Published online Aug 26, 2023. doi: 10.4330/wjc.v15.i8.406
Peer-review started: May 22, 2023
First decision: June 14, 2023
Revised: June 24, 2023
Accepted: July 19, 2023
Article in press: July 19, 2023
Published online: August 26, 2023
Processing time: 90 Days and 24 Hours
Spontaneous coronary artery dissection (SCAD) is underdiagnosed and requires comprehensive angiographic findings. Few SCAD occurrences have a comparable clinical appearance as takotsubo syndrome (TTS) or exist simultaneously, making it challenging for clinicians to treat and manage. Case reports lack consolidated data. We examined SCAD-TTS case reports.
To conduct a systematic review of available case reports on SCAD in order to investigate its potential association with TTS.
SCAD-associated TTS case reports were reviewed after thoroughly screening PubMed, EMBASE, Scopus, and Google Scholar databases till January 2023. Case reports described demographics, comorbidities, imaging, management, and results.
Twelve articles about 20 female patients were analyzed. 30% of patients (n = 6, > 60 years) were elderly (mean age 56.2 ± 9.07 years, range 36-70 years). Canada has 9 cases, United States 3, Australia 3, Sweden 2, Japan, Denmark, and France 1. Only 5 reports identified emotional stressors in these cases while 4 reports showed physical triggers for TTS. Nine had hypertension, 2 had hyperlipidemia, and 1 had prediabetes. 5 patients (25%) smoked. 10 (50%) troponin-positive myocardial infarction patients reported chest discomfort. 11 (55%) of 20 instances had TTS/SCAD. 12 (60%) of 20 patients exhibited ST elevation and 3 (15%) had T wave inversion on electrocardiogram. 19/20 patients had elevated troponin. 9 (45%) of 20 people had apical akinesis with TTS ballooning on cardiac imaging. All 20 exhibited echocardiographic wall motion abnormalities. 19 (95%) of 20 coronary angiography cases had SCAD. 10 of 19 SCAD patients had left anterior descending, 2 diagonal, and 2 left circumflex coronary artery involvement. 7 of 20 patients had left ventricular ejection fraction (LVEF) data. LVEF averaged 38.78 ± 7.35%. 5 (25%) of the 20 cases underwent dual antiplatelet therapy. Three (15%) of 20 cases experienced occasional ectopic ventricular complexes, Mobitz ll AV block, and paroxysmal atrial fibrillation. All 20 cases recovered and survived.
Given the clinical similarities and challenges in detecting TTS and SCAD, this subset needs more research to raise awareness and reduce morbidity.
Core Tip: This study highlights the coexistence and clinical similarities of takotsubo syndrome and spontaneous coronary artery dissection, therefore emphasizing the importance of further research, awareness as well as comprehensive angiographic testing for effective diagnosis and management.
- Citation: Bhanushali A, Kohli M, Prakash A, Sarvepalli SR, Pandey A, Odugbemi O, Reyaz N, Trambadia B, Reddy SA, Chauhan S, Desai R. Spontaneous coronary artery dissection-associated takotsubo syndrome: A systematic review of case reports. World J Cardiol 2023; 15(8): 406-414
- URL: https://www.wjgnet.com/1949-8462/full/v15/i8/406.htm
- DOI: https://dx.doi.org/10.4330/wjc.v15.i8.406
Takotsubo syndrome (TTS), also known as "broken heart syndrome," mimics a myocardial infarction and is typically caused by an abrupt surge of stress hormones, such as catecholamines, in reaction to mental or physical stress[1]. These hormones can produce a transitory weakening of the heart's contractile cells, resulting in myocardial stunning and a specific pattern of wall motion abnormalities[2]. The exact pathophysiological process behind this syndrome is not completely understood. In addition, endothelial and microvascular dysfunction can produce abrupt constriction or spasms of the coronary arteries, resulting in reduced blood supply to the cardiac muscle and precipitating the symptoms of TTS[3]. Spontaneous coronary artery dissection (SCAD) and TTS have similar causes and prevalence. Stress causes both conditions, which affect women more. However, there are differences between these conditions. A rupture in the inner layer of the coronary artery wall can block or restrict blood flow and cause SCAD. SCAD may result from arterial defects, hormones, and genetics. TTS, a type of transient heart failure, can cause chest pain, shortness of breath, and other heart attack-like symptoms. TTS may be caused by the sympathetic nervous system's "fight or flight" response.
SCAD has been reported in patients with TTS despite these differences. Genetic, hormonal, and environmental factors may be involved. SCAD and TTS affect predominantly women, particularly postmenopausal women. There may be a hormonal component to both of these conditions. SCAD and TTS share comparable pathophysiology, symptoms, triggers, prevalence, and etiology but have distinct prognoses. Recent studies suggest a possible link between the two. TTS and SCAD have similar symptoms and etiologies, but their prognoses and outcomes are distinct. The majority of TTS patients recover without lasting effects. Cardiogenic shock, left ventricular rupture, and malignant arrhythmias are potentially lethal conditions. Patients with TTS are more likely to experience recurrent episodes and cardiovascular complications. SCAD causes myocardial infarction, heart failure, and sudden cardiac death. The severity, location, and presence of CAD influence the outcomes of SCAD. Patients with SCAD require medication, invasive procedures, and prolonged hospitalizations. This systematic review examines the presentation, clinical features, comorbidities, investigations, therapy, and outcomes of TTS and SCAD patients. TTS patient case reports with SCAD imaging are reviewed. This review discusses the pathogenesis, causes, and potential links between these two cardiovascular disorders. The review examines patient data to identify trends that may improve the diagnosis, management, and outcomes of TTS and SCAD.
Literature review, Screening Titles/Abstracts and Population Selection Until January 2023, a comprehensive search of PubMed/Medline, EMBASE, Scopus, and Google Scholar was conducted to identify case reports and case series linked with spontaneous coronary artery dissection SCAD and TTS using relevant keywords such as Takotsubo syndrome, Takotsubo cardiomyopathy, broken heart syndrome, apical ballooning syndrome, stress-induced cardiomyopathy and spontaneous coronary artery dissection. The search was restricted to articles written in English only and with full text.
The systematic review comprised case reports and case series on the clinical presentation, diagnosis, and treatment of TTS with imaging evidence of SCAD. The exclusion of studies lacking sufficient TTS or SCAD-related information or failing to meet diagnostic criteria. Before retrieving the full-text papers for further evaluation, two reviewers evaluated the abstracts and titles of identified publications. To resolve conflicts, agreement or discussion with a third reviewer was sought.
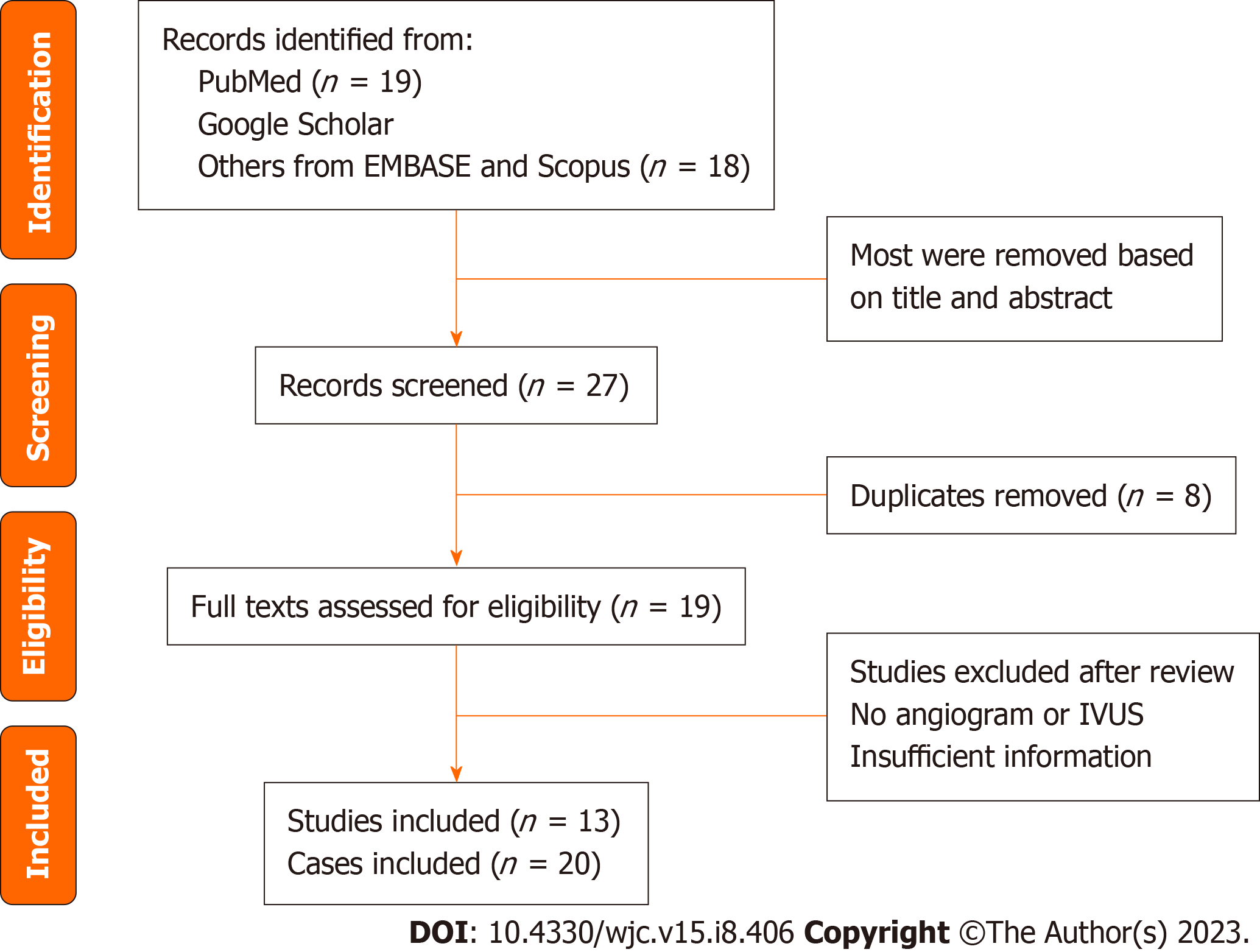
Up to January 2023, a thorough search as shown in PRISMA flow diagram (Figure 1) was carried out in the PubMed, Scopus, EMBASE and Google Scholar databases. "Spontaneous coronary artery dissection" (in title or abstract), "Takotsubo Syndrome" OR "Takotsubo Cardiomyopathy" OR "Broken Heart Syndrome" OR "apical ballooning syndrome" OR "stress-induced cardiomyopathy" (in title or abstract), and a publication date filter from 2000 to January 31, 2023, were all included in the search strategy. Publications classified as "editorial," "review," "comment," "meta-analysis," or "systematic review" were omitted; only case reports were included.
(1) Case studies describing the connection between TTS and SCAD; (2) Publications published from 2000 to January 31, 2023; and (3) Reports that detail the demographics, comorbidities, imaging results, management, and outcomes of SCAD-TTS cases.
(1) Publications labeled as "editorial," "review," "comment," "meta-analysis," or "systematic review"; (2) Studies that fail to mention how SCAD and TTS are related; (3) Publications released after January 31, 2023, but before 2000; and (4) Non-English articles. The search method was designed to locate pertinent case reports that satisfy the requirements for a thorough analysis of TTS related to SCAD.
From the included studies, we retrieved patient demographics (country of origin, age, gender), presenting complaints, comorbidities, medical interventions during hospitalization, imaging findings of SCAD, management, and outcomes. Using the Joanna Briggs Institute's critical appraisal criteria for case reports, the studies' quality was appraised.
It was determined that a meta-analysis was not viable due to the expected heterogeneity of the included studies. Instead, a narrative synthesis of the data with minimal descriptively pooled analysis, consisting of a systematic review and summary of findings, was performed. The clinical characteristics, imaging findings, treatment, and outcomes of TTS associated with SCAD were examined descriptively and presented in tabular format. Categorical data were displayed as numbers or percentages, whereas continuous data were displayed as means with standard deviations or medians with interquartile ranges. Excel was utilized for every descriptive statistic.
The data were synthesized by summarizing the features of the included studies, including the number of patients, gender distribution, age range, and the presence of co-morbidities. In addition, the imaging findings of SCAD, treatment, and results of TTS were presented.
The quality of the included studies was evaluated using the Joanna Briggs Institute's checklist for critical appraisal of case reports. Two reviewers examined the papers separately, and disagreements were resolved through consensus or contact with a third reviewer. Considering this is a systematic study of previously published case reports, ethical approval was not mandatory.
Twelve articles describing 20 female patients for the analysis were selected[4-15]. The mean age of the reported patients was 56.2 ± 9.07 years (range 36-70 years) out of which 40% of patients were elderly (n = 8, > 60 years). Out of the reported cases, 9 cases were from Canada, 3 cases each from USA, and Australia, 2 cases from Sweden and while Japan, Denmark and France contributed 1 case each. Only 5 reports identified emotional stressors in these cases while 4 reports showed physical stressors for TTS (Table 1).
| Ref. | Country | Age | Clinical presentation | Cardiovascular comorbidity | Prediabetes (Yes/No) | Smoker (Yes/No) |
| VI Chou et al[5], 2015 | Canada | 59 | Troponin positive MI | Yes | No | No |
| VII Chou et al[5], 2015 | Canada | 60 | Troponin positive MI | No | No | No |
| VIII Chou et al[5], 2015 | Canada | 50 | Troponin positive MI | Yes | No | No |
| IX Chou et al[5], 2015 | Canada | 50 | Troponin positive MI | Yes | No | No |
| Y-Hassan et al[14], 2016 | Sweden | 61 | Sudden onset of chest pain | No | No | No |
| Ghafoor et al[9], 2020 | United States | 52 | Chest pain, Palpitations | No | Yes | No |
| Takeuchi et al[13], 2021 | Japan | 36 | Left arm discomfort and convulsions | Yes | No | No |
| Blazak et al[4], 2022 | Australia | 65 | Severe chest pain | Yes | No | No |
| Y-Hassan et al[15], 2018 | Sweden | 67 | Chest pain, nausea, dyspnea | Yes | No | Yes |
| Fitouchi et al[7], 2022 | France | 49 | Retrosternal chest pain radiating to the left arm | No | No | No |
| Johnson et al[10], 2018 | United States | 66 | Chest pain, headache, and pain in her left jaw, left arm numbness | - | - | - |
| Desai et al[6], 2020 | United States | 67 | Chest discomfort, shortness of breath | Yes | No | No |
| Frederiksen et al[8], 2020 | Denmark | 57 | Left arm pain, chest discomfort, dyspnea, palpitation, elevated Bp | No | No | Yes |
| Sugito et al[12], 2020 | Australia | 56 | Central chest pain | No | No | No |
| McGhie et al[11], 2020 | Australia | 56 | Inferior STEMI | Yes | No | Yes |
Out of 20 cases, cardiovascular comorbidities were reported in 10 cases (hypertension in 9, hyperlipidemia in 2), and prediabetes in 1 case. 5 (25%) patients showed a history of smoking. The most common presenting symptom noticed was chest pain and discomfort in 9 cases (45%) and 10 (50%) cases presented with troponin-positive myocardial infarction. In 11 (55%) out of 20 cases, TTS and SCAD coexisted. Electrocardiogram was done in all 20 patients out of which 12 (60%) patients showed ST elevation and 3 (15%) showed T wave inversion. The baseline troponin level was measured in 19 cases and was elevated in all.
Out of 20, 9 (45%) cases showed apical akinesis and ballooning patterns of TTS on cardiac imaging. All 20 cases reported wall motion abnormalities on Echocardiography. In 19 (95%) out of 20 cases, SCAD was reported on coronary angiography. Out of 19 patients with SCAD, 10 showed involvement of left anterior descending (LAD) coronary artery, 2 showed diagonal artery, 2 showed left circumflex coronary (LCx) artery involvement, 2 showed marginal artery, 2 showed posterolateral artery, and a patient had a coexisting right coronary artery and LAD lesions. Out of 20 cases, data on left ventricular ejection fraction (LVEF) was reported in only 7 cases. The mean LVEF was 38.78 ± 7.35%. Out of 20, 5 (25%) cases were treated with dual antiplatelet therapy. Only 3 (15%) cases out of 20 reported complications with 1 case each of occasional ectopic ventricular complexes, Mobitz ll AV block, and ventricular fibrillation. All 20 cases survived and recovered (Table 2).
| Ref. | ECG | Troponin elevated? | Lesion & dissection involved which vessel? | LVgram | LVEF | DAPT (Yes/No) | SCAD and TTS coexist? | Complications | Final outcome |
| I Chou et al[5], 2015 | STEMI | Yes | RPLA | N/A | - | No | - | No | Survived |
| II Chou et al[5], 2015 | STEMI | Yes | 1st obtuse marginal and 1st Dx | N/A | - | No | - | No | Survived |
| III Chou et al[5], 2015 | Antero-lateral TWI | Yes | Distal LAD | N/A | - | No | - | No | Survived |
| IV Chou et al[5], 2015 | NSVT | Yes | Distal LPL | N/A | - | No | - | No | Survived |
| V Chou et al[5], 2015 | Antero-lateral TWI | Yes | 1st Dx | N/A | - | No | - | No | Survived |
| VI Chou et al[5], 2015 | STEMI | Yes | 1st mid-Dx | N/A | - | No | - | No | Survived |
| VII Chou et al[5], 2015 | Antero-lateral STD, TWI | Yes | Distal LAD, 3rd Dx | N/A | - | No | - | No | Survived |
| VIII Chou et al[5], 2015 | VT | Yes | Distal LAD | N/A | - | No | - | No | Survived |
| IX Chou et al[5], 2015 | STEMI | Yes | Distal LAD | N/A | - | No | - | No | Survived |
| Y-Hassan et al[14], 2016 | STEMI | Yes | Dx | LV apical ballooning | - | None | Coexist | No | Survived |
| Ghafoor et al[9], 2020 | STEMI | Yes | RCA and Distal LAD | Apical akinesis | 50-55% | Yes | Coexist | Occasional ectopic ventricular beats | Survived |
| Takeuchi et al[13], 2021 | STEMI | Yes | Middle to distal LAD | Apical ballooning | 39% | Yes | Coexist | No | Survived |
| Blazak et al[4], 2022 | NSTEMI | Yes | Dx | Apical akinesis | 28% | None | Coexist | No | Survived |
| Y-Hassan et al[23], 2018 | STEMI | Yes | Peripheral marginal branch | Circular mid-apical ballooning | 26% | None | Coexist | No | Survived |
| Fitouchi et al[7], 2022 | Sinus tachycardia | Yes | LAD | LV apical ballooning | 45% | Yes | Coexist | No | Survived |
| Johnson et al[10], 2018 | STEMI | Yes | - | Apical akinesis | 41% | None | Coexist | V. fib | |
| Desai et al[6], 2020 | STEMI | N/A | Typical TTS pattern | Apical ballooning | N/A | None | Coexist | No | Survived |
| Frederiksen et al[8], 2020 | NSTEMI | Yes | - | Apical akinesis | 40% | Yes | Coexist | No | Survived |
| Sugito et al[12], 2020 | STEMI | Yes | Typical TTS pattern | Circular mid-apical ballooning | N/A | None | Coexist | 3:1 Mobitz II | Survived |
| McGhie et al[11], 2020 | STEMI | Yes | Typical TTS pattern | LV apical ballooning | - | Yes | Coexist | N/A | Survived |
The coexistence of SCAD and TTS is rare and unclear[16]. The occurrence of the two is not coincidental and is mostly related to one another. SCAD was noted in many cases after a careful angiographic review of patients with TTS as the initial diagnosis[17]. SCAD rarely causes acute coronary syndrome and on the contrary, TTS shows ACS-like symptoms with left ventricular wall motion abnormality (LVWMA) without any obstructive lesions[18]. However, according to the recent update in the criteria of International Takotsubo Diagnostic criteria, TTS is diagnosed in patients with pre-existing SCAD. 2.5% of the cases diagnosed with TTS with coronary angiography (CAG) met the criteria for diagnosis of SCAD in a retrospective review.
Common factors which contribute to the development of SCAD include extreme physical activity, drugs, fibro
Interestingly, TTS and SCAD have congruent diagnostic, imaging, and histopathological findings post-ischemia[19]. Patients with TTS and SCAD both report having abnormal electrocardiogram findings initially with either ST elevation, T wave inversion, or both[15,20]. In addition, although the peak values are substantially lower in comparison to acute coronary syndrome, both disorders have elevated troponin levels similar to those in acute coronary syndrome[20]. Of the 20 cases included in the study, 12 were reported with ST elevation and 3 with T wave inversion and 19 of them reported a surge in baseline troponin levels. One of the most crucial diagnostic techniques for recognizing SCAD is invasive CAG which helps distinguish SCAD in three angiographic patterns, type 1 with the presence of a double lumen, type 2 with lumen narrowing, and type 3 with abrupt lumen narrowing mimicking an atherosclerotic lesion[21,22].
Echocardiography is one the most used imaging tool where the regional wall motion abnormalities are assessed that help differentiate between these two conditions[19,20]. The regional LVWMA with a distinctive circumferential pattern is the distinguishing feature of TTS that results in the ballooning of the left ventricle during the systole, besides, the coronary artery supply regions are discordant with the LVWMA in TTS[22]. Left ventricular ballooning can be characterized by an apical, mid-ventricular, basal, or localized pattern in TTS[22]. In SCAD, main lesions are observed in the LAD and its branches rather than the right coronary artery (RCA) or left circumflex artery (LCX)[17]. However, SCAD is argued to not have classical apical ballooning observed in TTS and the wall akinesia corresponds to only the regions supplied by the affected dissected artery which leads to reversible myocardial stunning[5]. This occurs because apical ballooning, a crucial hallmark of TTS, cannot be described by the dissection in LAD as it does not wrap around the cardiac apex instead the diagonal branches, LCX and RCA, correspond to the other locations coexistent in SCAD and TTS[17]. In this review, cardiac imaging revealed apical ballooning and akinesia in 9 cases (45%), and 19 (95%) out of 20 cases, were diagnosed as SCAD on CAG. In a case series by Chou et al[5], several of these patients (particularly those with a long wrap-around LAD artery) with implicated mid to distal LAD artery, SCAD was found to have a large-segmental akinesis comparable to typical TTS (anterolateral, apical, and inferior akinesis/dyskinesis). The authors of the case series determined that the LVWMA in these 9 patients was consistent with the regions supplied by the dissected coronary arteries, and all 9 SCAD cases were misinterpreted as TTS[22].
Furthermore, because both the SCAD and TTS present as ACS, the majority of the SCAD and TTS are treated with a similar treatment of ACS (beta blockers, aspirin, angiotensin-converting enzymes, and/or angiotensin receptor blockers, and diuretics)[5]. Although the idea of using dual platelet therapy is controversial in SCAD, it is continued to be used in concern to the presence of thrombus within the blood vessel[21]. The majority of the lesions found in both SCAD and TTS culminate in ‘restitution and integrum’[15].
The spontaneous resolution of LVWMA in hours to weeks is a defining trait of TTS[23]. In contrast to TTS, where angiographic abnormalities are frequently unchanged from prior investigations, SCAD exhibits acute and dynamic angiographic findings that resolve with time[5]. Interestingly in our review of the cases series, all 20 cases survived and recovered well with only one patient undergoing cardiac intervention and 3 cases reporting complications (case each of occasional ectopic ventricular complexes, Mobitz II AV block, and paroxysmal atrial fibrillation).
Several limitations should be acknowledged when evaluating the results of this systematic review. First, the evidence is based on case reports, which are susceptible to publication bias and may not reflect all patients with SCAD-associated TTS. Second, the quality of reporting in case reports is inconsistent and may not give comprehensive data on patient characteristics, comorbidities, and management. Thirdly, the small number of cases included in this analysis limits the findings' applicability to the larger population of patients with TTS or SCAD. Lack of established diagnostic criteria for SCAD and TTS may have led to misdiagnosis or underreporting of cases. The use of different imaging modalities in different investigations may have influenced the diagnostic precision and the reporting of the findings. In the absence of a control group, it is difficult to demonstrate a causal relation between SCAD and TTS. Further research with larger, more representative samples and established diagnostic criteria is required to confirm the results of this systematic review.
In conclusion, TTS and SCAD have peculiar similarities in clinical presentation, diagnosis, imaging findings, and management, thus, are misdiagnosed often. However, because of similar precipitant factors (physical and emotional stressors), both conditions can even co-exist. The angiographic and echocardiographic findings of SCAD can help differentiate between both conditions if interpreted with the familiarity of SCAD variants. Therefore, to avoid misdiagnosis and underreporting of SCAD, there is a need for further scientific literature to bring awareness and improve uncalled morbidity in the cohort.
Takotsubo syndrome (TTS) and spontaneous coronary artery dissection (SCAD) have similar symptoms and etiologies, but their prognoses and outcomes are distinct. This systematic review examines the presentation, clinical features, comorbidities, investigations, therapy, and outcomes of TTS and SCAD patients.
To examine the presentation, clinical features, comorbidities, investigations, therapy, and outcomes of TTS and SCAD patients.
Our objective is to conduct a systematic review of available case reports on SCAD in order to investigate its potential association with TTS.
SCAD-associated TTS case reports were reviewed after thoroughly screening PubMed, EMBASE, Scopus, and Google Scholar databases till January 2023. Case reports described demographics, comorbidities, imaging, management, and results.
Key findings include: Elderly patients constituted 30% of the sample, with a mean age of 56.2 years. Canada had the most cases (9), followed by the United States (3), Australia (3), and other countries. Emotional stressors were identified in only 5 cases, while physical triggers were observed in 4 cases. Half of the patients experienced chest discomfort, while a quarter were smokers. Over half of the cases (55%) had both TTS and SCAD. All 20 cases recovered and had a favorable prognosis.
This study highlights the coexistence and clinical similarities of TTS and SCAD, therefore emphasizing the importance of further research, awareness as well as comprehensive angiographic testing for effective diagnosis and management.
Further research with larger, more representative samples and established diagnostic criteria is required to confirm the results of this systematic review.
| 1. | Templin C, Ghadri JR, Diekmann J, Napp LC, Bataiosu DR, Jaguszewski M, Cammann VL, Sarcon A, Geyer V, Neumann CA, Seifert B, Hellermann J, Schwyzer M, Eisenhardt K, Jenewein J, Franke J, Katus HA, Burgdorf C, Schunkert H, Moeller C, Thiele H, Bauersachs J, Tschöpe C, Schultheiss HP, Laney CA, Rajan L, Michels G, Pfister R, Ukena C, Böhm M, Erbel R, Cuneo A, Kuck KH, Jacobshagen C, Hasenfuss G, Karakas M, Koenig W, Rottbauer W, Said SM, Braun-Dullaeus RC, Cuculi F, Banning A, Fischer TA, Vasankari T, Airaksinen KE, Fijalkowski M, Rynkiewicz A, Pawlak M, Opolski G, Dworakowski R, MacCarthy P, Kaiser C, Osswald S, Galiuto L, Crea F, Dichtl W, Franz WM, Empen K, Felix SB, Delmas C, Lairez O, Erne P, Bax JJ, Ford I, Ruschitzka F, Prasad A, Lüscher TF. Clinical Features and Outcomes of Takotsubo (Stress) Cardiomyopathy. N Engl J Med. 2015;373:929-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1401] [Cited by in RCA: 1818] [Article Influence: 165.3] [Reference Citation Analysis (1)] |
| 2. | Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J. 2008;155:408-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1193] [Cited by in RCA: 1321] [Article Influence: 73.4] [Reference Citation Analysis (0)] |
| 3. | Lyon AR, Citro R, Schneider B, Morel O, Ghadri JR, Templin C, Omerovic E. Pathophysiology of Takotsubo Syndrome: JACC State-of-the-Art Review. J Am Coll Cardiol. 2021;77:902-921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 235] [Article Influence: 47.0] [Reference Citation Analysis (0)] |
| 4. | Blazak PL, Holland DJ, Basso T, Martin J. Spontaneous coronary artery dissection, fibromuscular dysplasia, and biventricular stress cardiomyopathy: a case report. Eur Heart J Case Rep. 2022;6:ytac125. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 5. | Chou AY, Sedlak T, Aymong E, Sheth T, Starovoytov A, Humphries KH, Mancini GB, Saw J. Spontaneous Coronary Artery Dissection Misdiagnosed as Takotsubo Cardiomyopathy: A Case Series. Can J Cardiol. 2015;31:1073.e5-1073.e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 49] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 6. | Desai AR, Patel P, Patel R, Ghadiam H, Mukhopadhyay E. The Chicken or the Egg? An Interesting Case Presentation of Spontaneous Coronary Artery Dissection Versus Takotsubo Cardiomyopathy. Cureus. 2020;12:e7793. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 7. | Fitouchi S, Di Marco P, Motreff P, Lhoest N. Concomitant presentation of spontaneous coronary artery dissection with Takotsubo syndrome: a case report. Eur Heart J Case Rep. 2022;6:ytac172. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 8. | Frederiksen KP, Søholm H, Havndrup O, Procida K. Case report: spontaneous coronary artery dissection and suspicion of takotsubo cardiomyopathy in a patient presenting with T-wave inversions, severe QTc prolongation, elevated cardiac biomarkers, and apical akinesia. Eur Heart J Case Rep. 2020;4:1-6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 9. | Ghafoor HU, Bose A, El-Meligy A, Hannan J. A case report of recurrent spontaneous coronary artery dissection and Takotsubo cardiomyopathy: a treatment dilemma. Eur Heart J Case Rep. 2020;4:1-6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Johnson SW, Hedgire SS, Scott NS, Natarajan P. Spontaneous coronary artery dissection masquerading as Takotsubo cardiomyopathy: a case report. Eur Heart J Case Rep. 2018;2:yty102. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | McGhie D, Moss S, Elder A. 433 A Case of Concurrent Takostubo Cardiomyopathy and Spontaneous Coronary Artery Dissection. Heart Lung Circ. 2020;29:S233. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 12. | Sugito S, Yao Y, Ray M, Al-Omary M, O'Connor S. 064 A Case Report of Concurrent Spontaneous Coronary Artery Dissection and Takotsubo’s Cardiomyopathy. Heart Lung Circ. 2020;29:S66. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 13. | Takeuchi M, Okada T, Ikegami Y, Nakamoto Y, Idei N, Ohashi N. A breastfeeding woman with spontaneous coronary artery dissection and possible takotsubo syndrome: A case report. Medicine (Baltimore). 2021;100:e25775. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Y-Hassan S, Böhm F. The causal link between spontaneous coronary artery dissection and takotsubo syndrome: A case presented with both conditions. Int J Cardiol. 2016;203:828-831. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 15. | Y-Hassan S, Henareh L. Fibrinolysis-treated myocardial infarction in a patient with missed spontaneous coronary artery dissection associated with takotsubo syndrome: case report. Eur Heart J Case Rep. 2018;2:yty145. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 16. | Duran JM, Naderi S, Vidula M, Michalak N, Chi G, Lindsay M, Ghoshhajra B, Gibson CM, Wood MJ. Spontaneous coronary artery dissection and its association with takotsubo syndrome: Novel insights from a tertiary center registry. Catheter Cardiovasc Interv. 2020;95:485-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 17. | Kegai S, Sato K, Goto K, Ozawa T, Kimura T, Kobayashi K, Kikuta Y, Taniguchi M, Hiramatsu S, Takebayashi H, Haruta S. Coexistence of Spontaneous Coronary Artery Dissection, Takotsubo Cardiomyopathy, and Myocardial Bridge. JACC Case Rep. 2021;3:250-254. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Scantlebury DC, Prasad A. Diagnosis of Takotsubo cardiomyopathy. Circ J. 2014;78:2129-2139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 196] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 19. | Buccheri D, Zambelli G. The link between spontaneous coronary artery dissection and takotsubo cardiomyopathy: analysis of the published cases. J Thorac Dis. 2017;9:5489-5492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 20. | Ghadri JR, Wittstein IS, Prasad A, Sharkey S, Dote K, Akashi YJ, Cammann VL, Crea F, Galiuto L, Desmet W, Yoshida T, Manfredini R, Eitel I, Kosuge M, Nef HM, Deshmukh A, Lerman A, Bossone E, Citro R, Ueyama T, Corrado D, Kurisu S, Ruschitzka F, Winchester D, Lyon AR, Omerovic E, Bax JJ, Meimoun P, Tarantini G, Rihal C, Y-Hassan S, Migliore F, Horowitz JD, Shimokawa H, Lüscher TF, Templin C. International Expert Consensus Document on Takotsubo Syndrome (Part II): Diagnostic Workup, Outcome, and Management. Eur Heart J. 2018;39:2047-2062. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 506] [Cited by in RCA: 617] [Article Influence: 77.1] [Reference Citation Analysis (1)] |
| 21. | Garcia-Guimarães M, Bastante T, Antuña P, Jimenez C, de la Cuerda F, Cuesta J, Rivero F, Premawardhana D, Adlam D, Alfonso F. Spontaneous Coronary Artery Dissection: Mechanisms, Diagnosis and Management. Eur Cardiol. 2020;15:1-8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 22. | Y-Hassan S, Abdula G, Böhm F. Recurrent Spontaneous Coronary Artery Dissection: Association with Takotsubo Syndrome and Fibromuscular Dysplasia; Comprehensive Review. RCM. 2022;23. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 23. | Y-Hassan S, Tornvall P. Epidemiology, pathogenesis, and management of takotsubo syndrome. Clin Auton Res. 2018;28:53-65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 101] [Cited by in RCA: 159] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Buccheri D, Italy; Maslennikov R, Russia S-Editor: Liu JH L-Editor: A P-Editor: Xu ZH