Published online Nov 26, 2024. doi: 10.4330/wjc.v16.i11.644
Revised: August 24, 2024
Accepted: September 6, 2024
Published online: November 26, 2024
Processing time: 199 Days and 1.4 Hours
Permanent pacemaker implantation has the potential to impact left ventricular (LV) function and hence quality of life (QoL) in the long term.
To assess the effect of single- and dual-chamber pacing on LV function and QoL.
This study included 56 patients who underwent permanent pacing: Dual pacing, dual sensing, dual responsive and rate responsive (DDDR) for the initial 3 months and ventricular pacing, ventricular sensing, inhibited response and rate responsive (VVIR) for the next 3 months, and DDDR mode for the last 3 months. Throughout the study period, various echocardiographic parameters, functional status, and QoL were measured to assess the impact of pacing on LV function compared with baseline and at every 3 months interval.
A significant change appeared in cardiac function after VVIR pacing which included diastolic properties of LV as shown by increase in isovolumic relaxation time from (85.28 ± 9.54 ms) to (89.53 ± 9.65 ms). At the 3-, 6-, and 9-month follow-up, reduction in LV ejection fraction was observed to be 62.71 ± 4.66%, 61.07 ± 4.41%, and 58.48 ± 3.89%, respectively. An increase in the QoL scores was noted at every follow-up visit.
An apparent depressant effect on LV function due to right ventricular pacing, with a higher incidence of adverse outcomes in the VVIR mode. In addition, an upsurge in QoL scores for the study population was noted, which indicates improvement in the QoL of patients post-pacing, irrespective of the mode. Generally, the DDDR mode is a highly preferable pacing mode.
Core Tip: Pacemaker implantation is a common treatment for cardiac conduction disorders, but the impact of right ventricular pacing (RVP) on left ventricular (LV) function remains a concern. Limited information is available on the acute and early effects of RVP on LV function, particularly when comparing dual pacing, dual sensing, dual responsive and rate responsive (DDDR) with ventricular pacing, ventricular sensing, inhibited response and rate responsive (VVIR) pacemakers. This study found that RVP adversely affects LV function, with more significant impairment observed in VVIR mode compared to DDDR mode. However, both modes led to improvements in quality of life (QoL). The findings support the use of DDDR mode over VVIR mode for better clinical outcomes and preservation of LV function, while also improving QoL.
- Citation: Haque M, Bhandari M, Pradhan A, Vishwakarma P, Singh A, Shukla A, Sharma A, Chaudhary G, Sethi R, Chandra S, Jaiswal A, Dwivedi SK. Impact of single chamber and dual chamber permanent pacemaker implantation on left ventricular function: An observational study. World J Cardiol 2024; 16(11): 644-650
- URL: https://www.wjgnet.com/1949-8462/full/v16/i11/644.htm
- DOI: https://dx.doi.org/10.4330/wjc.v16.i11.644
Defects in cardiac impulse generation and conduction occur at various levels in the cardiac conduction system, starting from the sinus node to the Purkinje fibres which depolarize the ventricles. When this intrinsic cardiac automaticity or conduction integrity fails, an external stimulus is required to drive the myocytes to the threshold through excitation-contraction coupling, and pacemakers provide that external stimulus[1]. Implantation of pacemakers is an effective treatment option, especially for patients with sick sinus syndrome (SSS) and atrioventricular (AV) conduction disorders[2]. The types of implants include single-chamber [single-atrial chamber pacemakers atrial pacing, atrial sensing and inhibited response (AAI), and single-ventricular chamber pacemakers ventricular pacing, ventricular sensing, inhibited response and rate responsive (VVIR) and double-chamber chamber pacemakers dual pacing, dual sensing, dual responsive and dual pacing, dual sensing, dual responsive and rate responsive (DDDR)[3].
AAI are indicated in selected patients in whom only sinus node dysfunction is present and AV node conduction is preserved, whereas VVI, VVIR, and double-chamber pacemakers are indicated in patients with AV block and complete heart blocks[3]. During the implantation of permanent pacemaker devices, the endocardial right ventricular pacing (RVP) lead is often positioned at the right ventricular (RV) apex[2]. It is well known that RVP alters normal signal conduction and may result in a reduction in the left ventricular ejection fraction (LVEF). Therefore, it is paramount to measure left ventricular (LV) function, especially during RVP[4]. Deterioration of LV function can be measured using 2D echocardiography and strain imaging techniques after dual- and single-chamber pacemaker implantation[5,6]. Quality of life (QoL) is a scientific outcome measurement strategy that evaluates treatment effectiveness and is widely assessed using the SF-36 score[6]. In addition, previous studies have shown that permanent pacemaker implantation leads to improvement in symptoms and QoL[7].
The long-term effects of right ventricular apical pacing have been previously studied; however, little information is available on the acute and early effects of RVP on LV function. Hence, this study aimed to evaluate the impact of RVP on LV function by comparing LV function impairment in dual- and single-chamber pacemakers, along with its impact on QoL.
The study population included patients admitted for pacemaker implantation at a tertiary healthcare centre in India. Participating patients were those of all ages and of both sexes who were willing to provide consent and were undergoing permanent pacemaker implantation. Patients with preexisting LV systolic dysfunction were excluded.
This single-centre, hospital-based, prospective, observational study was conducted over a period of 9 months, during which a total of 56 patients were enrolled. Detailed demographic characteristics and baseline LV function parameters were recorded upon admission. The study population was initially kept in the DDDR mode for 3 months, post which the mode was changed to VVIR for the next 3 months, followed again by the DDDR mode. Thus, we had a cross-over study design. The pacemaker programming was conducted by the same person. After pacemaker implantation, echocardiographic parameters such as the LV size, LVEF, LV diastolic function, and LV strain were measured using Vivid E-95 4D cardiac ultrasound system (GE Health Care Technologies Inc, Chicago Illinois, United States). Echocardiography was performed by the same person on follow-up-for-changes in LV function. Echocardiographic imaging was repeated every 3 months to measure the impact of the pacemaker on LV function. In addition, the functional status of all patients was measured using the treadmill test, and they were categorised into the New York Heart Association (NYHA) functional class based on the observed symptoms, which were repeated at intervals of 3 months.
The QoL of the enrolled participants was assessed using the SF-36 questionnaire, which covers eight health domains: Physical functioning (10 items), bodily pain (2 items), role limitations due to physical health problems (4 items), role limitations due to personal or emotional problems (4 items), emotional well-being (5 items), social functioning (2 items), energy/fatigue (4 items), and general health perceptions (5 items). The scores for each domain ranged from 0 to 100, with higher scores indicating a more favourable health state. The patients received medications for comorbidities, such as hypertension, diabetes, or dyslipidaemia, as per the standard guidelines. Patients with LV dysfunction were prescribed heart failure therapy according to the guidelines.
All data were analysed using SPSS software (Version 16). Categorical variables are presented as frequencies and per
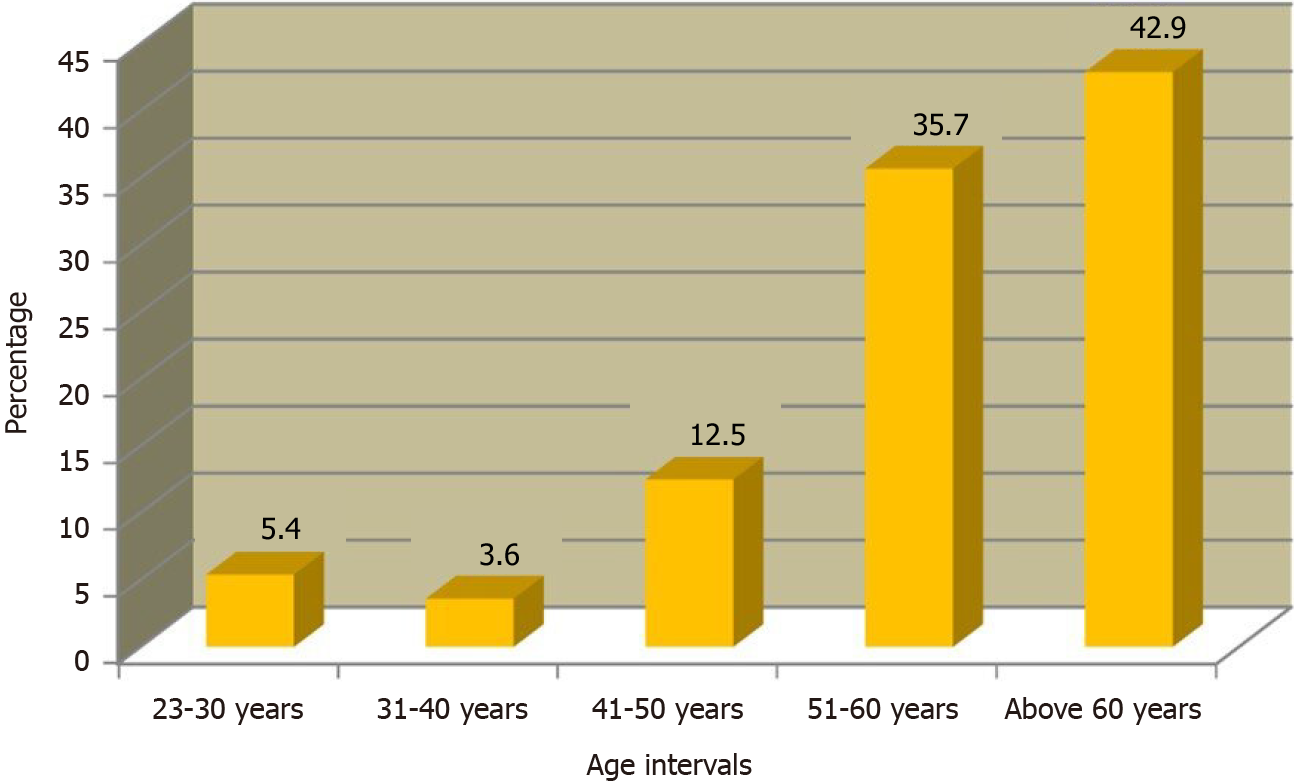
This study comprised 56 patients, among whom 73.2% were male. The mean age observed for the study population was 57.11 ± 11.87 years, and the majority of patients (42.9%) belonged to the age group above 60 years (Figure 1). The indication for pacemaker implantation in all patients was complete heart block. None of the patients had sinus node dysfunction. The atrial lead was a tined lead placed in the right atrial appendage, and the RV endocardial lead was placed at the apex. The post-ventricular atrial refractory period (PVARP) was programmed in the automatic mode (autonomous PVARP, approximately 250 ms) to enhance protection against pacemaker-induced tachycardia.
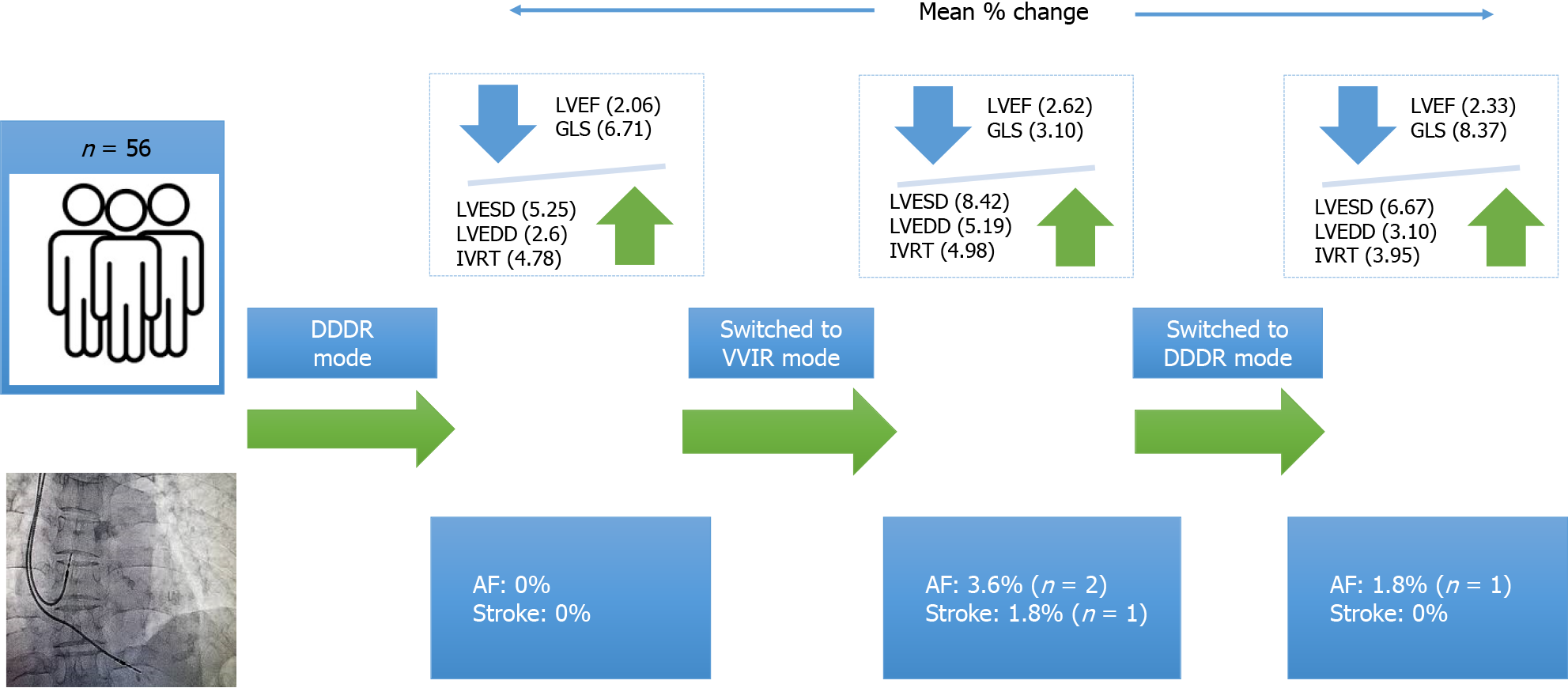
Various echocardiographic parameters, physical tests, and QoL domains were assessed at baseline and at 3, 6, and 9 months. Measurements of several systolic and diastolic parameters revealed significant differences at various follow-ups (P < 0.05). The LVEF, measured using the Simpson method, showed that the mean baseline LVEF was 64.03 ± 5.36%, which decreased to 62.71 ± 4.66% after 3 months, indicating a mean change of 2.06%. At the 6-month follow-up, the mean LVEF was 61.07 ± 4.41%, and at the 9-month follow-up, a further decrease of 2.33% was observed. The mean LV end-diastolic diameter (LVEDD), a key parameter for assessing ventricular performance, increased at each follow-up. Specifically, LVEDD increased by 2.60% at 3 months, by 5.19% at 6 months, and by 3.10% at 9 months. A reduction in stroke volume was noted, with a 5.15% decrease at 6 months and a more pronounced 7.59% decrease at 9 months. Global longitudinal strain, an echocardiographic parameter used to detect LV systolic dysfunction, declined by 6.71%, 16.21%, and 8.37% at the 3-, 6-, and 9-month follow-ups, respectively. The mean value of LV end-systolic dimension (LVESD) was 23.96 ± 1.46 mm at 3 months, which increased to 25.98 ± 1.30 mm at 6 months. Isovolumic relaxation time (IVRT), which measures diastolic function, increased at every follow-up. At 3 months, the mean IVRT was 85.27 ± 9.54 ms, rising to 93.07 ± 10.38 ms at 9 months. The QoL scores improved at every follow-up, with a mean score of 74.41 ± 12.83 at 3 months, 82.05 ± 7.46 at 6 months, and 90.44 ± 5.89 at 9 months. The mean values of other measured parameters and their statistical values are summarised in Table 1. According to the NYHA classification, a large proportion of patients (92.85%) had class 1 heart failure at baseline, whereas at the 9-month follow-up, a greater number of patients (58.9%) had progressed to class 2 heart failure. These findings were statistically significant (P < 0.05). Further details are provided in Table 2. Outcomes such as atrial fibrillation (AF) and stroke were lower in the dual-chamber mode than in the single-chamber mode. None of the patients had AF or flutter at baseline. However, at 6 months, two patients developed transient AF, which reverted to sinus rhythm in one patient at 9 months. Further details are presented in Table 3.
| Variable | Parameter | Baseline | 3 months | 3 months | 6 months | 6 months | 9 months | P value |
| LVEF (M Mode) (%) | mean ± SD | 63.69 ± 5.19 | 62.51 ± 4.76 | 62.51 ± 4.76 | 61.14 ± 4.71 | 61.14 ± 4.71 | 58.58 ± 4.24 | < 0.001 |
| % Mean change | 1.85 | 2.20 | 1.80 | |||||
| LVEF (Simpson) (%) | mean ± SD | 64.03 ± 5.36 | 62.71 ± 4.66 | 62.71 ± 4.66 | 61.07 ± 4.41 | 61.07 ± 4.41 | 58.48 ± 3.89 | |
| % Mean change | 2.06 | 2.62 | 2.33 | |||||
| LVEDD (MM) | mean ± SD | 40.57 ± 4.07 | 41.01 ± 3.55 | 41.01 ± 3.55 | 43.78 ± 3.04 | 43.78 ± 3.04 | 45.14 ± 3.07 | |
| % Mean change | -2.60 | -5.19 | -3.10 | |||||
| LVESD (MM) | mean ± SD | 22.76 ± 2.40 | 23.96 ± 1.46 | 23.96 ± 1.46 | 25.98 ± 1.30 | 25.98 ± 1.30 | 27.71 ± 1.56 | |
| % Mean change | -5.25 | -8.42 | -6.67 | |||||
| SV (ML) | mean ± SD | 84.96 ± 20.38 | 80.41 ± 17.89 | 80.41 ± 17.89 | 76.26 ± 16.44 | 76.26 ± 16.44 | 70.48 ± 11.30 | |
| % Mean change | 5.36 | 5.15 | 7.59 | |||||
| E/A | mean ± SD | 1.08 ± 0.191 | 1.18 ± 0.15 | 1.18 ± 0.15 | 1.36 ± 0.18 | 1.36 ± 0.18 | 1.50 ± 0.166 | |
| % Mean change | -8.86 | -14.93 | -10.63 | |||||
| E/E’ | mean ± SD | 9.05 ± 2.41 | 9.82 ± 2.52 | 9.82 ± 2.52 | 10.79 ± 3.03 | 10.79 ± 3.03 | 11.59 ± 3.60 | |
| % Mean change | -8.48 | -9.83 | -7.48 | |||||
| IVRT (MS) | mean ± SD | 81.39 ± 9.45 | 85.25 ± 9.54 | 85.25 ± 9.54 | 89.53 ± 9.54 | 89.53 ± 9.54 | 93.07 ± 10.38 | |
| % Mean change | -4.78 | -4.98 | -3.95 | |||||
| DT (SEC) | mean ± SD | 187.79 ± 32.58 | 194.84 ± 31.20 | 194.84 ± 31.20 | 204.79 ± 31.04 | 204.79 ± 31.04 | 214.46 ± 31.01 | |
| % Mean change | -3.75 | -5.11 | -4.72 | |||||
| TR (M/S) | mean ± SD | 1.50 ± 0.53 | 1.73 ± 0.43 | 1.73 ± 0.43 | 1.99 ± 0.43 | 1.99 ± 0.43 | 2.26 ± 0.46 | |
| % Mean change | -15.03 | -15.02 | -13.60 | |||||
| PASP (MM/HG) | mean ± SD | 17.47 ± 5.89 | 20.59 ± 6.90 | 20.59 ± 6.90 | 23.35 ± 7.83 | 23.35 ± 7.83 | 26.66 ± 9.96 | |
| % Mean change | -17.87 | -13.41 | -14.16 | |||||
| GLS (%) | mean ± SD | -17.95 ± 2.95 | -16.74 ± 2.86 | -16.74 ± 2.86 | -14.03 ± 2.34 | -14.03 ± 2.34 | -12.85 ± 1.95 | |
| % Mean change | 6.71 | 16.21 | 8.37 | |||||
| TMT (METS) | mean ± SD | 13.37 ± 3.23 | 11.83 ± 3.08 | 11.83 ± 3.08 | 9.75 ± 2.69 | 9.75 ± 2.69 | 8.58 ± 2.30 | |
| % Mean change | 11.48 | 17.65 | 11.90 | |||||
| QoL | mean ± SD | 69.83 ± 12.29 | 74.41 ± 12.83 | 74.41 ± 12.83 | 82.05 ± 7.46 | 82.05 ± 7.46 | 90.44 ± 5.89 | |
| % Mean change | -6.55 | -10.27 | -10.23 | |||||
| NYHA | Baseline | 3 months | 6 months | 9 months |
| Class 1 | 52 (92.85) | 45 (80.40) | 14 (25.00) | 10 (17.90) |
| Class 2 | 4 (7.15) | 11 (19.60) | 38 (67.90) | 33 (58.90) |
| Class 3 | 0 (0.00) | 0 (0.00) | 4 (7.10) | 13 (23.20) |
| Outcomes | Baseline | 3 months | 6 months | 9 months |
| Atrial fibrillation | 0 (0.00) | 0 (0.00) | 2 (3.60) | 1 (1.80) |
| Stroke | 0 (0.00) | 0 (0.00) | 1 (1.80) | 0 (0.00) |
Several studies have demonstrated the long-term effects of right ventricular apical pacing; however, information regarding its acute and early effects on LV function is limited. In the present study, the first significant change in LV function was observed in LVEF. Ejection fraction, which links preload, afterload, and contractility, is one of the most useful indices of LV function. Our study detected a subtle change in hemodynamic performance through a significant decrease in LVEF, consistent with previous studies where LVEF was observed to be 59.8 ± 12 in the DDDR mode of pacing. However, a significant decrease in LVEF was observed for both pacing modes in our study, suggesting that RVP impacts LV function, particularly by altering LVEF.
In this study, over 73.2% of the study population was male, similar to previous studies in which the majority of par
IVRT is the time interval between the end of aortic ejection and the beginning of ventricular filling. In our study, a slight increase in IVRT values (89.53 ± 9.54 ms) was found in patients in the VVIR, similar to the findings of Dwivedi et al[9], who reported a significantly higher value in the VVIR pacing mode (135.24 ± 28.54 ms). In our study, no significant differences in IVRT values were observed in the DDDR. The mean LVEDD and LVESD in the VVIR in our study were 43.78 ± 3.04 mm and 25.98 ± 1.30 mm, respectively, whereas in the study by Dwivedi et al[9], the respective values were 51.6 ± 1.01 mm and 39.6 ± 1.00 mm (VVIR mode).
A study conducted by Gupta et al[11] in 2021 estimated the E/A and E/E´ ratios and observed a progressive increase in their values over a 6-month period, suggesting a deterioration in LV diastolic function. Our results indicate that the ratios remained within normal limits for both pacing modes throughout the study period, consistent with a previous study that measured the E/A ratio during dual-chamber pacing, where it was noted to be 0.95 ± 0.2[12].
In this study, the complications of pacemaker implantation were not significantly different between the single- and DDDR modes. The overall incidence of AF at the 6-month follow-up (VVIR mode) was 3.6%, whereas it was lower at the 9-month follow-up (DDDR mode), i.e., 1.8%. However, in a study conducted by Mueller et al[13], a higher incidence of tachycardia was observed in patients with dual-chamber implantation. A study by Fisher et al[14] in 1988 indicated that the risk of stroke in patients with cardiac pacing is uncertain, although stroke has been reported in 4.5%-23% of paced patients with SSS during long-term follow-up. In our recent study, among 56 of our study population, 1.8% (1 patient) developed stroke during the VVIR mode (Figure 2).
Previous studies have suggested that a superior QoL is observed in patients with dual-chamber pacing. In a study by Lamas et al[15] in 1998, QoL was evaluated using the SF-36 scoring method, which showed no significant differences between the ventricular pacing and dual-chamber pacing groups at the 3- and 18-month follow-up. Our results demonstrate a significant improvement in the QoL scores for the study population in both dual- and single-pacing modes. Figure 2 depicts the centre all illustration of these study.
This was a single-centre, prospective study conducted at a tertiary healthcare facility with a small sample size. After switching the pacemaker mode to the dual-chamber mode, the patients were followed for a short period. Additionally, the effect of different pacing sites on LV function was not evaluated, as only the RV apex lead position was available for this study. Although the patients received the medications for associated comorbidities as per the guidelines but treatment data was not assessed.
This study suggests that RVP has a depressant effect on LV function, particularly in the VVIR mode. The DDDR mode appeared to achieve better clinical outcomes, with lower incidences of AF, stroke, and heart failure compared with the VVIR mode. Furthermore, health-related QoL significantly improved after pacemaker implantation. Overall, these findings indicate that the DDDR pacing mode is preferable to the VVIR mode.
| 1. | Mulpuru SK, Madhavan M, McLeod CJ, Cha YM, Friedman PA. Cardiac Pacemakers: Function, Troubleshooting, and Management: Part 1 of a 2-Part Series. J Am Coll Cardiol. 2017;69:189-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 150] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 2. | Haffajee CI. Temporary cardiac pacing: modes, evaluation of function, equipment, and trouble shooting. Cardiol Clin. 1985;3:515-526. [PubMed] |
| 3. | Fisher JD, Kim SG, Mercando AD. Electrical devices for treatment of arrhythmias. Am J Cardiol. 1988;61:45A-57A. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 42] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Nahlawi M, Waligora M, Spies SM, Bonow RO, Kadish AH, Goldberger JJ. Left ventricular function during and after right ventricular pacing. J Am Coll Cardiol. 2004;44:1883-1888. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 163] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 5. | Bleasdale RA, Turner MS, Mumford CE, Steendijk P, Paul V, Tyberg JV, Morris-Thurgood JA, Frenneaux MP. Left ventricular pacing minimizes diastolic ventricular interaction, allowing improved preload-dependent systolic performance. Circulation. 2004;110:2395-2400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 53] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 6. | Linde-Edelstam C, Nordlander R, Undén AL, Orth-Gomér K, Rydén L. Quality-of-life in patients treated with atrioventricular synchronous pacing compared to rate modulated ventricular pacing: a long-term, double-blind, crossover study. Pacing Clin Electrophysiol. 1992;15:1467-1476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 56] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Tang CY, Kerr CR, Connolly SJ. Clinical trials of pacing mode selection. Cardiol Clin. 2000;18:1-23, vii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Naegeli B, Kurz DJ, Koller D, Straumann E, Furrer M, Maurer D, Minder E, Bertel O. Single-chamber ventricular pacing increases markers of left ventricular dysfunction compared with dual-chamber pacing. Europace. 2007;9:194-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Dwivedi SK, Bansal S, Puri A, Makharia MK, Narain VS, Saran RK, Hasan M, Puri VK. Diastolic and systolic right ventricular dysfunction precedes left ventricular dysfunction in patients paced from right ventricular apex. Indian Pacing Electrophysiol J. 2006;6:142-152. [PubMed] |
| 10. | Kim WH, Joung B, Shim J, Park JS, Hwang ES, Pak HN, Kim S, Lee M. Long-term outcome of single-chamber atrial pacing compared with dual-chamber pacing in patients with sinus-node dysfunction and intact atrioventricular node conduction. Yonsei Med J. 2010;51:832-837. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Gupta H, Showkat HI, Aslam N, Tandon R, Wander GS, Gupta S, Anwar S, Sohil MM. Chronology of cardiac dysfunction after permanent pacemaker implantation: an observational 2 year prospective study in North India. Int J Arrhythm. 2021;22:11. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (1)] |
| 12. | Vardas PE, Simantirakis EN, Parthenakis FI, Chrysostomakis SI, Skalidis EI, Zuridakis EG. AAIR versus DDDR pacing in patients with impaired sinus node chronotropy: an echocardiographic and cardiopulmonary study. Pacing Clin Electrophysiol. 1997;20:1762-1768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Mueller X, Sadeghi H, Kappenberger L. Complications after single versus dual chamber pacemaker implantation. Pacing Clin Electrophysiol. 1990;13:711-714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Fisher M, Kase CS, Stelle B, Mills RM Jr. Ischemic stroke after cardiac pacemaker implantation in sick sinus syndrome. Stroke. 1988;19:712-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Lamas GA, Orav EJ, Stambler BS, Ellenbogen KA, Sgarbossa EB, Huang SK, Marinchak RA, Estes NA 3rd, Mitchell GF, Lieberman EH, Mangione CM, Goldman L. Quality of life and clinical outcomes in elderly patients treated with ventricular pacing as compared with dual-chamber pacing. Pacemaker Selection in the Elderly Investigators. N Engl J Med. 1998;338:1097-1104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 417] [Cited by in RCA: 373] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/