Published online Jan 26, 2024. doi: 10.4330/wjc.v16.i1.40
Peer-review started: August 29, 2023
First decision: October 24, 2023
Revised: November 21, 2023
Accepted: January 2, 2024
Article in press: January 2, 2024
Published online: January 26, 2024
Processing time: 142 Days and 14.8 Hours
Left bundle branch pacing (LBBP) is a novel pacing modality of cardiac resyn
To explore the validity of electromechanical resynchronization, clinical and echocardiographic response of LBBP-CRT.
Systematic review and Meta-analysis were conducted in accordance with the standard guidelines as mentioned in detail in the methodology section.
In our analysis, the success rate of LBBP-CRT was determined to be 91.1%. LBBP-CRT significantly shortened QRS duration, with significant improvement in echocardiographic parameters, including left ventricular ejection fraction, left ventricular end-diastolic diameter and left ventricular end-systolic diameter in comparison with BiVP-CRT.
A significant reduction in New York Heart Association class and B-type natriuretic peptide levels was also observed in the LBBP-CRT group vs BiVP-CRT group. Lastly, the LBBP-CRT cohort had a reduced pacing threshold at follow-up as compared to BiVP-CRT.
Core Tip: Left bundle branch pacing (LBBP) is a unique pacing modality in cardio resynchronization therapy. LBBP-cardiac resynchronization therapy (CRT) improves the left ventricular ejection fraction, echocardiographic parameters, and clinical outcomes when compared to biventricular pacing (BiVP). It causes significant reduction in New York Heart Association class, pacing threshold and B-type natriuretic peptide. This systematic review and meta-analysis reviews and analyze the data comparing LBBP vs BiVP-CRT.
- Citation: Yasmin F, Moeed A, Ochani RK, Raheel H, Awan MAE, Liaquat A, Saleem A, Aamir M, Hawwa N, Surani S. Left bundle branch pacing vs biventricular pacing in heart failure patients with left bundle branch block: A systematic review and meta-analysis. World J Cardiol 2024; 16(1): 40-48
- URL: https://www.wjgnet.com/1949-8462/full/v16/i1/40.htm
- DOI: https://dx.doi.org/10.4330/wjc.v16.i1.40
Left bundle branch block (LBBB) is of paramount importance given the evidence of worse prognosis in severe, symptomatic heart failure (HF) patients[1,2]. Cardiac resynchronization therapy (CRT) carries a strong recommendation for symptomatic patients with sinus rhythm, QRS duration (QRSd) ≥ 150 ms with LBBB morphology, and left ventricular ejection fraction (LVEF) ≤ 35% despite optimal medical therapy, with the goal of relieving symptoms and minimizing morbidity and mortality[3]. Biventricular pacing (BiVP) is the conventional CRT for LBBB, with HF showing significantly improved patient mortality[4]. However, not all patients respond to it, with an alarming non-response rate of approximately one-third[5]. Left bundle branch pacing (LBBP), a sub-type of conduction system pacing (CSP), has increasingly gained traction lately as an emerging, effective mode of CRT since it first showed a complete reversal of LBBB in HF patients[6]. Both procedures are subjected to non-responses due to variable patterns of mechanical desynchrony in HF patients, left ventricular pacing site, and cause of HF[5]. LBBP is deemed to be a less complex procedure and can target distal and deeper to the bundle of His such that it now serves as a potential alternative to His bundle pacing (HBP), i.e., the more traditionally used type of CSP for LBBB[6]. Very recently, Wang et al[7] conducted the first randomized control trial (RCT) evaluating the efficacy of LBBP-CRT in improving echocardiographic parameters among patients with HF and reduced LVEF and demonstrated a greater degree of LVEF improvement with LBBP-CRT in comparison to BiVP-CRT. Another recent analysis by Chen et al[8] showed LBBP-CRT to have better electromechanical resynchronization, higher clinical and echocardiographic response, and especially higher rate of super-response than BiVP-CRT in patients with LVEF ≤ 35%, and LBBB with HF. A previous meta-analysis conducted by Cheng et al[9] excluded these studies, thus resulting in lower statistical power and inconsistent results. Hence, we performed an updated analysis pooling the first ever RCT published in the literature to provide a comprehensive clinical evaluation of the efficacy of LBBP-CRT and confirm the validity of the improved electromechanical resynchronization and clinical outcomes in comparison to BiVP-CRT.
This systematic review and meta-analysis were conducted in accordance with the established methods recommended by the PRISMA, Cochrane, and AMSTAR-2 guidelines[10-12].
An extensive literature search was conducted using MEDLINE (PubMed), Cochrane Library, and Scopus from inception through October 2022 to identify relevant studies evaluating the clinical and echocardiographic metrics between LBBP-CRT vs BiVP-CRT among HF patients with LBBB. We applied Boolean Operators ‘OR’ and ‘AND’ among synonymous and different Medical subject headings terms and keywords, including ‘left bundle branch pacing’ OR ‘left bundle branch area pacing’ AND ‘left bundle branch block’ AND ‘heart failure’. We placed no restrictions based on time, language, year, or geographical location/country of publication. We further manually searched reference lists of retrieved original publications, review articles, editorials, and online databases comprising Clinicaltrials.gov and preprints via MedRix.org to identify any grey literature.
All the articles that were retrieved after the systematic search were exported to Endnote Reference Manager (Version X4; Clarivate Analytics, Philadelphia, PA, United States), where duplicates were identified and removed. Two independent reviewers (Moeed A and Raheel H) carefully examined the articles initially by title and abstract and then by full text to ensure relevance, and any disagreement was resolved through mutual consensus with the involvement of the senior investigator (Yasmin F). Articles with the following inclusion criteria were added to the review: (1) HF patients with LBBB; (2) comparative studies between LBBP and BVP; (3) studies reporting at least one of the outcomes of interest; and (4) retrospective or prospective cohort and RCT’s.
Two investigators (Moeed A and Raheel H) independently extracted data from shortlisted studies using pre-specified collection forms. All data related to the population and study characteristics were collected in addition to the outcomes of interest. The primary outcome of interest was QRSd. Secondary outcomes included pacing threshold, New York Heart Association (NYHA) classification, B-type natriuretic peptide (BNP) level, and echocardiographic parameters, including LVEF, left ventricular end-diastolic diameter (LVEDD) and left ventricular end-systolic diameter (LVESD). The quality assessment of the observational studies was performed using the Newcastle-Ottawa scale[13], based on the pre-specified criterion of comparability, selection, and outcome or exposure of included studies, while Cochrane Collaboration's risk of bias tool for randomized controlled trials[14] was used to assess the quality of the RCT.
Review Manager (Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) was utilized for all statistical analyses. A random-effects model was employed, and the effect size was pooled as mean differences (MD) with corresponding 95% confidence intervals (95%CIs). Heterogeneity across studies was evaluated using Higgins
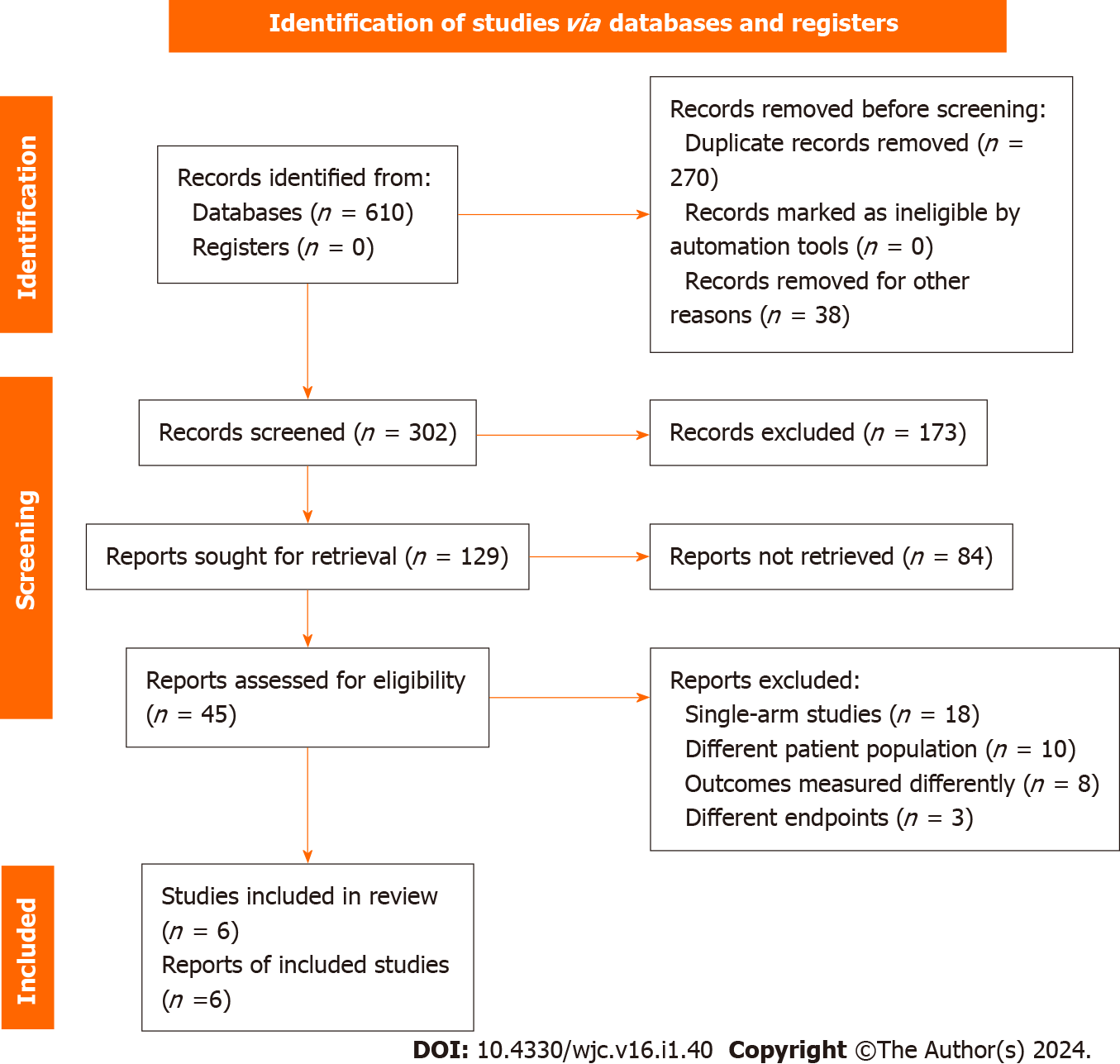
A preliminary search of the electronic databases yielded a total of 790 results. Applying the aforementioned eligibility criteria, 6 studies were included in the review[8,7,16-19]. A detailed description of the complete search strategy applied for each database is given in Supplementary Table 1, and the PRISMA flow chart summarizing the search and study selection process is given in Figure 1. A total of 6 studies (1 RCT and 5 comparative observational studies) with 389 participants (159 in LBBP-CRT vs 230 in BiVP-CRT) across 12 centers were included with a median follow-up of 9 mo (IQR 6-12.6)[8,7,16-19]. The LBBP-CRT success rate was 91.1%. Overall, 50.3% of the population constituted of males, and the mean age was 64 ± 4 years. Detailed study and patient characteristics are given in Table 1.
| Ref. | Area | Centre | Study design | Number of participants in LBBP | Number of participants in BiVP | Patients | Male sex in LBBP (%) | Age (yr) in LBBP | Success rate in LBBP (%) | Follow up (mo) | ICM (%) in LBBP |
| Wang et al[16], 2020 | China | 1 | Matched case-control | 10 | 30 | HF, LBBB | 90.0 | 64.8 ± 7.1 | 100.0 | 6.0 | 10 |
| Guo et al[17], 2020 | China | 1 | Prospective observational | 21 | 21 | HF, LBBB | 42.9 | 66.1 ± 9.7 | 87.5 | 14.3 | 9.5 |
| Wu et al[18], 2021 | China | 1 | Prospective non-randomized | 32 | 54 | HF, LBBB | 43.8 | 67.2 ± 13 | 100.0 | 12.0 | 3.1 |
| Li et al[19], 2020 | China | 3 | Prospective observational | 27 | 54 | HF, LBBB | 58.1 | 56.8 ± 1 0.1 | 81.1 | 6.0 | 18.9 |
| Chen et al[8], 2022 | China | 4 | Prospective observational | 49 | 51 | HF, LBBB | 50.0 | 67.1 ± 8.9 | 91.1 | 12.0 | 0 |
| Wang et al[7], 2022 | China | 2 | Randomized controlled trial | 20 | 20 | HF, LBBB | 35.0 | 62.3 ± 11.2 | 90.0 | 6.0 | 0 |
All articles reported QRSd as an outcome. QRSd was significantly decreased with LBBP-CRT vs BiVP-CRT (LBBP-CRT mean 115.4 vs BiVP-CRT mean 138.0; MD = -22.65, 95%CI: -30.87 to -14.44, P < 0.00001, I2 = 88%) (Figure 2).
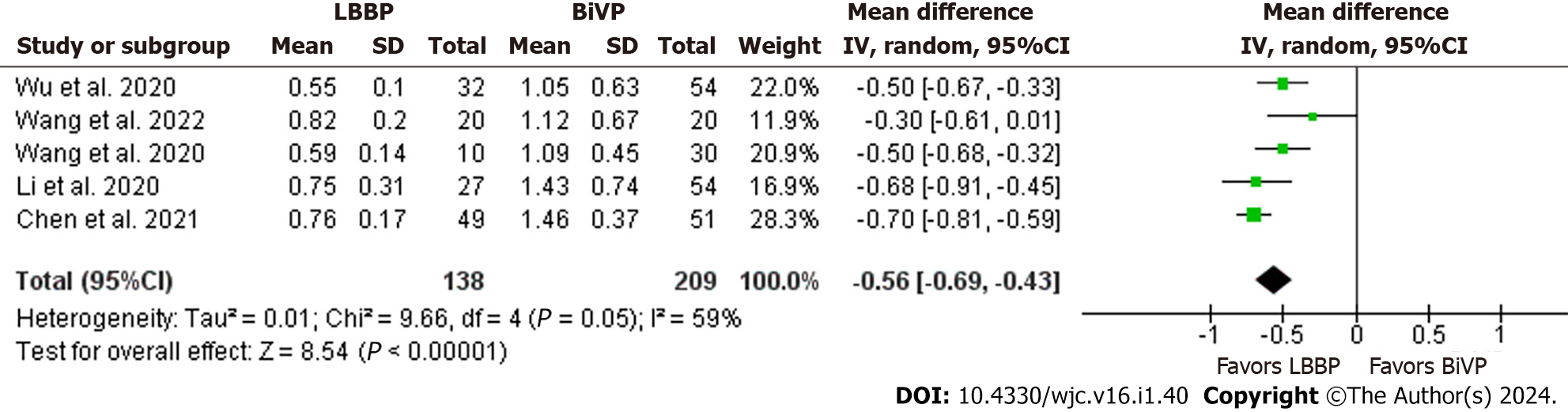
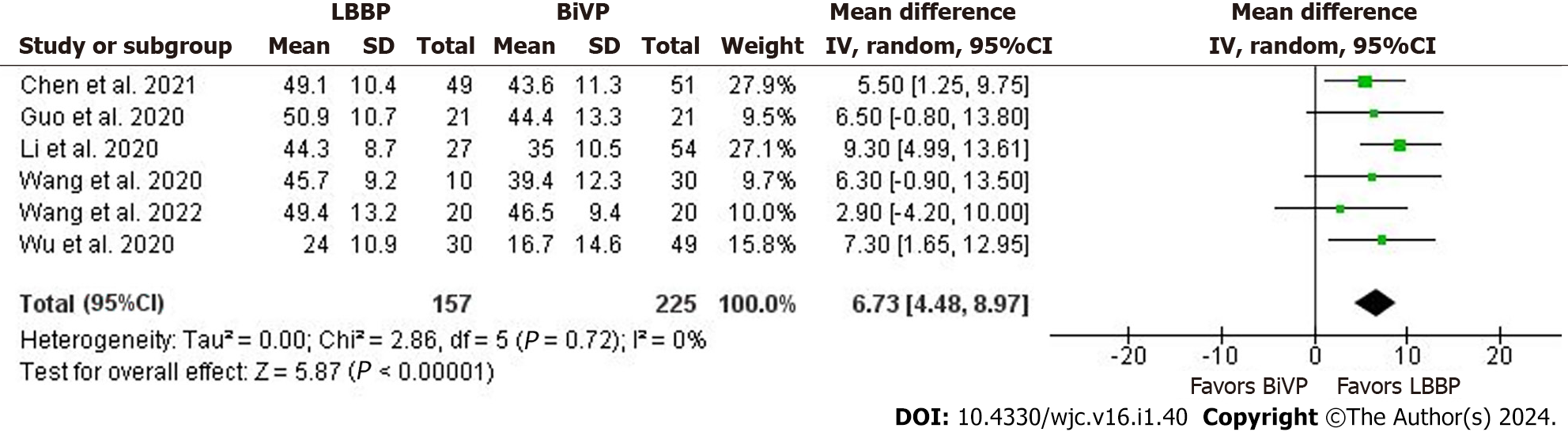
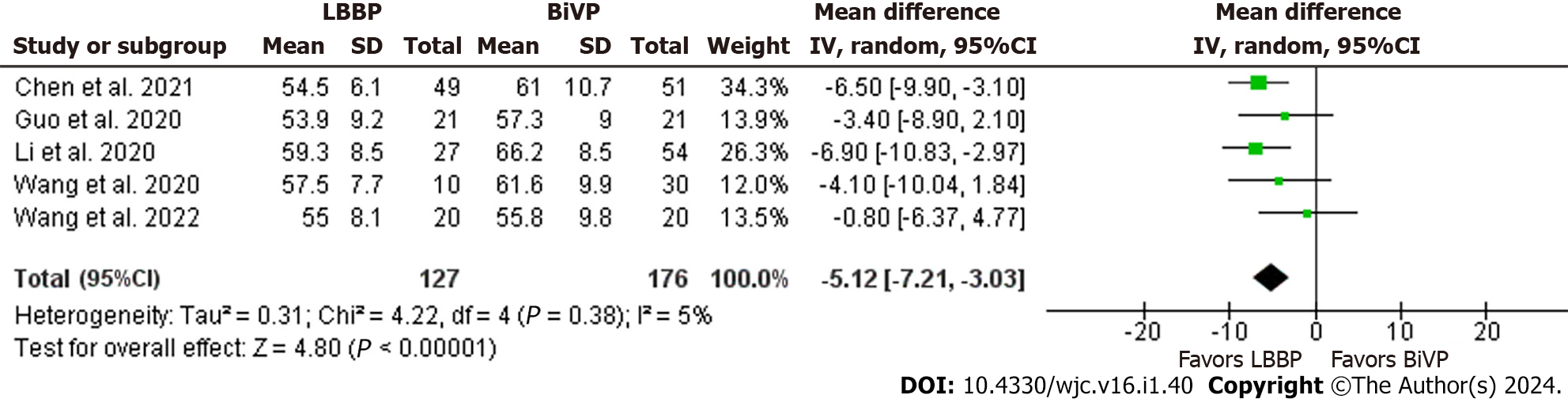
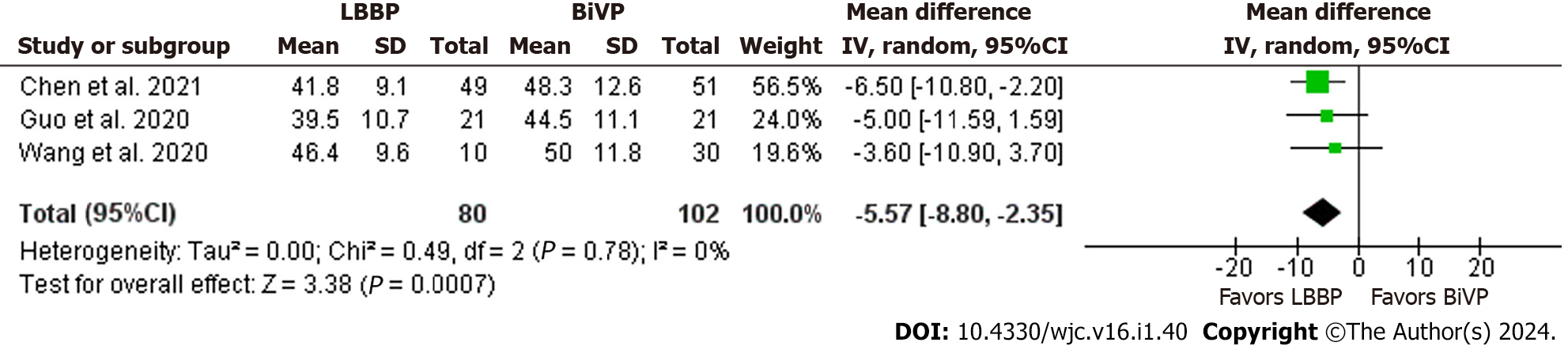
Pacing threshold was also significantly lower in LBBP-CRT group compared to BiVP-CRT (LBBP-CRT mean 0.69 vs BiVP-CRT mean 1.24; MD = -0.56, 95%CI: -0.69 to 0.43, P < 0.00001, I2 = 59%) (Figure 3). LBBP-CRT resulted in significantly increased LVEF (LBBP-CRT mean 43.8 vs BiVP-CRT mean 37.6; MD = 6.73, 95%CI: 4.48 to 8.97, P < 0.00001, I2 = 0%), significantly decreased LVEDD (LBBP-CRT mean 55.9 vs BiVP-CRT mean 60.6; MD = -5.12, 95%CI: -7.21 to -3.03, P < 0.00001, I2 = 5%), and reduced LVESD (LBBP-CRT mean 42.0 vs BiVP-CRT mean 47.3; MD = -5.57, 95%CI: -8.80 to -2.35, P < 0.00007, I2 = 0%) compared to BiVP-CRT (Figures 4-6). The pooled analysis showed a significant decrease in NYHA class in LBBP-CRT vs BiVP-CRT patients (LBBP-CRT mean 1.3 vs BiVP-CRT mean 1.8; MD = -0.47, 95%CI: -0.73 to -0.21, P < 0.00003, I2 = 65%) (Figure 7). LBBP-CRT showed a statistically significant decrease in BNP concentration on follow-up compared to BiVP-CRT (LBBP-CRT mean 311.3 vs BiVP-CRT mean 1145.3; SMD = -0.66, 95%CI: -0.96 to -0.35, P < 0.00001, I2 = 0%) (Figure 8).
We additionally performed a series of sensitivity analysis to determine if any outlier study had disproportionate effects on the pooled estimates for the outcomes of QRSd, pacing threshold, and NYHA class. We found no change in the significance of the pooled results (Supplementary Figures 1-3).
Owing to the robust methodology, most cohort studies were categorized as moderate to high quality on the NOS assessment tool. Wang et al[7] 2022 study was the only clinical trial included in the review, which was assessed through Cochrane risk of bias. All domains had a low risk of bias except the deviation from the intended interventions domain. The results of the quality assessment are mentioned in Supplementary Tables 2 and 3. The PRISMA and AMSTAR checklists have been included in Supplementary Tables 4 and 5.
In comparison to BiVP-CRT, LBBP-CRT was demonstrated to be safe and effective in enhancing LVEF with a low and consistent threshold. A smaller QRSd has been linked to improved mechanical synchronization of the ventricle[20]. Thus, our meta-analysis revealed that CRT provided more effective electrical and mechanical resynchronization via LBBP. Our study analyzed the pacing threshold at the time of implant and the pacing threshold at the time of follow-up. Five studies included in our analysis reported that the pacing threshold in LBBP-CRT was much lower than in BiVP-CRT. This is consistent with previous studies in which the pacing threshold at implant was lower in LBBP-CRT vs BiVP-CRT, and remained considerably lower in LBBP-CRT at 6-months and 1-year follow-up[8]. All six of our studies reported LVEF data. When compared to BiVP-CRT, LBBP-CRT dramatically raised LVEF. This is consistent with earlier studies in which patients in the LBBP-CRT group had significantly greater LVEF at 6-month follow-up than patients in the BiVP-CRT group[8], and a recent study by Vijayaraman et al[21] found a greater increase in LVEF with LBBP. In our analysis, five studies reported a substantial reduction in LVEDD with LBBP-CRT compared to BiVP-CRT. This is consistent with prior research, including a report by Huang et al[6], who first described LBBB and dilated cardiomyopathy in a 72-year-old lady with HF treated with LBBP.
They employed a low-pacing output to rectify the LBBB on the electrocardiogram, which RBBB accompanied. At one year, they discovered that LVEDD decreased to 42 mm from a baseline 76 mm[6].
Three studies reported on follow-up LVESD, which was much lower in LBBP-CRT patients compared to BiVP-CRT, which is consistent with earlier research in which LVESD was also significantly lower[22,23]. Furthermore, three studies reported increased BNP levels to have a strong clinical and hemodynamic correlation with the degree of left ventricular dysfunction. Our study demonstrated that LBBP-CRT patients had a statistically significant lower BNP concentration on follow-up than BiVP-CRT patients. Similar prior studies, such as Huang et al[6], reported a decrease in the BNP concentration from baseline. Moreover, NYHA classification was assessed when patients were followed up, and five studies revealed a substantial drop-in NYHA class in LBBP-CRT patients compared to BiVP-CRT patients. This is consistent with previous studies, which have shown that in comparison to BiVP-CRT, LBBP-CRT may reduce NYHA class[9].
This meta-analysis has some limitations. All of the studies included in the quantitative synthesis were conducted in China. Thus, the results may not be applicable to a more diverse population. The median follow-up time of the included studies was 9 mo, serving as a limitation in judging the long-term efficacy of either of the two pacing methods. Although we included the first and only RCT published in the literature in our analysis, the majority of our pooled comparative studies were observational with small to moderate sample sizes. This could have introduced significant heterogeneity, however, to mitigate this compromise, we chose a random-effects methodology for our analysis. Thus, to ascertain the benefit of LBBP or BiVP in LBBB patients, it is imperative to conduct large-scale RCTs to solidify which pacing method is more appropriate in HF patients.
To conclude, our meta-analysis provided further clarity regarding the benefits of the novel LBBP-CRT in improving LVEF, cardiac echocardiographic parameters, and clinical outcomes when compared to BiVP-CRT.
Biventricular pacing (BiVP) is the conventional mode of cardiac resynchronization therapy (CRT) for left bundle branch block (LBBB) with heart failure (HF), and shows significantly improved patient mortality. However, approximately one-third of the patients fail to response to it. Left bundle branch pacing (LBBP) has gained increasing attention recently as an effective mode of CRT showing complete reversal of LBBB among HF patients.
Several clinical studies evaluating the efficacy of LBBP-CRT in improving electromechanical resynchronization, clinical, and echocardiographic response in comparison to BiVP-CRT among patients with reduced left ventricular ejection fraction (LVEF), LBBP, and HF have been published but the results remain inconclusive. Hence, we performed an updated analysis pooling the recent clinical data to provide a comprehensive clinical evaluation of the efficacy of LBBP-CRT and confirm the validity of the improved electromechanical resynchronization and clinical outcomes in comparison to BiVP-CRT.
The primary outcome of interest was QRS duration. Secondary outcomes included pacing threshold, New York Heart Association (NYHA) classification, B-type natriuretic peptide (BNP) level, and echocardiographic parameters, including LVEF, l left ventricular end-diastolic diameter (LVEDD) and left ventricular end-systolic diameter (LVESD).
An extensive literature search was conducted using MEDLINE (PubMed), Cochrane Library, and Scopus from inception through October 2022 to identify relevant studies evaluating the clinical and echocardiographic metrics between LBBP-CRT vs BiVP-CRT among HF patients with LBBB. A random-effects model was employed, and the effect size was pooled as mean differences with corresponding 95% confidence intervals. A P < 0.05 was considered statistically significant in all cases.
The success rate of LBBP-CRT was observed to be 91.1% in our analysis. LBBP-CRT resulted in increased LVEF, reduction in LVEDD, and LVESD compared to BiVP-CRT. Significantly reduced BNP levels, and NYHA class was also noted in the LBBP-CRT group vs BiVP-CRT group. Lastly, the LBBP-CRT cohort had a reduced pacing threshold at follow-up as compared to BiVP-CRT.
Our analysis compared success rate, echocardiographic parameters and clinical response between LBBP-CRT vs BiVP-CRT and demonstrated LBBP-CRT to result in significantly improved cardiac echocardiographic parameters, and clinical outcomes when compared to BiVP-CRT.
LBBP-CRT resulting in significant improvement in the echocardiographic parameters and clinical outcomes can help shape the clinical practice. Further larger randomized control trials are needed.
| 1. | Master AM, Kalter H, Dack S, Jaffe HL. The relation between bundle branch block and cardiac enlargement. Am Heart J. 1940;20: 186-194. [RCA] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 18] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Tabrizi F, Englund A, Rosenqvist M, Wallentin L, Stenestrand U. Influence of left bundle branch block on long-term mortality in a population with heart failure. Eur Heart J. 2007;28:2449-2455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 56] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Authors/Task Force Members; McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, Cleland JGF, Coats AJS, Crespo-Leiro MG, Farmakis D, Gilard M, Heymans S, Hoes AW, Jaarsma T, Jankowska EA, Lainscak M, Lam CSP, Lyon AR, McMurray JJV, Mebazaa A, Mindham R, Muneretto C, Francesco Piepoli M, Price S, Rosano GMC, Ruschitzka F, Kathrine Skibelund A; ESC Scientific Document Group. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2022;24:4-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 1521] [Article Influence: 380.3] [Reference Citation Analysis (2)] |
| 4. | Kong NW, Upadhyay GA. Cardiac resynchronization considerations in left bundle branch block. Front Physiol. 2022;13:962042. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Birnie DH, Tang AS. The problem of non-response to cardiac resynchronization therapy. Curr Opin Cardiol. 2006;21:20-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 213] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 6. | Huang W, Su L, Wu S, Xu L, Xiao F, Zhou X, Ellenbogen KA. A Novel Pacing Strategy With Low and Stable Output: Pacing the Left Bundle Branch Immediately Beyond the Conduction Block. Can J Cardiol. 2017;33:1736.e1-1736.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 429] [Cited by in RCA: 561] [Article Influence: 62.3] [Reference Citation Analysis (0)] |
| 7. | Wang Y, Zhu H, Hou X, Wang Z, Zou F, Qian Z, Wei Y, Wang X, Zhang L, Li X, Liu Z, Xue S, Qin C, Zeng J, Li H, Wu H, Ma H, Ellenbogen KA, Gold MR, Fan X, Zou J; LBBP-RESYNC Investigators. Randomized Trial of Left Bundle Branch vs Biventricular Pacing for Cardiac Resynchronization Therapy. J Am Coll Cardiol. 2022;80:1205-1216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 256] [Article Influence: 64.0] [Reference Citation Analysis (0)] |
| 8. | Chen X, Ye Y, Wang Z, Jin Q, Qiu Z, Wang J, Qin S, Bai J, Wang W, Liang Y, Chen H, Sheng X, Gao F, Zhao X, Fu G, Ellenbogen KA, Su Y, Ge J. Cardiac resynchronization therapy via left bundle branch pacing vs. optimized biventricular pacing with adaptive algorithm in heart failure with left bundle branch block: a prospective, multi-centre, observational study. Europace. 2022;24:807-816. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 108] [Article Influence: 27.0] [Reference Citation Analysis (0)] |
| 9. | Cheng Y, Wang Z, Li Y, Qi J, Liu J. Left bundle branch pacing in heart failure patients with left bundle branch block: A systematic review and meta-analysis. Pacing Clin Electrophysiol. 2022;45:212-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44932] [Cited by in RCA: 51908] [Article Influence: 10381.6] [Reference Citation Analysis (2)] |
| 11. | Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, Thomas J. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:ED000142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1361] [Cited by in RCA: 3428] [Article Influence: 489.7] [Reference Citation Analysis (1)] |
| 12. | Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E, Henry DA. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3100] [Cited by in RCA: 6527] [Article Influence: 725.2] [Reference Citation Analysis (0)] |
| 13. | Wells GA, Shea B, Connell DO, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-OttawWells BS. a Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. [cited 13 December 2023]. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. |
| 14. | Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge SM, Emberson JR, Hernán MA, Hopewell S, Hróbjartsson A, Junqueira DR, Jüni P, Kirkham JJ, Lasserson T, Li T, McAleenan A, Reeves BC, Shepperd S, Shrier I, Stewart LA, Tilling K, White IR, Whiting PF, Higgins JPT. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6581] [Cited by in RCA: 18882] [Article Influence: 2697.4] [Reference Citation Analysis (0)] |
| 15. | Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39087] [Cited by in RCA: 48640] [Article Influence: 2114.8] [Reference Citation Analysis (4)] |
| 16. | Wang Y, Gu K, Qian Z, Hou X, Chen X, Qiu Y, Jiang Z, Zhang X, Wu H, Chen M, Zou J. The efficacy of left bundle branch area pacing compared with biventricular pacing in patients with heart failure: A matched case-control study. J Cardiovasc Electrophysiol. 2020;31:2068-2077. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 65] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 17. | Guo J, Li L, Xiao G, Ye T, Huang X, Meng F, Li Q, Chen S, Cai B. Remarkable response to cardiac resynchronization therapy via left bundle branch pacing in patients with true left bundle branch block. Clin Cardiol. 2020;43:1460-1468. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 48] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 18. | Wu S, Su L, Vijayaraman P, Zheng R, Cai M, Xu L, Shi R, Huang Z, Whinnett ZI, Huang W. Left Bundle Branch Pacing for Cardiac Resynchronization Therapy: Nonrandomized On-Treatment Comparison With His Bundle Pacing and Biventricular Pacing. Can J Cardiol. 2021;37:319-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 199] [Article Influence: 33.2] [Reference Citation Analysis (0)] |
| 19. | Li X, Qiu C, Xie R, Ma W, Wang Z, Li H, Wang H, Hua W, Zhang S, Yao Y, Fan X. Left bundle branch area pacing delivery of cardiac resynchronization therapy and comparison with biventricular pacing. ESC Heart Fail. 2020;7:1711-1722. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 101] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 20. | Gu Y, Li Y, Zhu Y, Lin X, Tian T, Zhang Q, Gong J, Wang L, Li J. Cardiac resynchronization therapy in heart failure patients by using left bundle branch pacing. Front Cardiovasc Med. 2022;9:990016. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 21. | Vijayaraman P, Sharma PS, Cano Ó, Ponnusamy SS, Herweg B, Zanon F, Jastrzebski M, Zou J, Chelu MG, Vernooy K, Whinnett ZI, Nair GM, Molina-Lerma M, Curila K, Zalavadia D, Haseeb A, Dye C, Vipparthy SC, Brunetti R, Moskal P, Ross A, van Stipdonk A, George J, Qadeer YK, Mumtaz M, Kolominsky J, Zahra SA, Golian M, Marcantoni L, Subzposh FA, Ellenbogen KA. Comparison of Left Bundle Branch Area Pacing and Biventricular Pacing in Candidates for Resynchronization Therapy. J Am Coll Cardiol. 2023;82:228-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 182] [Article Influence: 60.7] [Reference Citation Analysis (0)] |
| 22. | Zhang W, Huang J, Qi Y, Wang F, Guo L, Shi X, Wu W, Zhou X, Li R. Cardiac resynchronization therapy by left bundle branch area pacing in patients with heart failure and left bundle branch block. Heart Rhythm. 2019;16:1783-1790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 166] [Article Influence: 23.7] [Reference Citation Analysis (0)] |
| 23. | Liu P, Wang Q, Sun H, Qin X, Zheng Q. Left Bundle Branch Pacing: Current Knowledge and Future Prospects. Front Cardiovasc Med. 2021;8:630399. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Society of Critical Care Medicine.
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Batta A, India S-Editor: Lin C L-Editor: A P-Editor: Yu HG