Published online Apr 26, 2024. doi: 10.4330/wjc.v16.i4.199
Peer-review started: November 22, 2023
First decision: January 23, 2024
Revised: February 14, 2024
Accepted: April 1, 2024
Article in press: April 1, 2024
Published online: April 26, 2024
Processing time: 152 Days and 22.5 Hours
When exposed to high-altitude environments, the cardiovascular system un
To summarize the latest research advancements and hot research points in the cardiovascular system at high altitude by conducting a bibliometric and visualization analysis.
The literature was systematically retrieved and filtered using the Web of Science Core Collection of Science Citation Index Expanded. A visualization analysis of the identified publications was conducted employing CiteSpace and VOSviewer.
A total of 1674 publications were included in the study, with an observed annual increase in the number of publications spanning from 1990 to 2022. The United States of America emerged as the predominant contributor, while Universidad Peruana Cayetano Heredia stood out as the institution with the highest pub
Over the past 32 years, research on the cardiovascular system in high-altitude regions has been steadily increasing. Future research in this field may focus on areas such as hypoxia adaptation, metabolism, and cardiopulmonary exercise. Strengthening interdisciplinary and multi-team collaborations will facilitate further exploration of the pathophysiological mechanisms underlying cardiovascular changes in high-altitude environments and provide a theoretical basis for standardized disease diagnosis and treatment.
Core Tip: In this study, a bibliometric and visualization analysis was conducted to summarize the latest research ad
- Citation: Zhao ML, Lu ZJ, Yang L, Ding S, Gao F, Liu YZ, Yang XL, Li X, He SY. The cardiovascular system at high altitude: A bibliometric and visualization analysis. World J Cardiol 2024; 16(4): 199-214
- URL: https://www.wjgnet.com/1949-8462/full/v16/i4/199.htm
- DOI: https://dx.doi.org/10.4330/wjc.v16.i4.199
Globally, a large number of people visit, work, or reside at high altitude. An estimated 81.6 million people live at altitudes > 2500 m above sea level and 14.4 million people live at altitudes ≥ 3500 m above sea level[1]. The oxygen levels decline with increasing altitude. Exposure to hypoxia significantly affects physical performance and the cardiovascular system[2]. Exposure to hypoxia or intermittent hypoxia activates compensatory cardioprotective mechanisms[3]. Several studies have shown that short-term intermittent hypoxia promotes cardioprotective effects similar to ischemia preconditioning. For example, intermittent hypoxia protected cardiomyocytes against H2O2- and ischemia/reperfusion-induced oxidative stress and cell death by maintaining Ca2+ homeostasis and the mitochondrial membrane potential, and upregulating the expression levels of antioxidant enzymes[4]. Intermittent hypobaric hypoxia exposure in rats induced cardiovascular protective mechanisms against oxidative stress[5]. However, prolonged exposure to hypoxia at high altitude increases the risk of cardiovascular disease by chronically activating cellular responses that are detrimental to cardiac function. The damage to cardiac cells at high altitude because of exposure to hypoxic and hypobaric environment results in elevated serum levels of myocardial enzymes to varying degrees; in severe cases, myocardial damage causes malignant arrhythmia, heart failure, and even sudden death[6]. Furthermore, at high altitudes, many people experience acute mountain sickness (AMS), high-altitude cerebral edema, high-altitude pulmonary edema (HAPE), chronic mountain sickness (CMS), and high-altitude pulmonary hypertension (HAPH)[7]. The prevalence of myocardial injury at high altitude was 18.6%-33.2%[8,9]. Although several studies have reported the adverse effects of high altitude on the cardiovascular system, the mechanisms are complex and unclear. Therefore, there is an urgent need to identify the advances, trends, and hotpots in the research area of the cardiovascular system at high altitude based on previous publications. Such information would be beneficial for research investigators in this field to pursue studies in the right direction.
Bibliometric methods are used to investigate the productivity of researchers, institutions, and countries in specific subject areas to determine the research hotspots and future directions that can also be used to guide policy decisions[10]. Furthermore, bibliometric analysis is a good indicator of progress in a research field[11]. Moreover, co-citation is frequently used in the bibliometric analysis to identify links between authors, keywords, countries, and organizations.
Several bibliometric analyses have been performed in the field of the cardiovascular system in areas such as heart transplantation, future landscape of macrophage research in cardiovascular disease, and heart failure[12-15]. In this study, we performed a bibliometric analysis of studies on the cardiovascular system at high altitude using the Science Citation Index Expanded (SCIE) index of the Web of Science (WoS) Core Collection. Our aim was to identify the current hotpots of research and the frontier directions that would be helpful in investigating the mechanisms that affect the cardiovascular system at high altitude and the future clinical applications in this field.
CiteSpace 6.1 R6 software and VOSviewer 1.6.18.0 software were used for the bibliometric analysis of countries, institutions, journals, and keywords of research related to the cardiovascular system at high altitude between January 1, 1990 and December 31, 2022. The CiteSpace software was used to simultaneously visualize the co-occurrence network between time, frequency, and betweenness centrality. Cluster view was used to label the clusters with phrases. Furthermore, the CiteSpace software was used for temporal analysis and the pruning algorithms were used to highlight the main structure of the network[16]. The co-occurrence analysis in CiteSpace was used to visualize the co-authorship network of countries, institutions, journals, and authors. CiteSpace software was also used to visualize the timeline view of keyword clustering and identify the development process and hotpots in the cardiovascular system at high altitude. In CiteSpace, node size represents the frequency of publications and citations; purple rings represent centrality; and nodes in the red inner rings represent the burst in research[17]. Furthermore, connections between points represent the co-citation relationship and the number of interconnections represents the strength of co-occurrence or co-citation of the collaboration.
VOSviewer is a popular tool for visualizing the knowledge map and provides a variety of tools for viewing keywords, co-institutions, co-authors, etc., including Network Visualization, Overlay Visualization, and Density Visualizatio[18]. Co-citation analysis of cited references, journals, and authors, and the co-occurrence analysis of keywords were visualized using the VOSviewer. The points in the co-citation maps represent different co-cited references, journals, or authors. Size of the points represents the number of citations in individual publications. The lines between points show co-citation relationships. The colored points represent different clusters and the colored lines represent different years.
In this study, we searched for publications related to cardiac system at high altitude in the SCIE index of the WoS Core Collection using the following keywords and combinations: TS = ((“high altitude” OR “plateau” OR “mountain”) AND (“cardiovascular” OR “heart” OR “cardiac” OR “myocardial”)). The time span was set between January 1, 1990 and December 31, 2022. The literature language was restricted to English. We identified 6605 publications that met these criteria. The literature types were limited to articles and reviews. The exclusion criteria are shown in Table 1. After initial search, we retrieved 5992 publications as potential candidates for inclusion. Subsequently, the titles, abstracts, and the full texts of the publications were manually examined by two investigators (Zhao ML and He SY) and the irrelevant articles were excluded. Finally, after removing duplicates, we included 1674 journal articles, including 1331 articles and 133 reviews for further analysis.
| Date source | Web of Science |
| Citation index | SCIE |
| Searching period | January 1, 1990 to December 31, 2022 |
| Searching | TS = ((“high altitude” OR “plateau” OR “mountain”) AND (“cardiovascular” OR “heart” OR “cardiac” OR “myocardial”)) |
| Subject category | “Physiology”, “Cardiac Cardiovascular Systems”, “Sport Sciences” |
| Document type | “Articles” or “reviews” |
| Language | “English” |
| Sample size | 1674 |
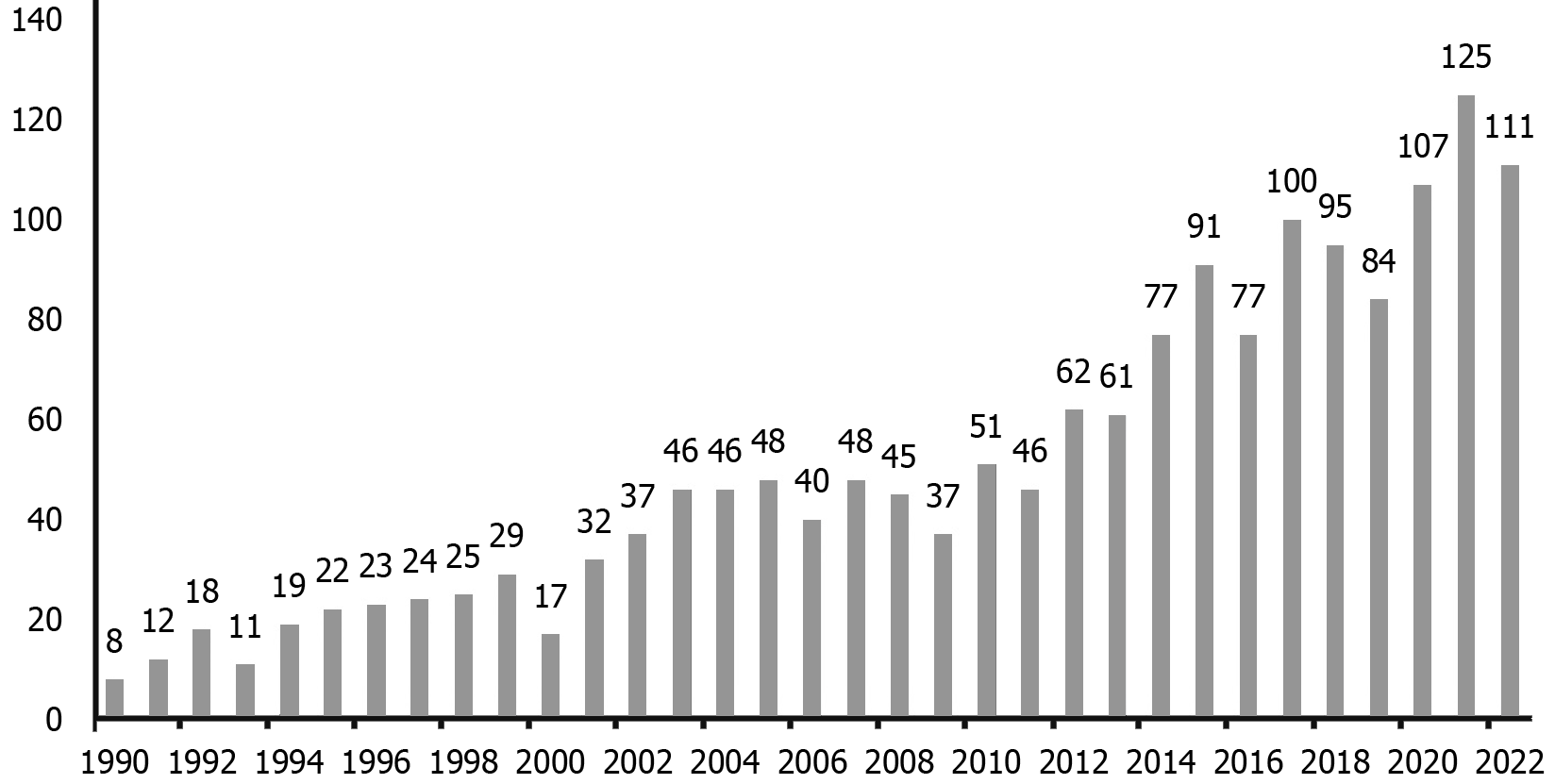
This study included 1674 papers with 7433 authors from 2041 organizations and 78 countries; these papers were published in 586 journals, and were cited in 44674 publications from 7775 journals (Table 2). Figure 1 shows the chronological distribution of publications in the field of research related to the cardiovascular system at high altitude. The number of papers published in this field increased every year from 1990 to 2022, especially from 2012 onwards. The annual publication rate was > 60. This suggested significant research in this area, especially after 2012.
| Criteria | Quantity |
| Publications | 1674 |
| Authors | 7433 |
| Journals | 586 |
| Institutions | 2041 |
| Countries | 78 |
| Cited references | 44674 |
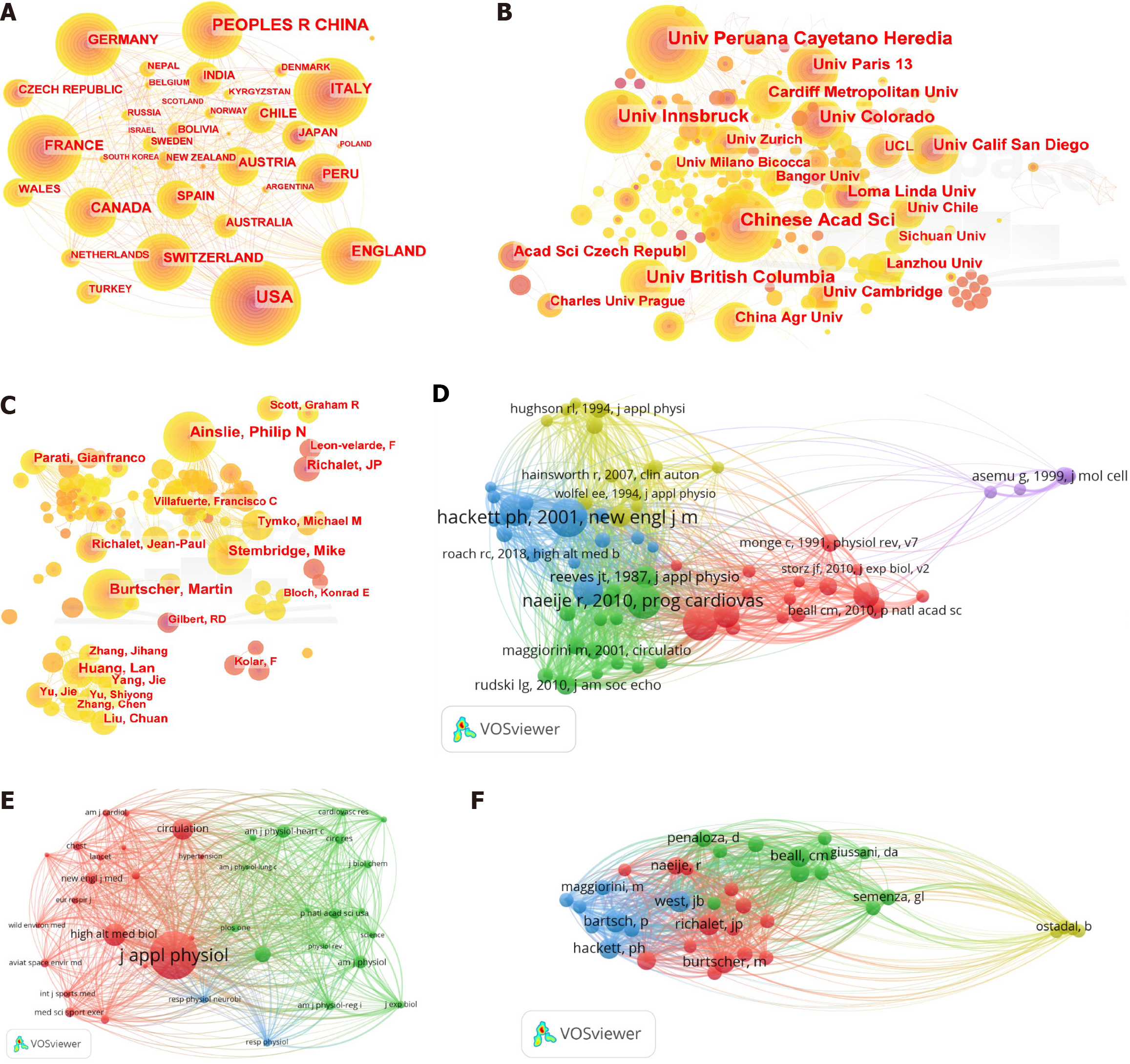
We constructed a co-occurrence network of countries and institutions to evaluate the progress of studies on the cardiovascular system at high altitude in different countries and institutions, and also determine the potential co-operation between countries and institutions in this area. Figure 2A shows the interactions between countries and Figure 2B shows the interactions between institutions in this research area. The top 5 productive countries in this research area were United States (409 papers), People’s Republic of China (367 papers), England (156 papers), France (129 papers), and Canada (124 papers; Table 3). The top 5 countries for centrality were the United States (0.41), People’s Republic of China (0.21), England (0.20), Germany (0.16), and Switzerland (0.13; Table 4). The betweenness centrality was more than 0.1 for these 5 countries, highlighting their leading role in research area. Table 5 shows the top 10 institutions in the research area of the cardiovascular system at high altitude. The universities with the highest number of publications were as follows: Universidad Peruana Cayetano Heredia (57 papers), University of British Columbia (51 papers), Chinese Academy of sciences (48 papers), University of Innsbruck (48 papers), and University of Colorado (46 papers). The top 10 countries in this area included six European countries (England, Germany, Switzerland, Italy, France, and Netherlands), two North American countries (the United States and Canada), one Asian country (People’s Republic of China), and one South American country (Chile). These top ten countries accounted for 93.91% of the publications.
| Rank | Country | Publications | Citations | Average citations |
| 1 | United States | 409 | 12146 | 29.70 |
| 2 | People’s Republic of China | 367 | 5268 | 14.35 |
| 3 | England | 156 | 4119 | 26.40 |
| 4 | France | 129 | 3296 | 25.55 |
| 5 | Canada | 124 | 3190 | 25.73 |
| 6 | Italy | 124 | 3065 | 24.72 |
| 7 | Switzerland | 113 | 3360 | 29.73 |
| 8 | Germany | 113 | 2330 | 20.62 |
| 9 | Austria | 79 | 1259 | 15.93 |
| 10 | Peru | 72 | 2431 | 33.76 |
| Rank | Country | Centrality |
| 1 | United States | 0.41 |
| 2 | People’s Republic of China | 0.21 |
| 3 | England | 0.20 |
| 4 | Germany | 0.16 |
| 5 | Switzerland | 0.13 |
| 6 | Italy | 0.11 |
| 7 | Chile | 0.09 |
| 8 | France | 0.08 |
| 9 | Canada | 0.08 |
| 10 | Netherlands | 0.07 |
| Rank | Institution | Publications | Citations | Average citations |
| 1 | Universidad Peruana Cayetano Heredia | 57 | 1704 | 29.90 |
| 2 | University of British Columbia | 51 | 1505 | 29.51 |
| 3 | Chinese Academy of Sciences | 48 | 1140 | 23.75 |
| 4 | University of Innsbruck | 48 | 819 | 17.07 |
| 5 | University of Colorado | 46 | 2311 | 50.24 |
| 6 | Loma Linda University | 39 | 1006 | 25.79 |
| 7 | The Third Military Medical University | 36 | 307 | 7.87 |
| 8 | University of Cambridge | 32 | 1335 | 42.34 |
| 9 | Université Sorbonne Paris Nord | 31 | 1300 | 41.94 |
| 10 | University of California-San Diego | 31 | 1119 | 36.10 |
Next, we analyzed the literature to identify the main research scholars studying the cardiovascular system at high altitude. Figure 2C shows the network of author-co-author relationships in this field. Table 6 shows the authors who have published 16 papers or more in the area of the cardiovascular system at high altitude. Jean-Paul Richalet from the University of Paris published 41 papers with 1616 citations and an average of 39 citations per article. In the second place, Philip N Ainslie from University of British Columbia contributed 31 articles with 565 citations and an average of 18 citations per article. Martin Burtscher from University of Paris published 30 articles with 488 citations and an average of 16 citations per article.
| Rank | Author | Documents | Citations | Average citations |
| 1 | Jean-Paul Richalet | 41 | 1616 | 39.41 |
| 2 | Philip N Ainslie | 31 | 565 | 18.23 |
| 3 | Martin Burtscher | 30 | 488 | 16.27 |
| 4 | Lan Huang | 25 | 216 | 8.64 |
| 5 | Mike Stembridge | 23 | 387 | 16.83 |
| 6 | Gianfranco Parati | 21 | 381 | 18.14 |
| 7 | Michael M Tymko | 18 | 214 | 11.89 |
| 8 | Jie Yu | 17 | 206 | 12.12 |
| 9 | Leon-Velarde Fabiola | 16 | 799 | 49.94 |
| 10 | Francisco C Villafuerte | 16 | 316 | 19.75 |
| 11 | Frantisek Kolar | 16 | 267 | 16.69 |
| 12 | Jie Yang | 16 | 71 | 4.44 |
Impact factor of a journal refers to the importance of a journal in the research area of interest, and is calculated by the frequency with which the articles published in the journal were cited in other articles[19]. Table 7 shows the top 10 journals in the field of the cardiovascular system at high altitude. The top 3 journals were High Altitude Medicine & Biology (144 publications), Journal of Applied Physiology (81 publications), and Frontiers in Physiology (55 publications). The top journals with the highest number of citations per article were The Journal of Physiology (London) (41.62 citations per publication), Journal of Applied Physiology (37.71 citations per publication), and American Journal of Physiology-Regulatory Integrative and Comparative Physiology (37.68 citations per publication).
| Rank | Source | Publications | Citations | Average citations |
| 1 | High Altitude Medicine & Biology | 144 | 2982 | 20.71 |
| 2 | Journal of Applied Physiology | 81 | 3070 | 37.91 |
| 3 | Frontiers in Physiology | 55 | 399 | 7.25 |
| 4 | Wilderness & Environmental Medicine | 38 | 622 | 16.37 |
| 5 | Journal of Physiology-London | 29 | 1207 | 41.62 |
| 6 | American Journal of Physiology-Heart and Circulatory Physiology | 29 | 827 | 28.52 |
| 7 | Plos One | 27 | 692 | 25.63 |
| 8 | European Journal of Applied Physiology | 26 | 489 | 18.81 |
| 9 | Experimental Physiology | 22 | 406 | 18.45 |
| 10 | American Journal of Physiology-Regulatory Integrative and Comparative | 22 | 829 | 37.68 |
The number of citations reflects the quality of a study and is an indicator of the importance of the findings for the research field[20]. The most cited references provide a theoretical basis for studying the cardiovascular system at high altitude and guide researchers for further studies. We performed a bibliometric analysis of the cited references and obtained 44674 citations in this study. Then, using 30 citations as a threshold, we identified 68 articles for co-citation analysis of the cited articles. We then constructed a network of publications that were related to research regarding the cardiovascular system at high altitude. We identified five clusters represented by different colors and the cited references are represented as nodes of different sizes (Figure 2D). Table 8 summarizes the top 10 most frequently cited references. The top 5 cited references were as follows: Hackett and Roach[21] in 2001 (123 citations), Naeije[22] in 2010 (107 citations), Penaloza and Arias-Stella[23] in 2007 (107 citations), Bártsch et al[24] in 2007 (90 citations), and Simonson et al[25] in 2010. Our study showed that the top 3 cited references were all reviews. The most cited publication was a review authored by Hackett and Roach[21], which described the epidemiology and risk factors, pathophysiological process, clinical manifestations, diagnosis, treatment, and disease preventive measures at high altitude[21]. The second and third most cited references also reviewed the pathophysiological processes of the cardiopulmonary vascular system at high altitude. The second reference was published by Naeije[22], mainly focused on the acclimatization of the cardiovascular system at high altitude[22]. The third reference was a review published by Penaloza and Aria-Stella[23] in Circulation and was titled "The Heart and Pulmonary Circulation at High Altitudes Healthy Highlanders and Chronic Mountain Sickness"[23]. This review described the physiology, pathology, pathogenesis, and clinical features of the heart and pulmonary circulation in healthy highlanders and patients with CMS[23]. The sixth most cited reference published by León-Velarde et al[26], reporting an expert consensus statement on the chronic and subacute diseases at high altitude, described the criteria for selecting a specific method or procedure to diagnose or manage these diseases[26]. The reference titled "Guidelines for Echocardiographic Evaluation of the Right Heart in Adult Patients: A Report by the American Society of Echocardiography" holds the tenth position in terms of citation count. This reference serves as a comprehensive document intended for healthcare professionals, providing them with guidelines for assessing the right ventricle and right atrium. It encompasses a range of parameters utilized for estimating both systolic and diastolic functions of the right ventricle, along with normal reference values derived from aggregated data[27].
| Rank | Ref. | Citations |
| 1 | High-altitude illness | 123 |
| 2 | Physiological adaptation of the cardiovascular system to high altitude | 107 |
| 3 | The heart and pulmonary circulation at high altitudes: Healthy highlanders and chronic mountain sickness | 107 |
| 4 | Effect of altitude on the heart and the lungs | 90 |
| 5 | Genetic evidence for high-altitude adaptation in Tibet | 78 |
| 6 | Consensus statement on chronic subacute high altitude diseases | 77 |
| 7 | Operation Everest II: Preservation of cardiac function at extreme altitude | 67 |
| 8 | Sympathetic neural overactivity in healthy humans after prolonged exposure to hypobaric hypoxia | 65 |
| 9 | Guidelines for the echocardiographic assessment of the right heart in adults: A report from the American society of echocardiography | 55 |
| 10 | Two routes to functional adaptation: Tibetan and Andean high-altitude natives | 52 |
Subsequently, using a citation threshold of 300, we selected 39 journals for co-citation analysis. Table 9 shows the top 10 most frequently cited journals. The co-citation network of journals consisted of three distinct clusters denoted by different colors (Figure 2E). Journal of Applied Physiology (5586 citations), High Altitude Medicine & Biology (2192 citations), and Circulation (2051 citations) were the most cited journals. These three journals are esteemed publications within the JCR1 region.
| Rank | Journals | Citations |
| 1 | Journal of Applied Physiology | 5586 |
| 2 | High Altitude Medicine & Biology | 2192 |
| 3 | Circulation | 2051 |
| 4 | Journal of Physiology-London | 1433 |
| 5 | American Journal of Physiology-Heart and Circulatory | 1138 |
| 6 | American Journal of Physiology | 1107 |
| 7 | The New England Journal of Medicine | 980 |
| 8 | Circulation Research | 891 |
| 9 | Proceedings of the National Academy of Sciences of the United States of America -Physical sciences | 886 |
| 10 | American Journal of Physiology-Regulatory Integrative and Comparative Physiology | 792 |
Next, we sought to identify the leading researchers in this research area. We used a citations threshold of 100 and identified 38 authors with a cumulative citation count of 29778. The co-citation network of these 38 authors demonstrated four distinct clusters (Figure 2F). Table 10 presents the top 10 most cited authors in this network, with Peter Bärtsch (382 citations), Martin Burtscher (378 citations), and John B West (358 citations) being the three most prominently cited authors.
| Rank | Authors | Citations |
| 1 | Peter Bärtsch | 382 |
| P | Martin Burtscher | 378 |
| 3 | John B West | 358 |
| 4 | Beall Cynthia M | 352 |
| 5 | Jean-Paul Richalet | 352 |
| 6 | Hackett Peter | 330 |
| 7 | Lorna G Moore | 265 |
| 8 | Robert C Roach | 261 |
| 9 | Robert Naeije | 235 |
| 10 | Dante Penaloza | 222 |
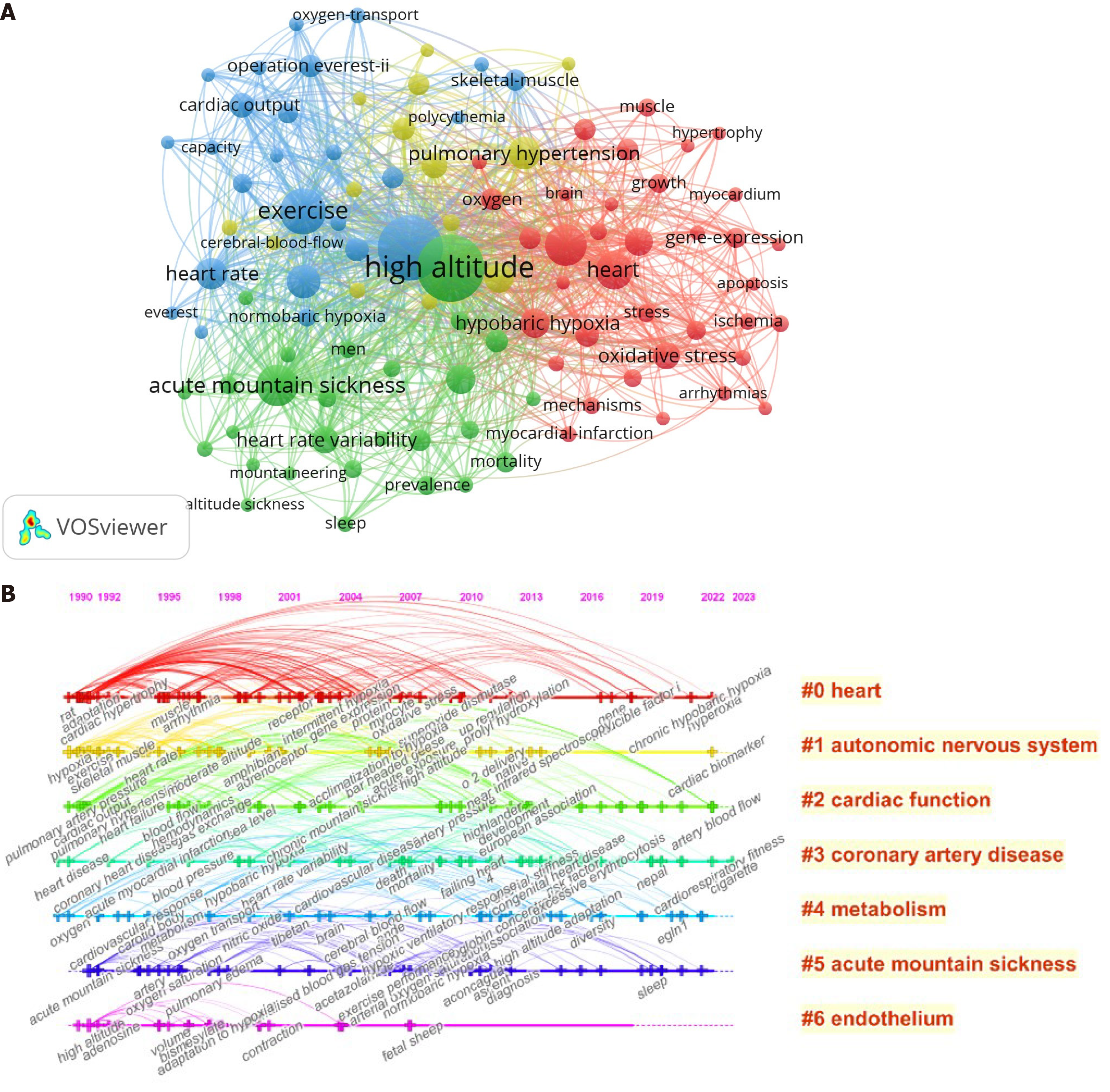
Keywords are specific terms or phrases that summarize the main subjects and concepts presented in the article. Therefore, co-occurrence analysis of keywords can be used to identify the hotspots in a research area. In the present study, we used the VOSviewer software to construct a network of keywords in the 1674 articles included in this study. Subsequently, we identified 103 keywords with a frequency of more than 20 (Figure 3A). In this network, size of the circle node denotes frequency of the keyword. For example, if the circle node is large, it suggests that the keyword occurs at a higher frequency. Hence, we considered high frequency key words as research hotspots in the field of study. The line of nodes represents the strength of the association. A thicker line indicates that the two words co-appear more times in the same article. Clusters of key words are represented by distinct colors. The top 10 keywords were high altitude (n = 598), hypoxia (n = 559), exercise (n = 269), AMS (n = 214), adaptation (n = 209), heart (n = 167), acclimatization (n = 137), pulmonary hypertension (n = 133), heart rate (n = 117), and blood pressure (n = 104; Table 11).
| Rank | Keyword | Occurrences | Total link strength |
| 1 | High altitude | 598 | 2537 |
| 2 | Hypoxia | 559 | 2391 |
| 3 | Exercise | 269 | 1254 |
| 4 | Acute mountain sickness | 214 | 971 |
| 5 | Adaptation | 209 | 994 |
| 6 | Heart | 167 | 746 |
| 7 | Acclimatization | 137 | 728 |
| 8 | Pulmonary hypertension | 133 | 655 |
| 9 | Heart rate | 117 | 507 |
| 10 | Blood pressure | 104 | 526 |
| 11 | Hypobaric hypoxia | 101 | 528 |
| 12 | Nitric oxide | 99 | 442 |
| 13 | Chronic hypoxia | 93 | 432 |
| 14 | Oxidative stress | 90 | 408 |
| 15 | Chronic mountain-sickness | 80 | 375 |
| 16 | Cardiac output | 71 | 365 |
| 17 | Intermittent hypoxia | 66 | 190 |
| 18 | Oxygen | 56 | 170 |
| 19 | Metabolism | 54 | 149 |
| 20 | Echocardiography | 53 | 217 |
Since the number and type of keywords were too complex, the research topics were ambiguous, and it was difficult to determine the current research hotspots and priorities, previous studies have used keyword clustering to address this issue. Keyword clustering involves extracting representative phrases from keyword groups with similar meanings as specific cluster labels[12]. We used keyword clustering to determine the distribution of topics. The keyword clustering results were as follows: Heart (clustering 0), autonomic nervous system (clustering 1), cardiac function (clustering 2), coronary artery disease (clustering 3), metabolism (clustering 4), AMS (clustering 5), and endothelium (clustering 6) (Figure 3B). Based on the timeline view and clusters of keywords, we observed certain specific trends in the research hotspots regarding the study of the cardiovascular system at high altitude. The main research hotspots between 1990 and 2022 were heart, cardiac function, coronary artery disease, metabolism, and AMS. Autonomic nervous system and endothelium were also research hotspots in this field before 2015. Furthermore, we compile and summarize several significant points to reveal high altitude cardiovascular system function based on the analysis of popular keywords (Table 12).
| Rank | Keyword | Significant points |
| 1 | Hypoxia | Hypoxia emerges as the predominant characteristic among individuals residing at high altitudes |
| 2 | Exercise at high altitude | Exercise training is advocated for enhancing adaptation to high altitude |
| 3 | Pulmonary hypertension | Pulmonary artery pressure increases at high altitude due to vasoconstriction |
| 4 | Oxidative stress | Oxidative stress is activity at high altitude |
| 5 | Metabolomics | Metabolomics has offered novel perspectives on the pathophysiological mechanisms that underlie adaptations to early hypobaric hypoxia, as well as other diseases associated with tissue hypoxia |
| 6 | Adaptation/acclimatization | Adaptation or acclimatization occurs in individuals residing at high altitudes for extended periods, including indigenous populations |
| 7 | Echocardiography | Echocardiography serves as a valuable diagnostic tool for identifying cardiac diseases in high-altitude environments |
The collaborations between countries have significantly advanced the understanding of the cardiovascular system at high altitude. The United States accounted for the highest number of publications. Many of these publications focused on subjects regarding the cardiovascular system at altitudes ≥ 4000 feet[28-33]. It should be noted that altitudes above 2000 m are generally considered as high altitudes. The risk of acute altitude illness is significantly higher at altitudes above 2500 m[34]. Therefore, it is not clear if all the studies included in this study can be considered as relevant for understanding the cardiovascular system at high altitude. Furthermore, except for China and Peru, the remaining eight countries in the top ten are considered as developed nations. Despite being categorized as a developing country, China ranks second in terms of publications in the field of the cardiovascular system at high altitude. This can be attributed to an extensive population residing at altitudes ≥ 3500 m in China[1]. Moreover, the world's highest plateau, the Qinghai-Tibet Plateau, is in China[35]. Peru is another country with a significant population residing at high altitude. Those residing at high altitude regions develop a variety of diseases, including diseases of the cardiovascular system. Therefore, extensive research has been conducted in these countries on the cardiovascular system at high altitude. Universidad Peruana Cayetano Heredia is one of the top ten institutions that have focused on studying cardiac health at high altitude[36,37].
The most cited author in this field was Peter Bärtsch from the Departments of Internal Medicine and Outpatient Medicine, Heidelberg University, Heidelberg, Germany. Luks et al[38] focused on the clinical manifestations, epidemiology, pathophysiology, and treatment of common diseases at high altitude[38]. Bärtsch and Gibbs[24] also described the acute physiological adjustments and early acclimatization of the cardiovascular system in healthy individuals who visited places at high altitude as well as altitude tolerance in patients with underlying cardiovascular diseases[24]. Furthermore, Bärtsch et al[39] also described the health risks for athletes at high altitude and the methods by which the performance of athletes can be improved at high altitude[39,40]. The second most highly cited author in this field was Martin Burtscher from the Department of Sport Science, University of Innsbruck, Austria. This is also an institution with the fourth highest number of publications. Burtscher and Ponchia[41] published reports focused on the cardiovascular system at high altitude[41-43], treatment and prevention recommendations of hypoxia-related altitude illnesses[44,45], and exercise at high altitude[46]. The third most highly cited research scholar was John B West from the Department of Medicine, University of California San Diego, La Jolla, United States. West[47] has published articles regarding high altitude-related medicine and physiology[47,48], the technology of oxygen enrichment in room air[2,49], and pulmonary function at high altitude[50,51]. University of California, San Diego is also one of the top ten institutions for publications in the field of cardiovascular system at high altitude because of major contributions from John B West.
Keywords reflect the core themes and main content of an article. Therefore, they highlight the research hotspots in a specialized field and provide directions for future research. Based on the top 20 keywords in this study, exercise at high altitude was identified as an important research hotspot. Previous reports have shown that visits to an area at high altitude may result in AMS or CMS; the heart undergoes a range of pathophysiological changes resulting in pulmonary hypertension, oxidative stress, and altered metabolism[22]. In the highlanders, changes in heart rate, blood pressure, nitric oxide (NO) levels, and cardiac output are closely related with altitude adaptation and acclimatization. Furthermore, echocardiography is a useful tool for diagnosing cardiac diseases at high altitude.
Exercise at high altitude: Hypoxia training is a useful strategy for improving the performance of athletes. Intense physical activity, including training at high altitude or mountaineering, does not increase the prevalence or severity of AMS at moderate altitudes[40]. A meta-analysis demonstrated that training at natural or simulated altitude improved high intensity intermittent running performance of the team-sport athletes[52]. Several contemporary elite endurance athletes incorporate some form of altitude/hypoxic training within their year-round training plan to improve their performance[53]. However, intermittent hypoxia at rest does not improve athletic performance in competitions held at sea level[39]. Therefore, exercise training is recommended to improve adaptation at high altitude[54]. Pulmonary artery pressure is elevated at high altitude because of vasoconstriction. Acute hypoxia leads to closure of the oxygen-sensitive potassium channels in the vascular smooth muscle cells; subsequent depolarization induces calcium influx and contraction of the smooth muscle cells[55]. Chronic exposure to hypoxia increases pulmonary artery pressure in the highlanders, but the criteria for the diagnosis of HAPH are not clear. The prevalence of HAPH varied significantly among the highlanders depending on the diagnostic criteria. The prevalence of HAPH in the highlanders was 6% according to the expert consensus definition of chronic high-altitude disease and 35% according to the current definition of pulmonary hypertension proposed for the lowlanders[56]. Chronic exposure to high altitude is also associated with arterial remodeling[57]. The proliferation of vascular smooth muscle cells in the alveolar wall is one of the first remodeling events that continues even after the elimination of hypoxic stimulation[58]. Furthermore, hypoxia promoted smooth muscle cell proliferation and pulmonary vascular thickening by impairing endothelial cell membrane integrity and stimulating the secretion of growth factors[59]. Moreover, chronic hypoxia promoted smooth muscle cell proliferation and pulmonary vascular thickening by maintaining fibroblasts in an activated state through epigenetic regulatory mechanisms[60].
Oxidative stress at high altitude: Oxidative stress is involved in the development of AMS, CMS, and HAPA[7]. Oxidative stress is elevated at higher altitude and may persist until return to the sea level. Exposure to hypoxia alters several signaling pathways, including generation of higher levels of reactive oxygen species that may activate important adaptive responses[61]. Endothelial cell function is affected by hypoxia and oxidative stress. Furthermore, persistent impairment in the vascular function of lowlanders after exposure to high altitude is in part attributed to increased oxidative stress[62]. Hu et al[63] demonstrated that the activity of the large-conductance Ca2+-activated K+ channels in the uterine arteries of pregnant sheep was inhibited by increased oxidative stress in an hypoxic environment.
Altered cardiovascular function at high altitude: Major changes are observed in the cardiovascular function of subjects upon exposure to high altitudes, including increased left ventricular systolic function, preserved right ventricular systolic function, and changes in biventricular diastolic filling pattern without changing filling pressure[22]. These changes can be explained by varying degrees of sympathetic activation, reduction of preload, and the effects of long-term hypoxia on the myocardial muscle strength. High altitude exposure initiates the cardiovascular response that is associated with increased sympathetic activities, increased cardiac output with tachycardia, absence of any change in output per vibration, and marginal increase in blood pressure temporarily[64]. After a few days of acclimation, cardiac output returns to normal, but stroke volume is reduced because the heart rate continues to increase. Furthermore, pulmonary artery pressure is elevated but the pulmonary artery wedge pressure remains unchanged[65]. It is worth noting that increased cardiac output is proportionally reduced to arterial oxygen levels so that the total amount of oxygen delivered to the tissues remain constant. However, these changes in the cardiovascular system in response to hypoxia are temporary. The cardiac output returns to normal after a few days and the changes plateau after a certain time of exposure at high altitude[66]. The HIF signaling pathway is altered at high altitude and is crucial for acclimatization. EGLN1 and EPAS1 are major regulators of the hypoxic response[67-69].
Short-term exposure to high altitude causes hypoxia, which induces dilation of blood vessels resulting in decreased blood pressure; subsequently, rapid activation of the sympathetic nerve promotes contraction of the blood vasculature; therefore, blood pressure remains unchanged or slightly increased[22,70,71]. The prevalence of hypertension is higher upon long-term exposure to high altitude; the incidence of hypertension increased by 2% for every 100 m increase in altitude in areas above 3000 m[72]. Aryal et al[73] performed a meta-analysis of 21 articles that included 40845 Tibetan residents living at 2400 m above sea level and reported that the average systolic and diastolic blood pressure increased by 17 mmHg and 9.5 mmHg, respectively, for an elevation of 1000 m[73]. However, long-term intermittent exposure to high altitude did not significantly alter blood pressure[74]. The increase in blood pressure at high altitude was proportional to an increase in the plasma levels of norepinephrine. This suggested that norepinephrine plays a key role in the activation of sympathetic nerves. However, the use of α- and β-receptor blockers did not completely restore blood pressure back to normal. This suggested that other mechanisms such as erythrocytosis and the renin-angiotensin system also participate in the elevation of increase of blood pressure at high altitude[24].
Metabolomics at high altitude: Metabolomics is a promising tool for discovering and understanding the novel bio
NO is a critical regulatory molecule in vivo that regulates oxygen transport cascade from the lung to the cardiovascular system, blood, and the mitochondria[81,82]. A 2-d exposure of rats to hypobaric hypoxia increased NO synthesis and promoted cardioprotective mechanisms[83]. NO is important for the pulmonary circulation response to acute and chronic hypoxia. Elevated levels of the endothelial nitric oxide synthase played a counterregulatory role in the pulmonary vasoconstriction response to acute hypoxia in Tibetan sheep adapated to high altitude[84]. Gonzales et al[85] also showed upregulation of the heart mitochondrial nitric oxide synthase in male rats exposed to high altitude[85].
Echocardiography for diagnosis of heart diseases at high altitude: Ultrasound is widely used in the diagnosis of heart disease at high altitude. Echocardiography is used to screen for congenital heart disease in newborns at high altitude[86]. Ultrasound is the best method for the clinical assessment of AMS[87]. Boussuges et al[88] performed echocardiography on eight subjects at different altitudes simulating a climb of Mount Everest and found elevated pulmonary artery pressure, normal left ventricular ejection fraction, reduced biventricular systolic and end-diastolic volumes, and decreased mitral early maximal ventricular filling velocity/atrial maximal ventricular filling velocity (E/A) ratio. A study of the echocardiographic changes in 41 healthy volunteers who rapidly ascended to 4559 m within 24 h demonstrated elevation of the tricuspid gradient from 16 to 44 mmHg and the mean pulmonary artery pressure to 32 mmHg, and reduction of the mitral E/A ratio from 1.4 to 1.1; this demonstrated atrial contractile fitness rather than a change in the diastolic function[70]. Echocardiography measurements of 58 plain residents exposed to a 4000 m altitude showed the following characteristics: Mean pulmonary artery pressure increased to 20-25 mmHg; E/A ratio of the right and left ventricles decreased; isovolumic relaxation time of the right ventricle prolonged; the Tei index of the right ventricle increased; and the ejection fraction remained normal; moreover, the pulmonary artery pressure increased further when the subjects were exposed to conditions simulating an altitude of 4850 m[89]. Compared with lowland residents, highlanders showed lower pulmonary arterial pressure, higher oxygen saturation, significant changes in the biventricular diastolic function, reduced left ventricular ejection fraction, and a more pronounced increase in the Tei index of the right ventricle[89].
In the present study, we performed a bibliometric analysis of publications in the field of the cardiovascular system at high altitude to identify the future research hotspots and new perspectives. Our data show that publications have increased rapidly over the past few decades in the field of the cardiovascular system at high altitude. Future research in this field may focus on areas such as hypoxia adaptation, metabolism, and cardiopulmonary exercise. Our study provides essential information for researchers in this field and identifies potential collaborative partners to further exploration of the pathophysiological changes in the high-altitude cardiovascular system and provide a theoretical basis for standardized disease diagnosis and treatment. The present study has several limitations. First, to ensure the quality and integrity of the collected data, this study selected articles and reviews from the WoS Core Collection of SCIE and excluded other databases such as Scopus. Thus, the data may not be comprehensive enough. Furthermore, quantitative analysis needs to analyze and interpret the data. This requires researchers with an adequate and comprehensive understanding of the field. Otherwise it will result in subjectivity. In the future research, we need to integrate the literature from multiple databases to diversify the data, and actively communicate with the scholars in this field to understand the frontier subjects of research in the cardiovascular system at high altitude.
| 1. | Tremblay JC, Ainslie PN. Global and country-level estimates of human population at high altitude. Proc Natl Acad Sci U S A. 2021;118. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 215] [Article Influence: 43.0] [Reference Citation Analysis (4)] |
| 2. | West JB. Barcroft's bold assertion: All dwellers at high altitudes are persons of impaired physical and mental powers. J Physiol. 2016;594:1127-1134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (5)] |
| 3. | Herrera EA, Farías JG, Ebensperger G, Reyes RV, Llanos AJ, Castillo RL. Pharmacological approaches in either intermittent or permanent hypoxia: A tale of two exposures. Pharmacol Res. 2015;101:94-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Chang JC, Lien CF, Lee WS, Chang HR, Hsu YC, Luo YP, Jeng JR, Hsieh JC, Yang KT. Intermittent Hypoxia Prevents Myocardial Mitochondrial Ca(2+) Overload and Cell Death during Ischemia/Reperfusion: The Role of Reactive Oxygen Species. Cells. 2019;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 61] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 5. | Aguilar M, González-Candia A, Rodríguez J, Carrasco-Pozo C, Cañas D, García-Herrera C, Herrera EA, Castillo RL. Mechanisms of Cardiovascular Protection Associated with Intermittent Hypobaric Hypoxia Exposure in a Rat Model: Role of Oxidative Stress. Int J Mol Sci. 2018;19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 6. | Lüscher TF. Refining cardiovascular risk: anthropometric measures, potassium, high altitude exposure, and cancer therapy. Eur Heart J. 2018;39:1499-1502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Pena E, El Alam S, Siques P, Brito J. Oxidative Stress and Diseases Associated with High-Altitude Exposure. Antioxidants (Basel). 2022;11:267. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 118] [Article Influence: 29.5] [Reference Citation Analysis (0)] |
| 8. | He S, He S, Yang Y, Li B, Gao L, Xie Q, Zhang L. Correlation Between Neutrophil to Lymphocyte Ratio and Myocardial Injury in Population Exposed to High Altitude. Front Cardiovasc Med. 2021;8:738817. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | He S, Zhang Q, Wu F, Chen J, He S, Ji Z, Li B, Gao L, Xie Q, Zhang J. Influence of cigarettes on myocardial injury in healthy population after exposure to high altitude over 5000 m. Sci Total Environ. 2023;855:158824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 10. | Sampson M, Horsley T, Doja A. A bibliometric analysis of evaluative medical education studies: characteristics and indexing accuracy. Acad Med. 2013;88:421-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Abramo G, D’Angelo CA, Viel F. The field-standardized average impact of national research systems compared to world average: the case of Italy. Scientometrics. 2011;88:599-615. [RCA] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 56] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 12. | Du Y, Duan C, Yang Y, Yuan G, Zhou Y, Zhu X, Wei N, Hu Y. Heart Transplantation: A Bibliometric Review From 1990-2021. Curr Probl Cardiol. 2022;47:101176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 13. | Wang H, Shi J, Shi S, Bo R, Zhang X, Hu Y. Bibliometric Analysis on the Progress of Chronic Heart Failure. Curr Probl Cardiol. 2022;47:101213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 54] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 14. | Xu X, Wang Y, Li Y, Zhang B, Song Q. The Future Landscape of Macrophage Research in Cardiovascular Disease: A Bibliometric Analysis. Curr Probl Cardiol. 2022;47:101311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 41] [Reference Citation Analysis (0)] |
| 15. | Zhang X, Zhou Y, Wei N, Shou X, Fan S, You Y, Li Y, Hu Y. A Bibliometric Analysis of Heart Failure with Preserved Ejection Fraction From 2000 to 2021. Curr Probl Cardiol. 2022;47:101243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 16. | Yang J, Cheng C, Shen S, Yang S. Comparison of complex network analysis software: Citespace, SCI 2 and Gephi. Proceedings of the 2017 IEEE 2nd International conference on Big data analysis (ICBDA); 2017; Beijing, China. IEEE. 2017;169-172. [DOI] [Full Text] |
| 17. | Chen Y, Wu C. The hot spot transformation in the research evolution of maker. Scientometrics. 2017;113:1307-1324. [RCA] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84:523-538. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4505] [Cited by in RCA: 5659] [Article Influence: 332.9] [Reference Citation Analysis (2)] |
| 19. | Dzikowski P. A bibliometric analysis of born global firms. J Bus Res. 2018;85:281-294. [DOI] [Full Text] |
| 20. | Jankovic MP, Kaufmann M, Kindler CH. Active research fields in anesthesia: a document co-citation analysis of the anesthetic literature. Anesth Analg. 2008;106:1524-1533, table of contents. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Hackett PH, Roach RC. High-altitude illness. N Engl J Med. 2001;345:107-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 860] [Cited by in RCA: 872] [Article Influence: 34.9] [Reference Citation Analysis (0)] |
| 22. | Naeije R. Physiological adaptation of the cardiovascular system to high altitude. Prog Cardiovasc Dis. 2010;52:456-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 289] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 23. | Penaloza D, Arias-Stella J. The heart and pulmonary circulation at high altitudes: healthy highlanders and chronic mountain sickness. Circulation. 2007;115:1132-1146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 392] [Cited by in RCA: 456] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 24. | Bärtsch P, Gibbs JS. Effect of altitude on the heart and the lungs. Circulation. 2007;116:2191-2202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 273] [Cited by in RCA: 321] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 25. | Simonson TS, Yang Y, Huff CD, Yun H, Qin G, Witherspoon DJ, Bai Z, Lorenzo FR, Xing J, Jorde LB, Prchal JT, Ge R. Genetic evidence for high-altitude adaptation in Tibet. Science. 2010;329:72-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 755] [Cited by in RCA: 898] [Article Influence: 56.1] [Reference Citation Analysis (0)] |
| 26. | León-Velarde F, Maggiorini M, Reeves JT, Aldashev A, Asmus I, Bernardi L, Ge RL, Hackett P, Kobayashi T, Moore LG, Penaloza D, Richalet JP, Roach R, Wu T, Vargas E, Zubieta-Castillo G, Zubieta-Calleja G. Consensus statement on chronic and subacute high altitude diseases. High Alt Med Biol. 2005;6:147-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 366] [Cited by in RCA: 452] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 27. | Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23:685-713; quiz 786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4670] [Cited by in RCA: 5486] [Article Influence: 342.9] [Reference Citation Analysis (0)] |
| 28. | Cancienne JM, Diduch DR, Werner BC. High Altitude Is an Independent Risk Factor for Postoperative Symptomatic Venous Thromboembolism After Knee Arthroscopy: A Matched Case-Control Study of Medicare Patients. Arthroscopy. 2017;33:422-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 29. | Cancienne JM, Burrus MT, Diduch DR, Werner BC. High altitude is an independent risk factor for venous thromboembolism following arthroscopic rotator cuff repair: a matched case-control study in Medicare patients. J Shoulder Elbow Surg. 2017;26:7-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 30. | Damodar D, Donnally CJ 3rd, Sheu JI, Law TY, Roche MW, Hernandez VH. A Higher Altitude Is an Independent Risk Factor for Venous Thromboembolisms After Total Hip Arthroplasty. J Arthroplasty. 2018;33:2627-2630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 31. | Damodar D, Vakharia R, Vakharia A, Sheu J, Donnally CJ 3rd, Levy JC, Kaplan L, Munoz J. A higher altitude is an independent risk factor for venous thromboembolisms following total shoulder arthroplasty. J Orthop. 2018;15:1017-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 32. | Donnally CJ 3rd, Vakharia AM, Sheu JI, Vakharia RM, Damodar D, Shenoy K, Gjolaj JP. High Altitude Is an Independent Risk Factor for Developing a Pulmonary Embolism, but Not a Deep Vein Thrombosis Following a 1- to 2-Level Lumbar Fusion. Global Spine J. 2019;9:729-734. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 33. | Tyson JJ, Bjerke BP, Genuario JW, Noonan TJ. Thromboembolic Events After Arthroscopic Knee Surgery: Increased Risk at High Elevation. Arthroscopy. 2016;32:2350-2354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 34. | Johnson NJ, Luks AM. High-Altitude Medicine. Med Clin North Am. 2016;100:357-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 35. | Wu J, Duan D, Lu J, Luo Y, Wen X, Guo X, Boman BJ. Inorganic pollution around the Qinghai-Tibet Plateau: An overview of the current observations. Sci Total Environ. 2016;550:628-636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 42] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 36. | León-Velarde F, Villafuerte FC, Richalet JP. Chronic mountain sickness and the heart. Prog Cardiovasc Dis. 2010;52:540-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 75] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 37. | Maignan M, Rivera-Ch M, Privat C, Leòn-Velarde F, Richalet JP, Pham I. Pulmonary pressure and cardiac function in chronic mountain sickness patients. Chest. 2009;135:499-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 52] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 38. | Luks AM, Swenson ER, Bärtsch P. Acute high-altitude sickness. Eur Respir Rev. 2017;26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 162] [Cited by in RCA: 322] [Article Influence: 35.8] [Reference Citation Analysis (0)] |
| 39. | Bärtsch P, Dehnert C, Friedmann-Bette B, Tadibi V. Intermittent hypoxia at rest for improvement of athletic performance. Scand J Med Sci Sports. 2008;18 Suppl 1:50-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 40. | Schommer K, Menold E, Subudhi AW, Bärtsch P. Health risk for athletes at moderate altitude and normobaric hypoxia. Br J Sports Med. 2012;46:828-832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 41. | Burtscher M, Ponchia A. The risk of cardiovascular events during leisure time activities at altitude. Prog Cardiovasc Dis. 2010;52:507-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 74] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 42. | Burtscher M, Philadelphy M, Likar R. Sudden cardiac death during mountain hiking and downhill skiing. N Engl J Med. 1993;329:1738-1739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 63] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 43. | Faulhaber M, Gatterer H, Burtscher M. Preexisting cardiovascular diseases among high-altitude mountaineers in the alps. J Travel Med. 2011;18:355-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 44. | Netzer N, Strohl K, Faulhaber M, Gatterer H, Burtscher M. Hypoxia-related altitude illnesses. J Travel Med. 2013;20:247-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 108] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 45. | Burtscher M. Climbing the Himalayas more safely. BMJ. 2012;344:e3778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 46. | Gatterer H, Menz V, Salazar-Martinez E, Sumbalova Z, Garcia-Souza LF, Velika B, Gnaiger E, Burtscher M. Exercise Performance, Muscle Oxygen Extraction and Blood Cell Mitochondrial Respiration after Repeated-Sprint and Sprint Interval Training in Hypoxia: A Pilot Study. J Sports Sci Med. 2018;17:339-347. [PubMed] |
| 47. | West JB. High-altitude medicine. Am J Respir Crit Care Med. 2012;186:1229-1237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 190] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 48. | West JB. Physiological Effects of Chronic Hypoxia. N Engl J Med. 2017;376:1965-1971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 110] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 49. | West JB. Oxygen Conditioning: A New Technique for Improving Living and Working at High Altitude. Physiology (Bethesda). 2016;31:216-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 50. | West JB, Mathieu-Costello O. Stress failure of pulmonary capillaries: role in lung and heart disease. Lancet. 1992;340:762-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 156] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 51. | West JB. Comparative physiology of the pulmonary circulation. Compr Physiol. 2011;1:1525-1539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 52. | Hamlin MJ, Lizamore CA, Hopkins WG. The Effect of Natural or Simulated Altitude Training on High-Intensity Intermittent Running Performance in Team-Sport Athletes: A Meta-Analysis. Sports Med. 2018;48:431-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 53. | Wilber RL. Application of altitude/hypoxic training by elite athletes. Med Sci Sports Exerc. 2007;39:1610-1624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 129] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 54. | Grover RF, Weil JV, Reeves JT. Cardiovascular adaptation to exercise at high altitude. Exerc Sport Sci Rev. 1986;14:269-302. [PubMed] |
| 55. | Wilkins MR, Ghofrani HA, Weissmann N, Aldashev A, Zhao L. Pathophysiology and treatment of high-altitude pulmonary vascular disease. Circulation. 2015;131:582-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 106] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 56. | Lichtblau M, Saxer S, Furian M, Mayer L, Bader PR, Scheiwiller PM, Mademilov M, Sheraliev U, Tanner FC, Sooronbaev TM, Bloch KE, Ulrich S. Cardiac function and pulmonary hypertension in Central Asian highlanders at 3250 m. Eur Respir J. 2020;56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 57. | Lewis NC, Bailey DM, Dumanoir GR, Messinger L, Lucas SJ, Cotter JD, Donnelly J, McEneny J, Young IS, Stembridge M, Burgess KR, Basnet AS, Ainslie PN. Conduit artery structure and function in lowlanders and native highlanders: relationships with oxidative stress and role of sympathoexcitation. J Physiol. 2014;592:1009-1024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 70] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 58. | Mirrakhimov AE, Strohl KP. High-altitude Pulmonary Hypertension: an Update on Disease Pathogenesis and Management. Open Cardiovasc Med J. 2016;10:19-27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 65] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 59. | Robinson JC, Abbott C, Meadows CA, Roach RC, Honigman B, Bull TM. Long-Term Health Outcomes in High-Altitude Pulmonary Hypertension. High Alt Med Biol. 2017;18:61-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 60. | Li M, Riddle SR, Frid MG, El Kasmi KC, McKinsey TA, Sokol RJ, Strassheim D, Meyrick B, Yeager ME, Flockton AR, McKeon BA, Lemon DD, Horn TR, Anwar A, Barajas C, Stenmark KR. Emergence of fibroblasts with a proinflammatory epigenetically altered phenotype in severe hypoxic pulmonary hypertension. J Immunol. 2011;187:2711-2722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 189] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 61. | Askew EW. Work at high altitude and oxidative stress: antioxidant nutrients. Toxicology. 2002;180:107-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 155] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 62. | Stone RM, Ainslie PN, Tremblay JC, Akins JD, MacLeod DB, Tymko MM, DeSouza CA, Bain AR. GLOBAL REACH 2018: intra-arterial vitamin C improves endothelial-dependent vasodilatory function in humans at high altitude. J Physiol. 2022;600:1373-1383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 63. | Hu XQ, Huang X, Xiao D, Zhang L. Direct effect of chronic hypoxia in suppressing large conductance Ca(2+)-activated K(+) channel activity in ovine uterine arteries via increasing oxidative stress. J Physiol. 2016;594:343-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 64. | Hainsworth R, Drinkhill MJ, Rivera-Chira M. The autonomic nervous system at high altitude. Clin Auton Res. 2007;17:13-19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 111] [Cited by in RCA: 129] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 65. | Naeije R, Mélot C, Mols P, Hallemans R. Effects of vasodilators on hypoxic pulmonary vasoconstriction in normal man. Chest. 1982;82:404-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 81] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 66. | Vogel JA, Hartley LH, Cruz JC. Cardiac output during exercise in altitude natives at sea level and high altitude. J Appl Physiol. 1974;36:173-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 36] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 67. | Petousi N, Croft QP, Cavalleri GL, Cheng HY, Formenti F, Ishida K, Lunn D, McCormack M, Shianna KV, Talbot NP, Ratcliffe PJ, Robbins PA. Tibetans living at sea level have a hyporesponsive hypoxia-inducible factor system and blunted physiological responses to hypoxia. J Appl Physiol (1985). 2014;116:893-904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 105] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 68. | Xiang K, Ouzhuluobu, Peng Y, Yang Z, Zhang X, Cui C, Zhang H, Li M, Zhang Y, Bianba, Gonggalanzi, Basang, Ciwangsangbu, Wu T, Chen H, Shi H, Qi X, Su B. Identification of a Tibetan-specific mutation in the hypoxic gene EGLN1 and its contribution to high-altitude adaptation. Mol Biol Evol. 2013;30:1889-1898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 123] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 69. | Xin J, Zhang H, He Y, Duren Z, Bai C, Chen L, Luo X, Yan DS, Zhang C, Zhu X, Yuan Q, Feng Z, Cui C, Qi X, Ouzhuluobu, Wong WH, Wang Y, Su B. Chromatin accessibility landscape and regulatory network of high-altitude hypoxia adaptation. Nat Commun. 2020;11:4928. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 64] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 70. | Allemann Y, Rotter M, Hutter D, Lipp E, Sartori C, Scherrer U, Seiler C. Impact of acute hypoxic pulmonary hypertension on LV diastolic function in healthy mountaineers at high altitude. Am J Physiol Heart Circ Physiol. 2004;286:H856-H862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 86] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 71. | Jung F, Palmer LA, Zhou N, Johns RA. Hypoxic regulation of inducible nitric oxide synthase via hypoxia inducible factor-1 in cardiac myocytes. Circ Res. 2000;86:319-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 239] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 72. | Mingji C, Onakpoya IJ, Perera R, Ward AM, Heneghan CJ. Relationship between altitude and the prevalence of hypertension in Tibet: a systematic review. Heart. 2015;101:1054-1060. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 92] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 73. | Aryal N, Weatherall M, Bhatta YK, Mann S. Blood Pressure and Hypertension in Adults Permanently Living at High Altitude: A Systematic Review and Meta-Analysis. High Alt Med Biol. 2016;17:185-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 74. | Vinnikov D, Brimkulov N, Krasotski V. Chronic Intermittent Hypoxia and Blood Pressure: Is There Risk for Hypertension in Healthy Individuals? High Alt Med Biol. 2016;17:5-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 75. | Koundal S, Gandhi S, Kaur T, Mazumder A, Khushu S. "Omics" of High Altitude Biology: A Urinary Metabolomics Biomarker Study of Rats Under Hypobaric Hypoxia. OMICS. 2015;19:757-765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 76. | Xie H, Xu G, Aa J, Gu S, Gao Y. Modulation of Perturbed Cardiac Metabolism in Rats Under High-Altitude Hypoxia by Combination Treatment With L-carnitine and Trimetazidine. Front Physiol. 2021;12:671161. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 77. | Leslie E, Lopez V, Anti NAO, Alvarez R, Kafeero I, Welsh DG, Romero M, Kaushal S, Johnson CM, Bosviel R, Blaženović I, Song R, Brito A, Frano MR, Zhang L, Newman JW, Fiehn O, Wilson SM. Gestational long-term hypoxia induces metabolomic reprogramming and phenotypic transformations in fetal sheep pulmonary arteries. Am J Physiol Lung Cell Mol Physiol. 2021;320:L770-L784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 78. | Guo L, Tan G, Liu P, Li H, Tang L, Huang L, Ren Q. Three plasma metabolite signatures for diagnosing high altitude pulmonary edema. Sci Rep. 2015;5:15126. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 79. | Liu C, Liu B, Liu L, Zhang EL, Sun BD, Xu G, Chen J, Gao YQ. Arachidonic Acid Metabolism Pathway Is Not Only Dominant in Metabolic Modulation but Associated With Phenotypic Variation After Acute Hypoxia Exposure. Front Physiol. 2018;9:236. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 80. | Liao WT, Liu B, Chen J, Cui JH, Gao YX, Liu FY, Xu G, Sun BD, Zhang EL, Yuan ZB, Zhang G, Gao YQ. Metabolite Modulation in Human Plasma in the Early Phase of Acclimatization to Hypobaric Hypoxia. Sci Rep. 2016;6:22589. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 81. | Moncada S, Higgs EA. The discovery of nitric oxide and its role in vascular biology. Br J Pharmacol. 2006;147 Suppl 1:S193-S201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 560] [Cited by in RCA: 614] [Article Influence: 30.7] [Reference Citation Analysis (0)] |
| 82. | Erusalimsky JD, Moncada S. Nitric oxide and mitochondrial signaling: from physiology to pathophysiology. Arterioscler Thromb Vasc Biol. 2007;27:2524-2531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 252] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 83. | La Padula PH, Etchegoyen M, Czerniczyniec A, Piotrkowski B, Arnaiz SL, Milei J, Costa LE. Cardioprotection after acute exposure to simulated high altitude in rats. Role of nitric oxide. Nitric Oxide. 2018;73:52-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 84. | Ruan Z, Koizumi T, Sakai A, Ishizaki T, Wang Z. Endogenous nitric oxide and pulmonary circulation response to hypoxia in high-altitude adapted Tibetan sheep. Eur J Appl Physiol. 2004;93:190-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 85. | Gonzales GF, Chung FA, Miranda S, Valdez LB, Zaobornyj T, Bustamante J, Boveris A. Heart mitochondrial nitric oxide synthase is upregulated in male rats exposed to high altitude (4,340 m). Am J Physiol Heart Circ Physiol. 2005;288:H2568-H2573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 33] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 86. | Li JJ, Liu Y, Xie SY, Zhao GD, Dai T, Chen H, Mu LF, Qi HY, Li J. Newborn screening for congenital heart disease using echocardiography and follow-up at high altitude in China. Int J Cardiol. 2019;274:106-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 87. | Russell TC, Crawford PF. Ultrasound in the austere environment: a review of the history, indications, and specifications. Mil Med. 2013;178:21-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 88. | Boussuges A, Molenat F, Burnet H, Cauchy E, Gardette B, Sainty JM, Jammes Y, Richalet JP. Operation Everest III (Comex '97): modifications of cardiac function secondary to altitude-induced hypoxia. An echocardiographic and Doppler study. Am J Respir Crit Care Med. 2000;161:264-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 103] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 89. | Huez S, Faoro V, Guénard H, Martinot JB, Naeije R. Echocardiographic and tissue Doppler imaging of cardiac adaptation to high altitude in native highlanders versus acclimatized lowlanders. Am J Cardiol. 2009;103:1605-1609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 69] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ong H, Malaysia S-Editor: Li L L-Editor: Wang TQ P-Editor: Zhao S