Published online Dec 26, 2024. doi: 10.4330/wjc.v16.i12.683
Revised: October 1, 2024
Accepted: November 4, 2024
Published online: December 26, 2024
Processing time: 178 Days and 22.9 Hours
Comments were made on some thought-provoking articles, which included articles that dealt with cardiac arrest (CA). Two articles on CA elaborate on the role of automated compression devices to provide chest compressions during cardiopulmonary resuscitation (CPR) in “hostile” environments and on a predictive model in cases of out-of-hospital CA (OHCA). CPR after CA has been practiced for centuries, and the evolution until current modern-day practices are discussed. The delay in adopting efficient techniques of resuscitation by the medical community for decades is also touched upon. Both in-hospital and OHCA are discussed along with guidelines and strategies to improve outcomes. Areas of possible research in the future are mentioned.
Core Tip: Volume No. 15 of the World Journal of Cardiology for 2023 published 12 monthly issues. This editorial comments on some of the thought-provoking articles on cardiac arrest. The evolution and current status of cardiopulmonary resuscitation are discussed. Future directions which might improve survival are mentioned.
- Citation: Sunder T. Thoughts on recent articles on cardiopulmonary resuscitation. World J Cardiol 2024; 16(12): 683-688
- URL: https://www.wjgnet.com/1949-8462/full/v16/i12/683.htm
- DOI: https://dx.doi.org/10.4330/wjc.v16.i12.683
Cardiac arrest (CA) is one of the most demanding medical emergencies, requiring immediate action. Timely and appropriate treatment can be lifesaving. If the victim is fortunate due to the availability of people who are well trained in cardiopulmonary resuscitation (CPR) techniques, full recovery is possible with no neurological deficit. Widespread awareness of the urgency of this condition and techniques of basic life support among the lay public is needed. As CA can happen anywhere and to anyone, out-of-hospital CA (OHCA) is particularly challenging.
While commencement of adequate chest compressions are vital in maintaining circulation, delivery of electrical energy to defibrillate the heart during CPR is vital, especially in the first few minutes in achieving return of spontaneous circulation (ROSC). Governmental policies in many countries aimed at making automated external defibrillators (AEDs) available in public places with a view to assisting in OHCA is a welcome move.
Despite an increase in our understanding of the disease process over the last few decades, there have not been significant improvements in outcomes of CPR, especially in OHCA. The most critical aspect is the time frames involved. Time to starting CPR, time to delivery of first defibrillation, and adequate ventilation are important determinants of clinical outcomes. The degree of neurological recovery is thus an important aspect, which has a significant impact on the patient’s life.
This editorial commentary looks back at some of the articles published recently in the World Journal of Cardiology. Among these articles, which cover wide range of topics in cardiology, those on CAs are the subject of discussion in this editorial.
Two articles on CA were published recently in World Journal of Cardiology. In one article, Latsios et al[1] discuss use of automatic compression device to protect rescuers in “hostile” environments, while Wang et al[2] discuss OHCAs.
CA refers to the complete cessation of any effective cardiac contraction with no circulation, and will lead to death if not resuscitated immediately. Attempts to revive patients have been described in the 16th century. Andreas Vesalius, at the age of 28, described resuscitation in 1543 and is regarded as father of resuscitation[3].
Different components of CPR were discovered, and strategies developed at different times over the last few centuries. Unfortunately, these notable findings were not recognized and were not put to good clinical use for decades since their discovery.
Artificial respiration progressed with the development of positive pressure ventilation in the 18th and 19th centuries. Sternal compressions were described by John Hill in 1868, but it is unclear whether the intent was to ventilate the lungs or compress the heart[4]. Although external cardiac massage had been discovered, work by Moritz Schiff encouraged use of internal cardiac massage for resuscitation. Internal cardiac massage was first described in 1901 by Keene for CA after an abdominal operation and by 1952, a successful revival was achieved in 33% of cases[4]. The landmark publication in 1960 by Kouwenhoven et al[5] on closed-chest cardiac massage ushered in the era of modern CPR. They reported a series of 20 patients who were all, quite remarkably, revived and reported to be well 14 months later. This led to the abandoning of internal cardiac massage. Defibrillation of the heart was reported on experiments carried out in 1899 and was not clinically achieved in humans until 50 years later. In 1964, the airway, breathing, and circulation of CPR was published by Safar[6]. The first CPR guidelines was published by an ad hoc Committee on CPR by National Academy of Sciences in 1966[7]. The most recent guidelines is the 2023 focused update of the American Heart Association on Advanced cardiac life support and CPR[8] and provides “recommendations on the use of medications, temperature management, percutaneous coronary angiography, extracorporeal CPR, and seizure management.”
As elaborated above, the inordinate delay by the medical community in adoption of effective resuscitation processes has to be noted so that it is not repeated. In his publication, based on the Fitzpatrick lecture that he delivered to the Royal College of Physicians, Chamberlain[3] discusses the discoveries and anguishes on the lamentable delay by the medical community in adopting useful treatments. Regarding the delay in clinical acceptance and practical adoption of these discoveries related to CPR, he quotes “So often our predecessors ‘did not learn’ when it seems in retrospect that they should have done, and so often they were ‘never quite there’ for developments that then had to wait many years. We share the same frailties and are no doubt guilty of the same sorts of errors. History will be our judge too.”
The International Liaison Committee on Resuscitation (ILCOR) was founded in 1992 with a panel of international experts[9]. The committee provides an International Consensus on CPR and Emergency Cardiac Care Science with Treatment Recommendations (CoSTR). Initially, the ILCOR guidelines with CoSTR were published once every 5 years; the last 5-year update was published in 2015. To avoid delay in adopting reliable new techniques, as aspired by Chamberlain[3], the ILCOR initiated a process from 2016 looking at continuous review and update of the science of resuscitation. Subsequently, annual ILCOR CoSTR statements are being published, the most recent of which is the 2023 ILCOR Summary Statement[10].
While the ILCOR scrutinizes the evidence and aims to provide the best possible recommendation, given the clinical scenario, it is readily apparent that the clinical reports when graded for quality are most often low quality evidence, which are subject to bias and other variables leading to weak recommendations. Data from OHCAs are more challenging to use due to the heterogenous and varying levels of expertise of bystanders until trained paramedics arrive.
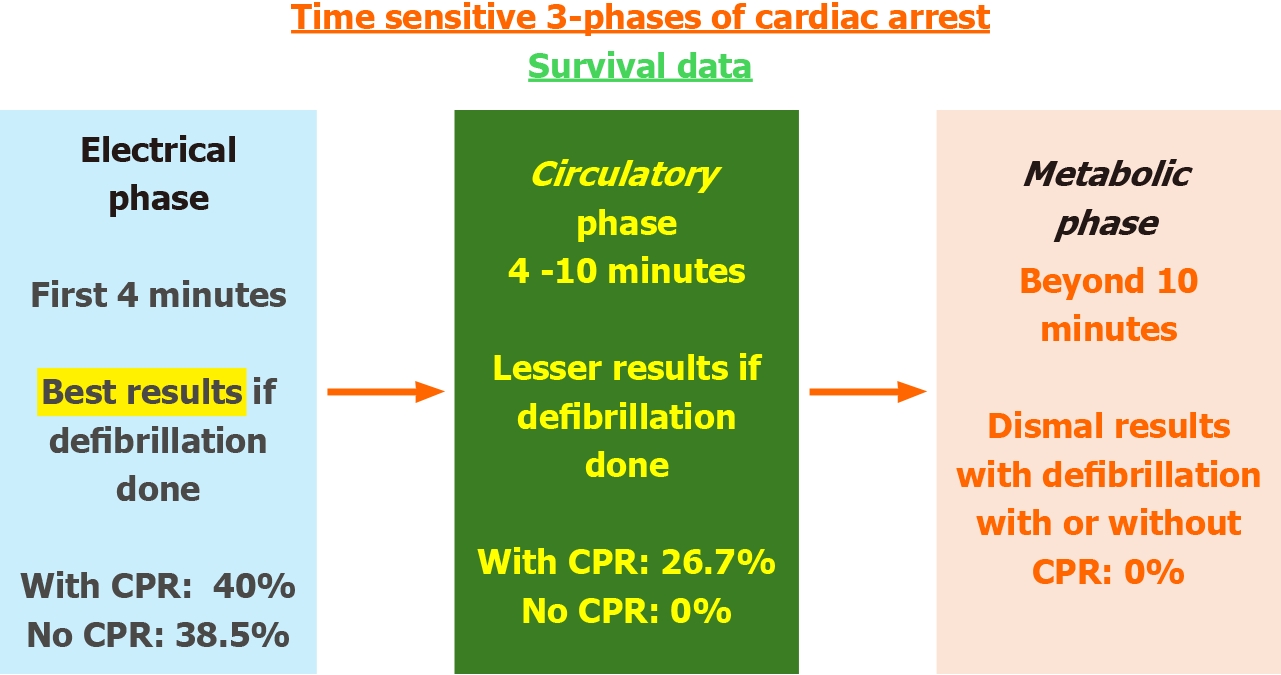
In 2002 Weisfeldt and Becker[11], who felt that the pathophysiology of ischemia and reperfusion is a function of time, described three time-sensitive phases after CA: The electrical phase (up to 4 minutes after ventricular fibrillation arrest), the circulatory phase (up to 10 minutes after arrest) and the metabolic phase (after 10 minutes commencing after the circulatory phase). These time-sensitive phases underscore the importance of achieving, whenever possible, an early ROSC. Figure 1 summarizes the three phases of CA and survival in each of these phases using defibrillation with or without CPR as described by Vilke et al[12].
In a successfully revived patient, the complex pathophysiological effects of ischemia and reperfusion in all organs of the body were described by Negovsky[13], who coined the term “post resuscitation syndrome.” This was then referred to as post CA syndrome (PCAS) by ILCOR[14] in their guidelines published in 2008. PCAS includes brain injury, myocardial dysfunction, and systemic effects of ischemia and reperfusion.
Approximately 424000 and 27500 OHCA occur annually in the United States and Europe respectively, of whom 1 in 12 (8.3%) victims survive to return home[15]. In China, the annual OHCA is approximately 550000 with 1.3% survival[2]. Among victims of OHCA, prehospital ROSC is vital and has better neurological outcomes. The global survival of OHCA at 1 year after discharge is 7.75%.
AEDs allow immediate defibrillation by untrained bystanders. Recommendations suggest placement and availability in public places where there is a high likelihood of OHCA. Public access AEDs are now increasingly available. Underutilization of public AEDs is common[16]. Challenges in the use of AEDs by the public and possibilities to increase them are discussed in the review article by Ringh et al[17].
It has been long recognized that automated compression devices (ACDs) can be put to meaningful use during CPR. They are two types: The piston driven type and the load distribution band type. They can provide high-quality compression in terms of nonstop regular frequency, depth and prolonged periods of compression, while eliminating back injury to the rescuers during CPR[18] and eliminating rescuer fatigue. ACD frees the hands, and the rescuer can devote their attention to other vital processes.
In the recent issue of World Journal of Cardiology, Latsios et al[1] published an interesting article titled “Cardiac arrest and cardiopulmonary resuscitation in "hostile" environments: Using automated compression devices to minimize the rescuers' danger.” The authors discussed an important and often overlooked aspect of emergency treatment, namely, the risks to the rescuer. Similar to the risks confronted by the rescue teams for natural calamities or major accidents, the risks to the healthcare worker delivering CPR can be significant. The authors describe the types of ACDs available and discuss the advantages and disadvantages of both types of ACDs. ACDs are not without risks to the patient. Trauma due to ACDs can result in rib fracture and improperly placed devices can cause trauma to liver and other organs. Therefore, the use of ACDs come with a “learning curve.” This can be offset by offering structured training sessions to the emergency team. Effective cardiac compressions are the key to successful resuscitation. Physical fatigue of the rescuers, especially in locations that may be hazardous to the rescuer, can result in suboptimal chest compressions and inferior outcomes. Both in-hospital CA and OHCA are considered. The “hostile” in-hospital locations include cardiac catheterization laboratory with its inherent radiation hazards and the intensive care unit/ward setting in patients with coronavirus disease 19. CAs in the emergency room (ER) are considered to be OHCAs, since most of them are brought to ER with ongoing CPR. The main limitations of the ACDs have been delay in the time to first defibrillation and time to deployment (deployment pause). Transport of a victim of CA with ongoing CPR is perhaps most challenging. Except for the time taken to deploy, the use of any type ACD is beneficial in terms of ROSC and survival[19]. The authors have elaborately considered the available evidence on ACDs[15,20,21]. Many randomized controlled trials and individual studies have compared manual chest compressions with ACDs. The results of these studies are often mixed and conflicting. Notwithstanding the above, it is noteworthy that the use of ACDs was recommended in the 2021 guidelines of European Resuscitation Council in special circumstances such during percutaneous intervention[22,23] or coronavirus disease[23]. The authors also touched upon an important aspect, namely the use of ACDs as a bridge to organ donation, and nicely pointed out that a reduction in “warm ischemia time” is possible with ACDs in appropriate circumstances. The authors, while reiterating that there is no evidence to support or refute the “routine” use of ACDs in CA, do make a convincing argument to consider ACDs in a “hostile” environment, ensuring both superior outcomes and rescuer safety.
In the recent issue of World Journal of Cardiology, Wang et al[2] published an interesting article titled “Establishment of a prediction model for prehospital return of spontaneous circulation in out-of-hospital patients with cardiac arrest.” The authors conducted this remarkable study on an important condition that has major public health implications. It has been demonstrated that patients with prehospital ROSC have better outcomes, and the authors set out to describe a predictive model for the same. This was a multicenter retrospective study involving 2685 patients across 150 hospitals from January 2012 to December 2019. The incidence of prehospital ROSC was 5.8%. The authors looked at factors prior to the arrival of an emergency team for OHCA. They identified six factors, namely, age, bystander CPR, initial rhythm, CPR duration, ventilation mode, and etiology, using least absolute shrinkage and selection operator regression and multivariate logistic regression. Each factor was assigned a numerical score, and the total of the score was predictive of the probability of ROSC (P-ROSC). A nomogram prediction model was established based on these influencing factors. The area under the receiver operating curve was 0.963. Decision curve analysis confirmed good clinical usability. The authors quite rightly conclude that this model could effective predict P-ROSC in victims of OHCA and will be a valuable tool to aid clinical decision making.
While the science behind resuscitation has been understood to a large degree, it is the prompt delivery of the knowledge amassed to the victim of CA that poses a major problem. Steps to tackle this “bottleneck” of prompt and universal delivery of adequate CPR should be the way forward to improve the current dismal outlook, especially in cases of OHCA.
An animal-based pilot study looking at “automated CPR,” which combines automatic defibrillation and chest compression at the same time, has been published and appears promising[24]. The authors have demonstrated the feasibility of combining ACD and AED and used this “automated CPR” device in five pigs. These were compared to conventional CPR in six pigs. The authors demonstrated significant reductions in time to charge, time to defibrillate, and time to resume chest compressions in the “automated CPR” group. If superior outcomes with survival advantage can be demonstrated, this “automated CPR” would be value addition in selected cases.
Decades of experience tell that the single most important factor is the time to first intervention, namely defibrillation and chest compression, which have the most significant impact on achieving full recovery. Widespread community awareness programs about basic life support can improve the results and outcomes of CPR provided by “bystanders.” Usage of AEDs, despite availability, is reportedly low, and this single point reiterates the need for more aggressive awareness programs. With the availability of social media platforms, dissemination of such knowledge is entirely feasible. The emphasis of awareness programs should be on timeliness and prompt action without which a lot of the effort expended in performing CPR can become futile.
Looking back historically, it is rather sobering that the medical community took its time in adopting efficient resuscitation techniques. Nonetheless, it is indeed gratifying to note the near-continuous review of available evidence on resuscitation by ILCOR with its worldwide representation. Humanity will only be best served if all units are kept updated of the latest guidelines.
To summarize, the need for timely intervention cannot be over emphasized and is worthy of reiteration. Universal availability of AEDs and emergency teams that would provide prompt assistance, while ideal, is not possible in the real world. The healthcare infrastructure varies between countries and within states in the same country.
To improve the outcomes of this dismal condition, the CA situation can be viewed from perspectives of the victim and the health care provider. From the victim’s aspect, carrying a health card is often beneficial to oneself and helps health care provider.
From the healthcare provider aspects, availability of equipment to deliver is vital. Emergency teams are often well equipped in terms of training and equipment but are not available within minutes of CA.
In cases of OHCA, it is often the bystanders who are the first to respond and it is the bystanders who need to be trained and knowledgeable. Bystanders are the people who must be “targeted” to provide basic life support for these unfortunate victims of CA. Bystander providers of CPR have increased recently, and the emphasis should be in equipping the bystanders with knowledge and training so that basic life support can be provided.
P-ROSC and timely intervention is achievable only if the bystander contribution increases. It is impractical to assume that emergency teams will always arrive within minutes.
Despite advances in healthcare, OHCA is still an important cause of death. Survival is directly related to the quality and adequacy of the initial rescue therapy offered. High quality CPR with early defibrillation plays a vital role. Increasing public awareness and education about CPR, provision of robust emergency services, ensuring appropriate use of available of AEDs in public places will improve outcomes in this group of patients.
| 1. | Latsios G, Leopoulou M, Synetos A, Karanasos A, Papanikolaou A, Bounas P, Stamatopoulou E, Toutouzas K, Tsioufis K. Cardiac arrest and cardiopulmonary resuscitation in "hostile" environments: Using automated compression devices to minimize the rescuers' danger. World J Cardiol. 2023;15:45-55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (1)] |
| 2. | Wang JJ, Zhou Q, Huang ZH, Han Y, Qin CZ, Chen ZQ, Xiao XY, Deng Z. Establishment of a prediction model for prehospital return of spontaneous circulation in out-of-hospital patients with cardiac arrest. World J Cardiol. 2023;15:508-517. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 3. | Chamberlain D. Never quite there: a tale of resuscitation medicine. Clin Med (Lond). 2003;3:573-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Hurt R. Modern cardiopulmonary resuscitation--not so new after all. J R Soc Med. 2005;98:327-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Kouwenhoven WB, Jude JR, Knickerbocker GG. Closed-chest cardiac massage. JAMA. 1960;173:1064-1067. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1417] [Cited by in RCA: 1235] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 6. | Safar P. Community-wide cardiopulmonary resuscitation. J Iowa Med Soc. 1964;54:629-635. [PubMed] |
| 7. | Cardiopulmonary resuscitation. JAMA. 1966;198:372-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 95] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Perman SM, Elmer J, Maciel CB, Uzendu A, May T, Mumma BE, Bartos JA, Rodriguez AJ, Kurz MC, Panchal AR, Rittenberger JC; American Heart Association. 2023 American Heart Association Focused Update on Adult Advanced Cardiovascular Life Support: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2024;149:e254-e273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 139] [Article Influence: 69.5] [Reference Citation Analysis (0)] |
| 9. | Hazinski MF, Nolan JP. International Collaboration With Dedicated Local Implementation Improves Survival From Out-of-Hospital Cardiac Arrest. J Am Heart Assoc. 2017;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Berg KM, Bray JE, Ng KC, Liley HG, Greif R, Carlson JN, Morley PT, Drennan IR, Smyth M, Scholefield BR, Weiner GM, Cheng A, Djärv T, Abelairas-Gómez C, Acworth J, Andersen LW, Atkins DL, Berry DC, Bhanji F, Bierens J, Bittencourt Couto T, Borra V, Böttiger BW, Bradley RN, Breckwoldt J, Cassan P, Chang WT, Charlton NP, Chung SP, Considine J, Costa-Nobre DT, Couper K, Dainty KN, Dassanayake V, Davis PG, Dawson JA, Fernanda de Almeida M, De Caen AR, Deakin CD, Dicker B, Douma MJ, Eastwood K, El-Naggar W, Fabres JG, Fawke J, Fijacko N, Finn JC, Flores GE, Foglia EE, Folke F, Gilfoyle E, Goolsby CA, Granfeldt A, Guerguerian AM, Guinsburg R, Hatanaka T, Hirsch KG, Holmberg MJ, Hosono S, Hsieh MJ, Hsu CH, Ikeyama T, Isayama T, Johnson NJ, Kapadia VS, Daripa Kawakami M, Kim HS, Kleinman ME, Kloeck DA, Kudenchuk P, Kule A, Kurosawa H, Lagina AT, Lauridsen KG, Lavonas EJ, Lee HC, Lin Y, Lockey AS, Macneil F, Maconochie IK, John Madar R, Malta Hansen C, Masterson S, Matsuyama T, McKinlay CJD, Meyran D, Monnelly V, Nadkarni V, Nakwa FL, Nation KJ, Nehme Z, Nemeth M, Neumar RW, Nicholson T, Nikolaou N, Nishiyama C, Norii T, Nuthall GA, Ohshimo S, Olasveengen TM, Gene Ong YK, Orkin AM, Parr MJ, Patocka C, Perkins GD, Perlman JM, Rabi Y, Raitt J, Ramachandran S, Ramaswamy VV, Raymond TT, Reis AG, Reynolds JC, Ristagno G, Rodriguez-Nunez A, Roehr CC, Rüdiger M, Sakamoto T, Sandroni C, Sawyer TL, Schexnayder SM, Schmölzer GM, Schnaubelt S, Semeraro F, Singletary EM, Skrifvars MB, Smith CM, Soar J, Stassen W, Sugiura T, Tijssen JA, Topjian AA, Trevisanuto D, Vaillancourt C, Wyckoff MH, Wyllie JP, Yang CW, Yeung J, Zelop CM, Zideman DA, Nolan JP, ;; and Collaborators. 2023 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations: Summary From the Basic Life Support; Advanced Life Support; Pediatric Life Support; Neonatal Life Support; Education, Implementation, and Teams; and First Aid Task Forces. Resuscitation. 2024;195:109992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 61] [Article Influence: 30.5] [Reference Citation Analysis (0)] |
| 11. | Weisfeldt ML, Becker LB. Resuscitation after cardiac arrest: a 3-phase time-sensitive model. JAMA. 2002;288:3035-3038. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 430] [Cited by in RCA: 455] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 12. | Vilke GM, Chan TC, Dunford JV, Metz M, Ochs G, Smith A, Fisher R, Poste JC, McCallum-Brown L, Davis DP. The three-phase model of cardiac arrest as applied to ventricular fibrillation in a large, urban emergency medical services system. Resuscitation. 2005;64:341-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 1.5] [Reference Citation Analysis (1)] |
| 13. | Negovsky VA. The second step in resuscitation--the treatment of the 'post-resuscitation disease'. Resuscitation. 1972;1:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 105] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Neumar RW, Nolan JP, Adrie C, Aibiki M, Berg RA, Böttiger BW, Callaway C, Clark RS, Geocadin RG, Jauch EC, Kern KB, Laurent I, Longstreth WT Jr, Merchant RM, Morley P, Morrison LJ, Nadkarni V, Peberdy MA, Rivers EP, Rodriguez-Nunez A, Sellke FW, Spaulding C, Sunde K, Vanden Hoek T. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A consensus statement from the International Liaison Committee on Resuscitation (American Heart Association, Australian and New Zealand Council on Resuscitation, European Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Asia, and the Resuscitation Council of Southern Africa); the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; and the Stroke Council. Circulation. 2008;118:2452-2483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1061] [Cited by in RCA: 1152] [Article Influence: 64.0] [Reference Citation Analysis (0)] |
| 15. | Perkins GD, Lall R, Quinn T, Deakin CD, Cooke MW, Horton J, Lamb SE, Slowther AM, Woollard M, Carson A, Smyth M, Whitfield R, Williams A, Pocock H, Black JJ, Wright J, Han K, Gates S; PARAMEDIC trial collaborators. Mechanical versus manual chest compression for out-of-hospital cardiac arrest (PARAMEDIC): a pragmatic, cluster randomised controlled trial. Lancet. 2015;385:947-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 350] [Article Influence: 31.8] [Reference Citation Analysis (0)] |
| 16. | Deakin CD, Anfield S, Hodgetts GA. Underutilisation of public access defibrillation is related to retrieval distance and time-dependent availability. Heart. 2018;104:1339-1343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 47] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 17. | Ringh M, Hollenberg J, Palsgaard-Moeller T, Svensson L, Rosenqvist M, Lippert FK, Wissenberg M, Malta Hansen C, Claesson A, Viereck S, Zijlstra JA, Koster RW, Herlitz J, Blom MT, Kramer-Johansen J, Tan HL, Beesems SG, Hulleman M, Olasveengen TM, Folke F; COSTA study group (research collaboration between Copenhagen, Oslo, STockholm, and Amsterdam). The challenges and possibilities of public access defibrillation. J Intern Med. 2018;283:238-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 61] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 18. | Jones AY. Can cardiopulmonary resuscitation injure the back? Resuscitation. 2004;61:63-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Ong ME, Mackey KE, Zhang ZC, Tanaka H, Ma MH, Swor R, Shin SD. Mechanical CPR devices compared to manual CPR during out-of-hospital cardiac arrest and ambulance transport: a systematic review. Scand J Trauma Resusc Emerg Med. 2012;20:39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 57] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 20. | Couper K, Quinn T, Booth K, Lall R, Devrell A, Orriss B, Regan S, Yeung J, Perkins GD. Mechanical versus manual chest compressions in the treatment of in-hospital cardiac arrest patients in a non-shockable rhythm: A multi-centre feasibility randomised controlled trial (COMPRESS-RCT). Resuscitation. 2021;158:228-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 21. | Kłosiewicz T, Puślecki M, Zalewski R, Sip M, Perek B. Impact of automatic chest compression devices in out-of-hospital cardiac arrest. J Thorac Dis. 2020;12:2220-2227. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Lott C, Truhlář A, Alfonzo A, Barelli A, González-Salvado V, Hinkelbein J, Nolan JP, Paal P, Perkins GD, Thies KC, Yeung J, Zideman DA, Soar J; ERC Special Circumstances Writing Group Collaborators. Corrigendum to "European Resuscitation Council Guidelines 2021: Cardiac arrest in special circumstances" [Resuscitation 161 (2021) 152-219]. Resuscitation. 2021;167:91-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 23. | Soar J, Böttiger BW, Carli P, Couper K, Deakin CD, Djärv T, Lott C, Olasveengen T, Paal P, Pellis T, Perkins GD, Sandroni C, Nolan JP. Corrigendum to "European Resuscitation Council Guidelines 2021: Adult Advanced Life Support" [Resuscitation 161 (2021) 115-151]. Resuscitation. 2021;167:105-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 24. | Roh YI, Jung WJ, Im HY, Lee Y, Im D, Cha KC, Hwang SO. Development of an automatic device performing chest compression and external defibrillation: An animal-based pilot study. PLoS One. 2023;18:e0288688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/