xu J. Hypoxic preconditioned aged BMSCs accelerates MI injury repair by modulating inflammation, oxidative stress and apoptosis. Biochem Biophys Res Commun. 2022;627:45-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 19. | Hu X, Yu SP, Fraser JL, Lu Z, Ogle ME, Wang JA, Wei L. Transplantation of hypoxia-preconditioned mesenchymal stem cells improves infarcted heart function via enhanced survival of implanted cells and angiogenesis. J Thorac Cardiovasc Surg. 2008;135:799-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 456] [Cited by in RCA: 478] [Article Influence: 26.6] [Reference Citation Analysis (0)] |
| 20. | Zhao Y, Xiong W, Li C, Zhao R, Lu H, Song S, Zhou Y, Hu Y, Shi B, Ge J. Hypoxia-induced signaling in the cardiovascular system: pathogenesis and therapeutic targets. Signal Transduct Target Ther. 2023;8:431. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 146] [Reference Citation Analysis (0)] |
| 21. | Zhuo H, Chen Y, Zhao G. Advances in application of hypoxia-preconditioned mesenchymal stem cell-derived exosomes. Front Cell Dev Biol. 2024;12:1446050. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 19] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 22. | Volz M, Wyse-Sookoo KR, Travascio F, Huang CY, Best TM. Mechanobiological Approaches for Stimulating Chondrogenesis of Stem Cells. Stem Cells Dev. 2022;31:460-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 23. | Haneef K, Lila N, Benadda S, Legrand F, Carpentier A, Chachques JC. Development of bioartificial myocardium by electrostimulation of 3D collagen scaffolds seeded with stem cells. Heart Int. 2012;7:e14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 24. | Huang Y, Qian JY, Cheng H, Li XM. Effects of shear stress on differentiation of stem cells into endothelial cells. World J Stem Cells. 2021;13:894-913. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 30] [Article Influence: 6.0] [Reference Citation Analysis (1)] |
| 25. | Correa-Meyer E, Pesce L, Guerrero C, Sznajder JI. Cyclic stretch activates ERK1/2 via G proteins and EGFR in alveolar epithelial cells. Am J Physiol Lung Cell Mol Physiol. 2002;282:L883-L891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 95] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 26. | Islam R, Hong Z. YAP/TAZ as mechanobiological signaling pathway in cardiovascular physiological regulation and pathogenesis. Mechanobiol Med. 2024;2:100085. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 27. | Raman N, Imran SAM, Ahmad Amin Noordin KB, Wan Kamarul Zaman WS, Nordin F. Mechanotransduction of mesenchymal stem cells (MSCs) during cardiomyocytes differentiation. Heliyon. 2022;8:e11624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 28. | Ullah M, Liu DD, Thakor AS. Mesenchymal Stromal Cell Homing: Mechanisms and Strategies for Improvement. iScience. 2019;15:421-438. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 381] [Cited by in RCA: 405] [Article Influence: 57.9] [Reference Citation Analysis (0)] |
| 29. | Matta A, Nader V, Lebrin M, Gross F, Prats AC, Cussac D, Galinier M, Roncalli J. Pre-Conditioning Methods and Novel Approaches with Mesenchymal Stem Cells Therapy in Cardiovascular Disease. Cells. 2022;11:1620. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 30. | Pasha Z, Wang Y, Sheikh R, Zhang D, Zhao T, Ashraf M. Preconditioning enhances cell survival and differentiation of stem cells during transplantation in infarcted myocardium. Cardiovasc Res. 2008;77:134-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 222] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 31. | Lin H, Ling Y, Pan J, Gong H. Therapeutic effects of erythropoietin expressed in mesenchymal stem cells for dilated cardiomyopathy in rat. Biochem Biophys Res Commun. 2019;517:575-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 32. | Kang M, Huang CC, Gajendrareddy P, Lu Y, Shirazi S, Ravindran S, Cooper LF. Extracellular Vesicles From TNFα Preconditioned MSCs: Effects on Immunomodulation and Bone Regeneration. Front Immunol. 2022;13:878194. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 62] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 33. | Huang X, Liang X, Han Q, Shen Y, Chen J, Li Z, Qiu J, Gao X, Hong Y, Lin F, Li W, Li X, Zhang Y. Pretreatment with growth differentiation factor 15 augments cardioprotection by mesenchymal stem cells in myocardial infarction by improving their survival. Stem Cell Res Ther. 2024;15:412. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (1)] |
| 34. | Nouri F, Nematollahi-Mahani SN, Sharifi AM. Preconditioning of Mesenchymal Stem Cells with Non-Toxic Concentration of Hydrogen Peroxide Against Oxidative Stress Induced Cell Death: The Role of Hypoxia-Inducible Factor-1. Adv Pharm Bull. 2019;9:76-83. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 35. | Guo L, Du J, Yuan DF, Zhang Y, Zhang S, Zhang HC, Mi JW, Ning YL, Chen MJ, Wen DL, Sun JH, Liu D, Zeng L, Zhang A, Jiang J, Huang H. Optimal H(2)O(2) preconditioning to improve bone marrow mesenchymal stem cells' engraftment in wound healing. Stem Cell Res Ther. 2020;11:434. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 36. | Jalali L, Allahveisie A, Rezaei S, Ravanyar L, Kiasatfar J, Rezaie MJ, Raoofi A. Effect of preconditioning of human umbilical cord mesenchymal stem cells with hydrogen peroxide on the therapeutic potential of MSCs in the cyclophosphamide -induced premature ovarian failure mice model. Taiwan J Obstet Gynecol. 2023;62:667-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 37. | Garrido-Pascual P, Alonso-Varona A, Castro B, Burón M, Palomares T. H(2)O(2)-preconditioned human adipose-derived stem cells (HC016) increase their resistance to oxidative stress by overexpressing Nrf2 and bioenergetic adaptation. Stem Cell Res Ther. 2020;11:335. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 38. | Burón M, Palomares T, Garrido-Pascual P, Herrero de la Parte B, García-Alonso I, Alonso-Varona A. Conditioned Medium from H(2)O(2)-Preconditioned Human Adipose-Derived Stem Cells Ameliorates UVB-Induced Damage to Human Dermal Fibroblasts. Antioxidants (Basel). 2022;11:2011. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 39. | Mahmoudi T, Abdolmohammadi K, Bashiri H, Mohammadi M, Rezaie MJ, Fathi F, Fakhari S, Rezaee MA, Jalili A, Rahmani MR, Tayebi L. Hydrogen Peroxide Preconditioning Promotes Protective Effects of Umbilical Cord Vein Mesenchymal Stem Cells in Experimental Pulmonary Fibrosis. Adv Pharm Bull. 2020;10:72-80. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 40. | Li D, Xu Y, Gao CY, Zhai YP. Adaptive protection against damage of preconditioning human umbilical cord-derived mesenchymal stem cells with hydrogen peroxide. Genet Mol Res. 2014;13:7304-7317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 41. | Khatlani T, Algudiri D, Alenzi R, Al Subayyil AM, Abomaray FM, Bahattab E, AlAskar AS, Kalionis B, El-Muzaini MF, Abumaree MH. Preconditioning by Hydrogen Peroxide Enhances Multiple Properties of Human Decidua Basalis Mesenchymal Stem/Multipotent Stromal Cells. Stem Cells Int. 2018;2018:6480793. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 42. | Boopathy AV, Pendergrass KD, Che PL, Yoon YS, Davis ME. Oxidative stress-induced Notch1 signaling promotes cardiogenic gene expression in mesenchymal stem cells. Stem Cell Res Ther. 2013;4:43. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 74] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 43. | O'Leary MF. Mesenchymal stem cell pre-treatment with cytokines and hydrogen peroxide modifies their adhesion to cardiac endothelium and murine heart sections AND A preliminary study of the molecular regulation of placental growth factor and vascular endothelial growth factor in murine preadipocytes. College of Medical and Dental Sciences University of Birmingham. 2014. |
| 44. | Angeloni C, Motori E, Fabbri D, Malaguti M, Leoncini E, Lorenzini A, Hrelia S. H2O2 preconditioning modulates phase II enzymes through p38 MAPK and PI3K/Akt activation. Am J Physiol Heart Circ Physiol. 2011;300:H2196-H2205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 52] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 45. | Garrido Pascual P, Elucidation of the molecular and bionergetic mechanisms underlying the resistance to oxidatives stress and the pro-recovery effect of H2O2- preconditioned adipose-derived stem cells. Universidad del País Vasco-Euskal Herriko Unibertsitatea. 2020. |
| 46. | Sadidi M, Lentz SI, Feldman EL. Hydrogen peroxide-induced Akt phosphorylation regulates Bax activation. Biochimie. 2009;91:577-585. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 66] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 47. | Vasanthan J, Gurusamy N, Rajasingh S, Sigamani V, Kirankumar S, Thomas EL, Rajasingh J. Role of Human Mesenchymal Stem Cells in Regenerative Therapy. Cells. 2020;10:54. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 104] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 48. | Zhang J, Chen GH, Wang YW, Zhao J, Duan HF, Liao LM, Zhang XZ, Chen YD, Chen H. Hydrogen peroxide preconditioning enhances the therapeutic efficacy of Wharton's Jelly mesenchymal stem cells after myocardial infarction. Chin Med J (Engl). 2012;125:3472-3478. [PubMed] |
| 49. | Castro B, Martinez-Redondo D, Gartzia I, Alonso-Varona A, Garrido P, Palomares T. Cryopreserved H(2) O(2) -preconditioned human adipose-derived stem cells exhibit fast post-thaw recovery and enhanced bioactivity against oxidative stress. J Tissue Eng Regen Med. 2019;13:328-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 50. | Han P, Zhou XH, Chang N, Xiao CL, Yan S, Ren H, Yang XZ, Zhang ML, Wu Q, Tang B, Diao JP, Zhu X, Zhang C, Li CY, Cheng H, Xiong JW. Hydrogen peroxide primes heart regeneration with a derepression mechanism. Cell Res. 2014;24:1091-1107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 112] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 51. | Cerrada I, Ruiz-Saurí A, Carrero R, Trigueros C, Dorronsoro A, Sanchez-Puelles JM, Diez-Juan A, Montero JA, Sepúlveda P. Hypoxia-inducible factor 1 alpha contributes to cardiac healing in mesenchymal stem cells-mediated cardiac repair. Stem Cells Dev. 2013;22:501-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 60] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 52. | Pankajakshan D, Agrawal DK. Mesenchymal Stem Cell Paracrine Factors in Vascular Repair and Regeneration. J Biomed Technol Res. 2014;1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 78] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 53. | Dave A, Kar S, Banerjee ER. Effect of CoCl2 or H2O2 pre-conditioned mesenchymal stem cells in a mouse model of pulmonary fibrosis. Biomed Res Ther. 2018;5:2208-2222. [RCA] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 54. | Pendergrass KD, Boopathy AV, Seshadri G, Maiellaro-Rafferty K, Che PL, Brown ME, Davis ME. Acute preconditioning of cardiac progenitor cells with hydrogen peroxide enhances angiogenic pathways following ischemia-reperfusion injury. Stem Cells Dev. 2013;22:2414-2424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 46] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 55. | Li Q, Wang Y, Deng Z. Pre-conditioned mesenchymal stem cells: a better way for cell-based therapy. Stem Cell Res Ther. 2013;4:63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 54] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 56. | Li Y, Hiroi Y, Liao JK. Notch signaling as an important mediator of cardiac repair and regeneration after myocardial infarction. Trends Cardiovasc Med. 2010;20:228-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 78] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 57. | Liang J, Wu M, Chen C, Mai M, Huang J, Zhu P. Roles of Reactive Oxygen Species in Cardiac Differentiation, Reprogramming, and Regenerative Therapies. Oxid Med Cell Longev. 2020;2020:2102841. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 58. | Dreger H, Westphal K, Weller A, Baumann G, Stangl V, Meiners S, Stangl K. Nrf2-dependent upregulation of antioxidative enzymes: a novel pathway for proteasome inhibitor-mediated cardioprotection. Cardiovasc Res. 2009;83:354-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 161] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 59. | Ye S, Zhao T, Zhang W, Tang Z, Gao C, Ma Z, Xiong JW, Peng J, Tan WQ, Chen J. p53 isoform Δ113p53 promotes zebrafish heart regeneration by maintaining redox homeostasis. Cell Death Dis. 2020;11:568. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 60. | Qin F, Siwik DA, Lancel S, Zhang J, Kuster GM, Luptak I, Wang L, Tong X, Kang YJ, Cohen RA, Colucci WS. Hydrogen peroxide-mediated SERCA cysteine 674 oxidation contributes to impaired cardiac myocyte relaxation in senescent mouse heart. J Am Heart Assoc. 2013;2:e000184. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 101] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 61. | Sartoretto JL, Kalwa H, Pluth MD, Lippard SJ, Michel T. Hydrogen peroxide differentially modulates cardiac myocyte nitric oxide synthesis. Proc Natl Acad Sci U S A. 2011;108:15792-15797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 73] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 62. | Bardaweel SK, Gul M, Alzweiri M, Ishaqat A, ALSalamat HA, Bashatwah RM. Reactive Oxygen Species: the Dual Role in Physiological and Pathological Conditions of the Human Body. Eurasian J Med. 2018;50:193-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 223] [Article Influence: 27.9] [Reference Citation Analysis (0)] |
| 63. | Andrés CMC, Pérez de la Lastra JM, Juan CA, Plou FJ, Pérez-lebeña E. Chemistry of Hydrogen Peroxide Formation and Elimination in Mammalian Cells, and Its Role in Various Pathologies. Stresses. 2022;2:256-274. [RCA] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 64. | Averill-Bates D. Reactive oxygen species and cell signaling. Review. Biochim Biophys Acta Mol Cell Res. 2024;1871:119573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 153] [Article Influence: 76.5] [Reference Citation Analysis (0)] |
| 65. | Jose E, March-Steinman W, Wilson BA, Shanks L, Parkinson C, Alvarado-Cruz I, Sweasy JB, Paek AL. Temporal coordination of the transcription factor response to H(2)O(2) stress. Nat Commun. 2024;15:3440. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 26] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 66. | Beisaw A, Kuenne C, Guenther S, Dallmann J, Wu CC, Bentsen M, Looso M, Stainier DYR. AP-1 Contributes to Chromatin Accessibility to Promote Sarcomere Disassembly and Cardiomyocyte Protrusion During Zebrafish Heart Regeneration. Circ Res. 2020;126:1760-1778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 119] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 67. | Hou J, Wang L, Long H, Wu H, Wu Q, Zhong T, Chen X, Zhou C, Guo T, Wang T. Hypoxia preconditioning promotes cardiac stem cell survival and cardiogenic differentiation in vitro involving activation of the HIF-1α/apelin/APJ axis. Stem Cell Res Ther. 2017;8:215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 68. | Hammad M, Raftari M, Cesário R, Salma R, Godoy P, Emami SN, Haghdoost S. Roles of Oxidative Stress and Nrf2 Signaling in Pathogenic and Non-Pathogenic Cells: A Possible General Mechanism of Resistance to Therapy. Antioxidants (Basel). 2023;12:1371. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 131] [Reference Citation Analysis (0)] |
| 69. | Ma K, Miao L, Li B, Yu W, Liu F, Liu K, Li Y, Huang C, Yang Z. Mechanism of action of Nrf2 and its related natural regulators in rheumatoid arthritis. J Orthop Surg Res. 2024;19:759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 70. | Dai X, Yan X, Wintergerst KA, Cai L, Keller BB, Tan Y. Nrf2: Redox and Metabolic Regulator of Stem Cell State and Function. Trends Mol Med. 2020;26:185-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 157] [Article Influence: 26.2] [Reference Citation Analysis (0)] |
| 71. | Márton M, Tihanyi N, Gyulavári P, Bánhegyi G, Kapuy O. NRF2-regulated cell cycle arrest at early stage of oxidative stress response mechanism. PLoS One. 2018;13:e0207949. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 72. | Park PSU, Mun SH, Zeng SL, Kim H, Bae S, Park-Min KH. NRF2 Is an Upstream Regulator of MYC-Mediated Osteoclastogenesis and Pathological Bone Erosion. Cells. 2020;9:2133. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 73. | Ishii T, Warabi E, Mann GE. Mechanisms underlying Nrf2 nuclear translocation by non-lethal levels of hydrogen peroxide: p38 MAPK-dependent neutral sphingomyelinase2 membrane trafficking and ceramide/PKCζ/CK2 signaling. Free Radic Biol Med. 2022;191:191-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 31] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 74. | Covas G, Marinho HS, Cyrne L, Antunes F. Activation of Nrf2 by H2O2: de novo synthesis versus nuclear translocation. Methods Enzymol. 2013;528:157-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 53] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 75. | Yang X, Fang Y, Hou J, Wang X, Li J, Li S, Zheng X, Liu Y, Zhang Z. The heart as a target for deltamethrin toxicity: Inhibition of Nrf2/HO-1 pathway induces oxidative stress and results in inflammation and apoptosis. Chemosphere. 2022;300:134479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 56] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 76. | Zoccarato A, Smyrnias I, Reumiller CM, Hafstad AD, Chong M, Richards DA, Santos CXC, Visnagri A, Verma S, Bromage DI, Zhang M, Zhang X, Sawyer G, Thompson R, Shah AM. NRF2 activation in the heart induces glucose metabolic reprogramming and reduces cardiac dysfunction via upregulation of the pentose phosphate pathway. Cardiovasc Res. 2025;121:339-352. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 17] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 77. | Hong Y, Boiti A, Vallone D, Foulkes NS. Reactive Oxygen Species Signaling and Oxidative Stress: Transcriptional Regulation and Evolution. Antioxidants (Basel). 2024;13:312. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 248] [Cited by in RCA: 297] [Article Influence: 148.5] [Reference Citation Analysis (0)] |
| 78. | Karin M, Liu Zg, Zandi E. AP-1 function and regulation. Curr Opin Cell Biol. 1997;9:240-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2004] [Cited by in RCA: 2107] [Article Influence: 72.7] [Reference Citation Analysis (0)] |
| 79. | Pinkus R, Weiner LM, Daniel V. Role of oxidants and antioxidants in the induction of AP-1, NF-kappaB, and glutathione S-transferase gene expression. J Biol Chem. 1996;271:13422-13429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 344] [Cited by in RCA: 346] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 80. | Eferl R, Wagner EF. AP-1: a double-edged sword in tumorigenesis. Nat Rev Cancer. 2003;3:859-868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1583] [Cited by in RCA: 1722] [Article Influence: 74.9] [Reference Citation Analysis (0)] |
| 81. | Windak R, Müller J, Felley A, Akhmedov A, Wagner EF, Pedrazzini T, Sumara G, Ricci R. The AP-1 transcription factor c-Jun prevents stress-imposed maladaptive remodeling of the heart. PLoS One. 2013;8:e73294. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 57] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 82. | Eriksson M, Leppä S. Mitogen-activated protein kinases and activator protein 1 are required for proliferation and cardiomyocyte differentiation of P19 embryonal carcinoma cells. J Biol Chem. 2002;277:15992-16001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 65] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 83. | Murray TV, Smyrnias I, Shah AM, Brewer AC. NADPH oxidase 4 regulates cardiomyocyte differentiation via redox activation of c-Jun protein and the cis-regulation of GATA-4 gene transcription. J Biol Chem. 2013;288:15745-15759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 46] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 84. | López-Camarillo C, Ocampo EA, Casamichana ML, Pérez-Plasencia C, Alvarez-Sánchez E, Marchat LA. Protein kinases and transcription factors activation in response to UV-radiation of skin: implications for carcinogenesis. Int J Mol Sci. 2012;13:142-172. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 101] [Cited by in RCA: 119] [Article Influence: 7.9] [Reference Citation Analysis (7)] |
| 85. | Kikuta K, Masamune A, Satoh M, Suzuki N, Satoh K, Shimosegawa T. Hydrogen peroxide activates activator protein-1 and mitogen-activated protein kinases in pancreatic stellate cells. Mol Cell Biochem. 2006;291:11-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 86. | Xu Y, Bradham C, Brenner DA, Czaja MJ. Hydrogen peroxide-induced liver cell necrosis is dependent on AP-1 activation. Am J Physiol. 1997;273:G795-G803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 87. | Jiang T, Qu JJ, Nishinaka T, Zhang N. Transcription factor AP-1 regulates TGF-beta(1)-induced expression of aldose reductase in cultured human mesangial cells. Nephrology (Carlton). 2008;13:212-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 88. | Guo ZY, Hao XH, Tan FF, Pei X, Shang LM, Jiang XL, Yang F. The elements of human cyclin D1 promoter and regulation involved. Clin Epigenetics. 2011;2:63-76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 50] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 89. | Zuppo DA, Missinato MA, Santana-Santos L, Li G, Benos PV, Tsang M. Foxm1 regulates cardiomyocyte proliferation in adult zebrafish after cardiac injury. Development. 2023;150:dev201163. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 21] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 90. | Basheeruddin M, Qausain S. Hypoxia-Inducible Factor 1-Alpha (HIF-1α): An Essential Regulator in Cellular Metabolic Control. Cureus. 2024;16:e63852. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 20] [Reference Citation Analysis (0)] |
| 91. | Yang M, Su H, Soga T, Kranc KR, Pollard PJ. Prolyl hydroxylase domain enzymes: important regulators of cancer metabolism. Hypoxia (Auckl). 2014;2:127-142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 92. | Bae T, Hallis SP, Kwak MK. Hypoxia, oxidative stress, and the interplay of HIFs and NRF2 signaling in cancer. Exp Mol Med. 2024;56:501-514. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 151] [Reference Citation Analysis (0)] |
| 93. | Zimna A, Kurpisz M. Hypoxia-Inducible Factor-1 in Physiological and Pathophysiological Angiogenesis: Applications and Therapies. Biomed Res Int. 2015;2015:549412. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 249] [Cited by in RCA: 444] [Article Influence: 40.4] [Reference Citation Analysis (0)] |
| 94. | Zhang J, Gao P, Chang WR, Song JY, An FY, Wang YJ, Xiao ZP, Jin H, Zhang XH, Yan CL. The role of HIF-1α in hypoxic metabolic reprogramming in osteoarthritis. Pharmacol Res. 2025;213:107649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 19] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 95. | Kuiper C, Dachs GU, Currie MJ, Vissers MC. Intracellular ascorbate enhances hypoxia-inducible factor (HIF)-hydroxylase activity and preferentially suppresses the HIF-1 transcriptional response. Free Radic Biol Med. 2014;69:308-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 95] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 96. | Xie M, Roy R. Increased levels of hydrogen peroxide induce a HIF-1-dependent modification of lipid metabolism in AMPK compromised C. elegans dauer larvae. Cell Metab. 2012;16:322-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 61] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 97. | Chang S, Jiang X, Zhao C, Lee C, Ferriero DM. Exogenous low dose hydrogen peroxide increases hypoxia-inducible factor-1alpha protein expression and induces preconditioning protection against ischemia in primary cortical neurons. Neurosci Lett. 2008;441:134-138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 52] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 98. | Sun J, Shen H, Shao L, Teng X, Chen Y, Liu X, Yang Z, Shen Z. HIF-1α overexpression in mesenchymal stem cell-derived exosomes mediates cardioprotection in myocardial infarction by enhanced angiogenesis. Stem Cell Res Ther. 2020;11:373. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 213] [Article Influence: 35.5] [Reference Citation Analysis (0)] |
| 99. | He Z, Simon HU. A novel link between p53 and ROS. Cell Cycle. 2013;12:201-202. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 100. | Sablina AA, Budanov AV, Ilyinskaya GV, Agapova LS, Kravchenko JE, Chumakov PM. The antioxidant function of the p53 tumor suppressor. Nat Med. 2005;11:1306-1313. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 907] [Cited by in RCA: 884] [Article Influence: 42.1] [Reference Citation Analysis (0)] |
| 101. | Hussain SP, Amstad P, He P, Robles A, Lupold S, Kaneko I, Ichimiya M, Sengupta S, Mechanic L, Okamura S, Hofseth LJ, Moake M, Nagashima M, Forrester KS, Harris CC. p53-induced up-regulation of MnSOD and GPx but not catalase increases oxidative stress and apoptosis. Cancer Res. 2004;64:2350-2356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 279] [Cited by in RCA: 297] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 102. | Kang MY, Kim HB, Piao C, Lee KH, Hyun JW, Chang IY, You HJ. The critical role of catalase in prooxidant and antioxidant function of p53. Cell Death Differ. 2013;20:117-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 103] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 103. | Ogata FT, Branco V, Vale FF, Coppo L. Glutaredoxin: Discovery, redox defense and much more. Redox Biol. 2021;43:101975. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 109] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 104. | Budanov AV, Sablina AA, Feinstein E, Koonin EV, Chumakov PM. Regeneration of peroxiredoxins by p53-regulated sestrins, homologs of bacterial AhpD. Science. 2004;304:596-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 572] [Cited by in RCA: 607] [Article Influence: 27.6] [Reference Citation Analysis (0)] |
| 105. | Aubrey BJ, Kelly GL, Janic A, Herold MJ, Strasser A. How does p53 induce apoptosis and how does this relate to p53-mediated tumour suppression? Cell Death Differ. 2018;25:104-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 509] [Cited by in RCA: 1016] [Article Influence: 112.9] [Reference Citation Analysis (0)] |
| 106. | Pitolli C, Wang Y, Candi E, Shi Y, Melino G, Amelio I. p53-Mediated Tumor Suppression: DNA-Damage Response and Alternative Mechanisms. Cancers (Basel). 2019;11:1983. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 64] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 107. | Zhang XD, Qin ZH, Wang J. The role of p53 in cell metabolism. Acta Pharmacol Sin. 2010;31:1208-1212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 100] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 108. | Yuan A, Yu CJ, Luh KT, Kuo SH, Lee YC, Yang PC. Aberrant p53 expression correlates with expression of vascular endothelial growth factor mRNA and interleukin-8 mRNA and neoangiogenesis in non-small-cell lung cancer. J Clin Oncol. 2002;20:900-910. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 33] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 109. | Elston R, Inman GJ. Crosstalk between p53 and TGF-β Signalling. J Signal Transduct. 2012;2012:294097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 98] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 110. | Lowe JM, Menendez D, Bushel PR, Shatz M, Kirk EL, Troester MA, Garantziotis S, Fessler MB, Resnick MA. p53 and NF-κB coregulate proinflammatory gene responses in human macrophages. Cancer Res. 2014;74:2182-2192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 148] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 111. | Araki K, Ebata T, Guo AK, Tobiume K, Wolf SJ, Kawauchi K. p53 regulates cytoskeleton remodeling to suppress tumor progression. Cell Mol Life Sci. 2015;72:4077-4094. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 112. | Wang H, Yu W, Wang Y, Wu R, Dai Y, Deng Y, Wang S, Yuan J, Tan R. p53 contributes to cardiovascular diseases via mitochondria dysfunction: A new paradigm. Free Radic Biol Med. 2023;208:846-858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 22] [Reference Citation Analysis (0)] |
| 113. | Goshovska YV, Fedichkina RA, Balatskyi VV, Piven OO, Dobrzyn P, Sagach VF. Induction of Glutathione Synthesis Provides Cardioprotection Regulating NO, AMPK and PPARa Signaling in Ischemic Rat Hearts. Life (Basel). 2021;11:631. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 114. | Humpton TJ, Hall H, Kiourtis C, Nixon C, Clark W, Hedley A, Shaw R, Bird TG, Blyth K, Vousden KH. p53-mediated redox control promotes liver regeneration and maintains liver function in response to CCl(4). Cell Death Differ. 2022;29:514-526. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/