Published online Sep 26, 2022. doi: 10.4330/wjc.v14.i9.473
Peer-review started: March 25, 2022
First decision: May 31, 2022
Revised: June 16, 2022
Accepted: July 27, 2022
Article in press: July 27, 2022
Published online: September 26, 2022
Processing time: 179 Days and 3.9 Hours
There are rising numbers of patients who have heart failure with preserved ejection fraction (HFpEF). Poorly understood pathophysiology of heart failure with preserved and reduced ejection fraction and due to a sparsity of studies, the management of HFpEF is challenging.
To determine the hospital readmission rate within 30 d of acute or acute on chronic heart failure with preserved ejection fraction and its effect on mortality and burden on health care in the United States.
We performed a retrospective study using the Agency for Health-care Research and Quality Health-care Cost and Utilization Project, Nationwide Readmissions Database for the year 2017. We collected data on hospital readmissions of 60514 adults hospitalized for acute or acute on chronic HFpEF. The primary outcome was the rate of all-cause readmission within 30 d of discharge. Secondary out
The thirty day readmission rate was 21%. Approximately 9.17% of readmissions were in the setting of acute on chronic diastolic heart failure. Hypertensive chronic kidney disease with heart failure (1245; 9.7%) was the most common readmission diagnosis. Readmitted patients had higher in-hospital mortality (7.9% vs 2.9%, P = 0.000). Our study showed that Medicaid insurance, higher Charlson co-morbidity score, patient admitted to a teaching hospital and longer hospital stay were significant variables associated with higher readmission rates. Lower readmission rate was found in residents of small metropolitan or micropolitan areas, older age, female gender, and private insurance or no insurance were associated with lower risk of readmission.
We found that patients hospitalized for acute or acute on chronic HFpEF, the thirty day readmission rate was 21%. Readmission cases had a higher mortality rate and increased healthcare resource utilization. The most common cause of readmission was cardio-renal syndrome.
Core Tip: Our study highlights the current trend in heart failure with preserved ejection fraction (HFpEF) readmissions, and important causes and predictors of readmissions. It also highlights that mortality in readmission is greater compared to index admissions. The economic burden of HFpEF is also highlighted.
- Citation: Jha AK, Ojha CP, Krishnan AM, Paul TK. Thirty-day readmission in patients with heart failure with preserved ejection fraction: Insights from the nationwide readmission database. World J Cardiol 2022; 14(9): 473-482
- URL: https://www.wjgnet.com/1949-8462/full/v14/i9/473.htm
- DOI: https://dx.doi.org/10.4330/wjc.v14.i9.473
The prevalence of heart failure (HF) is constantly increasing over time. Approximately 6.2 million adults ≥ 20 years of age were diagnosed with HF between 2013 and 2016 in the United States, which was lower than that in 2009 to 2012 with an estimated 5.7 million diagnosed with HF[1]. Heart failure with preserved ejection fraction (HFpEF) is a clinical syndrome with patients having signs and symptoms of HF with normal or near normal left ventricle (LV) ejection fraction as a result of high LV filling pressure[2,3]. Among HF hospitalizations, approximately half are characterized by HFpEF[4]. The prevalence of HFpEF compared to HF with reduced ejection fraction, seems to be going up due to the increasing elderly population.
The total cost associated with HF treatment for 2012 was $30.7 billion. According to Medicare, from 2009 to 2012 the median risk-standardized 30-d readmission rate for HF was 23.0%[1,5]. Readmissions receive greater attention from researchers and policy makers as they are recognized as being related to deficient medical care and a preventable cause of higher healthcare expenditure. The Affordable Care Act introduced a financial penalty for higher readmissions for hospitals that are capped at 3% of a hospital’s total Medicare payments for 2015 and beyond. Previously, Medicare’s diagnosis-related group payment system lacked a financial disincentive to reduce readmissions[6]. The Centers for Medicare and Medicaid Services’ (CMS) Hospital Readmission Reduction Program currently only assesses risk-adjusted 30-d readmission rates for HF, acute myocardial infarctions, pneumonia, chronic obstructive pulmonary disease, and elective total knee and hip arthroplasty[7].
The objective of our study was to use the Healthcare Cost and Utilization Project (HCUP), Nationwide Readmission Database (NRD) 2017 to assess HFpEF readmission rate, compare mortality rate between the index hospitalization and readmissions, assess etiologies, and determine predictors of HFpEF readmissions to recognize areas of improvement and implement the targeted interventions.
We performed a retrospective analysis of the NRD database of 2017. Our study populations were derived from the HCUP NRD database. The NRD database is sponsored by the agency for healthcare research and quality. It is an administrative database which records de-identified admission data to acute care hospitals during that specific year. The NRD includes discharges for patients with and without repeat hospital visits in a year and those who have died in the hospital.
In 2017, approximately eighteen million discharges were recorded from 2454 participating hospitals. Variable “NRD_visitlink” was used to identify the patients and the time between the two admissions was obtained by subtracting the variable “NRD_DaysToEvent.” Subtracting length of stay of index admissions from time between two admissions provided the interval time to readmission. Index hospitalizations were studied between January to November to facilitate identification of 30-d readmission rates for all discharged patients for the 2017 calendar year. During this specified period, index hospitalizations were defined as non-elective admission with a primary International Classification of Diseases and Related Health Problems (ICD)-10 diagnosis code of acute diastolic heart failure/HFpEF, (I5031) or acute on chronic HFpEF (I5033). Index hospitalizations were excluded if: (1) The patients were younger than 18 years; (2) the patient died during the index hospitalization; and (3) there was no information on the length of stay (LOS).
We extracted baseline patient characteristics such as age, discharge destination, sex, primary expected payer, and median household income from the NRD database. The Charlson comorbidity index was used to determine the effect of chronic comorbidities in patients on primary and secondary outcomes[8]. Hospital-level variables included bed size, rural/urban location, and teaching status. Discharge to a rehabilitation facility was also obtained.
The primary outcome was defined as any non-elective, non-traumatic readmission that occurred within the first 30 d of discharge from the index hospitalization. For index hospitalizations with more than one readmission within 30 d, only the first readmission was included.
Secondary outcomes were: (1) In-hospital mortality rate for index admissions; (2) 30-day mortality rate for index admissions; (3) ten most common principal diagnoses for readmission; (4) in-hospital mortality rate during readmissions; (5) resource utilization due to readmission: LOS, total hospitalizations cost and charges; and (6) independent risk factors for admissions.
For the in-patient mortality rate, we used the patient’s recorded vitals at discharge which are directly coded in the NRD database. The thirty-day mortality was calculated by following the patient’s vital status at discharge after any readmission within 30-d of index admission.
Total hospitalization charge is the amount that hospitals billed for the entire hospital stay but not equal to the actual cost of care. The HCUP provides hospital-specific cost to charge ratios based on all-payer inpatient cost. We used this information to calculate total cost of hospitalization by multiplying total hospitalization charges by the cost to charge ratio.
We obtained the ten most common reasons for readmission by tallying the principal diagnosis for each readmission. Independent risk factors for readmission were identified using Cox regression analysis. The statistical analyses were performed using STATA statistical software (StataCorp LLC, College Station, TX 77845, United States). P values < 0.005 was considered statistically significant.
The study included 60514 adult patients with acute and acute on chronic HFpEF admitted between January to November in 2017, of which 61.1% of patients were female. The mean age was 74.8 years. About 59.4% patients had a Charlson comorbidity index greater than three. The majority of patients came from large metropolitan areas [46%] and had Medicare insurance (82.4%). The number of patients discharged to rehabilitation facilities was minimal [0.098%]. Teaching hospitals had a comparatively higher admission rate of 58.9% compared to non-teaching hospitals. Table 1 summarizes details of patient and hospital level characteristics of index admission.
| Variable | n (%) |
| Total number of index admissions | 60514 |
| Female | 37156 (61.4) |
| Mean age in year (Confidence interval) | 74.8 (74.52-75.1) |
| Charlson comorbidity index score | |
| 0 | 0 |
| 1 | 8956 (14.8) |
| 2 | 15613 (25.8) |
| ≥ 3 | 35945 (59.4) |
| Median income in patient zip code, US dollars | |
| 1-43999 | 16823 (27.8) |
| 44000-55999 | 18275 (30.2) |
| 56000-73999 | 15007 (24.8) |
| 74000+ | 10408 (17.2) |
| Patient residence | |
| Large metropolitan areas with at least 1 million residents | 27836 (46.0) |
| Small metropolitan areas with less than 1 million residents | 22753 (37.6) |
| Micropolitan areas 18493 (9.1) | 7201 (11.9) |
| Not metropolitan or micropolitan (non-urban residents) | 2723 (4.5) |
| Insurance type | |
| Medicare | 49864 (82.4) |
| Medicaid | 4054 (6.7) |
| Private | 5809 (9.6) |
| Self-pay | 726 (1.2) |
| Rehab transfer | 59 (0.098) |
| Hospital teaching status | |
| Non-teaching | 24871 (41.1) |
| Teaching | 35643 (58.9) |
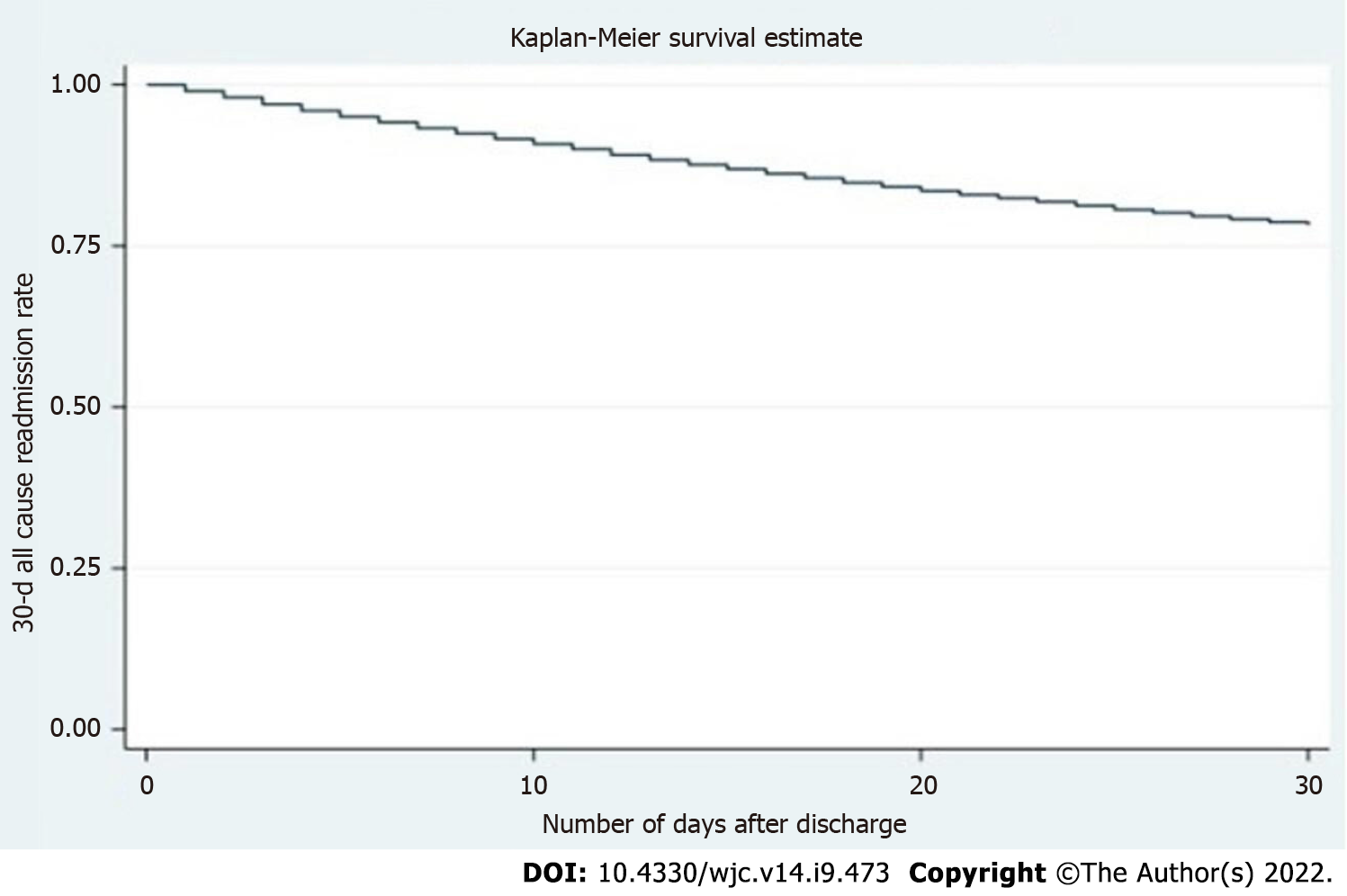
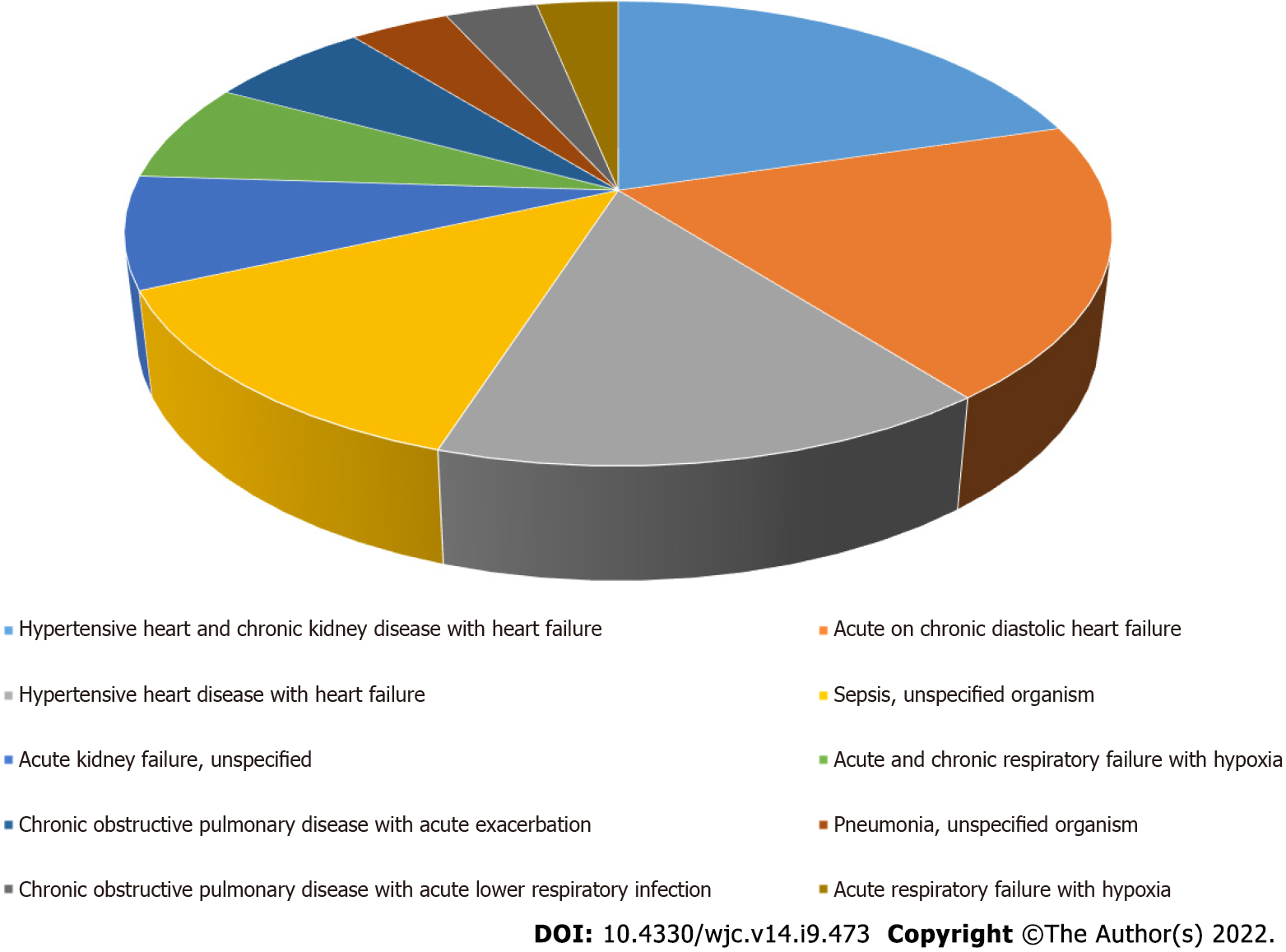
The 30-d rate of readmission was 21%. Only 1175 (9.17%) of readmissions were associated with an admitting diagnosis of acute on chronic HFpEF. Figure 1 shows the Kaplan-Meier survival curve, which showed the total time at risk was 850749 d, with the initial readmission occurring at day one and the last readmission at day twenty-eight. Hypertensive chronic kidney disease with HF (1245; 9.7%) was the most common diagnosis at readmission. Figure 2 shows the ten most common etiologies of readmission. Readmissions showed higher in-hospital mortality compared to index admissions (7.9% vs 2.9%, P = 0.000).
Readmission was associated with a total of 81997 hospital days. Total inpatient healthcare-related financial burden was $206 million in costs and $779 million in charges. Statistically significant predictors of higher rate of 30-d readmission were, higher Charlson comorbidity index (CCI) (1.08, 1.06–1.09, P = 0.000), Medicaid insurance (1.15, 1.05-1.27, P = 0.004), longer LOS in the hospital (1.01, 1.01-1.02, P = 0.000) and teaching hospital admissions (1.09, 1.04-1.15, P = 0.001). Lower readmission risk was associated with female gender (0.91, 0.86-0.95, P = 0.000), elderly patients (0.99, 0.993–0.997, P = 0.000), patients from a micropolitan area (0.83, 0.77-0.90, P = 0.000) or small metropolitan area (0.91, 0.86-0.97, P = 0.003), private insurance (0.85, 0.77-0.93, P = 0.000) or self-paying patients (0.70, 0.53-0.93, P = 0.015). Interestingly, discharges to rehabilitation did not have a significant effect on re-admission rate (0.67, 0.28-1.6, P = 0.381). Table 2 displays the independent predictors of 30-d readmission.
| Variable | Adjusted OR (95%CI) | P value |
| Age | 0.99 (0.99-0.99) | < 0.001 |
| Female gender | 0.91 (0.86-0.95) | < 0.001 |
| Insurance provider (compared to medicare) | ||
| Medicaid | 1.15 (1.05-1.27) | 0.004 |
| Private | 0.85 (0.77-0.93) | < 0.001 |
| Self-pay | 0.70 (0.53-0.93) | 0.015 |
| Charlson comorbidity index score | 1.08 (1.06-1.09) | < 0.001 |
| Patients admitted to teaching hospital | 1.09 (1.04-1.15) | 0.001 |
| Length of stay | 1.01 (1.01-1.01) | < 0.001 |
| Geographic area (compared to large metropolitan area with at least 1 million residents) | ||
| Small (area with < 1 million residents) | 0.91 (0.86-0.97) | 0.003 |
| Micropolitan area | 0.83 (0.77-0.90) | < 0.001 |
| Patients admitted to teaching hospital | 1.09 (1.04-1.15) | 0.001 |
| Length of stay | 1.01 (1.01-1.01) | < 0.001 |
| Geographic area (compared to large metropolitan area with at least 1 million residents) | ||
| Small (area with < 1 million residents) | 0.91 (0.86-0.97) | 0.003 |
| Micropolitan area | 0.83 (0.77-0.90) | < 0.001 |
Mean LOS during index admissions was 5.2 d and 6.4 d during readmission. Readmitted patients had higher LOS (Coefficient 1.15, 95%CI 0.99-1.31, P = 0.000). Total cost of hospitalization was higher for readmitted patients (USD 4831, 95%CI 4251-5410, P = 0.000). Table 3 shows the primary and secondary outcome details.
| Outcome measures | N (%), linearized standard error, 95%CI |
| Readmission rate | 12812 (21%), 357.43, [12111-13513] |
| Mortality | |
| Index cases | 1727 (2.9%), 76.98, [1576-1878] |
| Readmission | 1012 (7.9%), 56.61, [901-1123] |
| Mean length of stay | |
| Index cases | 5.2, 0.05, [5.15-5.32] |
| Readmission | 6.4, 0.9, [6.21-6.56] |
| Total charges (in USD) | |
| Index cases | 40570, 796.7, [39008-42132] |
| Readmission | 60822, 1662.9, [57561-64083] |
| Total cost (in USD) | |
| Index cases | 11234.2, 154.1, [10932-11536] |
| Readmission | 16065, 349.7, [15379-16751] |
Heart failure readmission is one of the major outcomes measured by CMS. Several studies have analyzed the burden of HF to identify the predictors related to readmission[4,9,10]; however, most of these combined HF as a single entity, with only a few studies focusing on HFpEF specific readmission[10]. This study specifically evaluates HFpEF readmission rates and outcomes using the latest NRD database available at the time of study.
The patient population involved was primarily elderly, with a mean age of 74.8 years and predominantly female (61.4%) in line with previous studies[11-13]. Approximately 59.4% of patients had a CCI greater than three. A prior study had shown a mean CCI of 2.9[12]. Another study revealed a higher percentage of patients with CCI>3[14].
The 30-d rate of readmission was 21%, which is comparable to other studies[11,14,15]. A study by Arora et al[11] using the NRD database of 2013 and 2014 showed a readmission rate of 18.5% and this is likely due to the increasing prevalence of HFpEF among the elderly accounting for increased readmission rates.
About 1175 (9.17%) of readmissions were admitted with acute on chronic HFpEF. The most common readmission diagnosis was HF associated with hypertensive chronic kidney disease (1245; 9.7%). Combining all cardiac readmission reasons, our study found approximately 26.3% readmissions were due to cardiac etiologies. A previous study reported higher numbers (approximately 41%-50%) in this category[11]. A study carried out by Goyal et al[14] in 2018 showed a higher percentage of non-cardiac causes of readmission. This significant reduction in cardiac cause as the reason for readmission is encouraging, as it could be due to improvement in treatment modalities for HFpEF. This is despite the fact that there is no established goal directed medical therapy for this condition or use of monitoring modalities such as Cardiomems, which have been proven to reduce readmission rate.
Significant predictors of increased 30-d readmission rate were Medicaid insurance, higher CCI, patient admitted to a teaching hospital and longer LOS in the hospital. Higher CCI is an obvious indicator of high readmission rate as multiple comorbidities are associated with frequent hospitalizations. Previous studies demonstrated that patients with HFpEF are also diagnosed with multiple comorbidities[16,17]. We did not further analyze individual medical conditions associated with HF readmission, although it would be interesting to see how these conditions affect frequent readmission. Teaching hospital patient populations are generally complex and that could explain higher readmissions. Similarly, longer LOS is explained during readmissions as this occurs with sicker patients, consistent with the study by Bergethon et al[18].
Residence in a small metropolitan (or micropolitan area), older age, female sex, and private or no insurance were associated with lower odds of readmission. López-Vilella et al[19] has shown that female gender is associated with a higher number of readmissions when compared to males, independent of the left ventricular ejection fraction (females = 33.5% vs males = 26.8%; P = 0.009). Our study showed lower odds of readmissions in females. The study by Manemann et al[20] revealed that the rural population with HF has an increased risk of death but reduced risk of emergency department visits as well as hospitalizations. Our study has shown residence in a small metropolitan or micropolitan area is a predictor of decreased risk of readmission. This might be due to the decreased or delayed access to health care facilities. Further study in this direction will help identify the gaps in healthcare access in these areas.
Private insurance and no insurance are two extreme ends of the spectrum, and our study showed a lower rate of readmissions with both. The lower rate of readmission could be explained by the fact that the patients with private insurance have good preventive and acute care along with good access to healthcare compared to patients with no insurance. Patients with no insurance may have delayed care and died before hospital readmission.
Interestingly, discharges to rehabilitation facilities had no effect on readmission. There are some contradicting results as per recent studies. Arora et al[4] showed an increased risk of readmission in patients discharged to rehabilitation facilities. The study by Gupta et al[21] showed no effect on readmission rate based on discharge to a hospital-based skilled nursing facility on chronic conditions like congestive heart failure, although this study showed lower readmission rate for acute conditions such as acute myocardial infarction and pneumonia. This study’s results aligned to our study even though currently we do not see many hospital-based skilled nursing facilities compared to free standing skilled nursing facilities. This result could be due to a different patient population which requires discharge to a skilled nursing facility due to their complex medical history. Further research in this regard will certainly help to identify the associated factors.
Our study showed increased in-hospital mortality in readmitted patients when compared to index admission (7.9% vs 2.9%, P = 0.000). Multiple studies have shown readmission cases are associated with increased mortality[22-24]. This seems to be aligned to the predictors of readmissions, as these patients are generally sicker with multiple comorbidities. It would be helpful to analyze the basic characteristics of these patients, which could further highlight mortality related to cardiac vs non cardiac causes.
Mean LOS during index admissions was 5.2 d while it was 6.4 d for readmission. Several studies have shown that increased LOS has a negative effect on readmission rate, with longer index LOS correlating with a higher risk for readmission[24-26]. This finding is similar to our study result, which we hypothesize could be due to sicker patients and those with multiple comorbidities requiring a longer LOS, portending to higher readmission rates.
Total cost of hospitalization was higher for readmitted patients. 81997 hospital d were associated with readmissions. The total economic burden associated with readmissions was $206 million in costs and $779 million in charges. A study by Fingar et al[27] using NRD HCUP databases showed the total economic burden of readmissions for congestive HF patients was approximately $2728 million in 2013. This study did not further differentiate between the cost associated with heart failure with reduced ejection fraction and HFpEF. However, given the increasing prevalence of HFpEF, it is likely that HFpEF will soon, if not already, account for the majority of the economic burden of heart failure and targeted interventions are required to reduce the economic burden while improving patient care by identifying key variables involved.
For patients hospitalized for acute or acute on chronic HFpEF, 30-d readmission rate is comparable to recent studies, although readmissions were associated with higher mortality and resource utilization compared to index admission. Multiple comorbidities were associated with increased risk of readmission. Most readmissions were due to hypertensive chronic kidney disease with heart failure.
Heart failure with preserved ejection fraction is a growing problem with a high risk for readmissions. Highlighting the cause and effect of this condition will further help in preparing guidelines to treat and prevent readmissions.
This study will help to understand important variables associated with readmission risks and burden on the American health care resource utilization.
The main research objective is to identify common hospital and patient related variables of increased or decreased risk of readmission in patients with heart failure with preserved ejection fraction. Identifying these variables can help clinicians as well as researchers to further modify these variables to improve the morbidity as well as financial burden.
This study used the National Readmissions Dataset for 2017 to obtain patients with heart failure with preserved ejection fraction using International Classification of Diseases (ICD) codes-10. This was a retrospective study. Cox regression analysis was used to identify the significant variables on read
This study clearly showed different hospital-related and patient-related variables which increased the risk of readmissions. Also, we found some interesting results showing the variables with decreased risk of readmissions. Some of these results align with recent study results but some others show different results which needs further research to identify new changes in the dynamics of this condition.
Our results show that the rates of readmissions are similar to recent studies which indicate that we have to work harder to reduce this rate. We were able to provide different variables which are easy to modify which can reduce the risk of readmissions. Our study showed discharge to rehabilitation facility has no effect on the rate of readmissions.
Further study on this important topic will be helpful to determine the ongoing change in managing this condition and decreasing its effect both on patients as well as the health care sector.
Our sincere gratitude to Dr. Karen Glatfelter for editing the language in this manuscript.
| 1. | Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Després JP, Fullerton HJ, Howard VJ, Huffman MD, Judd SE, Kissela BM, Lackland DT, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Matchar DB, McGuire DK, Mohler ER 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Willey JZ, Woo D, Yeh RW, Turner MB; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015;131:e29-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3462] [Cited by in RCA: 4563] [Article Influence: 380.3] [Reference Citation Analysis (1)] |
| 2. | Sharma K, Kass DA. Heart failure with preserved ejection fraction: mechanisms, clinical features, and therapies. Circ Res. 2014;115:79-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 387] [Cited by in RCA: 393] [Article Influence: 32.8] [Reference Citation Analysis (0)] |
| 3. | Zile MR, Bourge RC, Bennett TD, Stevenson LW, Cho YK, Adamson PB, Aaron MF, Aranda JM Jr, Abraham WT, Smart FW, Kueffer FJ. Application of implantable hemodynamic monitoring in the management of patients with diastolic heart failure: a subgroup analysis of the COMPASS-HF trial. J Card Fail. 2008;14:816-823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 36] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Arora S, Patel P, Lahewala S, Patel N, Patel NJ, Thakore K, Amin A, Tripathi B, Kumar V, Shah H, Shah M, Panaich S, Deshmukh A, Badheka A, Gidwani U, Gopalan R. Etiologies, Trends, and Predictors of 30-Day Readmission in Patients With Heart Failure. Am J Cardiol. 2017;119:760-769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 103] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 5. | Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Shay CM, Spartano NL, Stokes A, Tirschwell DL, VanWagner LB, Tsao CW; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation. 2020;141:e139-e596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3254] [Cited by in RCA: 5791] [Article Influence: 965.2] [Reference Citation Analysis (2)] |
| 6. | Berenson RA, Paulus RA, Kalman NS. Medicare's readmissions-reduction program--a positive alternative. N Engl J Med. 2012;366:1364-1366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 157] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 7. | Centers for Medicare & Medicaid Services. Readmissions Reduction Program. 2015. Available from: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html. |
| 8. | Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32099] [Cited by in RCA: 39659] [Article Influence: 1016.9] [Reference Citation Analysis (0)] |
| 9. | Dharmarajan K, Hsieh AF, Lin Z, Bueno H, Ross JS, Horwitz LI, Barreto-Filho JA, Kim N, Bernheim SM, Suter LG, Drye EE, Krumholz HM. Diagnoses and Timing of 30-Day Readmissions After Hospitalization for Heart Failure, Acute Myocardial Infarction, or Pneumonia. JAMA. 2013;309:355-363 Available from: http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.2012.216476. |
| 10. | Chamberlain AM, Dunlay SM, Gerber Y, Manemann SM, Jiang R, Weston SA, Roger VL. Burden and Timing of Hospitalizations in Heart Failure: A Community Study. Mayo Clin Proc. 2017;92:184-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 50] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 11. | Arora S, Lahewala S, Hassan Virk HU, Setareh-Shenas S, Patel P, Kumar V, Tripathi B, Shah H, Patel V, Gidwani U, Deshmukh A, Badheka A, Gopalan R. Etiologies, Trends, and Predictors of 30-Day Readmissions in Patients With Diastolic Heart Failure. Am J Cardiol. 2017;120:616-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 12. | Steinberg BA, Zhao X, Heidenreich PA, Peterson ED, Bhatt DL, Cannon CP, Hernandez AF, Fonarow GC; Get With the Guidelines Scientific Advisory Committee and Investigators. Trends in patients hospitalized with heart failure and preserved left ventricular ejection fraction: prevalence, therapies, and outcomes. Circulation. 2012;126:65-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 553] [Cited by in RCA: 667] [Article Influence: 47.6] [Reference Citation Analysis (0)] |
| 13. | Philbin EF, Rocco TA Jr, Lindenmuth NW, Ulrich K, Jenkins PL. Systolic versus diastolic heart failure in community practice: clinical features, outcomes, and the use of angiotensin-converting enzyme inhibitors. Am J Med. 2000;109:605-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 168] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 14. | Goyal P, Loop M, Chen L, Brown TM, Durant RW, Safford MM, Levitan EB. Causes and Temporal Patterns of 30-Day Readmission Among Older Adults Hospitalized With Heart Failure With Preserved or Reduced Ejection Fraction. J Am Heart Assoc. 2018;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 15. | Hogg K, Swedberg K, McMurray J. Heart failure with preserved left ventricular systolic function; epidemiology, clinical characteristics, and prognosis. J Am Coll Cardiol. 2004;43:317-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 578] [Cited by in RCA: 574] [Article Influence: 26.1] [Reference Citation Analysis (7)] |
| 16. | Nanayakkara S, Patel HC, Kaye DM. Hospitalisation in Patients With Heart Failure With Preserved Ejection Fraction. Clin Med Insights Cardiol. 2018;12:1179546817751609. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 17. | Tran RH, Aldemerdash A, Chang P, Sueta CA, Kaufman B, Asafu-Adjei J, Vardeny O, Daubert E, Alburikan KA, Kucharska-Newton AM, Stearns SC, Rodgers JE. Guideline-Directed Medical Therapy and Survival Following Hospitalization in Patients with Heart Failure. Pharmacotherapy. 2018;38:406-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 59] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 18. | Bergethon KE, Ju C, DeVore AD, Hardy NC, Fonarow GC, Yancy CW, Heidenreich PA, Bhatt DL, Peterson ED, Hernandez AF. Trends in 30-Day Readmission Rates for Patients Hospitalized With Heart Failure: Findings From the Get With The Guidelines-Heart Failure Registry. Circ Heart Fail. 2016;9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 123] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 19. | López-Vilella R, Marqués-Sulé E, Laymito Quispe RDP, Sánchez-Lázaro I, Donoso Trenado V, Martínez Dolz L, Almenar Bonet L. The Female Sex Confers Different Prognosis in Heart Failure: Same Mortality but More Readmissions. Front Cardiovasc Med. 2021;8:618398. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 20. | Manemann SM, St Sauver J, Henning-Smith C, Finney Rutten LJ, Chamberlain AM, Fabbri M, Weston SA, Jiang R, Roger VL. Rurality, Death, and Healthcare Utilization in Heart Failure in the Community. J Am Heart Assoc. 2021;10:e018026. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 21. | Gupta S, Zengul FD, Davlyatov GK, Weech-Maldonado R. Reduction in Hospitals' Readmission Rates: Role of Hospital-Based Skilled Nursing Facilities. Inquiry. 2019;56:46958018817994. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Setoguchi S, Stevenson LW, Schneeweiss S. Repeated hospitalizations predict mortality in the community population with heart failure. Am Heart J. 2007;154:260-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 384] [Cited by in RCA: 514] [Article Influence: 27.1] [Reference Citation Analysis (0)] |
| 23. | Fernandez-Gasso L, Hernando-Arizaleta L, Palomar-Rodríguez JA, Abellán-Pérez MV, Pascual-Figal DA. Trends, causes and timing of 30-day readmissions after hospitalization for heart failure: 11-year population-based analysis with linked data. Int J Cardiol. 2017;248:246-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 24. | Fudim M, O'Connor CM, Dunning A, Ambrosy AP, Armstrong PW, Coles A, Ezekowitz JA, Greene SJ, Metra M, Starling RC, Voors AA, Hernandez AF, Michael Felker G, Mentz RJ. Aetiology, timing and clinical predictors of early vs. late readmission following index hospitalization for acute heart failure: insights from ASCEND-HF. Eur J Heart Fail. 2018;20:304-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 25. | Miñana G, Bosch MJ, Núñez E, Mollar A, Santas E, Valero E, García-Blas S, Pellicer M, Bodí V, Chorro FJ, Sanchis J, Núñez J. Length of stay and risk of very early readmission in acute heart failure. Eur J Intern Med. 2017;42:61-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 26. | Khan H, Greene SJ, Fonarow GC, Kalogeropoulos AP, Ambrosy AP, Maggioni AP, Zannad F, Konstam MA, Swedberg K, Yancy CW, Gheorghiade M, Butler J; EVEREST Trial Investigators. Length of hospital stay and 30-day readmission following heart failure hospitalization: insights from the EVEREST trial. Eur J Heart Fail. 2015;17:1022-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 61] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Chen S, China; Kharlamov AN, Netherlands; Pradhan A, India S-Editor: Liu JH L-Editor: Webster JR P-Editor: Liu JH