Published online Feb 26, 2024. doi: 10.4330/wjc.v16.i2.49
Peer-review started: October 28, 2023
First decision: December 29, 2023
Revised: December 30, 2023
Accepted: January 11, 2024
Article in press: January 11, 2024
Published online: February 26, 2024
Processing time: 115 Days and 12.4 Hours
Transcatheter aortic valve replacement (TAVR) has emerged as a formidable treatment option for severe symptomatic aortic stenosis ahead of surgical aortic valve replacement. The encouraging results from large randomized controlled trials has resulted in an exponential rise in the use of TAVR even in the low-risk patients. However, this is not without challenges. Need for permanent pacemaker (PPM) post-TAVR remains the most frequent and clinically relevant challenge. Naturally, identifying risk factors which predispose an individual to develop high grade conduction block post-TAVR is important. Various demographic factors, electrocardiographic features, anatomic factors and procedural characteristics have all been linked to the development of advanced conduction block and need for PPM following TAVR. Amongst these electrophysiological variables, most notably a prolonged QRS > 120 ms regardless of the type of conduction block seems to be one of the strongest predictors on logistic regression models. The index study by Nwaedozie et al highlights that patients requiring PPM post-TAVR had higher odds of having a baseline QRS > 120 ms and were more likely to be having diabetes mellitus that those who did not require PPM.
Core Tip: Transcatheter aortic valve replacement (TAVR) has emerged as a formidable treatment option for severe symptomatic aortic stenosis ahead of surgical aortic valve replacement. Despite the progress in technology, the improved valve-design and delivery systems, and the improvement in clinical skill and deployment techniques, permanent pacemaker (PPM) implantation remains a major cause of concern post-TAVR. Naturally, identifying risk factors which predispose an individual to develop high grade conduction block post-TAVR is relevant. In the index study by Nwaedozie et al, a baseline QRS > 120 ms and the presence of diabetes mellitus were strongest predictors of PPM need post-TAVR.
- Citation: Batta A, Hatwal J. Risk of permanent pacemaker implantation following transcatheter aortic valve replacement: Which factors are most relevant? World J Cardiol 2024; 16(2): 49-53
- URL: https://www.wjgnet.com/1949-8462/full/v16/i2/49.htm
- DOI: https://dx.doi.org/10.4330/wjc.v16.i2.49
Over the last 2 decades, transcatheter aortic valve replacement (TAVR) has emerged as a formidable treatment option for severe symptomatic aortic stenosis ahead of surgical aortic valve replacement (SAVR). Encouraging results from large randomized controlled trials (RCTs) has resulted in expansion of its use even in the younger population with low surgical risk[1,2]. This ever-increasing volume of TAVR is expected to be coupled with complications which will have significant long-term impact. Amongst them, conduction disturbances leading to permanent pacemaker (PPM) implantation is one of the most relevant challenge. The rate of PPM implantation is around 5%-33% of all patients undergoing TAVR[3-5]. This is thought to result from a mechanical injury, ischemia, hemorrhage or associated inflammation in the conduction system which passes posterior-inferiorly to the non-coronary cusp of the aortic valve[6]. Despite the progress in technology leading to improved valve-designs and delivery systems, and improvement in clinical skill and deployment techniques, PPM implantation remains a major cause of concern post-TAVR[6]. Long-term right ventricular pacing has adverse impact on cardiac hemodynamics, chamber dimensions and ventricular functions all of which contribute to increased morbidity and mortality in the long run[7]. Although long-term impact of PPM after TAVR has been sparingly studied, emerging data points to the worse clinical outcomes in this population following PPM[8]. This association is most relevant today younger patients are who are expected to live longer are increasingly undergoing TAVR and will be most vulnerable to long-term impact of PPM. Traditionally, PPM implantation rate following SAVR is around 2-7%, which in general is lower than PPM need after TAVR. Hence, choosing between SAVR and TAVR in low-risk younger patients should take into account the risk of PPM implantation and its long-term impact[9,10]. Naturally, knowledge and awareness of preprocedural characteristics that predispose an individual to develop high-grade conduction disturbances following TAVR remains critical.
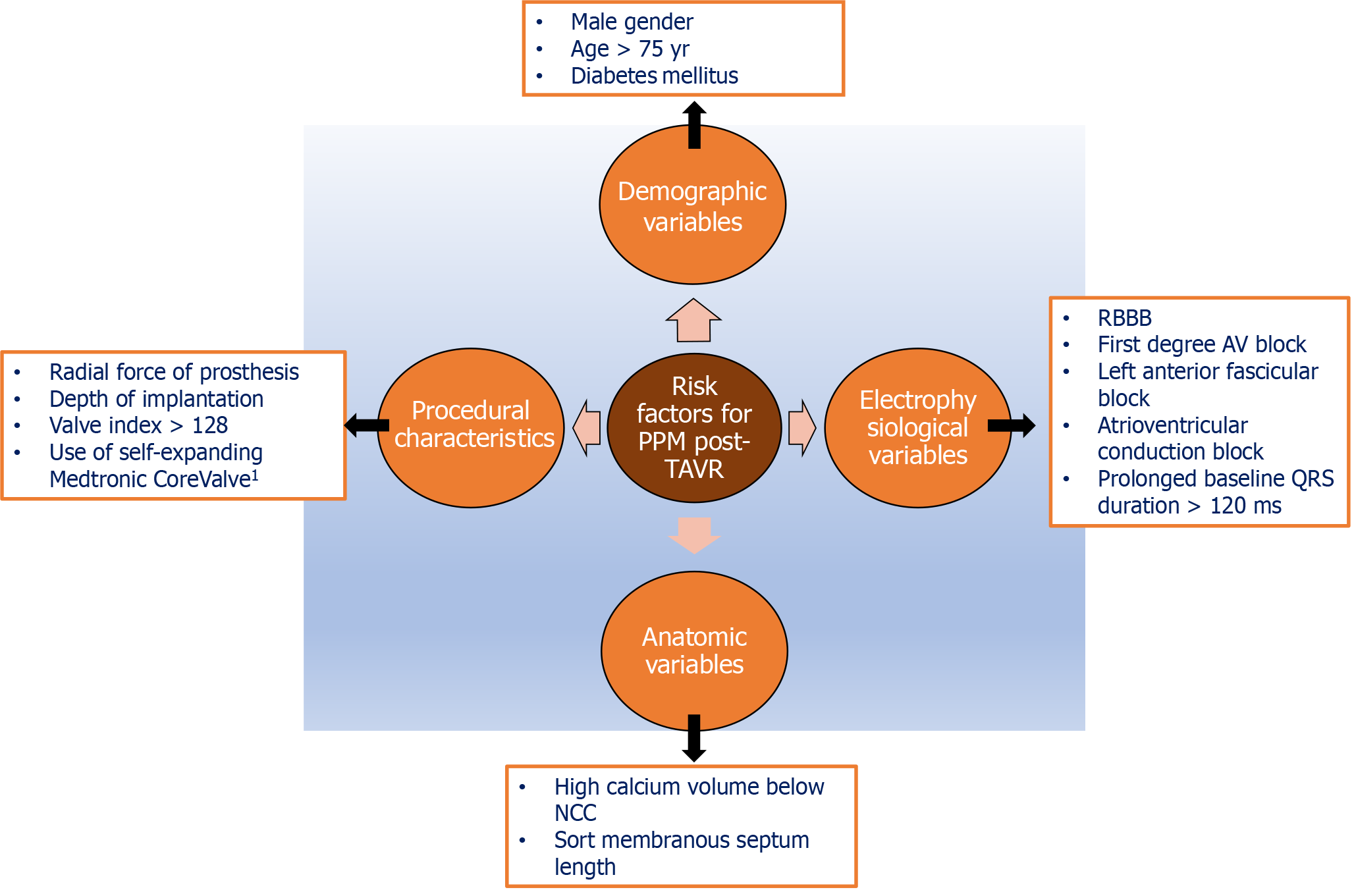
As we enter the 3rd decade since the first reported use of TAVR in humans in 2002, an ever-increasing pool of data is available to clinicians and researchers to draw meaningful conclusions and ultimately improve patient outcomes. Large scale RCTs and the subsequent meta-analysis have shed light on the risk factors for PPM after TAVR. Various demographic factors, electrocardiographic features, anatomic factors and procedural characteristics have all been linked to the development of advanced conduction blocks and need for PPM following TAVR[5,11,12]. Evidence from various high-quality studies on the predictors of PPM need following TAVR has been depicted in Figure 1. Overall, the risk factors which appear to be the most closely linked to the risk of PPM following TAVR are diabetes mellitus (DM), presence of baseline RBBB or left anterior fascicular block, short membranous septum length, high volume calcium just below the non-coronary and the right coronary cusps, increased depth of valve implantation, utilization of larger valves with resultant large valve index[(valve size/LVOT diameter) × 100 > 128)] and the use of self-expanding valve in particular the Medtronic CoreValve systems (Medtronic, Inc.; Minneapolis, MN)[5,11-15].
The most recent evidence on the predictors of PPM following TAVR comes from the study by Nwaedozie et al[16] in which they have explored various risk factors (particularly focusing on electrophysiological variables) for PPM in patients undergoing TAVR at their centre over the last decade. In this retrospective study they conclude that the presence of DM and prolonged baseline QRS > 120 ms regardless of the type of conduction block were the strongest predictors on logistic regression model for need for PPM post-TAVR. While the results of the study are not entirely novel, the study does add to the existing pool of literature. They highlight that baseline QRS prolongation (> 120 ms) even without underlying LBBB or RBBB is an independent and a strong predictor for need for PPM. Even those with QRS 100-120 ms were found to have higher odds of needing PPM following TAVR in their study than those with a QRS < 100 ms. This is unlike previous data which suggested that it was RBBB more than other conduction disturbances that predicted PPM need. A prolonged QRS represents conduction delays from the atrioventricular node to the ventricular purkinje system. Even in general population, a prolonged QRS without typical RBBB or LBBB is associated with worse long-term outcomes and increased likelihood of sudden cardiac death[17]. It often is present as a bystander in ischemic heart disease and is believed to be a precursor to both bradyarrhythmia and tachyarrhythmia in future. Whether TAVR aggravates this ischemia process or the surrounding inflammation impairs the already compromised conduction is still a matter of debate. The other major finding of the study was higher odds of DM amongst patients needing PPM. This is not surprising since DM impairs microcirculation throughout the cardiovascular system including the blood supply of the conduction tissue. Further a large recent nationwide Danish study highlighted the fact that DM patients have a higher likelihood of developing advanced conduction disease even in general population[18]. Also in the recent meta-analysis by Mahajan et al[5], DM was the only demographic variable on multivariable regression analysis which was independently linked to PPM following TAVR.
Another relevant area that the authors have touched upon is the clinical impact of PPM post TAVR. Unlike in general population, where the harmful effects of PPM are well established, the impact of PPM in TAVR patients is less studied and conflicting[19-22]. This study by Nwaedozie et al[16] is one of the few which highlights the negative impact of PPM post TAVR. They found higher odds of heart failure hospitalizations and non-fatal myocardial infarction amongst the PPM cohort at 1 year. However, the overall survival was similar in the 2 groups. Perhaps a longer follow-up would have further clarified the impact of PPM on mortality in these patients.
While the strength of the study is well apparent, one must take the results with a pinch of salt. Being a single-centre study with a retrospective study design, unaccounted biases cannot be ruled out. Hence, one cannot accept these results on their face value. Lack of validation arm is yet another limitation. Thus, generalizability of the study must be established in future studies before incorporating the evidence from the index study in our clinical practice.
The encouraging results from large RCTs has resulted in an exponential rise in the use of TAVR even in younger individuals at low-risk for surgery. Need for PPM post-TAVR remains the most frequent and clinically relevant challenge. Various risk factors have been identified and linked to PPM need following TAVR. As newer evidence emerges, our understanding of the pathophysiology improves and novel predictors are identified. Amongst them none seems to be more relevant that prolonged baseline QRS irrespective of the type of conduction block. Perhaps generating a tool or risk scoring system incorporating the current evidence seems to be the most promising approach for the future. The potential of artificial intelligence should be explored to identify and validate the emerging predictors.
| 1. | Popma JJ, Deeb GM, Yakubov SJ, Mumtaz M, Gada H, O'Hair D, Bajwa T, Heiser JC, Merhi W, Kleiman NS, Askew J, Sorajja P, Rovin J, Chetcuti SJ, Adams DH, Teirstein PS, Zorn GL 3rd, Forrest JK, Tchétché D, Resar J, Walton A, Piazza N, Ramlawi B, Robinson N, Petrossian G, Gleason TG, Oh JK, Boulware MJ, Qiao H, Mugglin AS, Reardon MJ; Evolut Low Risk Trial Investigators. Transcatheter Aortic-Valve Replacement with a Self-Expanding Valve in Low-Risk Patients. N Engl J Med. 2019;380:1706-1715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2802] [Cited by in RCA: 2840] [Article Influence: 405.7] [Reference Citation Analysis (0)] |
| 2. | Mack MJ, Leon MB, Thourani VH, Makkar R, Kodali SK, Russo M, Kapadia SR, Malaisrie SC, Cohen DJ, Pibarot P, Leipsic J, Hahn RT, Blanke P, Williams MR, McCabe JM, Brown DL, Babaliaros V, Goldman S, Szeto WY, Genereux P, Pershad A, Pocock SJ, Alu MC, Webb JG, Smith CR; PARTNER 3 Investigators. Transcatheter Aortic-Valve Replacement with a Balloon-Expandable Valve in Low-Risk Patients. N Engl J Med. 2019;380:1695-1705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3668] [Cited by in RCA: 3730] [Article Influence: 532.9] [Reference Citation Analysis (0)] |
| 3. | Abu Rmilah AA, Al-Zu'bi H, Haq IU, Yagmour AH, Jaber SA, Alkurashi AK, Qaisi I, Kowlgi GN, Cha YM, Mulpuru S, DeSimone CV, Deshmukh AJ. Predicting permanent pacemaker implantation following transcatheter aortic valve replacement: A contemporary meta-analysis of 981,168 patients. Heart Rhythm O2. 2022;3:385-392. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 30] [Reference Citation Analysis (4)] |
| 4. | Laynez A, Ben-Dor I, Barbash IM, Hauville C, Sardi G, Maluenda G, Xue Z, Satler LF, Pichard AD, Lindsay J, Waksman R. Frequency of conduction disturbances after Edwards SAPIEN percutaneous valve implantation. Am J Cardiol. 2012;110:1164-1168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 41] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 5. | Mahajan S, Gupta R, Malik AH, Mahajan P, Aedma SK, Aronow WS, Mehta SS, Lakkireddy DR. Predictors of permanent pacemaker insertion after TAVR: A systematic review and updated meta-analysis. J Cardiovasc Electrophysiol. 2021;32:1411-1420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 49] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 6. | Huang HD, Mansour M. Pacemaker Implantation After Transcatheter Aortic Valve Replacement: A Necessary Evil Perhaps But Are We Making Progress? J Am Heart Assoc. 2020;9:e016700. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 7. | Naqvi TZ, Chao CJ. Adverse effects of right ventricular pacing on cardiac function: prevalence, prevention and treatment with physiologic pacing. Trends Cardiovasc Med. 2023;33:109-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 36] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 8. | Lauten P, Costello-Boerrigter LC, Goebel B, Gonzalez-Lopez D, Schreiber M, Kuntze T, Al Jassem M, Lapp H. Transcatheter Aortic Valve Implantation: Addressing the Subsequent Risk of Permanent Pacemaker Implantation. J Cardiovasc Dev Dis. 2023;10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 9. | Robich MP, Schiltz NK, Johnston DR, Mick S, Krishnaswamy A, Iglesias RA, Hang D, Roselli EE, Soltesz EG. Risk Factors and Outcomes of Patients Requiring a Permanent Pacemaker After Aortic Valve Replacement in the United States. J Card Surg. 2016;31:476-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 10. | Young Lee M, Chilakamarri Yeshwant S, Chava S, Lawrence Lustgarten D. Mechanisms of Heart Block after Transcatheter Aortic Valve Replacement - Cardiac Anatomy, Clinical Predictors and Mechanical Factors that Contribute to Permanent Pacemaker Implantation. Arrhythm Electrophysiol Rev. 2015;4:81-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 68] [Article Influence: 6.8] [Reference Citation Analysis (4)] |
| 11. | Siontis GC, Jüni P, Pilgrim T, Stortecky S, Büllesfeld L, Meier B, Wenaweser P, Windecker S. Predictors of permanent pacemaker implantation in patients with severe aortic stenosis undergoing TAVR: a meta-analysis. J Am Coll Cardiol. 2014;64:129-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 413] [Cited by in RCA: 530] [Article Influence: 44.2] [Reference Citation Analysis (0)] |
| 12. | Sá MP, Van den Eynde J, Jacquemyn X, Erten O, Rodriguez R, Goldman S, Coady PM, Gnall E, Gray WA, Jarrett H, Abramson SV, Clavel MA, Pibarot P, Ramlawi B. Computed tomography-derived membranous septum length as predictor of conduction abnormalities and permanent pacemaker implantation after TAVI: A meta-analysis of observational studies. Catheter Cardiovasc Interv. 2023;101:1203-1213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 20] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 13. | Rudolph T, Droppa M, Baan J, Nielsen NE, Baranowski J, Hachaturyan V, Kurucova J, Hack L, Bramlage P, Geisler T. Modifiable risk factors for permanent pacemaker after transcatheter aortic valve implantation: CONDUCT registry. Open Heart. 2023;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 14. | Pavlicek V, Mahfoud F, Bubel K, Fries P, Ewen S, Böhm M, Scheller B, Ukena C. Prediction of conduction disturbances in patients undergoing transcatheter aortic valve replacement. Clin Res Cardiol. 2023;112:677-690. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 15. | Kawsara A, Sulaiman S, Alqahtani F, Eleid MF, Deshmukh AJ, Cha YM, Rihal CS, Alkhouli M. Temporal Trends in the Incidence and Outcomes of Pacemaker Implantation After Transcatheter Aortic Valve Replacement in the United States (2012-2017). J Am Heart Assoc. 2020;9:e016685. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 16. | Nwaedozie S, Zhang H, Najjar Mojarrab J, Sharma P, Yeung P, Umukoro P, Soodi D, Gabor R, Anderson K, Garcia-Montilla R. Novel predictors of permanent pacemaker implantation following transcatheter aortic valve replacement. World J Cardiol. 2023;15:582-598. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (4)] |
| 17. | Aro AL, Anttonen O, Tikkanen JT, Junttila MJ, Kerola T, Rissanen HA, Reunanen A, Huikuri HV. Intraventricular conduction delay in a standard 12-lead electrocardiogram as a predictor of mortality in the general population. Circ Arrhythm Electrophysiol. 2011;4:704-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 131] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 18. | Haxha S, Halili A, Malmborg M, Pedersen-Bjergaard U, Philbert BT, Lindhardt TB, Hoejberg S, Schjerning AM, Ruwald MH, Gislason GH, Torp-Pedersen C, Bang CN. Type 2 diabetes mellitus and higher rate of complete atrioventricular block: a Danish Nationwide Registry. Eur Heart J. 2023;44:752-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 19. | Sammour Y, Krishnaswamy A, Kumar A, Puri R, Tarakji KG, Bazarbashi N, Harb S, Griffin B, Svensson L, Wazni O, Kapadia SR. Incidence, Predictors, and Implications of Permanent Pacemaker Requirement After Transcatheter Aortic Valve Replacement. JACC Cardiovasc Interv. 2021;14:115-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 192] [Article Influence: 38.4] [Reference Citation Analysis (4)] |
| 20. | Ullah W, Zahid S, Zaidi SR, Sarvepalli D, Haq S, Roomi S, Mukhtar M, Khan MA, Gowda SN, Ruggiero N, Vishnevsky A, Fischman DL. Predictors of Permanent Pacemaker Implantation in Patients Undergoing Transcatheter Aortic Valve Replacement - A Systematic Review and Meta-Analysis. J Am Heart Assoc. 2021;10:e020906. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 21. | Nazif TM, Dizon JM, Hahn RT, Xu K, Babaliaros V, Douglas PS, El-Chami MF, Herrmann HC, Mack M, Makkar RR, Miller DC, Pichard A, Tuzcu EM, Szeto WY, Webb JG, Moses JW, Smith CR, Williams MR, Leon MB, Kodali SK; PARTNER Publications Office. Predictors and clinical outcomes of permanent pacemaker implantation after transcatheter aortic valve replacement: the PARTNER (Placement of AoRtic TraNscathetER Valves) trial and registry. JACC Cardiovasc Interv. 2015;8:60-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 353] [Cited by in RCA: 455] [Article Influence: 41.4] [Reference Citation Analysis (1)] |
| 22. | Urena M, Webb JG, Tamburino C, Muñoz-García AJ, Cheema A, Dager AE, Serra V, Amat-Santos IJ, Barbanti M, Immè S, Briales JH, Benitez LM, Al Lawati H, Cucalon AM, García Del Blanco B, López J, Dumont E, Delarochellière R, Ribeiro HB, Nombela-Franco L, Philippon F, Rodés-Cabau J. Permanent pacemaker implantation after transcatheter aortic valve implantation: impact on late clinical outcomes and left ventricular function. Circulation. 2014;129:1233-1243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 262] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Polewczyk A, Poland S-Editor: Liu JH L-Editor: A P-Editor: Zhao S