Published online Sep 26, 2024. doi: 10.4330/wjc.v16.i9.542
Revised: July 30, 2024
Accepted: August 26, 2024
Published online: September 26, 2024
Processing time: 94 Days and 15.6 Hours
The recent systematic review and meta-analysis provided a comprehensive focus on the current state of cardiac resynchronization therapy (CRT). The authors determined the feasibility of physiological left bundle branch area pacing (LBB
Core Tip: In heart failure, conduction defects, such as left bundle branch block, are common and result in regionally delayed electrical activation. Traditional pacing mo
- Citation: Caruzzo CA, Rigamonti E, Scopigni FR. Left bundle branch area pacing: A new era of cardiac resynchronization therapy? World J Cardiol 2024; 16(9): 542-545
- URL: https://www.wjgnet.com/1949-8462/full/v16/i9/542.htm
- DOI: https://dx.doi.org/10.4330/wjc.v16.i9.542
Cardiac resynchronization therapy (CRT) with biventricular pacing (BiVP) is an established therapy for patients with left ventricular ejection fraction ≤ 35%, heart failure symptoms, and left bundle branch block with a QRS duration ≥ 150 ms or expected frequent ventricular pacing of > 20%-40%[1-4]. Over the last 25 years several randomized controlled trials have shown that CRT with BiVP reduces heart failure hospitalization (HFH) and all-cause mortality[4-7].
Left bundle branch area pacing (LBBAP) is a newer procedure for CRT that has shown promising results. A re
LBBAP is the most recent technique established for conduction system pacing. It overcame several limitations of its predecessor, His-bundle pacing (HBP). The stimulation of the left bundle branch often shows lower thresholds, resulting in longer battery life compared to HBP[10]. Despite the initial success of the first conduction system pacing through HBP, widespread use of CRT was hindered by issues such as lead instability, dislodgements, a steep learning curve, and rapid battery depletion.
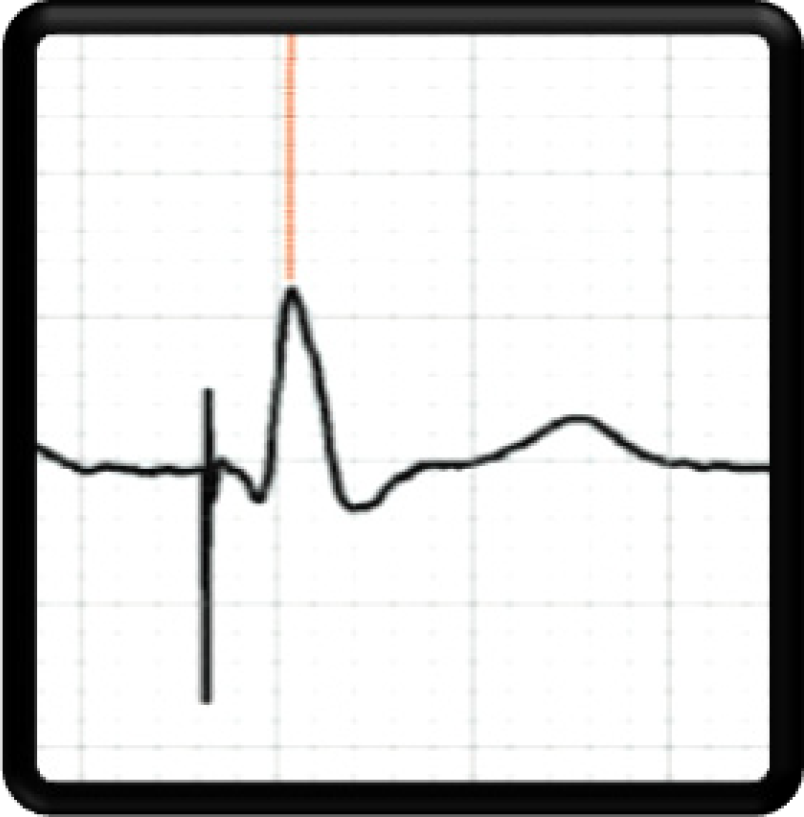
The aim of this editorial was to expound on the recent meta-analysis regarding LBBAP by Yasmin et al[11] in the World Journal of Cardiology. LBBAP is a safe and effective means for achieving physiological conduction system pacing. It involves the placement of the pacing lead tip into the left side of the interventricular septum, 15-20 mm beyond the tricuspid annulus on fluoroscopic imaging[12]. Appropriate lead placement is confirmed through various criteria, including left ventricle activation time < 80 ms and V6-V1 interpeak interval > 44 ms[13]. Left ventricle activation time is illustrated in Figure 1.
The current literature suggests that conduction system pacing is a valid alternative in terms of safety[14]. LBBAP results in a lower risk of all-cause mortality or HFH compared to BiVP and left ventricular septal pacing (LVSP), while LVSP and BiVP have a similar risk. LVSP had a higher risk of all-cause mortality compared to both LBBAP and BiVP. The echocardiographic response and super response were highest for patients treated with LBBP[15].
Choosing the ideal site for CRT is often difficult using conduction system pacing, especially in patients without left bundle branch block due to the risk of conduction block progression distal to the pacing site. Therefore, HBP and epicardial left ventricular (LV) pacing or LBBAP and epicardial LV pacing may be better options to optimize results in patients without left bundle branch block[16].
Yasmin et al[11] reported in the meta-analysis that the baseline characteristics of the population were well-balanced according to sex (49.7% female). Subzposh et al[17] reported that females are better responders to resynchronization therapy. The meta-analysis included 389 patients with heart failure and left bundle branch block from six studies. Only one of the studies was randomized, and the median follow-up was 9 months. QRS duration was the primary outcome and was significantly reduced by LBBAP. This result is fundamentally important in corroborating the effectiveness of direct stimulation of the conduction system.
The propagation speed through the myocardium is 0.15-1.00 m/s, which is 25% of the physiological speed of the conduction pathways of the heart (3.00-4.00 m/s)[18], highlighting the inherent superiority of physiological pacing through the native conduction system. QRS duration reduction leads to reverse remodeling and avoids interventricular mechanical delay. Patients with greater QRS shortening (> 14 ms) after CRT have lower mortality and hospitalizations compared to those with smaller QRS reductions[19]. Implementing a general strategy of CRT device optimization for shorter QRS duration should lead to better clinical outcomes.
Secondary outcomes included pacing threshold, NYHA functional class, B-type natriuretic peptide level, and echocardiographic parameters such as left ventricular ejection fraction, left ventricular end-diastolic diameter, and left ventricular end-systolic diameter. Five of the included studies reported a significantly reduced pacing threshold in LBBAP compared to BiVP, which also remained considerably lower at the 6-month and 12-month follow-up.
We are in full support of the conclusions of Yasmin et al[11] about LBBAP as a promising modality, and we await with fervid anticipation the results of ongoing randomized controlled trials. The advantages of LBBAP over BiVP have emerged in recent years and include better ventricular electrical and mechanical resynchronization and improvements in cardiac function, NYHA function class, and clinical outcomes.
Despite these encouraging results, widespread adoption of LBBAP depends on the improvement of tools and further validation of its efficacy in large randomized clinical trials. Furthermore, randomized clinical trials with long-term follow-up are necessary to confirm the clinical benefits of conduction system pacing CRT compared with BiVP in CRT can
| 1. | Cheng A, Helm RH, Abraham TP. Pathophysiological mechanisms underlying ventricular dyssynchrony. Europace. 2009;11 Suppl 5:v10-v14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 41] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 2. | Zhang S, Zhou X, Gold MR. Left Bundle Branch Pacing: JACC Review Topic of the Week. J Am Coll Cardiol. 2019;74:3039-3049. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 161] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 3. | Cleland JG, Daubert JC, Erdmann E, Freemantle N, Gras D, Kappenberger L, Tavazzi L; Cardiac Resynchronization-Heart Failure (CARE-HF) Study Investigators. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005;352:1539-1549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4673] [Cited by in RCA: 4596] [Article Influence: 218.9] [Reference Citation Analysis (0)] |
| 4. | Bristow MR, Saxon LA, Boehmer J, Krueger S, Kass DA, De Marco T, Carson P, DiCarlo L, DeMets D, White BG, DeVries DW, Feldman AM; Comparison of Medical Therapy, Pacing, and Defibrillation in Heart Failure (COMPANION) Investigators. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med. 2004;350:2140-2150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4324] [Cited by in RCA: 4202] [Article Influence: 191.0] [Reference Citation Analysis (0)] |
| 5. | Jones S, Lumens J, Sohaib SMA, Finegold JA, Kanagaratnam P, Tanner M, Duncan E, Moore P, Leyva F, Frenneaux M, Mason M, Hughes AD, Francis DP, Whinnett ZI; BRAVO Investigators. Cardiac resynchronization therapy: mechanisms of action and scope for further improvement in cardiac function. Europace. 2017;19:1178-1186. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Sapp JL, Sivakumaran S, Redpath CJ, Khan H, Parkash R, Exner DV, Healey JS, Thibault B, Sterns LD, Lam NHN, Manlucu J, Mokhtar A, Sumner G, McKinlay S, Kimber S, Mondesert B, Talajic M, Rouleau J, McCarron CE, Wells G, Tang ASL; RAFT Long-Term Study Team. Long-Term Outcomes of Resynchronization-Defibrillation for Heart Failure. N Engl J Med. 2024;390:212-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 7. | Authors/Task Force Members; McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, Cleland JGF, Coats AJS, Crespo-Leiro MG, Farmakis D, Gilard M, Heymans S, Hoes AW, Jaarsma T, Jankowska EA, Lainscak M, Lam CSP, Lyon AR, McMurray JJV, Mebazaa A, Mindham R, Muneretto C, Francesco Piepoli M, Price S, Rosano GMC, Ruschitzka F, Kathrine Skibelund A; ESC Scientific Document Group. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2022;24:4-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 1517] [Article Influence: 379.3] [Reference Citation Analysis (2)] |
| 8. | Vijayaraman P, Sharma PS, Cano Ó, Ponnusamy SS, Herweg B, Zanon F, Jastrzebski M, Zou J, Chelu MG, Vernooy K, Whinnett ZI, Nair GM, Molina-Lerma M, Curila K, Zalavadia D, Haseeb A, Dye C, Vipparthy SC, Brunetti R, Moskal P, Ross A, van Stipdonk A, George J, Qadeer YK, Mumtaz M, Kolominsky J, Zahra SA, Golian M, Marcantoni L, Subzposh FA, Ellenbogen KA. Comparison of Left Bundle Branch Area Pacing and Biventricular Pacing in Candidates for Resynchronization Therapy. J Am Coll Cardiol. 2023;82:228-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 181] [Article Influence: 60.3] [Reference Citation Analysis (0)] |
| 9. | Fu Y, Liu P, Jin L, Li Y, Zhang Y, Qin X, Zheng Q. Left bundle branch area pacing: A promising modality for cardiac resynchronization therapy. Front Cardiovasc Med. 2022;9:901046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Padala SK, Master VM, Terricabras M, Chiocchini A, Garg A, Kron J, Shepard R, Kalahasty G, Azizi Z, Tsang B, Khaykin Y, Pantano A, Koneru JN, Ellenbogen KA, Verma A. Initial Experience, Safety, and Feasibility of Left Bundle Branch Area Pacing: A Multicenter Prospective Study. JACC Clin Electrophysiol. 2020;6:1773-1782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 91] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 11. | Yasmin F, Moeed A, Ochani RK, Raheel H, Awan MAE, Liaquat A, Saleem A, Aamir M, Hawwa N, Surani S. Left bundle branch pacing vs biventricular pacing in heart failure patients with left bundle branch block: A systematic review and meta-analysis. World J Cardiol. 2024;16:40-48. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 12. | Lewis NDH, Cheung CC. Left Bundle Branch Area Pacing Leading the Way: Emerging Trends in Cardiac Pacing. Can J Cardiol. 2024;S0828-282X(24)00204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Ponnusamy SS, Arora V, Namboodiri N, Kumar V, Kapoor A, Vijayaraman P. Left bundle branch pacing: A comprehensive review. J Cardiovasc Electrophysiol. 2020;31:2462-2473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 130] [Article Influence: 21.7] [Reference Citation Analysis (0)] |
| 14. | Vijayaraman P, Pokharel P, Subzposh FA, Oren JW, Storm RH, Batul SA, Beer DA, Hughes G, Leri G, Manganiello M, Jastremsky JL, Mroczka K, Johns AM, Mascarenhas V. His-Purkinje Conduction System Pacing Optimized Trial of Cardiac Resynchronization Therapy vs Biventricular Pacing: HOT-CRT Clinical Trial. JACC Clin Electrophysiol. 2023;9:2628-2638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 55] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 15. | Zhu H, Qin C, Du A, Wang Q, He C, Zou F, Li X, Tao J, Wang C, Liu Z, Xue S, Zeng J, Qian Z, Wang Y, Hou X, Ellenbogen KA, Gold MR, Yao Y, Zou J, Fan X. Comparisons of long-term clinical outcomes with left bundle branch pacing, left ventricular septal pacing, and biventricular pacing for cardiac resynchronization therapy. Heart Rhythm. 2024;21:1342-1353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 36] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 16. | Batta A, Hatwal J. Left bundle branch pacing set to outshine biventricular pacing for cardiac resynchronization therapy? World J Cardiol. 2024;16:186-190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 17. | Subzposh FA, Sharma PS, Cano Ó, Ponnusamy SS, Herweg B, Zanon F, Jastrzebski M, Zou J, Chelu MG, Vernooy K, Whinnett ZI, Nair GM, Molina-Lerma M, Curila K, Ellenbogen KA, Vijayaraman P. Sex-Specific Outcomes of LBBAP Versus Biventricular Pacing: Results From I-CLAS. JACC Clin Electrophysiol. 2024;10:96-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 18. | Prinzen FW, Hunter WC, Wyman BT, McVeigh ER. Mapping of regional myocardial strain and work during ventricular pacing: experimental study using magnetic resonance imaging tagging. J Am Coll Cardiol. 1999;33:1735-1742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 477] [Cited by in RCA: 468] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 19. | Borgquist R, Marinko S, Platonov PG, Wang L, Chaudhry U, Brandt J, Mörtsell D. Maximizing QRS duration reduction in contemporary cardiac resynchronization therapy is feasible and shorter QRS duration is associated with better clinical outcome. J Interv Card Electrophysiol. 2023;66:1799-1806. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/