Published online Dec 26, 2022. doi: 10.4330/wjc.v14.i12.626
Peer-review started: August 13, 2022
First decision: September 5, 2022
Revised: September 11, 2022
Accepted: November 22, 2022
Article in press: November 22, 2022
Published online: December 26, 2022
Processing time: 127 Days and 10.9 Hours
One of the efforts to reduce hypertension rates in the community is through an educational campaign that refers to the NIH's National Heart, Lung, and Blood Institute curricula or abbreviated as NHLBI. However, during the coronavirus disease 2019 (COVID-19) pandemic, one of the hardest hit areas is health promo
To evaluate the impact of the virtual anti-hypertensive educational campaign towards knowledge, attitude, and the practice of hypertension management in the primary care setting during the COVID-19 pandemic.
An online action research with a randomized crossover-controlled trial using a pretest-posttest control group design. The study was conducted in October 2020-April 2021. The population in this study were patients with hypertension who were treated in the Mojo primary health care setting. A purposive sampling technique was done to receive 110 participants using an online questionnaire and invitation letter.
A total of 110 participants were included in the analysis, 55 in the intervention group and 55 in the control group. Following the Virtual Anti-Hypertensive Educational Campaign implementation, the only parameter that showed significant improvement was knowledge and attitude (P < 0.001). There is no significant change in the practice parameters (P = 0.131).
The Virtual Anti-Hypertensive Educational Campaign implementation in our study population seems to be effective to improve knowledge and attitude of participants, nevertheless, this program seems to be ineffective to improve the practice of hypertension management aspect in participants. Future study with longer durations and more comprehensive programs need to be done to scrutinize the clinical impact of this program nationwide.
Core Tip: In the unprecedented times of the coronavirus disease 2019 (COVID-19) pandemic, many offices shut down across the world. Onsite classes and events were postponed and as a result, the educational health campaign has changed dramatically. With the distinctive rise of e-learning, health campaigns can be undertaken remotely by digital platforms. With this sudden shift away from the conventional campaign, in many parts of the globe, some are wondering whether the adoption of virtual learning will continue to persist post-pandemic and how such a shift would impact the perception and transfer of knowledge towards hypertensive patients. To keep the community safe, but still well-informed about the dangers of hypertension and how to build a healthy lifestyle, we decided to create a Virtual Anti-Hypertensive Educational Campaign. The importance of this paper is to evaluate the impact of the Virtual Anti-Hypertensive Educational Campaign towards knowledge, attitude, and the practice of hypertension management in the primary care setting during the COVID-19 pandemic.
- Citation: Andrianto A, Ardiana M, Nugraha RA, Yutha A, Khrisna BPD, Putra TS, Shahab AR, Andrianto H, Kikuko IH, Puspitasari AN, Hajjrin MR. Impact of the virtual anti-hypertensive educational campaign towards knowledge, attitude, and practice of hypertension management during the COVID-19 pandemic. World J Cardiol 2022; 14(12): 626-639
- URL: https://www.wjgnet.com/1949-8462/full/v14/i12/626.htm
- DOI: https://dx.doi.org/10.4330/wjc.v14.i12.626
From early 2020, the world has been living in a state of public health disruption due to the novel coronavirus disease 2019 (COVID-19) pandemic[1]. COVID-19 has added various challenges and changes to human life worldwide, causing an unprecedented impact on human health, lifestyle, and social life, and has affected the local and international economy[2]. In Indonesia, schools and offices have been suspended during the pandemic and many people have been staying at home[3]. Amid the confinement due to the COVID-19 pandemic, offline activities involving large numbers of people were nearly interrupted[4]. Educators are scrambling to adapt to social distancing (self-quarantine) and the durations of quarantine and social isolation are unpredictable[5].
The COVID-19 pandemic also highlights the fact that the lack of health literacy is an underestimated public health problem in Indonesia[6]. The lack of health literacy is linked to the spread of communicable disease and also gives an opportunity to the increased burden of several non-communicable diseases such as hypertension and cardiovascular diseases[7]. There is no doubt that during times of quarantine and social isolation, food accessibility and availability may be affected, which in turn affects diet quality[8]. Levels of physical activity were also negatively affected during self-isolation and quarantine, due to closure of sport facilities and parks, overall movement restrictions have reduced the ability to engage in physical activity[9]. This was accompanied with an increase of sedentary behaviors related to self-isolation and quarantine, including distance learning and telework[10].
Hypertension can be prevented or delayed through mitigation of modifiable risk factors, such as healthier eating, weight loss, and increased physical activity[11]. Efforts to improve population health literacy can bring spectacular benefits in terms of building the populations’ resilience to health threats, promoting healthy lifestyle changes, and empowering individuals to make a well- informed health decision[12]. One of the effective non-pharmacologic strategies to combat hypertension is a dietary campaign[13]. One of the examples of effective diet to combat hypertension is Dietary Approaches to Stop Hypertension (DASH) Diet. DASH diet is one of the flexible and balanced dietary plans that is proven to reduce blood pressure[14]. The DASH eating plan requires no special foods and instead provides daily and weekly nutritional goals. Current evidence showed that a DASH diet could reduce blood pressure within 2 to 4 wk (by 6 mmHg systolic and 3 mmHg diastolic)[15-17]. Unfortunately, the COVID-19 pandemic which locked down policy in Indonesia have disrupted the opportunity for the conventional health education process and has increased the necessity to find alternative health campaign strategies[18].
Therefore, we try to build the anti-hypertensive educational campaign based on the DASH diet. Since the pandemic will undeniably continue to disrupt the conventional health campaign activity, some virtual alternatives are being used to continue health education activities. As we face the prospect of many urban people who have easy access to the internet and social media, we try to assess their feasibility and determine whether they are adequate in getting health education virtually.
Our teams designed a virtual anti-hypertensive educational campaign curriculum for community health care advocates in the community health care of the Mojo District, Surabaya, Indonesia to identify and prevent health risks of hypertension. The first goal is to conduct research on the risks of hypertension and identify an educational model for community health advocates. The second goal is to educate people to improve health literacy in the field of hypertensive healthy plans. The virtual anti-hypertensive educational campaign aims to help dispel misinformation while promoting healthy lifestyle recommendations and medical guidelines set by the Ministry of Health of the Indonesian Government and Indonesian Cardiologist Association. Therefore, the purpose of this paper is to highlight the impact of the virtual anti-hypertensive educational campaign towards knowledge, attitude, and the practice of hypertension management during the COVID-19 pandemic.
In order to conduct the study, approval was obtained on July 1st, 2020 with a decision of the Bioethics Committee at the Faculty of Medicine Universitas Airlangga (Ref. number 532/UN3/2020) under the name of Andrianto as the principal investigator. All participants provided virtual informed consent prior to participating in the study, without identifiable data. The schedule of enrollment, intervention and measurements according to Standard Protocol Items: Recommendations for Intervention Trials requirements. The study’s data were collected in accordance with the Helsinki Declaration. The consent form documented the aims, nature, and procedure of the study. Anonymity and confidentially were strictly maintained.
The trial was a randomized double-blind, placebo controlled, crossover design. The study was completed over a 6 mo duration (1 October 2020-30 April 2021) of the virtual anti-hypertensive educational campaign with randomization (1 mo); treatment period one (2 mo); washout (1 mo); and finally, treatment period two (2 mo). Subjects were randomly assigned among patients with established hypertension using a pre-test, post-test, controlled group design. This study was conducted in October-December 2020 in the Mojo District, Surabaya City. We conducted an online survey from October to December, 2020. The survey involved an online questionnaire that was distributed virtually, either by email or by WhatsApp and social media, to more than 500 hypertensive patients in the Mojo district of Surabaya, Indonesia, of which, 110 participants actively replied. The questionnaire was self-administered without intervention by the authors or any specific person, and it did not contain any identifying data of the participants to ensure confidentiality. Questionnaires with incomplete information or missing data were excluded from the analysis. Completed paper questionnaires were collected anonymously to ensure confidentiality and to prevent any response bias. Unreturned or uncompleted questionnaires were recorded as missing. Participants were not aware of the study aim or outcomes to reduce the risk of any possible bias. The survey included only hypertensive patients who were living in the Mojo district of Surabaya city.
In accordance with the aim of the study, a questionnaire consisting of “knowledge, attitudes, and practices” was prepared using the literature. The questionnaire covered participants’ basic demographic data, such as their sex, age, and marital status, as well as general questions about their financial status, occupation, level of education, internal displacement, history of health problems, psychological illness, and learning disabilities, if present. The questionnaire also addressed their experience with telemedicine, including questions related to sphygmomanometer usage proficiency, type and quality of sphygmomanometer used, daily antihypertensive drugs, and daily diets. We improved the previous questionnaire by conducting it virtually and adapting local wisdom for our hypertensive patients. Items in the questionnaire were then modified and new items were added based on the qualitative data collected in these interviews. We developed the questionnaire in Bahasa and tested its internal consistency in a pilot study comprising 40 subjects. We revised the questionnaire several times to ensure high internal consistency, which was determined by Cronbach's alpha. The sample from the pilot study was not included in the final analysis. We provided the questionnaire in Bahasa to accommodate respondents' native language. After designing the Bahasa version, three independent translators translated the questionnaire separately and compared the three versions to reach a consensus after consultation with a linguistic expert and three authors to ensure the same intended meaning. The “knowledge, attitudes, and practices” questionnaire had a high internal consistency, as evidenced by Cronbach’s alpha values of 0.88 and 0.86 for the Bahasa versions.
The population in this study were all patients with hypertension who were treated in the Mojo primary health care setting or referred by general practitioners in the Mojo district of Surabaya city. Participants included in this study were adults, aged 18 years and older, with a grade I hypertension according to the ESC/ESH 2018 guideline (SBP of 140 to 159 mmHg and DBP of 90 to 99 mmHg) based on the average BP across three screening visits. Persons with a prior diagnosis of coronary heart disease, renal insufficiency, poorly controlled dyslipidemia, diabetes mellitus or heart failure were excluded from participation. Participants who have already taken more than 1 antihypertensive agent or insulin, education level higher than graduate school, subjects with cognitive impairment, and subjects who were unable to join or complete 7 virtual sessions had been excluded. Invitation letters to the study were sent to all subjects who met eligibility criteria.
To detect a blood pressure difference of 10 mmHg (clinically relevant) with 90% power and α = 0.05, 40 patients are needed in crossover design[19]. Silagy et al[20] detected a difference of 10 mmHg with less than 50 patients per group in a parallel trial. We have carried out a pilot cross-over virtual educational campaign study that detected a difference of 10 mmHg units with 40 patients, confirming that cross-over design substantially reduced the sample size required (unpublished results). To account for drop-out or non-compliance, this trial included 55 participants in the intervention group and 55 participants in the control group. Sample size calculation was performed with nQuery 7.0. Purposive sampling techniques were done to receive 110 participants.
After the Indonesian government called for cooperation of its residents to practice social distancing measures, the Department of Cardiology and Vascular Medicine Universitas Airlangga created an approachable Virtual Anti-Hypertensive Educational Campaign using social media and a webinar-based platform to educate hypertensive patients in the Mojo District of Surabaya. The virtual campaign consisted of 7 sessions, between 1 October, 2020 and 30 April, 2021. The virtual campaign was held once a week and the duration of each session was approximately 2 h. The virtual anti-hypertensive educational campaign had been focusing on hypertensive prevention strategy towards society. The curriculum of our virtual anti-hypertensive educational campaign was based on NIH's National Heart, Lung, and Blood Institute curricula, with several improvisations in the usage of Bahasa and virtual content based on local wisdom. The schedule and subjects for the Virtual Anti-Hypertensive Educational Campaign can be seen in (Table 1).
| No. | Sessions | Subjects | Duration |
| 1 | Session 1 | Hypertension awareness campaign, definition and how to measure home blood pressure monitoring, understanding the silent killer of hypertension: dangerous effect towards cardiovascular diseases | 2 h |
| 2 | Session 2 | Healthy lifestyle: focusing on health diet, physical activity, and avoiding stress. Health benefits of the DASH eating plan and why DASH eating plan works | 2 h |
| 3 | Session 3 | Dietary recommendation for hypertension: getting started on DASH (live demo) | 2 h + 2 h of live demo |
| 4 | Session 4 | Tips to reduce salt and sodium intake (live demo: weigh salt before cooking) | 2 h + 2 h of live demo |
| 5 | Session 5 | Meal plans, measure each ingredients and oil products for cooking (live demo) | 2 h + 2 h of live demo |
| 6 | Session 6 | Living with the DASH eating plans. How to choose grains, fruits, vegetables, low fat and non-daily product (live demo) | 2 h + 2 h of live demo |
| 7 | Session 7 | How to educate others about dispelling misinformation in the healthy diet | 2 h |
The intervention and control periods were 2 mo, designed to coincide with the length of the virtual anti-hypertensive educational campaign curricula. The control arm was given a standard medical check and medical treatment without any anti-hypertensive education. Subjects were assigned to the group by random allocation based on block to assign sample numbers equally to each group and assign the block.
The knowledge concerning high blood pressure was measured using a 22-item Hypertension Knowledge Level Scale (HK-LS), from a previous study regarding patient knowledge of hypertension translated into Bahasa Indonesia[21,22].
The attitude towards hypertension was assessed with a 28-item instrument called Treatment Adherence Questionnaire for Patients with Hypertension (TAQPH), using a 4-point Likert-type scale (alpha-reliability = 0.74) in the Bahasa version[23].
Practice was assessed by the 8-item Morisky Medication Adherence Scale (MMAS-8) translated into Bahasa[24].
We used descriptive statistics to examine respondents’ characteristics and responses using frequencies and percentages. We described categorical variables as frequencies and percentages, and continuous variables as mean (SD) or median (lower-upper) values, as appropriate. The Kolmogorov-Smirnov test revealed that several variables did not follow a normal distribution. We conducted independent sample t-tests, paired sample t-tests, Wilcoxon signed rank tests and the Mann-Whitney U-test to identify differences between two groups of continuous variables. The Pearson’s and Spearman’s rank correlation coefficient was used to explore the relationship between knowledge, attitudes, and practice scores in respect to the virtual health education program and the studied variables. We performed all statistical analyses using SPSS version 25.0 (IBM Corp., Armonk, NY, United States).
Selection bias was reduced by ensuring high participation rates and reducing the subject’s loss to follow-up. Interviewer bias was reduced by using standardized questionnaires. The “knowledge, attitudes, and practices” questionnaire had a high internal consistency, as evidenced by Cronbach’s alpha values of 0.88 and 0.86 for the Bahasa versions. The Kaiser-Meyer-Olkin measure of sampling adequacy was 0.78. Bartlett’s test of sphericity was significant (χ2 = 3300.796, df = 231, P < 0.001). The stability of our instrument over time was tested by the test-retest reliability methods. In instances, where clinic records were available, they were utilized for triangulation and to reduce information bias.
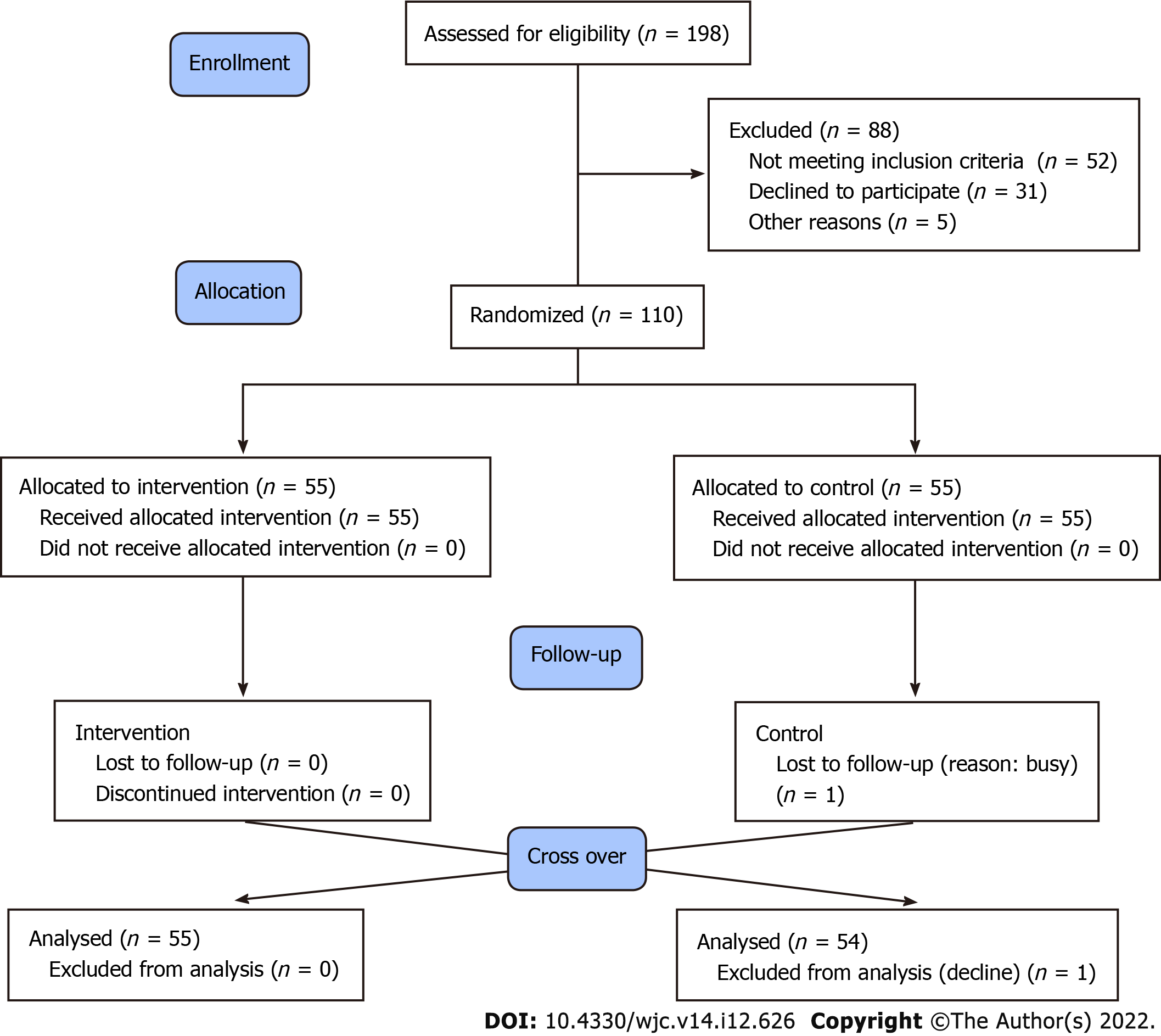
All participants (n = 110) were recruited from the Mojo District, Surabaya City. A total of 110 study participants included in the cross-over study, 55 in the intervention group and 55 in the control group (Figure 1).
The demographic characteristics of participants in (Table 2) are outlined by sex, occupation, age and education level. Patients with hypertension who follow a virtual anti-hypertensive educational campaign at Mojo District, Surabaya City amounted to 41 males (37.27%) and 69 females (62.72%). The number of participants with hypertension who follow the virtual anti-hypertensive educational campaign at Mojo District, Surabaya City with the status of employed (civil servants/police, laborers, traders/entrepreneurs and private employees) was fewer, i.e., 38 people (34.54%) compared with unemployed (unemployed, retired and housewife), i.e., 72 people (65.45%). The average age of hypertensive patients who follow a virtual anti-hypertensive educational campaign at Mojo District, Surabaya City is 54.26 years, with the lowest age being 19 years and the highest age is 77 years. Among them, participants with the lowest level of education were 0 years (not attending school) and the highest level of education was 19 years (magister student). All patients completed the double-blind protocol. Of the 55 participants in the control group who started combined intervention, one interrupted and declined further participation. The age of the 109 remaining participants averaged 45 ± 5 years. Baseline sitting BP was 152 ± 15/93 ± 13 mmHg and the 24-h ambulatory pressure was 149 ± 12/87 ± 10 mmHg.
| Characteristics | Intervention, n = 55 | Control, n = 55 | P value |
| Sex | |||
| Male | 22 (40.0) | 19 (34.5) | 0.23 |
| Female | 33 (60.0) | 36 (65.5) | |
| Age group, yr | |||
| < 20 | 0 | 1 (1.8) | 0.33 |
| 20-29 | 3 (5.4) | 4 (7.2) | |
| 30-39 | 12 (21.8) | 10 (18.2) | |
| 40-49 | 19 (34.5) | 20 (36.4) | |
| 50-59 | 16 (29.1) | 16 (29.1) | |
| 60-69 | 4 (7.2) | 2 (3.6) | |
| > 70 | 1 (1.8) | 2 (3.6) | |
| Marital status | |||
| Single | 2 (3.6) | 1 (1.8) | 0.35 |
| Married | 30 (54.5) | 29 (52.7) | |
| Widowed | 23 (41.8) | 25 (45.4) | |
| Religion | |||
| Muslim | 42 (76.4) | 47 (85.5) | 0.28 |
| Christianity | 9 (16.4) | 5 (9.1) | |
| Others | 4 (7.2) | 3 (5.4) | |
| Educational degree | |||
| Not attending | 4 (7.2) | 4 (7.2) | 0.41 |
| Elementary school | 16 (29.1) | 18 (32.7) | |
| Junior high school | 8 (14.5) | 5 (9.1) | |
| Senior high school | 20 (36.4) | 19 (34.5) | |
| Diploma | 5 (9.1) | 4 (7.2) | |
| Undergraduate | 2 (3.6) | 4 (7.2) | |
| Graduate (magister) | 0 | 1 (1.8) | |
| Occupation | |||
| Civil servants | 2 (3.6) | 3 (5.4) | 0.38 |
| Police | 1 (1.8) | 0 | |
| Laborers | 7 (12.7) | 4 (7.2) | |
| Entrepreneurs | 5 (9.1) | 7 (12.7) | |
| Private workers | 5 (9.1) | 4 (7.2) | |
| Housewives | 25 (45.5) | 29 (52.7) | |
| Retired | 10 (18.2) | 8 (14.5) | |
| Antihypertensive drugs | |||
| ACE-inhibitor | 17 (30.9) | 15 (27.3) | 0.27 |
| ARBs | 2 (3.6) | 1 (1.8) | |
| Beta blocker | 3 (5.4) | 2 (3.6) | |
| CCBs | 31 (56.4) | 29 (52.7) | |
| Diuretics | 2 (3.6) | 8 (14.5) | |
| Baseline systolic BP | 153 ± 15 mmHg | 151 ± 15 mmHg | 0.49 |
| Baseline diastolic BP | 96 ± 13 mm Hg | 91 ± 13 mm Hg | 0.42 |
For each question of knowledge, the distribution of responses from participants is presented in (Table 3). The HK-LS was generated based on content, face, and construct validity, internal consistency, test re-test reliability, and discriminative validity procedures. The final scale had 22 items with six sub-dimensions. The 22-item HK-LS scale was applied to all participants, before and 2 mo after the intervention ended. Following the Virtual Anti-Hypertensive Educational Campaign implementation, there was a significant improvement in the knowledge aspects (P < 0.001) in the intervention group[22].
| No. | Item | Subjects answered true | P value | |
| Before intervention, n = 110 | After intervention, n = 109 | |||
| 1 | Increased diastolic blood pressure also indicates increased blood pressure | 65 (59.1) | 81 (74.3) | < 0.001 |
| 2 | High diastolic or systolic blood pressure indicates increased blood pressure | 71 (64.5) | 84 (77.1) | < 0.001 |
| 3 | Drugs for increased blood pressure must be taken every day | 76 (69.1) | 99 (90.8) | < 0.001 |
| 4 | Individuals with increased blood pressure must take their medication only when they feel ill | 44 (40.0) | 77 (70.6) | < 0.001 |
| 5 | Individuals with increased blood pressure must take their medication throughout their life | 43 (39.1) | 75 (68.8) | < 0.001 |
| 6 | Individuals with increased blood pressure must take their medication in a manner that makes them feel good | 83 (75.5) | 89 (81.6) | 0.042 |
| 7 | If the medication for increased blood pressure can control blood pressure, there is no need to change lifestyles | 99 (90.0) | 103 (94.5) | 0.120 |
| 8 | Increased blood pressure is the result of aging, so treatment is unnecessary | 96 (87.3) | 103 (94.5) | 0.042 |
| 9 | If individuals with increased blood pressure change their lifestyles, there is no need for treatment | 17 (15.5) | 59 (54.1) | < 0.001 |
| 10 | Individuals with increased blood pressure can eat salty foods as long as they take their drugs regularly | 78 (70.9) | 96 (88.1) | < 0.001 |
| 11 | Individuals with increased blood pressure can drink alcoholic beverages | 107 (97.3) | 107 (98.2) | 0.420 |
| 12 | Individuals with increased blood pressure must not smoke | 103 (93.6) | 105 (96.3) | 0.270 |
| 13 | Individuals with increased blood pressure must eat fruits and vegetables frequently | 108 (98.2) | 108 (99.1) | 0.440 |
| 14 | For individuals with increased blood pressure, the best cooking method is frying | 107 (97.3) | 106 (97.2) | 0.490 |
| 15 | For individuals with increased blood pressure, the best cooking method is boiling or grilling | 98 (89.1) | 101 (92.7) | 0.120 |
| 16 | The best type of meat for individuals with increased blood pressure is white meat | 31 (28.2) | 99 (80.7) | < 0.001 |
| 17 | The best type of meat for individuals with increased blood pressure is red meat | 103 (93.6) | 105 (96.3) | 0.270 |
| 18 | Increased blood pressure can cause premature death if left untreated | 46 (41.8) | 91 (83.5) | < 0.001 |
| 19 | Increased blood pressure can cause heart diseases, such as heart attack, if left untreated | 87 (79.1) | 108 (99.1) | < 0.001 |
| 20 | Increased blood pressure can cause strokes, if left untreated | 61 (55.5) | 106 (97.2) | < 0.001 |
| 21 | Increased blood pressure can cause kidney failure, if left untreated | 57 (51.8) | 91 (83.5) | < 0.001 |
| 22 | Increased blood pressure can cause visual disturbances, if left untreated | 39 (35.5) | 59 (54.1) | < 0.001 |
For each question that focused on attitude, the distribution of responses from participants is presented in (Table 4). We used the adapted 28-Likert items instrument of TAQPH instrument, to measure adherence to pharmacological and non-pharmacological treatment (lifestyle), in patients with primary hypertension, before and after the intervention. The adapted TAQPH version had modifications without affecting the instrument’s original structure to maintain the semantic equivalence, a fact validated by its author. An average of a 4-point Likert-type scale were being used to determine the attitude of the subject participants (1 = strongly disagree; 2 = disagree; 3 = agree; 4 = strongly agree). Following the Virtual Anti-Hypertensive Educational Campaign implementation, there was a significant improvement in the knowledge aspects (P < 0 .001) in the intervention group.
| No. | Likert item | Average Likert scale | P value | |
| Before intervention, n = 110 | After intervention, n = 109 | |||
| 1 | Have you taken the medications according to the frequency indicated in the formula provided by the physician? | 38 (34.5) | 61 (55.9) | < 0.001 |
| 2 | Have you taken the medications according to the dosage indicated by the physician? | 82 (74.5) | 87 (79.8) | 0.035 |
| 3 | Have you taken the medications according to the schedule indicated by the physician? | 45 (40.9) | 64 (58.7) | < 0.001 |
| 4 | Have you taken the medications for a long period without interruptions, according to indications provided by the physician? | 32 (29.1) | 35 (32.1) | 0.032 |
| 5 | Have you taken the medications according to indications by the physician, without increasing or diminishing the dosage? | 82 (74.5) | 87 (79.8) | 0.035 |
| 6 | Have you continued taking the medications even if you don’t have symptoms of hypertension? | 38 (34.5) | 61 (55.9) | < 0.001 |
| 7 | Have you forgotten to take your medications? | 72 (65.5) | 49 (44.9) | < 0.001 |
| 8 | Have you suspended the medications when you have felt that symptoms have improved? | 73 (66.4) | 59 (54.1) | < 0.001 |
| 9 | Have kept using the medications in spite of feeling that the symptoms have worsened? | 37 (33.6) | 60 (55.0) | < 0.001 |
| 10 | Have you complied with a low-salt diet? | 32 (29.1) | 81 (74.3) | < 0.001 |
| 11 | Have you complied with a low-fat diet? Reducing consumption of fried preparations, sauces, dressings, sausages (cold cuts - Mortadella - fast foods in general) | 28 (25.5) | 67 (61.5) | < 0.001 |
| 12 | Have you complied with a low-cholesterol diet? Reducing consumption of red meats, chicken skin, eggs, sauces (mayonnaise - tomato sauce - industrial vinaigrettes), oil, lard and butter) | 45 (40.9) | 71 (65.1) | < 0.001 |
| 13 | Have you diminished consumption of sugar and sweets? | 18 (16.4) | 31 (28.4) | < 0.001 |
| 14 | Have you increased consumption of fiber? Such as papaya, pineapple, soursop, peaches, pears, and apples; also cereals, like oats, quinoa and bran | 29 (26.4) | 47 (43.1) | < 0.001 |
| 15 | Have you increased consumption of fresh vegetables? | 71 (64.5) | 89 (81.6) | 0.006 |
| 16 | Have you increased consumption of fresh fruits? | 36 (32.7) | 70 (64.2) | < 0.001 |
| 17 | Have you increased consumption of grains? Including beans, chickpeas, lentils, peas. Besides dry nuts, like peanuts and almonds? | 28 (25.5) | 47 (43.1) | < 0.001 |
| 18 | Have you increased consumption of low-fat dairy products? | 28 (25.5) | 67 (61.5) | < 0.001 |
| 19 | Have you diminished the consumption of coffee? | 63 (57.3) | 70 (64.2) | 0.028 |
| 20 | Have you limited consumption of alcoholic beverages? | 106 (96.4) | 107 (98.2) | 0.440 |
| 21 | Have you stopped smoking? | 13 (11.8) | 28 (25.7) | < 0.001 |
| 22 | Have you performed physical exercise at least five times per week? | 17 (15.5) | 32 (29.4) | < 0.001 |
| 23 | When performing physical exercise, have you dedicated at least 30 min to it? | 12 (10.9) | 25 (22.9) | < 0.001 |
| 24 | Have you been able to control the amount of food you consume? | 63 (57.3) | 68 (62.4) | 0.032 |
| 25 | Have you maintained your body weight under control? | 59 (53.6) | 61 (55.9) | 0.280 |
| 26 | Have you set aside daily time for relaxation for yourself? | 14 (12.7) | 26 (23.8) | < 0.001 |
| 27 | Have you recurred to some forms to relieve stress or tension? | 17 (15.5) | 18 (16.5) | 0.240 |
| 28 | Have you controlled yourself emotionally in light of sudden events? | 51 (46.4) | 59 (54.1) | 0.012 |
For each question of practice, the distribution of responses from participants is presented in (Table 5). Medication adherence was tested using the Bahasa version of the validated MMAS-8. The MMAS-8 is a structured self-report measure of medication-taking behavior that has been widely used in various cultures. Following the virtual anti-hypertensive educational health campaign, no significant change had been observed in the overall practice parameters (P = 0.131).
| No. | Items | Subjects answered “yes” | P value | |
| Before intervention, n = 110 | After intervention, n = 109 | |||
| 1 | Do you sometimes forget to take your hypertensive pills? | 47 (42.7) | 39 (35.8) | 0.160 |
| 2 | People sometimes miss taking their medications for reasons other than forgetting. Thinking over the past two weeks, were there any days when you did not take your hypertensive medicine? | 70 (63.6) | 65 (59.6) | 0.310 |
| 3 | Have you ever cut back or stopped taking your hypertensive medication without telling your doctor, because you felt worse when you took it? | 23 (20.9) | 19 (17.4) | 0.180 |
| 4 | When you travel or leave home, do you sometimes forget to bring along your hypertensive medication? | 49 (44.5) | 47 (43.1) | 0.380 |
| 5 | Did you take your hypertensive medicine yesterday? | 96 (87.3) | 97 (89.0) | 0.430 |
| 6 | When you feel like your hypertension is under control, do you sometimes stop taking your medicine? | 81 (73.6) | 65 (59.6) | < 0.001 |
| 7 | Taking medication every day is a real inconvenience for some people. Do you ever feel hassled about sticking to your hypertensive treatment plan? | 51 (46.4) | 49 (44.9) | 0.390 |
| 8 | How often do you have difficulty remembering to take all your medications? (likert scale: 1 = never; 2 = seldom; 3 = sometime; 4 = frequently) | 3.1 ± 0.8 | 2.3 ± 0.6 | < 0.001 |
This study was conducted and aimed at measuring the baseline level of knowledge, attitude, and practice of hypertension management and perceptions regarding the disease among Indonesian people. The findings reveal the effects of planning virtual health education programs for non-communicable diseases and regarding the change of knowledge, attitude, and practice of hypertension management. Since the outbreak of the COVID-19 pandemic in Surabaya City which started in March 2020, this pandemic led to substantial socioeconomic damages in the whole town. Vigorous measurements have been enforced and implemented including lockdown of Surabaya City and a community quarantine by Surabaya local governments since the outbreak to mitigate the disease effectively. In addition, public health education has been recognized as an effective measure to prevent and control non-communicable diseases.
In managing non-communicable diseases such as hypertension and cardiovascular diseases, there are no better ways than prevention[25]. However, traditional diet campaign may not be the optimal educational strategy during this situation. In our study, the virtual anti-hypertensive educational campaign and various educational interventions augments the health literacy of individuals and found to moderately improve knowledge and attitude towards hypertension, medication and healthy lifestyle. While individuals with hypertension benefited from practical interventions, there is no beneficial effect on practical aspects with the virtual anti-hypertensive educational campaigns. Different from knowledge and attitude aspects, practice of our subjects did not change significantly. Therefore, an effective strategy to improve the practical aspects in hypertension management and to achieve blood pressure goal is mandatory.
Virtual anti-hypertensive educational campaigns alone are unable to increase the individual's practice towards healthy diets and lifestyles, and therefore there may be no tangible benefit to blood pressure reduction. Despite finding heterogeneity in the population of this study, there are a few reasons why practical aspects did not improve significantly following serial interventions. Firstly, conducting only one education session every week may diminish the importance in lifestyle changing. Secondly, in virtual education, subjects are more engaged in the home environment and healthcare professionals find it difficult to accurately assess each individuals lifestyle changes and get immediate feedback. Thirdly, conducting an education session virtually has greater physical and psychological barriers compared with face-to-face education. However, in the pandemic era, online education modalities should be encouraged as improvement was seen in the knowledge and attitude aspects in hypertensive patients who received the virtual anti-hypertensive educational campaigns where barriers to face-to-face education were assessed and addressed.
Dealing with hypertension is a behavior change process which demands serious learning efforts from patients, families and caregivers. Strong organized efforts by multiple stakeholders, including governments, non-government organizations, public and private partnership, and medical workers at all levels, will be key not only to improve health literacy, but also to achieve sustainable strengthening of health systems for a healthier future and well-being for all[26]. While the outbreak is ongoing, staying at home is safe. In many ways, social media and webinar platforms have transformed the practice of cardiovascular preventionists and have opened up new avenues for communicating food and nutrition information. Social media and webinar have also been an effective tool for virtual nutrition counselling, patient education, peer-to-peer support, and public health campaigns[27]. Virtual health education activities should enhance the overall goal of the health promotion and disease prevention program[28].
In a previous study by Oliveira-Filho et al[29], the diagnosis of non-adherent behavior through the use of the new MMAS-8 in patients treated with antihypertensive drugs was a risk factor of elevated systolic and diastolic blood pressure[29]. Considering that non-adherence is a major cause of uncontrolled blood pressure, the use of self-report scales related to BP is a simple and inexpensive measure to assist the clinical treatment of patients with hypertension.
The strengths of the present study include that our population is a crossover experimental study and that the study used strict quality control methods. Also, we have developed an interactive session of virtual education with the aid of a webinar-based platform. Several instructors were involved in observing participants’ focus and concentration. Each session had a 2 h duration, with serial evaluation given at the end of each session. However, some limitations should be acknowledged. First, the nature of our data precludes establishing causal associations between education and CV health. Therefore, we may only discern association. Second, since our virtual anti-hypertensive educational campaign consisted of online self-assessment questionnaires and online education, we cannot guarantee that our population is characterized as real-practice patients, because subjects may not be sincere and may even over-evaluate their own performance. Compared with face-to-face interviews, a virtual self-report has limitations including multiple biases. Third, the study sample was drawn from one district in Surabaya; thus, the findings cannot be generalized to all subjects across the country. Fourth, virtual assessment from population surveys invariably poses the problem of social desirability, whereby study participants are reluctant to admit socially poor acceptable knowledge, attitude, and practice to avoid giving a negative impression.
Despite several limitations, our data clearly indicates a significant improvement of knowledge and attitude, but no significant change in the practice and blood pressure status in the setting of hypertensive patients. In our opinion, these data have important implications for policy making. The general recommendation would be to focus on creating the most effective way to transfer practice and health benefits throughout the virtual education series. Such a strategy should ensure that subjects with hypertension are not disadvantaged with respect to educational background or access to the internet or other opportunities. Accordingly, a virtual healthy educational campaign clearly has to be considered in the strategies of hypertension control and global cardiovascular risk reduction.
The COVID-19 pandemic has created many challenges for healthcare providers to deliver health education to the society, even during the new normal era. Remote and virtual options that align with the WHO’s social distancing guidelines are essential for the continuation of health education. Creating a virtual health education program takes time and does not happen overnight. It requires sources, funding and precise guidelines. It is similar to telemedicine applied to society. The different background of subjects in the society poses a unique challenge to the maintenance of quality of information transmitted to the subjects in these pandemics. It should be remembered that conducting virtual health education programs may be better than doing nothing during this pandemic. This study relied on online questionnaires, suggesting that virtual anti-hypertensive educational campaigns may be effective in transforming knowledge and attitude, yet may not be effective to improve practice of hypertension management in the society. It is concluded that multiple experts from different fields are needed to work together addressing this issue and put their suggestions into practice.
In the unprecedented times of the coronavirus disease 2019 (COVID-19) pandemic, many offices were shut down all across the world. Onsite classes and events were postponed. As a result, the educational health campaign has changed dramatically, with the distinctive rise of e-learning, whereby the health campaign is undertaken remotely by digital platforms. With this sudden shift away from the conventional campaign, in many parts of the globe, some are wondering whether the adoption of virtual learning will continue to persist post-pandemic, and how such a shift would impact the perception and transfer of knowledge towards hypertensive patients. To keep the community safe, but still well-informed about the dangers of hypertension and how to build a healthy lifestyle, we decided to create a Virtual Anti-Hypertensive Educational Campaign.
The importance of this paper is to evaluate the impact of the Virtual Anti-Hypertensive Educational Campaign towards knowledge, attitude, and the practice of hypertension management in the primary care setting during the COVID-19 pandemic.
Our teams designed a virtual anti-hypertensive educational campaign curriculum for community health care advocates in the community health care of the Mojo District, Surabaya, Indonesia to identify and prevent health risks of hypertension. The first goal is to conduct research on the risks of hypertension and identify an educational model for community health advocates. The second goal is to educate people to improve health literacy in the field of hypertensive healthy plans. The virtual anti-hypertensive educational campaign aimed to help dispel misinformation while promoting healthy lifestyle recommendations and medical guidelines set by the Ministry of Health of the Indonesian Government and Indonesian Cardiologist Association. Therefore, the purpose of this paper is to highlight the impact of the virtual anti-hypertensive educational campaign towards knowledge, attitude, and the practice of hypertension management during the COVID-19 pandemic.
The trial was a randomized double-blind, placebo controlled, crossover design. The study was completed over 6 mo duration (1 October 2020-30 April 2021) of the virtual anti-hypertensive educational campaign with randomization (1 mo); treatment period one (2 mo); washout (1 mo); and finally, treatment period two (2 mo). Subjects were randomly assigned among patients with established hypertension using a pre-test post-test-controlled group design. This study was conducted in October-December 2020 in the Mojo District of Surabaya City. We conducted an online survey from October to December 2020. The survey involved an online questionnaire that was distributed virtually, by email or by WhatsApp and social media, to more than 500 hypertensive patients in the Mojo district of Surabaya, Indonesia, to which 110 participants actively replied. The questionnaire was self-administered without intervention by the authors or any specific person, and it did not contain any identifying data of the participants to ensure confidentiality. Questionnaires with incomplete information or missing data were excluded from the analysis. Completed paper questionnaires were collected anonymously to ensure confidentiality and to prevent any response bias. Unreturned or uncompleted questionnaires were recorded as missing. Participants were not aware of the study aim or outcomes to reduce the risk of any possible bias. The survey included only hypertensive patients who were living in the Mojo district of Surabaya city.
A total of 110 participants were included in the analysis, 55 in the intervention group and 55 in the control group. Following the Virtual Anti-Hypertensive Educational Campaign implementation, the only parameter that showed significant improvement were knowledge and attitude (P < 0.001). There is no significant change in the practice parameters (P = 0.131).
The COVID-19 pandemic has created many challenges for healthcare providers to deliver health education to the society, even during the new normal era. Remote and virtual options that align with the WHO’s social distancing guidelines are essential for the continuation of health education. Creating a virtual health education program takes time and does not happen overnight. It requires sources, funding, and precise guidelines. It is like telemedicine applied to society. The different background of subjects in the society poses a unique challenge to the maintenance of quality of information transmitted to the subjects in these pandemics. It should be remembered that conducting virtual health education programs may be better than doing nothing during this pandemic. This study relied on online questionnaires, suggesting that virtual anti-hypertensive educational campaigns may be effective in transforming knowledge and attitude, yet may not be effective to improve the practice of hypertension management in the society. It is concluded that multiple experts from different fields are needed to work together addressing this issue and put their suggestions into practice.
The Department of Cardiology and Vascular Medicine created a virtual education series about healthy lifestyle and dietary guidelines that refers to Dietary Approaches to Stop Hypertension by adapting the local wisdom of the Surabaya community. We aimed to evaluate the impact of the Virtual Anti-Hypertensive Educational Campaign towards knowledge, attitude, and the practice of hypertension management in the primary care setting during the COVID-19 pandemic.
The authors gratefully acknowledge the assistance of Mrs. Fita Triastuti, Mr. Kurniadi Doni and Mrs. Sri Redjeki for the excellent administrative support of the survey. The authors would also like to acknowledge Dr. I Gde Rurus Suryawan and Mrs. Anudya Kartika Ratri for their assistance in verifying the statistical approach used in our study and proof editing. The authors would like to dedicate this manuscript to honor the effort of brave health-care workers who sacrificed their lives to fight against COVID-19.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Indonesian Medical Association; and Indonesian Heart Association.
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: Indonesia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Wondmagegn H, Ethiopia; Zhang JW, China S-Editor: Gong ZM L-Editor: Filipodia P-Editor: Gong ZM
| 1. | Sohrabi C, Alsafi Z, O'Neill N, Khan M, Kerwan A, Al-Jabir A, Iosifidis C, Agha R. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int J Surg. 2020;76:71-76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3213] [Cited by in RCA: 2674] [Article Influence: 445.7] [Reference Citation Analysis (1)] |
| 2. | Ibn-Mohammed T, Mustapha KB, Godsell J, Adamu Z, Babatunde KA, Akintade DD, Acquaye A, Fujii H, Ndiaye MM, Yamoah FA, Koh SCL. A critical analysis of the impacts of COVID-19 on the global economy and ecosystems and opportunities for circular economy strategies. Resour Conserv Recycl. 2021;164:105169. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 406] [Cited by in RCA: 214] [Article Influence: 42.8] [Reference Citation Analysis (0)] |
| 3. | Abidah A, Hidaayatullaah HN, Simamora RM, Fehabutar D, Mutakinati L. The Impact of Covid-19 to Indonesian Education and Its Relation to the Philosophy of “Merdeka Belajar. Stud Philos Sci Educ. 2020;1: 38-49. [RCA] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 4. | Bozkurt A, Jung I, Xiao J, Vladimirschi V, Schuwer R, Egorov G, Lambert SR, Al-Freih M, Pete J, Olcott Jr. D, Rodes V, Aranciaga I, Bali M, Alvarez Jr. AV, Roberts J, Pazurek A, Raffaghelli JE, Panagiotou N, de Coëtlogon P, Shahadu S, Brown M, Asino TI, Tumwesige J, Ramirez Reyes T, Barrios Ipenza E, Ossiannilsson E, Bond M, Belhamel K, Irvine V, Sharma RC, Adam T, Janssen B, Sklyarova T, Olcott N, Ambrosino A, Lazou C, Mocquet B, Mano M, Paskevicius M. A global outlook to the interruption of education due to COVID-19 Pandemic: Navigating in a time of uncertainty and crisis. Asian J Distance Educ. 2020;15:1-126. [DOI] [Full Text] |
| 5. | Hwang TJ, Rabheru K, Peisah C, Reichman W, Ikeda M. Loneliness and social isolation during the COVID-19 pandemic. Int Psychogeriatr. 2020;32:1217-1220. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 706] [Cited by in RCA: 568] [Article Influence: 94.7] [Reference Citation Analysis (0)] |
| 6. | Ifroh RH, Asrianti T. Health Literacy, Media Exposure and Behavior Among Young Adults During the Covid-19 Pandemic. J Ilmu Kesehat Masy. 2020;11:223-236. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Miranda JJ, Kinra S, Casas JP, Davey Smith G, Ebrahim S. Non-communicable diseases in low- and middle-income countries: context, determinants and health policy. Trop Med Int Health. 2008;13:1225-1234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 259] [Cited by in RCA: 254] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 8. | Cheikh Ismail L, Osaili TM, Mohamad MN, Al Marzouqi A, Jarrar AH, Abu Jamous DO, Magriplis E, Ali HI, Al Sabbah H, Hasan H, AlMarzooqi LMR, Stojanovska L, Hashim M, Shaker Obaid RR, Saleh ST, Al Dhaheri AS. Eating Habits and Lifestyle during COVID-19 Lockdown in the United Arab Emirates: A Cross-Sectional Study. Nutrients. 2020;12:3314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 152] [Cited by in RCA: 151] [Article Influence: 25.2] [Reference Citation Analysis (0)] |
| 9. | Dunton GF, Do B, Wang SD. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health. 2020;20:1351. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 603] [Cited by in RCA: 517] [Article Influence: 86.2] [Reference Citation Analysis (0)] |
| 10. | Ricci F, Izzicupo P, Moscucci F, Sciomer S, Maffei S, Di Baldassarre A, Mattioli AV, Gallina S. Recommendations for Physical Inactivity and Sedentary Behavior During the Coronavirus Disease (COVID-19) Pandemic. Front Public Health. 2020;8:199. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 90] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 11. | Campbell NR, Niebylski ML; World Hypertension League Executive. Prevention and control of hypertension: developing a global agenda. Curr Opin Cardiol. 2014;29:324-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 12. | Miranda R, Meeks KAC, Snijder MB, van den Born BJ, Fransen MP, Peters RJ, Stronks K, Agyemang C. Health literacy and hypertension outcomes in a multi-ethnic population: the HELIUS study. Eur J Public Health. 2020;30:545-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Ozemek C, Laddu DR, Arena R, Lavie CJ. The role of diet for prevention and management of hypertension. Curr Opin Cardiol. 2018;33:388-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 102] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 14. | Svetkey LP, Sacks FM, Obarzanek E, Vollmer WM, Appel LJ, Lin PH, Karanja NM, Harsha DW, Bray GA, Aickin M, Proschan MA, Windhauser MM, Swain JF, McCarron PB, Rhodes DG, Laws RL. The DASH Diet, Sodium Intake and Blood Pressure Trial (DASH-sodium): rationale and design. DASH-Sodium Collaborative Research Group. J Am Diet Assoc. 1999;99:S96-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 147] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 15. | Hollenberg NK. Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet: Editor’s comments. Curr Hypertens Rep. 2001;3:373. [DOI] [Full Text] |
| 16. | Saneei P, Salehi-Abargouei A, Esmaillzadeh A, Azadbakht L. Influence of Dietary Approaches to Stop Hypertension (DASH) diet on blood pressure: a systematic review and meta-analysis on randomized controlled trials. Nutr Metab Cardiovasc Dis. 2014;24:1253-1261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 280] [Cited by in RCA: 248] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 17. | Juraschek SP, Woodward M, Sacks FM, Carey VJ, Miller ER 3rd, Appel LJ. Time Course of Change in Blood Pressure From Sodium Reduction and the DASH Diet. Hypertension. 2017;70:923-929. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 18. | Alsoufi A, Alsuyihili A, Msherghi A, Elhadi A, Atiyah H, Ashini A, Ashwieb A, Ghula M, Ben Hasan H, Abudabuos S, Alameen H, Abokhdhir T, Anaiba M, Nagib T, Shuwayyah A, Benothman R, Arrefae G, Alkhwayildi A, Alhadi A, Zaid A, Elhadi M. Impact of the COVID-19 pandemic on medical education: Medical students' knowledge, attitudes, and practices regarding electronic learning. PLoS One. 2020;15:e0242905. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 360] [Cited by in RCA: 334] [Article Influence: 55.7] [Reference Citation Analysis (0)] |
| 19. | Kasiulevičius V, Šapoka V, Filipavičiūtė R. Sample size calculation in epidemiological studies. Gerontologija. 2006;7:225-231. |
| 20. | Silagy CA, McNeil JJ, McGrath BP. Sample size requirements for clinical trials of isolated systolic hypertension. Clin Exp Pharmacol Physiol. 1992;19:294-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 21. | Erkoc SB, Isikli B, Metintas S, Kalyoncu C. Hypertension Knowledge-Level Scale (HK-LS): a study on development, validity and reliability. Int J Environ Res Public Health. 2012;9:1018-1029. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 83] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 22. | Archirel P, Bergès J, Houée-Lévin C. Radical Cations of the Monomer and van der Waals Dimer of a Methionine Residue as Prototypes of (2 Center-3 Electron) SN and SS Bonds. Molecular Simulations of Their Absorption Spectra in Water. J Phys Chem B. 2016;120:9875-9886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 23. | Esquivel Garzón N, Díaz Heredia LP. Validity and Reliability of the Treatment Adherence Questionnaire for Patients with Hypertension. Invest Educ Enferm. 2019;37:e09. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Okello S, Nasasira B, Muiru AN, Muyingo A. Validity and Reliability of a Self-Reported Measure of Antihypertensive Medication Adherence in Uganda. PLoS One. 2016;11:e0158499. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 47] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 25. | Budreviciute A, Damiati S, Sabir DK, Onder K, Schuller-Goetzburg P, Plakys G, Katileviciute A, Khoja S, Kodzius R. Management and Prevention Strategies for Non-communicable Diseases (NCDs) and Their Risk Factors. Front Public Health. 2020;8:574111. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 204] [Cited by in RCA: 421] [Article Influence: 70.2] [Reference Citation Analysis (0)] |
| 26. | Laar AK, Adler AJ, Kotoh AM, Legido-Quigley H, Lange IL, Perel P, Lamptey P. Health system challenges to hypertension and related non-communicable diseases prevention and treatment: perspectives from Ghanaian stakeholders. BMC Health Serv Res. 2019;19:693. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 43] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 27. | Helm J, Jones RM. Practice Paper of the Academy of Nutrition and Dietetics: Social Media and the Dietetics Practitioner: Opportunities, Challenges, and Best Practices. J Acad Nutr Diet. 2016;116:1825-1835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 53] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 28. | Aung MN, Yuasa M, Koyanagi Y, Aung TNN, Moolphate S, Matsumoto H, Yoshioka T. Sustainable health promotion for the seniors during COVID-19 outbreak: a lesson from Tokyo. J Infect Dev Ctries. 2020;14:328-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 29. | Oliveira-Filho AD, Barreto-Filho JA, Neves SJ, Lyra Junior DP. Association between the 8-item Morisky Medication Adherence Scale (MMAS-8) and blood pressure control. Arq Bras Cardiol. 2012;99:649-658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 81] [Article Influence: 5.8] [Reference Citation Analysis (0)] |