Published online Dec 26, 2024. doi: 10.4330/wjc.v16.i12.760
Revised: September 30, 2024
Accepted: November 8, 2024
Published online: December 26, 2024
Processing time: 221 Days and 8.6 Hours
Ventricular diverticula are a rare congenital cardiac disorder presenting with an extremely low incidence. The presence of an apical diverticulum of the right ventricle has been associated with other congenital heart diseases such as tetralogy of Fallot. An important defining characteristic of ventricular diverticula that separates them from aneurysms through imaging techniques, is that they possess myocardial contraction synchronous to the adjacent walls, contributing to the ventricular stroke volume, so they do not usually require surgical treatment.
A 15-year-old male, currently asymptomatic, in follow up due to a pulmonary valve prosthesis placement and a history of corrected tetralogy of Fallot at 18 months old, underwent a cardiac magnetic resonance imaging in February 2024. A diverticulum was detected in the apical inferolateral wall of the right ventricle, which was not documented in the cardiac magnetic resonance imaging prior to valve prosthesis placement.
Right ventricular diverticula are a rare entity. To this date we could not find another case of a pulmonary valve placement, followed by a right ventricular diverticulum appearance.
Core Tip: Cardiac magnetic resonance imaging characterization is the gold standard for classifying anatomical abnormalities of the right ventricular wall. In asymptomatic patients, conservative management and close follow-up are recommended since no arrhythmias or thrombotic events occurred after the diverticulum was discovered; However, in some cases where there is a high risk of thrombosis (when the diverticulum is large or associated with arrhythmias or other malformations such as ventricular septal defect), anticoagulation is recommended. Surgery also is mainly reserved for cases of large and symptomatic diverticula.
- Citation: Martinez Juarez D, Gomez Monterrosas O, Tlecuitl Mendoza A, Zamora Rosales F, Álvarez Calderón R, Cepeda Ortiz DA, Espinosa Solis EE. Right ventricular diverticulum following a pulmonary valve placement for correction of tetralogy of Fallot: A case report. World J Cardiol 2024; 16(12): 760-767
- URL: https://www.wjgnet.com/1949-8462/full/v16/i12/760.htm
- DOI: https://dx.doi.org/10.4330/wjc.v16.i12.760
Ventricular diverticula are a rare congenital cardiac disorder presenting with an extremely low incidence ratio of 0.013 to 0.016, both for right and left diverticula, appearing mainly in the anterolateral wall of the apex.
Ventricular diverticula are not common. Since 1940, 200 cases have been reported and only 18 to 20 cases belong to the right ventricle. Autopsy series have found an incidence of 0.4%, while computed tomography scans have reported a frequency of 2.2%[1].
The presence of an apical diverticulum of the right ventricle has been associated with other congenital heart diseases such as tetralogy of Fallot and ventricular septal defects. An important defining characteristic of ventricular diverticula that separates them from aneurysms through imaging techniques, is that they possess myocardial contraction like the adjacent walls, contributing to the ventricular stroke volume, so they are not usually treated surgically[2].
Among imaging modalities, echocardiography has been considered a good first approach to the diagnosis; However, cardiac magnetic resonance imaging (CMR) has risen as the main tool for morphological and functional characterization[3].
A 15-year-old male, currently asymptomatic, attends a CMR control study in February 2024, incidentally detecting a saccular lesion in the apical inferolateral wall of the right ventricle compatible with a ventricular diverticulum.
The patient is currently asymptomatic, in follow-up due to the placement of a pulmonary valve prosthesis and corrected tetralogy of Fallot.
Afterbirth diagnosis of tetralogy of Fallot, corrected at 18 months old, with placement of an infundibular patch, presenting satisfactory evolution; In the long-term follow-up, at the age of 11 years, he developed severe pulmonary insufficiency and main stenosis, as well as right ventricle and atrial enlargement, which triggered dyspnea to great exertion. A protocol for transcatheter pulmonary valve replacement surgery was successfully carried out in January 2023 (Table 1).
| Age | Event | Work up |
| 0 months | Diagnosis of tetralogy of Fallot | Tracking |
| 18 months | Tetralogy of Fallot correction | Infundibular patching and correction of IVC |
| 11 years | Onset of high-exertional dyspnea | Tracking |
| 14 years | Echocardiogram and MRI showed pulmonary insufficiency severe and main stenosis | A transcatheter pulmonary valve prosthesis replacement |
| 15 years | Incidental findings of diverticulum in right ventricle | Post-surgical follow-up with CMR |
On physical examination, the patient presented with normal vital signs, rhythmic heart sounds with pulmonary hyper flow, pulmonary auscultation was normal.
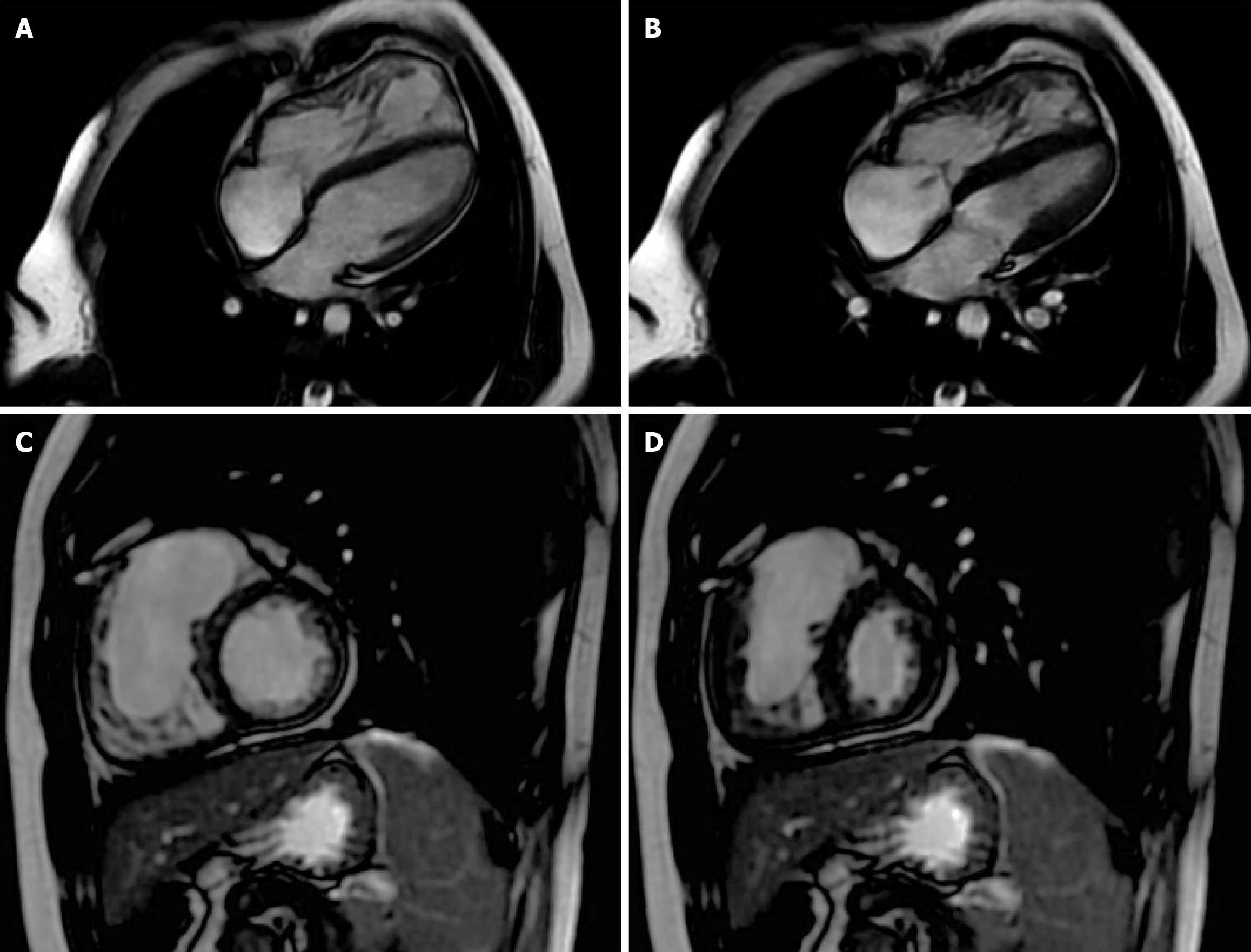
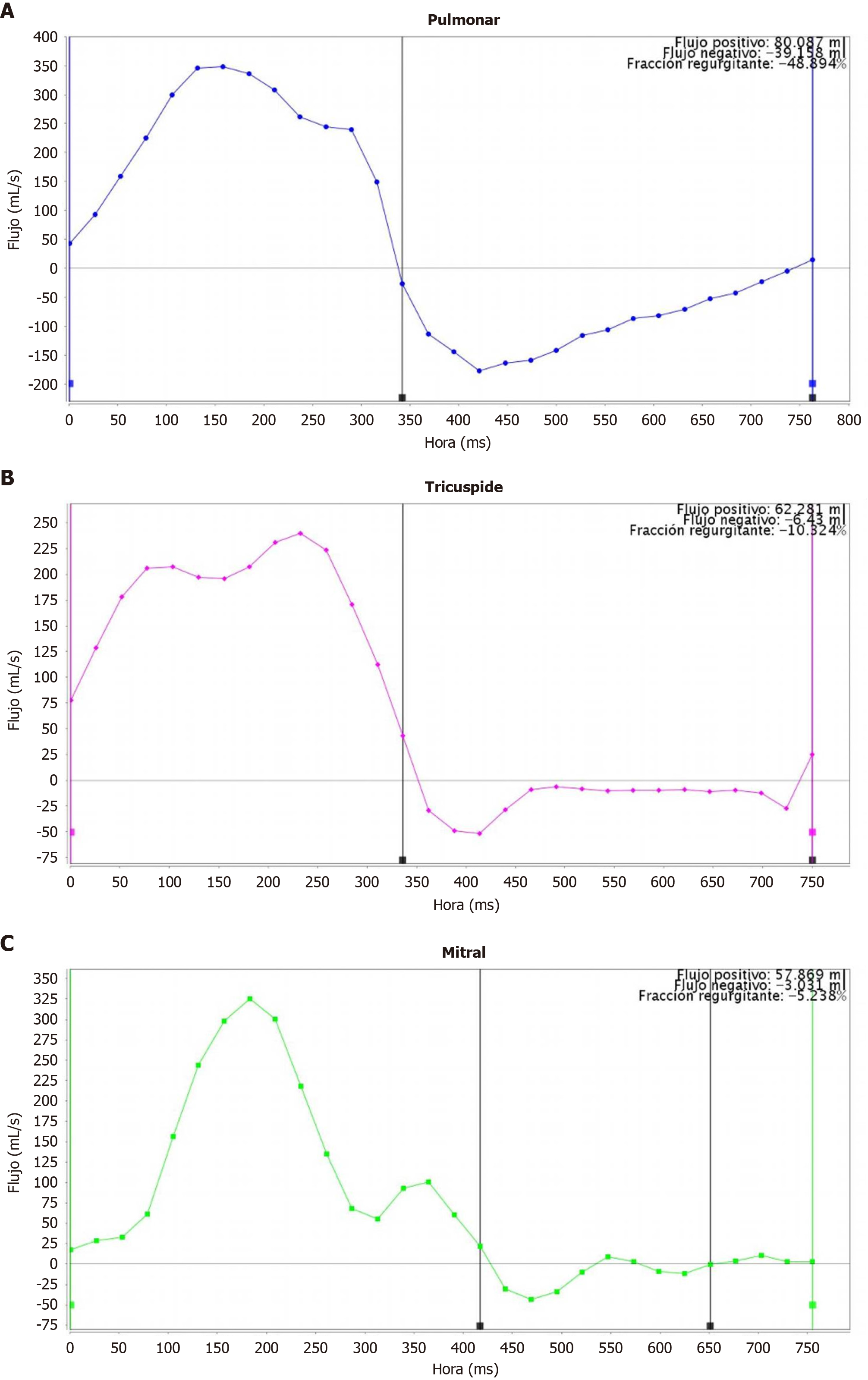
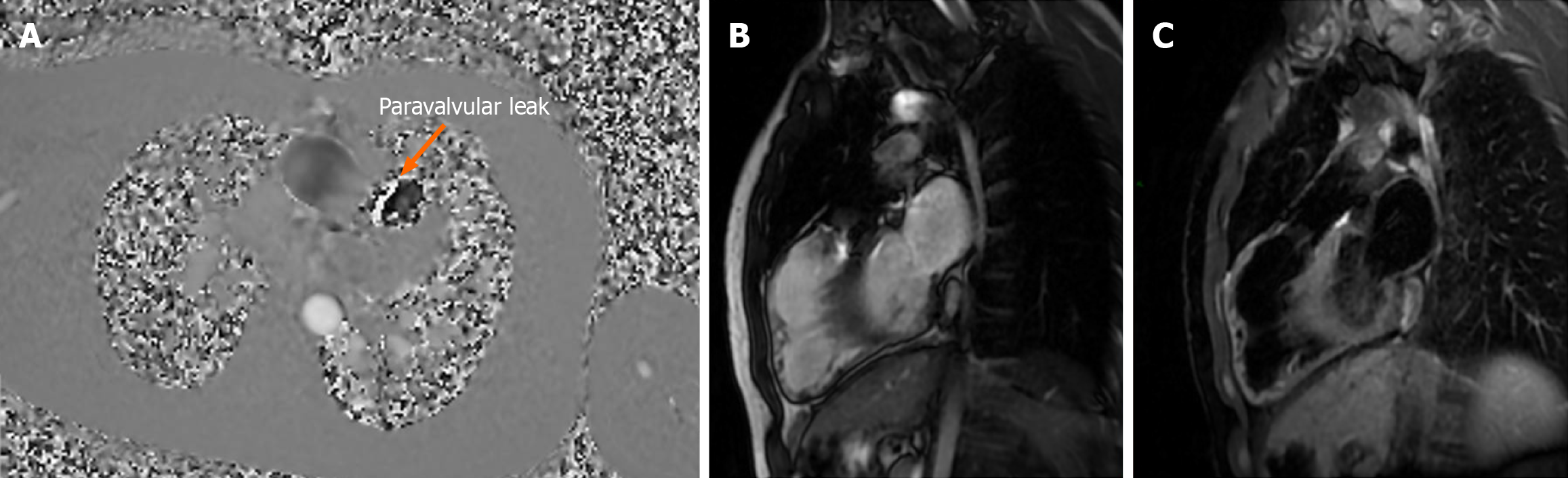
The patient was approached in the past for presenting dyspnea at great exertion, for which a transthoracic echocardiogram was performed in January 2022, reporting: Mild pulmonary stenosis, severe pulmonary failure and right ventricular dilation. Subsequently, in June 2022, contrasted magnetic resonance imaging (MRI) was performed as part of the pre-surgical protocol (Figure 1), identifying: Pulmonary valve showed severe pulmonary insufficiency and main stenosis: 2.2 meters/seconds; area: 2.5 cm2; regurgitant volume (RV): 30.1 mL; regurgitant fraction (RF): 48%. Tricuspid valve with RV: 6.4 mL; RF: 10.3%.
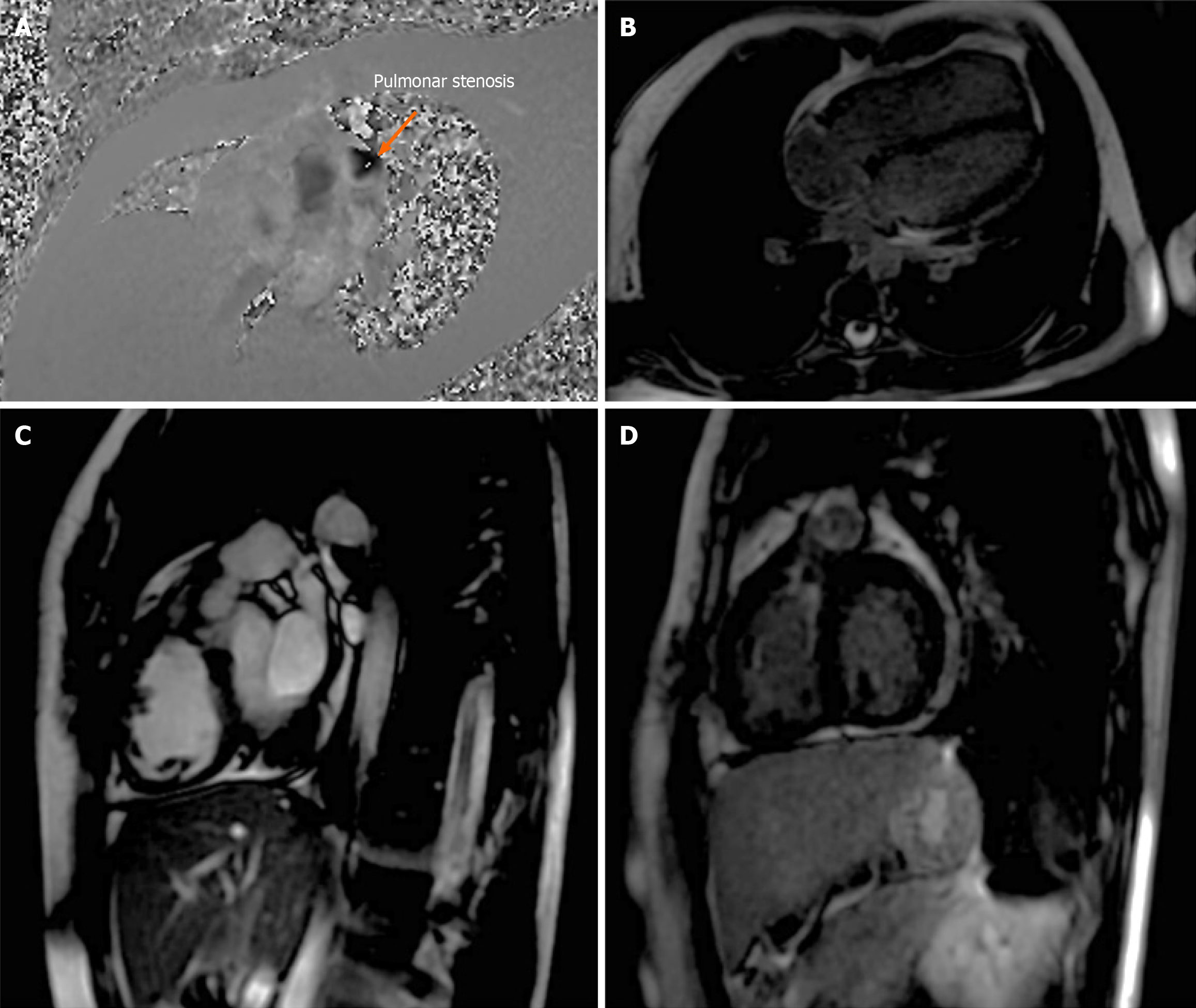
The late gadolinium enhancement (LGE) sequence showed enhancement of the right atrium wall, and the patch of the right ventricular outflow tract (RVOT). The study concluded a right ventricular dilation, mild pulmonary stenosis, moderate pulmonary insufficiency, and mild tricuspid regurgitation (Figure 2A and B, Figure 3).
Subsequently, a transcatheter pulmonary valve was placed in January 2023 without any incident being reported during the surgery.
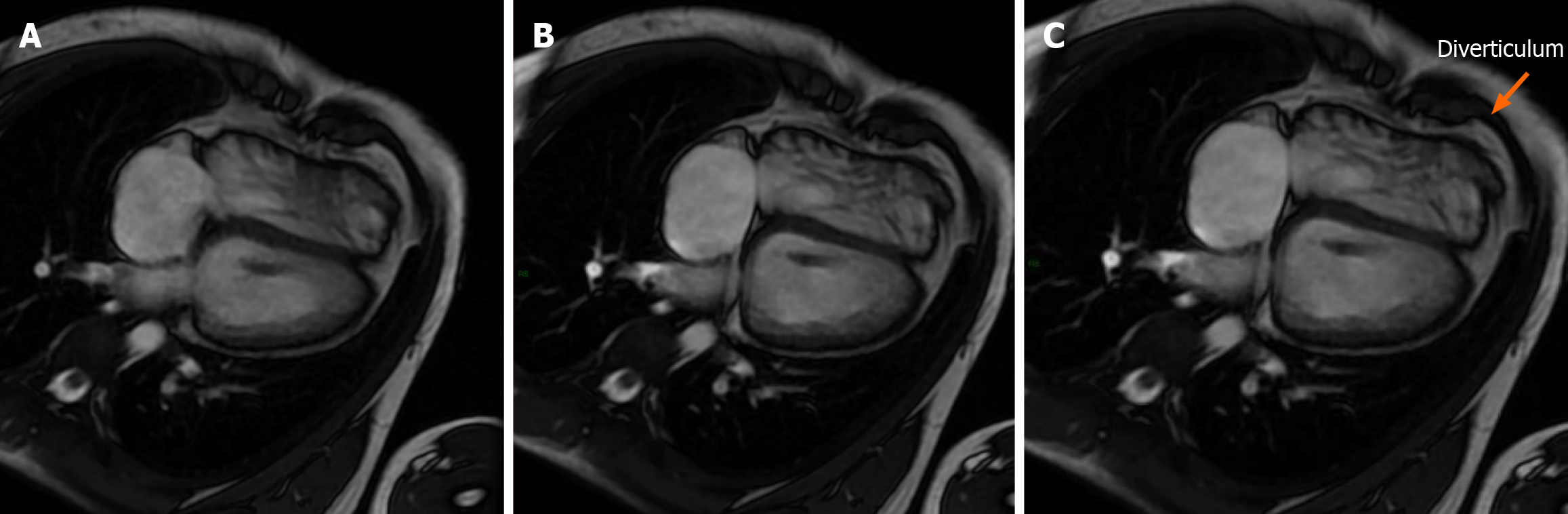
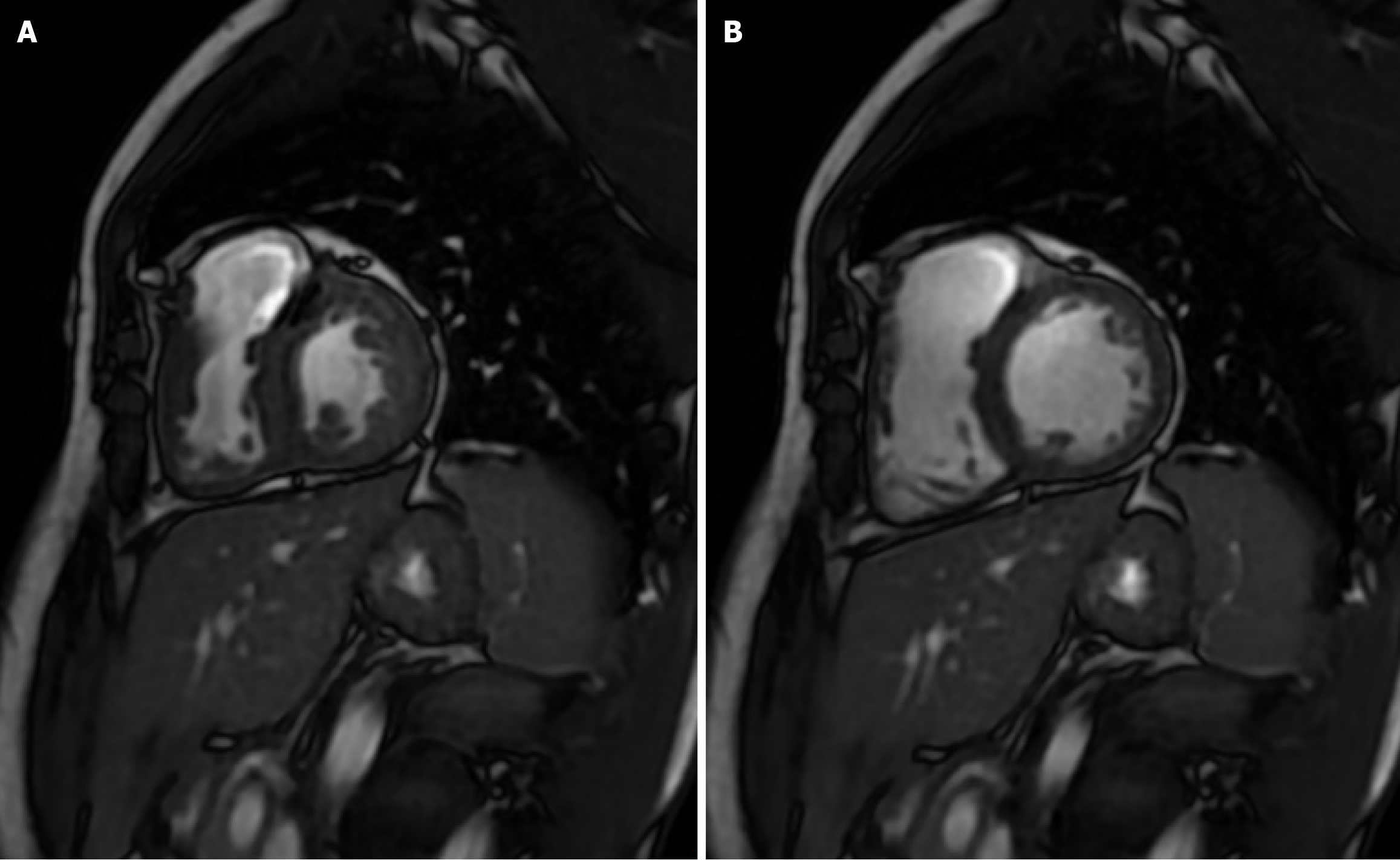
A follow-up MRI scan performed in February 2024 (Figure 4A and B) showed: Saccular image in the apical segment of the inferolateral wall of the right ventricle, which showed synchronous contraction, suggestive of diverticulum with a neck of 9 mm, longitudinal axis of 21 mm and transverse axis of 7 mm (Figure 4C).
Valve prosthesis with paravalvular leakage, regurgitant volume of 4.8 mL, and regurgitating fraction of 14.8% moderate-severe tricuspid regurgitation with regurgitant volume of 49.6% (Figure 2C and Figure 5). After surgery, the control MRI (Figure 6) showed a right ventricle of normal size.
It was concluded that the formation of a right ventricular diverticulum was associated with tetralogy of Fallot.
The patient underwent medical treatment with 100 mg orally (PO) day, clopidogrel 75 mg PO day and captopril 12.5 mg PO q 12 hours.
The patient will continue under medical follow-up and therapeutic behaviors will be regulated according to the evolution.
Within the current review in the literature, there are no similar case reports to this unusual presentation.
Right ventricular wall anomalies are rare[4]. They are divided into congenital (diverticulum) and acquired (aneurysm) secondary to trauma, iatrogenic aneurysm (due to surgical procedure) or secondary to myocarditis according to their etiology. The differential diagnosis should be made according to the history and image characteristics, especially by CMR.
In our case, the aneurysm was ruled out, with CMR being crucial since it demonstrated synchronous mobility of the lesion with respect to the wall of the right ventricle in a cine sequence, (the aneurysm would show asynchronous mobility or akinesia) in addition, the LGE images showed no evidence of reinforcement of the wall, ruling out infarction or fibrosis. In T2 weighted sequences, no wall edema or associated thrombus was found.
The echocardiogram, being operator-dependent and partially evaluating RV by position, may miss some defects, especially in patients with poor acoustic windows. The gold standard for characterization of RV wall defects by imaging is by CMR.
Due to the low incidence of this pathology, there is little information allowing the establishment of therapeutic strategies; in asymptomatic patients, as in our case, conservative management and close follow-up are recommended since no arrhythmias or thrombotic events occurred after the diverticulum was discovered; However, in some cases where there is a high risk of thrombosis (when the diverticulum is large or associated with arrhythmias or other malformations such as ventricular septal defect), anticoagulation is recommended. Surgery also is mainly reserved for cases of large and symptomatic diverticula[5].
Patients with corrected tetralogy of Fallot should be adequately monitored as they normally require surgical re-interventions, either due to residual obstruction of the RVOT or pulmonary regurgitation. Residual obstruction of the RVOT can lead to progressive concentric hypertrophy of the RV which implies a greater risk factor for the future development of ventricular tachycardia; In addition, if there is an association with a diverticulum (as in our case), monitoring and closer evaluation is important because of the additional risk of arrhythmia.
Between 40% to 85% of patients will develop pulmonary regurgitation in the medium and long term follow-up, at 5 or 10 years. This results in RV volume overload with progressive dilation that may be accompanied by tricuspid regurgitation and RV dysfunction. In these cases, pulmonary valve replacement is recommended as it allows us to reduce RV volumes, increase left ventricular ejection fraction and improve the patient’s functional status[6].
In our case report, paravalvular leakage was found through CMR after the placement of valve prosthesis (an incidence to this event is located between 2%-3%, usually due to the dehiscence of the valve with the native tissue)[7].
Although the association of diverticulum with tetralogy of Fallot has been reported, there seem to be no such cases after a placement of a pulmonary valve. In this case, the absence of it in the study prior to the prosthesis installation is probably due to masking of dilation of the right ventricle; characterization by CMR was crucial to be able to differentiate it from an aneurysm (which imply important differences in treatment).
Right ventricular diverticula are a rare entity, normally associated with tetralogy of Fallot or Cantrell’s pentalogy. To this date we could not find another case of a pulmonary valve placement, followed by a right ventricular diverticula formation.
| 1. | Iqbal S, Abidin N, Irwin RB, Schmitt M. A case report: multiple right ventricular diverticula with constrictive pericarditis and right heart failure. Eur Heart J Case Rep. 2019;3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 2. | Ojha V, Sharma A, Gulati G, Ramakrishnan S. True Right Ventricular Diverticulum in Tetralogy of Fallot: A Rare Association. Ann Thorac Surg. 2019;108:e345. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Losada Mora P, Valenzuela Vicente Mdel C, Ruiz CE. Diagnosis of ventricular diverticulum by cardiac computed tomography. Rev Esp Cardiol (Engl Ed). 2014;67:850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Magrassi P, Chartrand C, Guerin R, Kratz C, Stanley P. True diverticulum of the right ventricle: two cases associated with tetralogy of Fallot. Ann Thorac Surg. 1980;29:357-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Das D, Dutta N, Das AK, Sharma MK, Koley R, Chattopadhyay A, Ghosh S, Das S. Congenital right ventricular diverticulum: An atypical presentation. Ann Pediatr Cardiol. 2020;13:368-370. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 6. | van der Ven JPG, van den Bosch E, Bogers AJCC, Helbing WA. Current outcomes and treatment of tetralogy of Fallot. F1000Res. 2019;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 108] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 7. | Seery TJ, Slack MC. Percutaneous closure of a prosthetic pulmonary paravalvular leak. Congenit Heart Dis. 2014;9:E19-E22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/