Published online Sep 26, 2024. doi: 10.4330/wjc.v16.i9.522
Revised: August 18, 2024
Accepted: August 28, 2024
Published online: September 26, 2024
Processing time: 66 Days and 0.3 Hours
Coronary artery diseases can cause myocardial ischemia and hypoxia, angina pectoris, myocardial infarction, arrhythmia, and even sudden death led to inflight incapacitation of aircrew. As the main cause of grounding due to illness, they severe threats to the health and fighting strength of military aircrew. Early war
To figure out the flight factors and clinical characteristics of military aircrew with abnormal results of coronary artery computed tomographic angiography (CTA), thereby rendering theoretical references for clinical aeromedical support of military flying personnel.
The clinical data of 15 flying personnel who received physical examinations in a military medical center from December 2020 to June 2023 and were diagnosed with coronary artery diseases by coronary artery CTA were collected and retrospectively analyzed, and a descriptive statistical analysis was conducted on their onset age, aircraft type and clinical data.
The 15 military flying personnel diagnosed with coronary artery diseases by coronary artery CTA were composed of 9 pilots, 1 navigator and 5 air combat service workers. Multi-vessel disease was detected in 9 flying personnel, among which 8 (88.9%) were pilots. Flying personnel with multi-vessel disease had higher content of cholesterol, low-density lipoprotein cholesterol and apolipoprotein B than those with single-vessel disease.
Coronary artery diseases are the major heart disease for the grounding of flying personnel due to illness, which can lead to inflight incapacitation. Coronary artery CTA is conducive to early detection and early intervention treatment of such diseases in clinic.
Core Tip: Early warning and intervention of diseases leading to inflight incapacitation is not only the most crucial task in clinical aeromedical work, but also the key link to reduce the grounding rate, ensure the fighting strength of troops and extend the life cycle of pilots. Construction of early warning model, accurate early warning and early intervention of key parameters in the results of routine physical examination are of great military significance for ensuring the health improvement of flying personnel.
- Citation: Zeng J, Zhao Y, Gao D, Lu X, Dong JJ, Liu YB, Shen B. Medical appraisal of Chinese military aircrew with abnormal results of coronary computed tomographic angiography. World J Cardiol 2024; 16(9): 522-530
- URL: https://www.wjgnet.com/1949-8462/full/v16/i9/522.htm
- DOI: https://dx.doi.org/10.4330/wjc.v16.i9.522
Coronary artery diseases can not only cause severe complications such as myocardial ischemia and hypoxia, angina pectoris, myocardial infarction, arrhythmia, and even sudden death, but also lead to inflight incapacitation of flying personnel, which also serve as the main cause of grounding due to illness[1-3]. As a result, they act as severe threats to the health and fighting strength of military aircrew. Early warning in an early and accurate manner and early intervention of diseases possibly resulting in inflight incapacitation are key emphases of aeromedical support in clinic. A recent study in a military medical center reported that 15 military flying personnel hospitalized for physical examination had abnormal results of coronary artery computed tomographic angiography (CTA), ranking second in the disease spectra of temporary disqualification from flying. In this study, the clinical data of such personnel were retrospectively analyzed to understand the characteristics of coronary artery diseases in them and their relationships with flight factors, avoiding severe adverse events in flying (Table 1). It is now reported as follows.
| Aircraft type (aviation duty) | n | Proportion (%) | Age (year) | Median age (year) | Flying time (hour) | |
| Pilot | Fighter | 1 | 6.7 | 40 | 40.0 | 1800 |
| Fighter plane (Bomber) | 1 | 6.7 | 47 | 47.0 | 3000 | |
| Bomber | 1 | 6.7 | 49 | 49.0 | 3200 | |
| Transport plane | 2 | 13.3 | 48-55 | 51.5 ± 4.9 | 5000-5600 | |
| Primary trainer | 1 | 6.7 | 49 | 49.0 | 3000 | |
| Helicopter | 3 | 20.0 | 48-51 | 50.0 ± 1.7 | 2600-3100 | |
| Navigator | 1 | 6.7 | 50 | 50.0 | 4000 | |
| Air combat service worker | 5 | 33.3 | 42-56 | 52.0 ± 5.8 | 2100-5000 | |
The enrolled flying personnel were assigned into a single-vessel disease group and a multi-vessel disease group based on the results of coronary artery CTA. Peripheral venous blood was harvested from the subjects in the two groups for all-item blood lipid test, and carotid artery ultrasound examination, coronary artery CTA and angiography were implemented. Then, high-risk factors for coronary atherosclerosis found in the above test and examinations were used as observation indicators. Besides, comparisons and analyses were conducted on these indicators between the two groups. In addition, a retrospective analysis was carried out on flying appraisal conclusions.
Peripheral venous blood (5 mL) was collected from all fasting subjects, followed by centrifugation. Next, the serum was harvested to determine the content of total cholesterol (TC), triglyceride (TG), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol [Roche Diagnostics (Suzhou) Co., Ltd. China] using an automatic biochemical analyzer (cobas-c702, Roche, Germany) according to the instructions. And the apolipoprotein (Apo)B and ApoAI. ApoB and ApoAI content was measured by turbidimetric immunoassay (Daiichi Pure Chemicals Co., Ltd., Japan) using an automatic biochemical analyzer (7600, HITACHI, Japan) according to the instructions.
Electrocardiogram (ECG)signals were collected with a 12-lead electrocardiograph (SE-1201, EDAN, Shenzhen, China), and the data were read by the machine and interpreted by two experienced physicians alone.
The intima-media thickness (IMT) of the common carotid artery was detected at 10 mm near the bifurcation of the common carotid artery by an ultrasonic diagnostic instrument (E9, GE, United States) at the probe center frequency of 7-12 MHz The IMT was the distance from the intimal interface of the lumen far from the skin to the media adventitia interface, that is, the distance between two parallel bright lines separated by relatively hypoecho on longitudinal ultrasound images of the posterior wall of the artery. The left and right common carotid arteries were measured three times, and the average was taken. IMT ≥ 1.4 mm or presence of local bulge suggested carotid plaque formation. The IMT values of bilateral common carotid arteries plus internal and external carotid arteries were measured and their sum was recorded.
Coronary artery CTA was carried out in accordance with the method of intravenous injection of Ultravist 370. The severity of coronary artery stenosis was analyzed and assessed at two mutually perpendicular projection positions. For coronary vessels with diameter stenosis, an analysis was conducted on the quantity of diseased vessels and the severity of stenosis. In addition, single-vessel and multi-vessel (double vessels and above) disease groups were set up based on the quantity of diseased vessels. The maximum stenosis in single-vessel disease was recorded, and the sum of stenosis of diseased vessels was calculated.
The systolic blood pressure and diastolic blood pressure were recorded respectively.
An imaging system (Siemens DFC or Philips FD20/10) was employed for projection of left and right coronary arteries at conventional position by virtue of Judkins method through radial artery or femoral artery, and the results were evaluated by professional physicians of cardiac catheterization for coronary heart diseases. Lesions involving 1, 2 and 3 branches of the anterior descending branch, circumflex branch and right coronary artery (RCA) were regarded as single, double and triple vessel diseases, respectively. If the left main coronary artery (LM) was involved, it was recorded as involving both the anterior descending branch and circumflex branch.
Data analysis was accomplished with SPSS 24.0 software. Measurement data were expressed by (mean ± SD). The F-test was adopted for intergroup comparison of the measurement data with skewed distribution, while for measurement data with normal distribution and homogeneity of variance, t-test was utilized for their comparisons between groups, and t' test was implemented for those with heterogeneity of variance. In terms of numeration data, sample rate pairwise comparison was completed by χ2 test or Fisher exact test. Pearson correlation analysis was carried out to clarify the correlations of systolic blood pressure, diastolic blood pressure, LDL-C, TG, TC, and serum ApoB with the sum of carotid artery IMT values, the maximum coronary artery stenosis in single vessel disease and the sum of stenosis.
It was found that the onset age and flying time showed no statistical differences between the two groups, but the flying post was obviously different between the two groups, and the incidence rate of multi-vessel disease was obviously higher than that of single vessel disease in pilots (Table 2).
| Group | n | Pilot, n (%) | Age (year) | Flying time (hour) |
| Single vessel disease group | 6 | 1 (16.7) | 49.0 ± 4.9 | 3850 ± 1282.7 |
| Multi-vessel disease group | 9 | 8 (88.9) | 48.5 ± 4.7 | 3750 ± 1125.1 |
| Statistical value | 0.199 | 0.160 | ||
| P value | 0.011 | 0.845 | 0.876 |
The multi-vessel disease group had higher levels of TC, TG, LDL-C and ApoB than single vessel disease group. However, the differences were of no statistical significance due to the small sample size (Table 3).
| Group | n | Systolic blood pressure (mmHg) | Diastolic pressure (mmHg) | TC (mmol/L) | TG (mmol/L) | LDL-C (mmol/L) | ApoB (g/L) | Sum of IMT (mm) | Number of carotid plaques (%) |
| Single vessel disease group | 6 | 134.5 ± 14.6 | 84.1± 9.4 | 4.3 ± 1.4 | 1.3 ± 0.6 | 3.0 ± 1.3 | 0.9 ± 0.4 | 4.3± 0.2 | 2 (33.3) |
| Multi-vessel disease group | 9 | 122.5 ± 10.0 | 78.2± 9.5 | 5.9 ± 3.5 | 1.6± 0.3 | 4.2 ± 3.4 | 1.3± 0.7 | 4.0± 0.6 | 2 (22.2) |
According to the results of relevant laboratory tests, oral administration of lipid-lowering and crown-expanding agents plus drug balloon dilatation was adopted for flying personnel needing treatment. The details are stated in Table 4.
| Case | ECG | Coronary artery CTA | Coronary angiography | Flying appraisal conclusion |
| 1 | Biphase or low-flat T-wave in leads V4-V6 | Small calcified plaques in the middle segment of both RCA and the posterior branch of left ventricle, without stenosis of the lumen, calcified plaques in the proximal segment of RCA, with slight stenosis of the corresponding lumen, and calcified plaques in the middle segment of LAD, with mild stenosis of the corresponding lumen | Qualified | |
| 2 | Normal | Calcified plaques in the proximal segment of RCA, with slight stenosis of the corresponding lumen, and calcified plaques in the middle segment of LAD, with slight stenosis of the corresponding lumen | Qualified | |
| 3 | Low-flat T-wave in leads V5 and V6 | Soft plaques in the proximal segment of RCA, with local mild stenosis of the lumen, mixed plaques in the proximal segment of LAD, with local mild stenosis of the lumen, and calcified plaques in the proximal segment of LCX, with local mild stenosis of the lumen | Suggested to undergo coronary angiography | Unqualified for specially permitted flying of overage pilots |
| 4 | Normal | Calcified plaques in the middle segment of LAD, with mild stenosis of the lumen, superficial myocardial bridge formation in its distal segment, and calcified plaques in the proximal and middle segments of D1 and D2, with mild stenosis of the lumen | LAD: Myocardial bridge in the middle segment, with stenosis of 40%-50% in systole, TIMI3. LCX: Stenosis of 40% of the junction between the proximal and distal segments, TIMI3. RCA: Slight stenosis of the middle segment, with rough wall, indicating the changes of arteriosclerosis, TIMI3 | Qualified |
| 5 | Normal | Soft plaques in the proximal segment of RCA, with mild stenosis of the corresponding lumen, soft plaques in the proximal segments of LAD, with mild stenosis of the corresponding lumen, and calcified plaques in the middle segment of LAD, with moderate stenosis of the corresponding lumen, and soft plaques in the proximal segments of LCX, with mild stenosis of the corresponding lumen | Suggested to undergo coronary angiography | Qualified |
| 6 | Abnormal q wave in side wall | (1) Calcified plaques in the proximal and middle segments of LAD, with local moderate stenosis (50%-70%) and distal myocardial bridge; (2) Severe stenosis of intermediate branch and mild stenosis in the proximal segment of circumflex branch (30%); (3) Mild stenosis of RCA (< 50%) | LM: No abnormalities. LAD: Continuous calcification in the proximal and middle segments, with the most severe stenosis above 85%, TIMI3, a FFR value of 0.59 (normal FFR > 0.75). LCX: Thick high OM, with CTO after originating from the proximal segment, and the distal segment supplied with blood through the collateral branch. RCA: Stenosis of about 50% of the proximal lumen after opening, TIMI3 | Temporarily unqualified for flying |
| 7 | T wave changes in leads II, III, avF and V3-6 | Mixed plaques in the first diagonal branch of the anterior descending branch, with slight stenosis of the lumen | Qualified | |
| 8 | Sinus bradycardia | Soft plaques in the proximal segment of RCA, with mild stenosis of the lumen | Qualified | |
| 9 | Low-flat T wave in leads V5 and V6 | Calcified plaques in the proximal segment of LAD, with slight stenosis of the corresponding lumen (< 25%) | Qualified | |
| 10 | Low-flat T wave in leads V4-6 | Superficial myocardial bridge formed in the middle segment of LAD, with slight stenosis of the lumen (20%) | Qualified | |
| 11 | Low-flat T wave in leads V4-6 | Local mild and moderate stenosis of the proximal segment of LAD, with possibility of soft plaque formation | Qualified | |
| 12 | Low-flat or inverted T wave in leads II, III and avF | High-density calcified plaques in the proximal segment of LAD, with mild stenosis of the lumen | Qualified | |
| 13 | Grade I atrioventricular block and left ventricular hypertrophy accompanied with mild strain | Chest CT showed calcified plaques in coronary artery. Coronary artery CTA suggested calcified plaques in the middle segment of LAD, with slight stenosis of the lumen. Small calcified plaques in D2 segment, with slight stenosis of the lumen, and small calcified plaques in middle and distal segments of LCX, with slight stenosis of the lumen | LAD: Stenosis of 50%, TIMI3, FFR 0.91. LM(-), LCX(-) and RCA: Abnormally thick lumen, TIMI3 | Unqualified for specially permitted flying of overage pilots |
| 14 | Normal | Chest CT showed multiple calcified plaques in coronary artery. Coronary artery CTA indicated mixed plaques in the proximal segment, calcified plaques in the middle and soft plaques in the distal segment of RCA, with mild to moderate stenosis of the lumen. Mixed plaques in LM, with mild stenosis of the lumen. Mixed plaques in the proximal and middle segments of LAD, with mild to moderate stenosis of the lumen. Mixed plaques in the proximal segment of LCX, with mild stenosis of the lumen. Mixed plaques in the proximal and middle segments of OM, with mild to moderate stenosis of the lumen | LM(-): Presence of IB, with stenosis of 60% in IB opening. LAD: Calcification shadow in the proximal segment, stenosis of 30%-40% in the proximal and middle segments, myocardial bridge in the middle segment, with stenosis in systole, TIMI3. LCX(-) and OM: Thick. OM2: Beaded stenosis of 50%-80% in the proximal and middle segments, TIMI3, FFR 0.78. RCA: Stenosis of about 50% in the proximal and middle segments, focal stenosis of 50% in the middle segment, stenosis of 40%-50% in the middle and distal segments, eccentric stenosis of 80% in the distal segment, presence of PDA and PL, TIMI3, FFR 0.77 | Unqualified for specially permitted flying of overage pilots |
| 15 | Sinus bradycardia with low-flat T wave (V5V6) | Coronary artery calcification score: 229 points. Coronary artery CTA showed calcified plaques in the proximal and middle segments of RCA, with mild stenosis of the lumen, soft plaques in the proximal segment of LAD, with mild stenosis of the lumen, superficial myocardial bridge in the middle and distal segments, without stenosis of the lumen, calcification at the proximal end of D1, without stenosis of the lumen | LM(-) and LAD: Stenosis of 50% in the proximal segment, myocardial bridge in the middle and distal segments, stenosis of about 20% in systole, stenosis of about 30% of D1 opening, TIMI3. LCX: Presence of high OM originating the proximal segment, tiny PL in the distal segment, TIMI3. RCA: Thick lumen, and two focal plaques in the middle and distal segments, with stenosis of 30%, thick PDA and PL, with TIMI3 | Unqualified for specially permitted flying of overage pilots |
One trainer pilot diagnosed with multi-vessel disease was grounded because he had reached the maximum flying years.
One air combat service worker was diagnosed with multi-vessel disease, and coronary angiography showed that the total coronary artery stenosis was < 120%, and single vessel stenosis > 50% was not found. He was recommended to take statins orally to stabilize plaques, strictly control blood lipid and blood pressure, and was qualified for flying.
One helicopter pilot was diagnosed with multi-vessel disease and had reached the maximum flying years. CTA indicated single vessel stenosis < 50% and total coronary artery stenosis < 120%. Coronary angiography showed single vessel stenosis of 66% and total coronary artery stenosis of 126%. Hence, grounding was suggested.
One helicopter pilot was diagnosed with multi-vessel disease. The ECG showed left ventricular hypertrophy with strain. Chest computed tomography (CT) suggested multiple plaques, so coronary artery CTA was performed. The results showed that single vessel stenosis was 25%-50%, and the total coronary artery stenosis was 100%. Coronary angiography demonstrated that single vessel stenosis was 50%, and no stenosis was found in other vessels. The pilot also had grade 2 hypertension and took Betaloc and amlodipine orally for blood pressure control, but the control outcome was unsatisfactory (148/100 mmHg). He was unqualified for specially permitted flying of overage pilots, and thus grounded.
One fighter pilot was found to have abnormal Q wave on the side wall, but he denied chest pain and other discomfort, and myocardial necrosis markers such as myocardial enzymes were normal. The results of dynamic radionuclide myocardial perfusion imaging-single-photon emission CT showed that (1) No obvious sign of myocardial ischemia was found in the left ventricle; (2) The left ventricular EF values in load state and rest state were 59% and 57%, respectively, within the normal range; and (3) The fractional flow reserve index in left anterior descending coronary artery, left circumflex coronary artery and RCA dominated areas was normal. However, an abnormal increase was detected in the blood lipid, and coronary artery CTA suggested multi-vessel disease. Flying appraisal conclusion: He was temporarily unqualified for flying. Coronary angiography was performed in time, and it was revealed that the single vessel stenosis exceeded 70%, and the total coronary artery stenosis exceeded 120%. Drug balloon dilatation was performed during the operation. Strict control of blood lipid and blood pressure was implemented after operation, after which observation on the ground was conducted for 6 months. The reexaminations showed that the coronary artery stenosis was relieved. Hence, he was qualified for specially permitted flying of two-seat planes. At present, he has flown for more than 3 years, during which the blood lipid and blood pressure were examined every three months, with LDL-C < 0.8. Besides, the physiological parameters dynamically monitored during each flight were normal. In addition, the annual coronary artery CTA and dynamic radionuclide myocardial perfusion imaging suggested normal cardiopulmonary exercise.
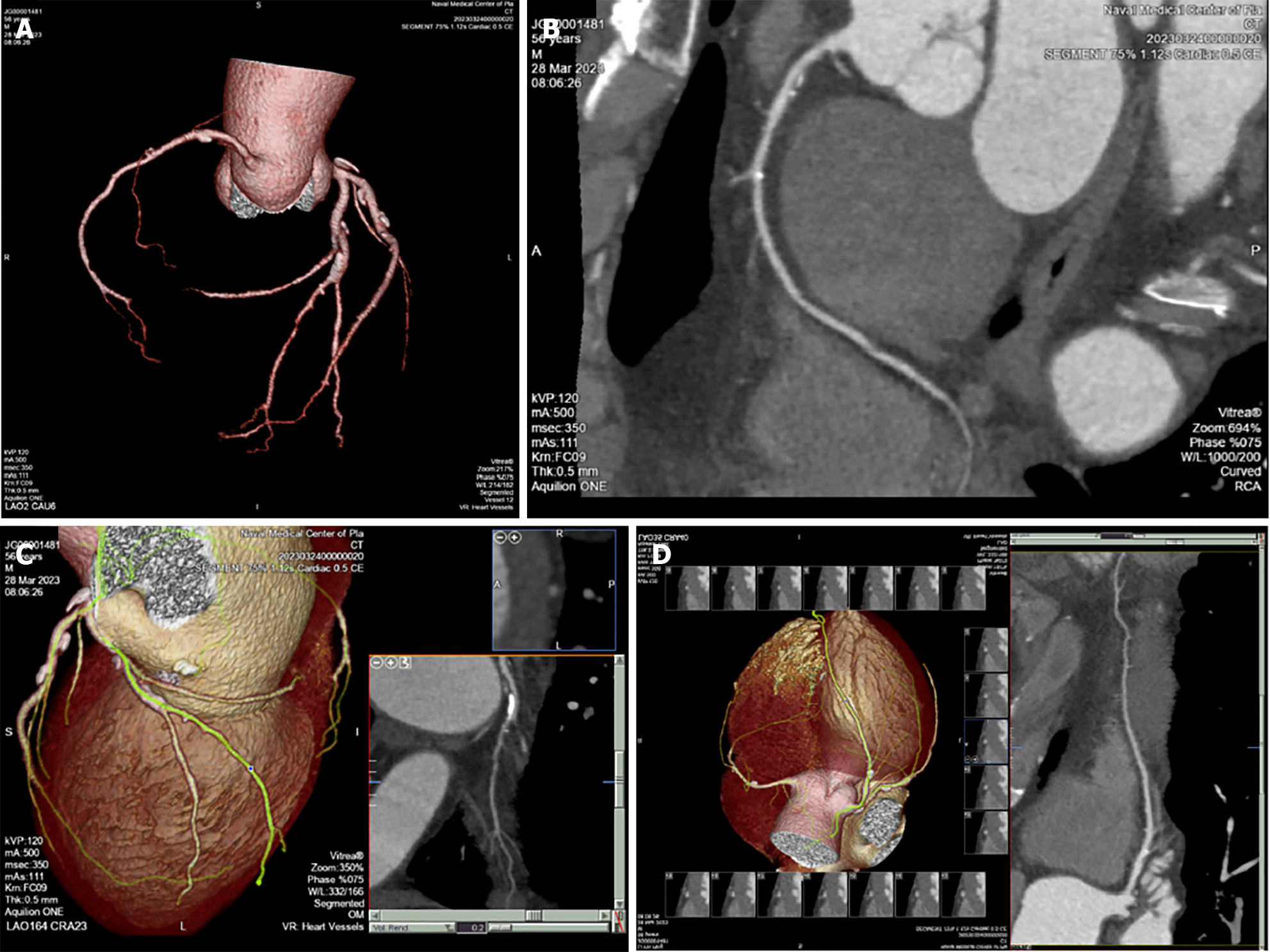
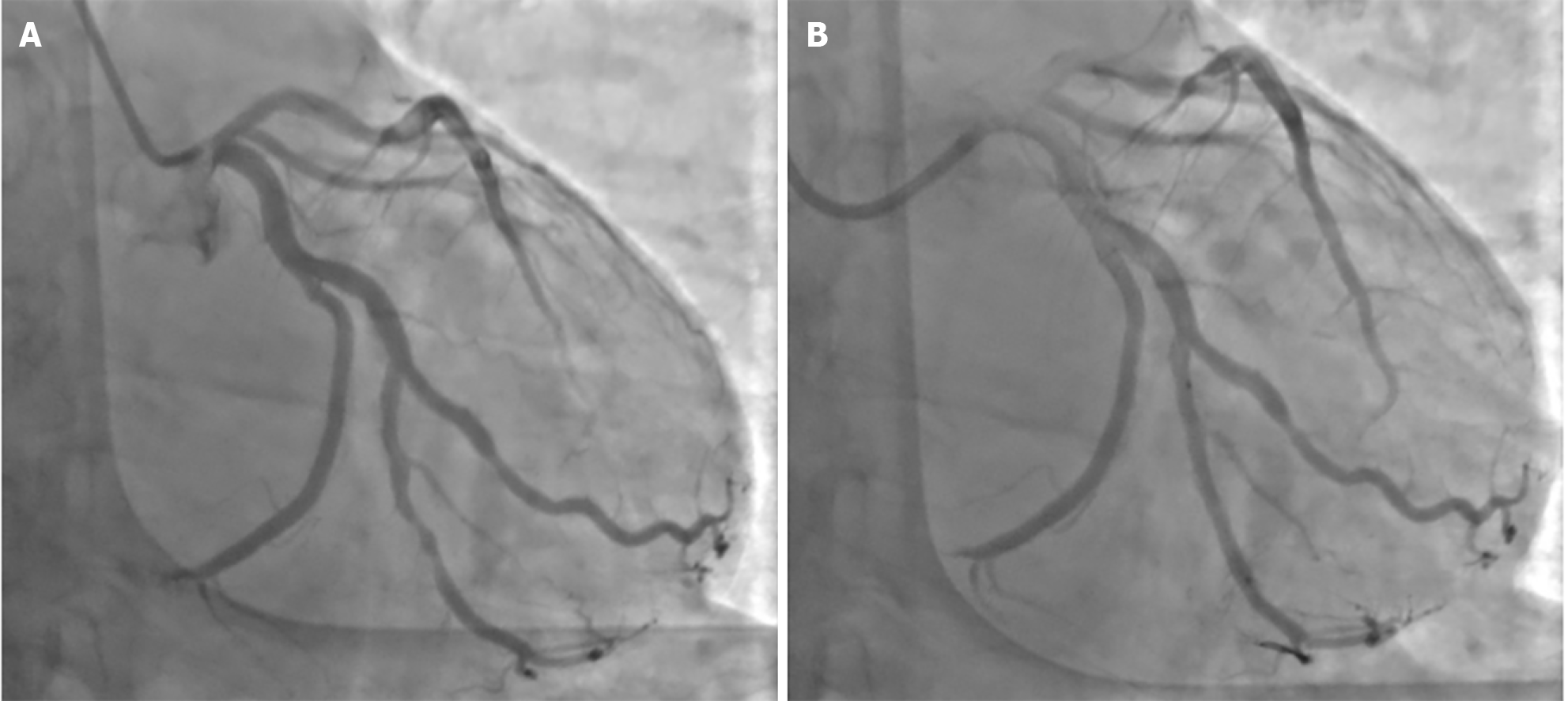
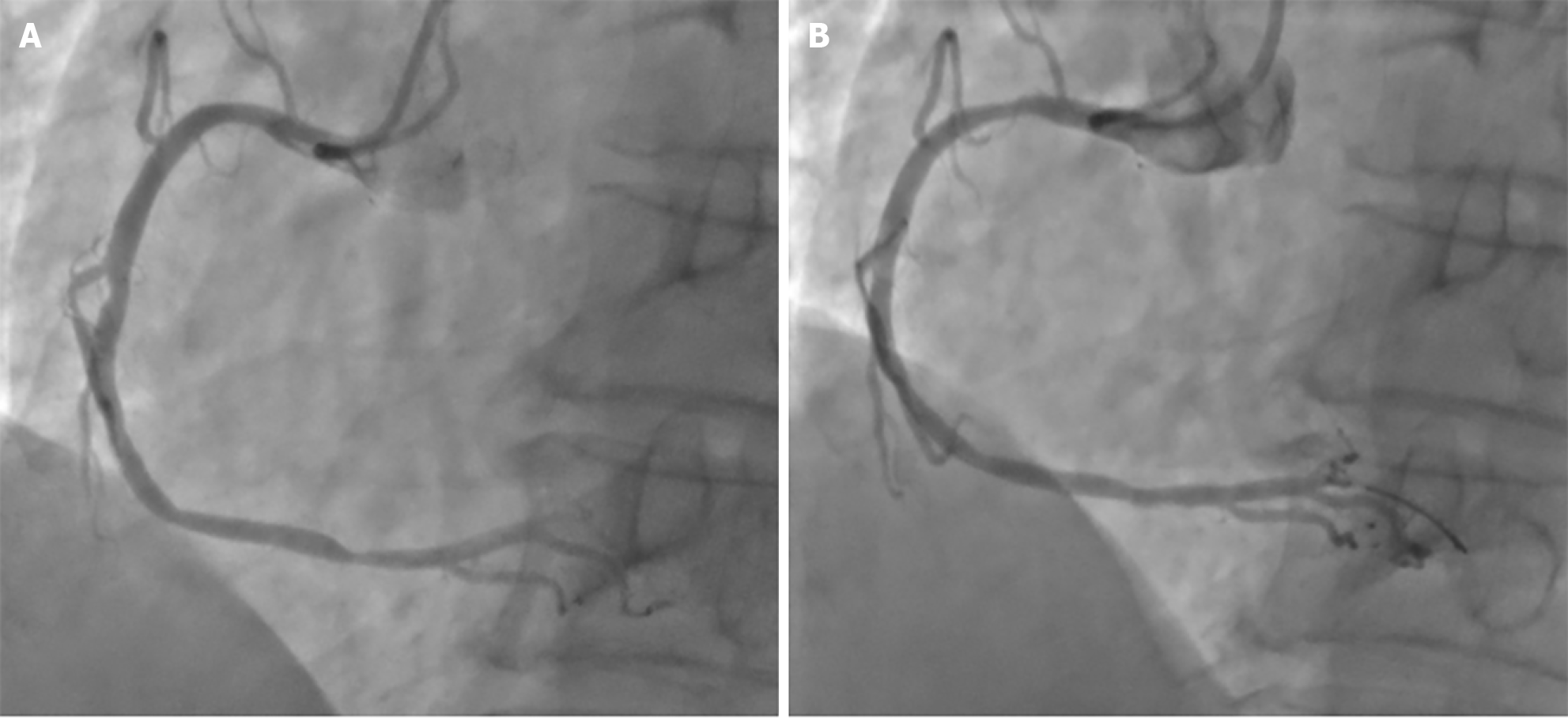
One transport plane pilot was diagnosed with multi-vessel disease, and had reached the maximum flying years. The physical examination showed that the ECG was normal. chest CT suggested coronary artery plaques, and coronary artery CTA showed multi-vessel disease. He received drug balloon dilatation and was unqualified for flying (Figure 1, Figure 2 and Figure 3).
The other cases were treated with statins to stabilize plaques. One year later, they underwent reexaminations, and the results denoted that the low-density lipoprotein and cholesterol were strictly controlled. Besides, the coronary artery CTA indicated no aggravation. They were recommended to receive reexaminations and follow-up every year.
Early warning and intervention of diseases leading to inflight incapacitation is not only the most crucial task in clinical aeromedical work, but also the key link to reduce the grounding rate, ensure the fighting strength of troops and extend the life cycle of pilots. Construction of early warning model, accurate early warning and early intervention of key parameters in the results of routine physical examination are of great military significance for ensuring the health improvement of military aircrew[4,5]. In Europe and the United States, the risks of major adverse cardiovascular events (MACEs) including death, myocardial infarction and revascularization (or repeated revascularization) have been used as markers of sudden incapacitation[6,7]. Through long-term follow-up of military pilots with coronary artery diseases, it is found that the annual incidence rate of MACEs is 0.6% for pilots with total coronary artery stenosis < 50%, and 1.1% for those with total coronary artery stenosis of 50%-120%. Therefore, a low risk is identified in the case of total coronary artery stenosis < 120% without single vessel stenosis > 70%, two vessel stenoses > 50%, and LM stenosis > 50%. specially permitted flying can be considered for two-seat or multi-seat plane pilots. However, the average annual risk of MACEs is 3% for pilots with total coronary artery stenosis > 120%, and it is over 3% for pilots with single vessel stenosis > 70% or two vessel stenoses > 50%, and/or LM stenosis > 50%, and the aviation risk is relatively high.
Coronary artery CTA is minimally invasive and convenient, so it can be given in priority. However, coronary artery CTA is not the gold standard for the diagnosis of coronary diseases[8]. The gold standard is coronary angiography, which is an invasive examination, and requires observation on the ground for 1-3 months after operation even if the examination results are normal. As a result, coronary angiography is not routinely used in clinic. Treadmill exercise test and coronary artery CTA can serve as effective means to screen and eliminate coronary heart diseases in military aircrew, and coronary angiography is the final method to diagnose and eliminate coronary heart diseases at present[9]. However, if a patient has abnormally high blood lipid, abnormal ECG results, and severe multi-vessel disease according to coronary artery CTA, the patient is suggested to receive coronary angiography as early as possible.
Currently, it is clearly pointed out in the special permission guidelines in China and foreign countries that after interventional therapy for coronary artery diseases and strict control of various high-risk factors, flying personnel with single-vessel disease < 50% and total coronary artery stenosis < 120% in reexaminations are qualified for piloting transport planes, helicopters and multi-seat planes and unqualified for piloting fighters[10]. The appraisal conclusion of specially permitted flying of fighter pilots needs to continue to accumulate practical experience and be strictly controlled. One fighter pilot in this study had piloted two-seat planes for over 3 years after coronary intervention. At present, the flying time is controlled to be less than 50 hours per year, the physiological indexes are closely monitored in each flight, and all blood lipid and blood pressure indexes are closely controlled and followed up.
Among the 15 flying personnel with coronary artery diseases in this study, there were 5 air combat service workers and 1 navigator (accounting for 40% in total), and these 6 had a relatively high incidence rate, which may be related to the fact that the selection criteria of air combat service workers are less strict than those of pilots, and the maximum service length of air combat service workers is higher than that of pilots of various aircraft. For high-risk groups aged over 45 years old, it is necessary to focus on various early warning indicators. In the multi-vessel disease group, 8 pilots (1 pilot each of helicopters, fighters and bombers) had normal ECG, but had transient chest tightness and discomfort in the past. Considering the flight safety of pilots, it was suggested to undergo additional dynamic ECG and coronary artery CTA, and the results showed abnormalities in the coronary artery[11]. In the annual physical examination, 4 pilots had normal ECG, but coronary plaques were found by thin-slice chest CT. They were suggested to receive coronary artery CTA, and abnormalities were detected. At the same time, it was uncovered that the proportion of pilots in the multi-vessel disease group was high, signifying that the disease is already in the advanced stage at the time of discovery and the symptoms are atypical at ordinary times. Therefore, it is suggested that aviation military doctors should pay attention to communication with pilots at ordinary times, ask about medical history in detail, carefully perform physical examination, and avoid dependence only on routine examination results. In particular, the tolerance of pilots is higher than that of ordinary people, so they are likely to ignore ordinary discomforts.
In this study, the TC, LDL-C and ApoB were higher in the multi-vessel disease group than those in the single vessel disease group. In the health management of air combat service workers, great importance has been attached to the concept of the full life cycle: From the pilot physical examination to grounding, close attention should be paid to these early warning indicators in each physical examination, early intervention should be implemented, and strict control of blood lipid and blood pressure should be emphasized to prevent the initial coronary events[12]. Moreover, long-term follow-up and dynamic monitoring are suggested. Furthermore, reasonable arrangement of meals and control of the total calories should be implemented, a low-fat and low-cholesterol diet should be provided, and the intake of sucrose and sugary foods should be limited. In addition, it is suggested to have appropriate physical training, ensure adequate sleeping, quit smoking and limit alcohol.
Coronary artery diseases are the main cause of flying personnel's inflight incapacitation and grounding due to illness, so it is necessary to pay close attention to relevant early warning indicators and intervene and treat them as early as possible. Coronary artery CTA is simple and noninvasive, conducive to early detection and early warning of coronary diseases in flying personnel.
| 1. | Zerrik M, Moumen A, El Ghazi M, Smiress FB, Iloughmane Z, El M'hadi C, Chemsi M. Screening for Coronary Artery Disease in Asymptomatic Pilots with Diabetes Mellitus. Aerosp Med Hum Perform. 2024;95:200-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Davenport ED, Gray G, Rienks R, Bron D, Syburra T, d'Arcy JL, Guettler NJ, Manen O, Nicol ED. Management of established coronary artery disease in aircrew without myocardial infarction or revascularisation. Heart. 2019;105:s25-s30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Guettler N, Sammito S. Coronary Artery Disease Management in Military Aircrew. Aerosp Med Hum Perform. 2023;94:917-922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Gunduz SH, Metin S. Medical reasons for permanent and temporary disqualification of Turkish civil aviation pilots. Arch Environ Occup Health. 2024;1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 5. | Simons R, Maire R, Van Drongelen A, Valk P. Grounding of Pilots: Medical Reasons and Recommendations for Prevention. Aerosp Med Hum Perform. 2021;92:950-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 6. | Long Cheong RW, See B, Chuan Tan BB, Koh CH. Coronary Artery Disease Screening Using CT Coronary Angiography. Aerosp Med Hum Perform. 2020;91:812-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Elsaid N, Saied A, Kandil H, Soliman A, Taher F, Hadi M, Giridharan G, Jennings R, Casanova M, Keynton R, El-Baz A. Impact of stress and hypertension on the cerebrovasculature. Front Biosci (Landmark Ed). 2021;26:1643-1652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 8. | Li K, Hu P, Luo X, Li F, Chen L, Zhao J, Wang Z, Luo W, Jin J, Qin Z. Anomalous origin of the coronary artery: prevalence and coronary artery disease in adults undergoing coronary tomographic angiography. BMC Cardiovasc Disord. 2024;24:271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Holland J, Eveson L, Holdsworth D, Nicol E. Coronary artery calcium scoring vs. coronary CT angiography for the assessment of occupationally significant coronary artery disease. J Cardiovasc Comput Tomogr. 2022;16:454-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 10. | Hou KC. Challenges in Utilizing CT Coronary Angiography and CT Calcium Scoring to Determine Aeromedical Fitness for Aicrew: A Tale of 3 CTs. Curr Probl Cardiol. 2022;47:100906. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Guettler N, Nicol ED, Sammito S. Exercise ECG for Screening in Military Aircrew. Aerosp Med Hum Perform. 2022;93:666-672. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 12. | Khazale NS, Haddad F. Prevalence and characteristics of metabolic syndrome in 111 Royal Jordanian Air Force pilots. Aviat Space Environ Med. 2007;78:968-972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |