Published online Sep 26, 2021. doi: 10.4330/wjc.v13.i9.446
Peer-review started: March 4, 2021
First decision: June 7, 2021
Revised: June 9, 2021
Accepted: July 29, 2021
Article in press: July 29, 2021
Published online: September 26, 2021
Processing time: 197 Days and 16.5 Hours
Coronary artery aneurysm (CAA) is a clinical entity defined by a focal enlargement of the coronary artery exceeding the 1.5-fold diameter of the adjacent normal segment. Atherosclerosis is the main cause in adults and Kawasaki disease in children. CAA is a silent progressive disorder incidentally detected by coronary angiography, but it may end with fatal complications such as rupture, compre
Core Tip: Most patients with coronary artery aneurysm remain asymptomatic until the development of complications or the occurrence of obstructive coronary disease-related clinical manifestations. The underlying pathophysiology is miscellaneous. The ideal management of coronary artery aneurysm has not yet been defined, but computed tomography angiography is the recommended non-invasive test for long-term follow-up. Future prospective comparative trials targeted to define the appropriate strategy and the optimal time to intervene are required.
- Citation: Matta AG, Yaacoub N, Nader V, Moussallem N, Carrie D, Roncalli J. Coronary artery aneurysm: A review. World J Cardiol 2021; 13(9): 446-455
- URL: https://www.wjgnet.com/1949-8462/full/v13/i9/446.htm
- DOI: https://dx.doi.org/10.4330/wjc.v13.i9.446
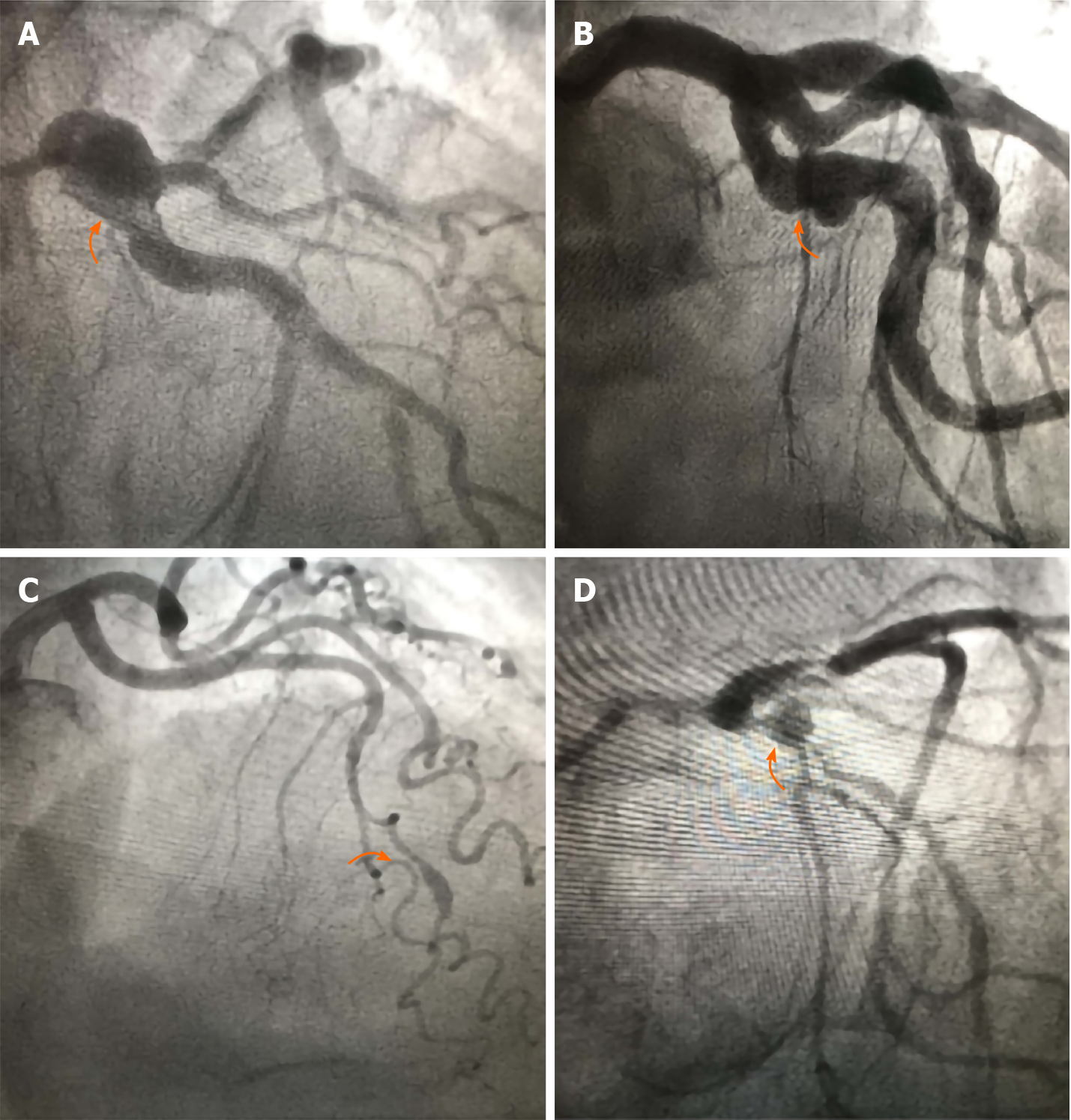
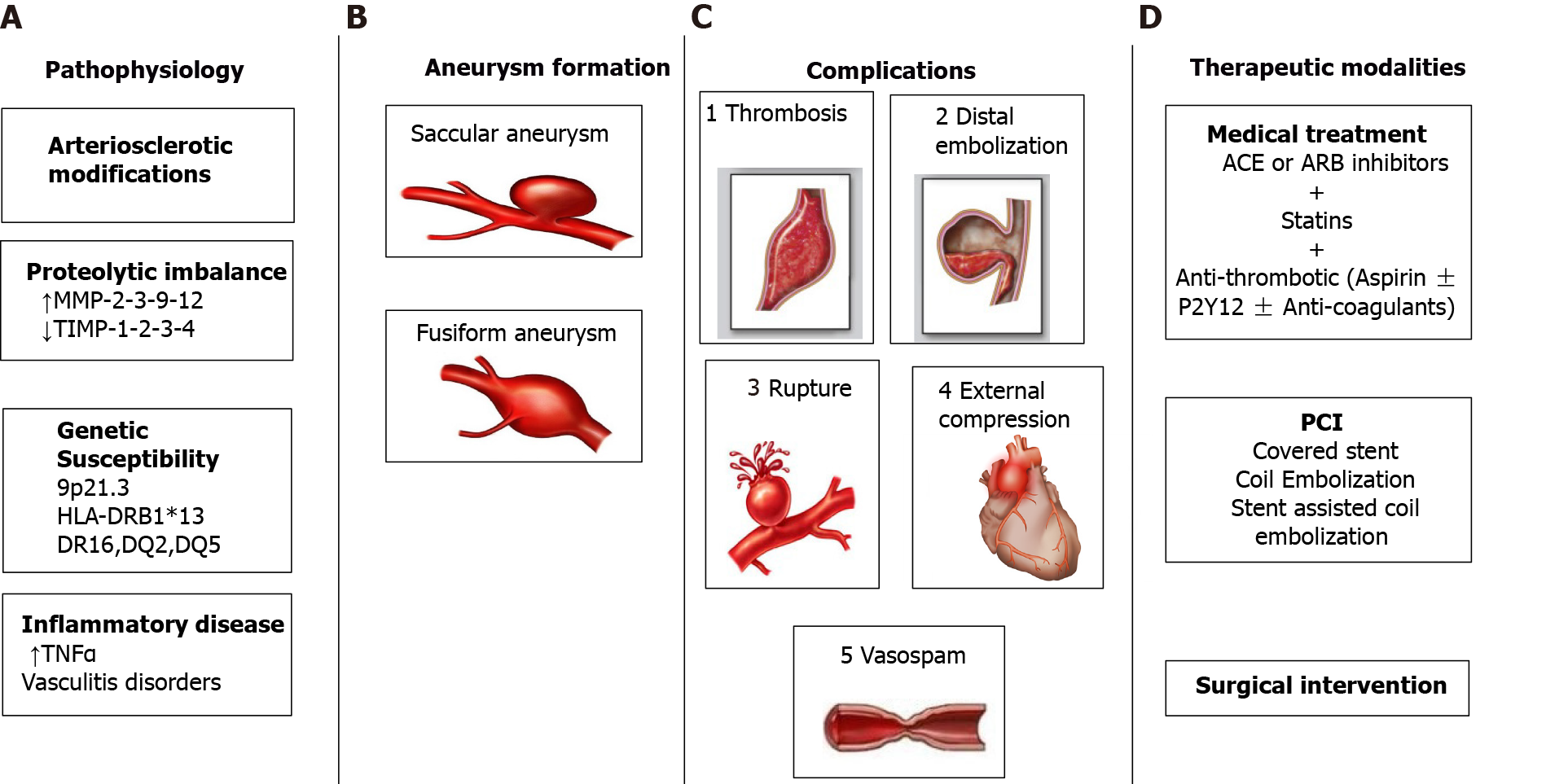
Coronary artery aneurysm (CAA) is a rare clinical entity defined by an abnormal focal dilation of the coronary artery exceeding the 1.5-fold diameter of the adjacent normal segment, whereas coronary artery ectasia describes similar but diffuse lesions involving ≥ 50% of the coronary artery length[1]. Thus, aneurysmal coronary disease is seen as focal aneurysm (e.g., Kawasaki) but also in more diffuse forms (diffuse ectasia). In general, CAAs are divided into two types: saccular when the longitudinal diameter is less than the transverse diameter; and fusiform in the opposite condition[2-4] (Figure 1). Fusiform CAAs are commonly found in the left anterior descending artery[2-4]. Aneurysmal dilation ≥ 8 mm in diameter or four times higher than reference coronary diameter characterized a giant CAA[5-7]. The incidence of true CAA varies from 0.3% to 5.3%[8,9] knowing that most recent studies reported an incidence rate below 1%[10-13]. The right coronary artery is most commonly involved followed by left anterior descending artery, circumflex and left main[8,9]. A predilection to male gender and proximal coronary segment was described[14].
CAA is usually a silent disorder incidentally detected by coronary angiography or computed tomography (CT) angiography. The wide spectrum of clinical presentations ranging from chest pain to sudden cardiac death results from the development of complications and/or the coexistence of obstructive coronary artery disease[8,15-20]. Until now, the management of CAA is individualized depending on clinical manifestations, patient conditions, CAA characteristics, physician experience and preference. A poor long-term prognosis has been attributed to the presence of CAA[21,22]. Herein, we provide an up-to-date systematic review on the pathogenesis, complications and management of CAA.
The pathophysiological mechanisms of CAA are not well understood, but atherosclerosis is the main identified etiology in adults and Kawasaki disease in children[5]. Atherosclerosis is a chronic progressive transmural inflammatory disease affecting the different vascular layers from the tunica intima to the external elastic lamina, thereby contributing to a weakened vascular wall[23-27]. It is worthy to mention that stenotic coronary atherosclerosis and CAA commonly coexist. They share in common several histological patterns like hyalinization, lipid deposition, destruction of coronary layers, focal calcification and fibrosis[23-27]. All of these arteriosclerotic modifications on top of the liberation of nitric oxide, which enhances vasodilation, reduce the coronary resistance to intraluminal pressure predisposing it to dilatation and CAA formation. Kawasaki disease is an acute inflammatory syndrome that may infiltrate the arterial wall resulting in acute vasculitis and subsequent aneurysmal dilation[28]. Indeed, a high level of tumor necrosis factor-alpha, which is an inflammatory cytokine, was linked to the breakdown of elastin and the development of CAA[29]. Currently, coronavirus disease 2019 markedly increased the incidence of Kawasaki disease with cardiovascular involvement in children and young adults[30]. Other vasculitic disorders like Takayasu arteritis, polyarteritis nodosa, systemic lupus erythematosus and rheumatoid arthritis may lead to CAA[31,32].
Otherwise, matrix-degrading enzymes play a pivotal role in the pathogenesis of CAA. A proteolytic imbalance caused by a high level of matrix metalloproteinases (MMP-2,-3,-9,-12) and a reduced level of matrix metalloproteinase inhibitors (tissue-specific inhibitors of metalloproteinases, TIMP-1,-2,-3,-4) resulting in connective tissue proteins and arterial wall matrix degradation, is reported in aneurysmal vessels[33-35]. Genetic susceptibility such as variants on chromosome 9p21.3, HLA-DR B1*13, DR16, DQ2, DQ5 and several hereditary disorders such as Marfan syndrome and Ehler-Danlos were linked to CAA[9,36]. Infectious processes that directly invade the vascular wall or provoke immune complex deposition contribute to CAA formation[37].
Lastly, CAA may complicate coronary angioplasty with stent implantation[38-40]. Aneurysmal formation was observed with bare metal stents, drug eluting stents and biodegradable stents[38-40]. Coronary dissection, oversizing, stent malapposition, high pressure balloons and local wall injury are the main mechanisms associated to stent-related CAA[41,42].
Most patients with CAA are asymptomatic, and the occurrence of clinical manifestations is related to a concomitant atherosclerotic coronary artery disease or to the development of complications. Local thrombosis, distal embolization, aneurysm rupture, coronary spasm and compression of adjacent structure by massive enlargement of CAA are the most observed complications[17,18,43,44] (Figure 2). The stagnation of blood flow and the reduction of shear stress in CAA contribute to thrombus formation and subsequent potential distal embolization[45]. Several published cases reported the presence of thrombus inside the aneurysm[46,47] and described myocardial wall motion abnormalities following distal embolization in patients with CAA[48]. Theoretically, CAA does not have enough intact smooth muscle to produce significant vasoconstriction knowing that smooth muscle hypercontractility is implicated in the pathophysiological mechanism of coronary artery spasm[49]. However, Bove et al[50] were the first to describe a recurrent angina linked to spasm of aneurysmal coronary arteries. The rupture of CAA is rare, unpredictable and a serious life-threatening condition that results in cardiac tamponade and sudden death. Since previously published data[51-53], the incidence of rupture of CAA was dramatically decreased[54]. An excessively enlarged CAA may compress the surrounding adjacent cardiopulmonary structures like the right atrium[55], the right ventricular wall[55], the pulmonary artery and the tricuspid valve[56].
Until now, there are no standardized international recommendations for the management of CAA due to the lack of data from randomized clinical trials. Most of the available data are based on case series and anecdotal evidence. The management of CAA is individualized and depends on clinical presentation (silent or symptomatic), characteristics of CAA (location, size, shape, evolution, etiology), patient profile (age, comorbidities, cardiovascular risk factors) and physician experience. Different approaches including medical treatment, percutaneous coronary intervention (stent angioplasty and coil embolization) and surgical excision were priorly performed. Indeed, the optimal therapeutic strategy leading to the best outcome was not yet defined due to the absence of comparative studies. Coronary angiography is the invasive gold standard tool to assess the anatomic features of CAA, while coronary CT is the alternative non-invasive technique of choice for the follow-up[57].
First of all, an intense control of cardiovascular risk factors is advocated in patients with CAA regardless of the presence of concomitant obstructive coronary artery disease[58]. Basing on the association between the overexpression of angiotensin-converting enzyme and aneurysm formation, it was hypothesized that angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers may slow the progression of CAA[59]. Also, the use of statins in CAA patients is desirable. A beneficial role was attributed to statins by inhibiting the expression of matrix metalloproteinases, which play a crucial role in the physiological mechanism of aneurysm formation[60]. Otherwise, the proper indication of anti-thrombotic regimen for the management of CAA is a matter of debate noticing that data from previously published studies are controversial.
Despite the risk of thrombus formation and distal embolization described above, few retrospective studies conclude that anticoagulation strategy is unbeneficial by showing a similar rate of thrombotic events in patients with and without CAA[61-63]. Contradictory results were revealed by Warisawa et al[21] and Baman et al[57] who showed greater rates of 5-year mortality and major cardiovascular adverse events (MACE) in patients with CAA. A recently published study found that prescribing oral anticoagulation led to positive outcomes in patients with coronary artery ectasia by reporting 0% of MACE in patients treated with oral anticoagulation compared to those who did not receive anti-thrombotic therapy after 49 mo of follow-up[22]. Therefore, coronary artery ectasia was identified as an independent predictor of cardiac events in patients presenting with acute coronary syndromes[22]. Myocardial infarction, MACE and death were two to four times higher in patients with coronary artery ectasia[22]. However, it is worthy to mention that prolonged anti-thrombotic therapy may provoke complications, such as bleeding. Lastly, intravenous immunoglobulin therapy in Kawasaki disease promotes CAA regression and decreases the incidence of MACE[64].
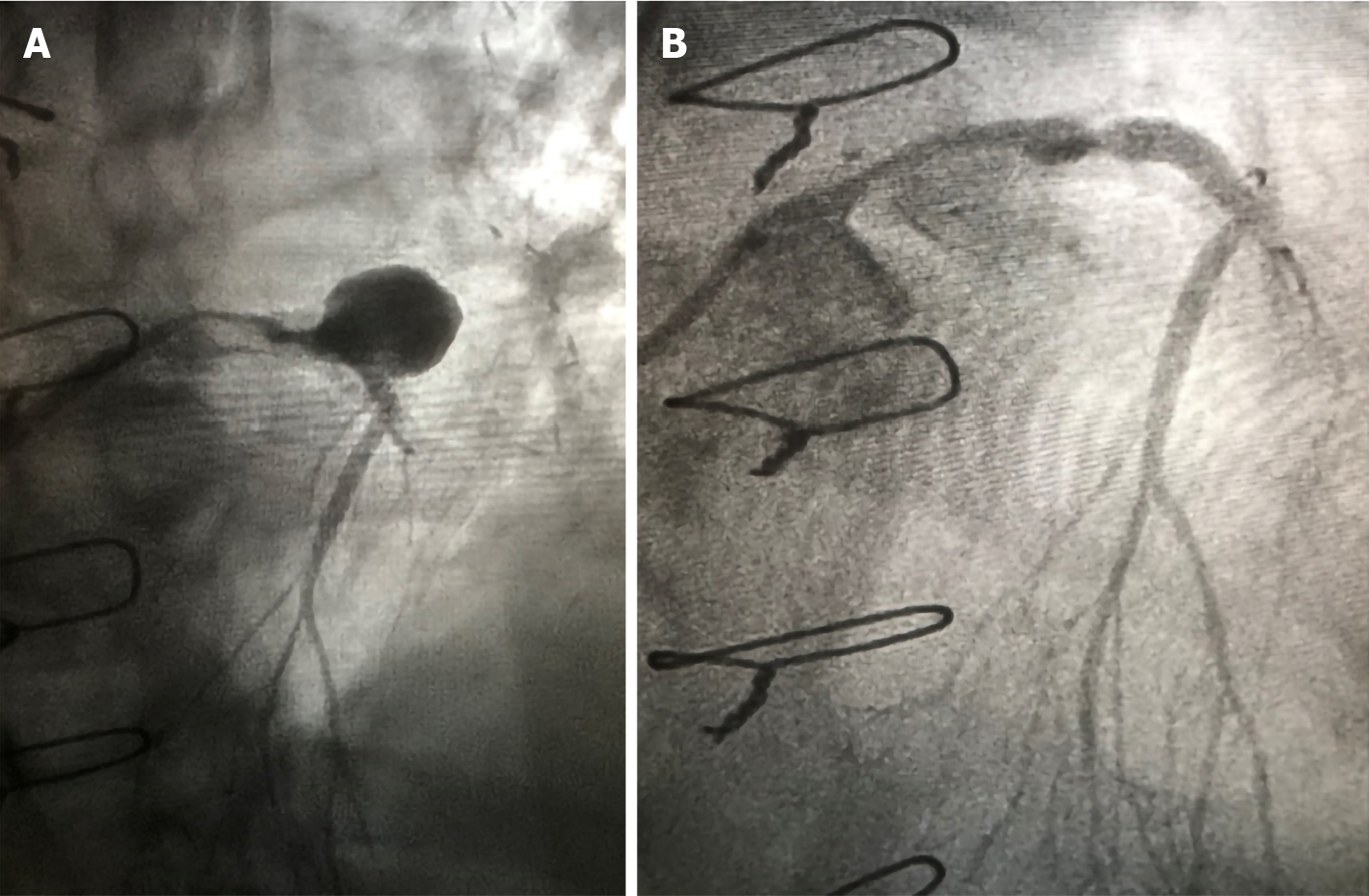
Percutaneous coronary intervention (PCI) is a relatively new therapeutic option allowing to exclude CAA when the clinical and/or anatomical risk is high (Figure 3). Several techniques were reported in the literature, like covered stent implantation[65], coil embolization and stent-assisted coil insertion[66]. Conventionally, PCI is the preferred approach to exclude smaller CAA, while surgical approach is preferred for the larger aneurysms[67]. Several limitations like difficulty of stent delivery, occlusion of side branches and high percentage of restenosis were observed with covered stent angioplasty[68]. Bare metal stents were previously preferred over polytetrafluoroethylene covered stents due to the lower incidence of thrombosis and restenosis[69]. The last generation of covered stents, such as PK Papyrus stents, achieve a greater bending flexibility and a smaller crossing profile compared to the traditional sandwich designed stents that allow sealing of perforations and exclude aneurysms[70]. Therefore, stent-assisted coil insertion technique is favored over coil embolization in the management of wide-necked CAA because it reduces the risk of occlusion of the parent coronary vessel and rupture of CAA[66].
Previous studies investigating the outcomes of PCI performed in patients with CAA in the setting of acute myocardial infarction found a worst prognosis, thereby showing higher rates of procedural failure, mortality, no-reflow, stent thrombosis, distal embolization and target vessel revascularization[10-13,71]. Performing PCI in the setting of aneurysmal coronary arteries imposes technical challenges for physicians, such as appropriate sizing, landing zone assessment and thrombus burden. As a result, it is rare to intervene in asymptomatic patients with CAA.
Different surgical techniques have been described including aneurysmectomy with or without coronary artery bypass graft, aneurysm ligation, resection and marsupialization[72]. Indeed, the optimal surgical approach has not yet been defined. Overall, surgery is considered an alternative adequate therapeutic strategy for the management of symptomatic patients unsuitable for PCI, patients with concomitant obstructive coronary artery disease, CAA involving the large bifurcation or the left main, complicated CAA and giant CAA at high risk of rupture[72,73].
A recently published study showed that CT angiography is superior to cardiac magnetic resonance imaging for detection, risk stratification and follow-up of CAA in patients with Kawasaki disease[74]. Also, CT angiography has already proven its value for the assessment of the diameter of coronary arteries in adults and patients with Kawasaki disease when compared to coronary angiography[75-78]. Indeed, the sensitivity of CT angiography for detection of CAA and related complications is remarkably high. Because radiation exposure is associated with an increase in lifetime cancer risk, especially in children, the lack of radiation exposure is the main described benefit to cardiac magnetic resonance imaging over coronary angiography and CT angiography for CAA detection[74]. Lastly, CT angiography provides accurate data concerning the coronary anatomy, calcification, luminal diameter, thrombi and aneurysmal features[79]. It represents the imaging of choice for the long-term monitoring of CAA[57].
Usually, CAA is an incidental angiographic finding associated to atherosclerosis. The natural history of CAA is not well understood, but it is a progressive silent disease. Future prospective comparative trials to define the appropriate strategy and the optimal time to intervene are required in order to avoid the development of serious complications, especially in those with concomitant obstructive coronary artery disease.
| 1. | Luo Y, Tang J, Liu X, Qiu J, Ye Z, Lai Y, Yao Y, Li J, Wang X. Coronary Artery Aneurysm Differs From Coronary Artery Ectasia: Angiographic Characteristics and Cardiovascular Risk Factor Analysis in Patients Referred for Coronary Angiography. Angiology. 2017;68:823-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 53] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 2. | Aqel RA, Zoghbi GJ, Iskandrian A. Spontaneous coronary artery dissection, aneurysms, and pseudoaneurysms: a review. Echocardiography. 2004;21:175-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 84] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 3. | Harikrishnan S, Sunder KR, Tharakan JM, Titus T, Bhat A, Sivasankaran S, Bimal F. Saccular coronary aneurysms: angiographic and clinical profile and follow-up of 22 cases. Indian Heart J. 2000;52:178-182. [PubMed] |
| 4. | Tunick PA, Slater J, Kronzon I, Glassman E. Discrete atherosclerotic coronary artery aneurysms: a study of 20 patients. J Am Coll Cardiol. 1990;15:279-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 118] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Díaz-Zamudio M, Bacilio-Pérez U, Herrera-Zarza MC, Meave-González A, Alexanderson-Rosas E, Zambrana-Balta GF, Kimura-Hayama ET. Coronary artery aneurysms and ectasia: role of coronary CT angiography. Radiographics. 2009;29:1939-1954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 118] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 6. | Nikolaidou CN, Vassiliou VS, Watson WD. Coronary artery aneurysms-a truly rare entity or simply unrecognized so far? Oxf Med Case Reports. 2019;2019:omz009. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Kato H, Sugimura T, Akagi T, Sato N, Hashino K, Maeno Y, Kazue T, Eto G, Yamakawa R. Long-term consequences of Kawasaki disease. A 10- to 21-year follow-up study of 594 patients. Circulation. 1996;94:1379-1385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 923] [Cited by in RCA: 951] [Article Influence: 31.7] [Reference Citation Analysis (0)] |
| 8. | Kawsara A, Núñez Gil IJ, Alqahtani F, Moreland J, Rihal CS, Alkhouli M. Management of Coronary Artery Aneurysms. JACC Cardiovasc Interv. 2018;11:1211-1223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 284] [Article Influence: 35.5] [Reference Citation Analysis (0)] |
| 9. | Abou Sherif S, Ozden Tok O, Taşköylü Ö, Goktekin O, Kilic ID. Coronary Artery Aneurysms: A Review of the Epidemiology, Pathophysiology, Diagnosis, and Treatment. Front Cardiovasc Med. 2017;4:24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 103] [Cited by in RCA: 197] [Article Influence: 21.9] [Reference Citation Analysis (0)] |
| 10. | Núñez-Gil IJ, Terol B, Feltes G, Nombela-Franco L, Salinas P, Escaned J, Jiménez-Quevedo P, Gonzalo N, Vivas D, Bautista D, Macaya C, Fernández-Ortiz A. Coronary aneurysms in the acute patient: Incidence, characterization and long-term management results. Cardiovasc Revasc Med. 2018;19:589-596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 11. | Iannopollo G, Ferlini M, Koziński M, Ormezzano MF, Crimi G, Lanfranchi L, Camporotondo R, Visconti LO, De Ferrari GM, De Servi S. Patient Outcomes With STEMI Caused by Aneurysmal Coronary Artery Disease and Treated With Primary PCI. J Am Coll Cardiol. 2017;69:3006-3007. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 40] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 12. | Ipek G, Gungor B, Karatas MB, Onuk T, Keskin M, Tanik O, Hayiroglu MI, Oz A, Borklu EB, Bolca O. Risk factors and outcomes in patients with ectatic infarct-related artery who underwent primary percutaneous coronary intervention after ST elevated myocardial infarction. Catheter Cardiovasc Interv. 2016;88:748-753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 13. | Joo HJ, Woong Yu C, Choi R, Park J, Lee HJ, Kim JS, Choi YJ, Park JH, Hong SJ, Lim DS. Clinical outcomes of patients with coronary artery aneurysm after the first generation drug-eluting stent implantation. Catheter Cardiovasc Interv. 2018;92:E235-E245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Manginas A, Cokkinos DV. Coronary artery ectasias: imaging, functional assessment and clinical implications. Eur Heart J. 2006;27:1026-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 109] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 15. | Sheikh AS, Hailan A, Kinnaird T, Choudhury A, Smith D. Coronary Artery Aneurysm: Evaluation, Prognosis, and Proposed Treatment Strategies. Heart Views. 2019;20:101-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 91] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 16. | Aboeata AS, Sontineni SP, Alla VM, Esterbrooks DJ. Coronary artery ectasia: current concepts and interventions. Front Biosci (Elite Ed). 2012;4:300-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Ramirez FD, Hibbert B, Simard T, Pourdjabbar A, Wilson KR, Hibbert R, Kazmi M, Hawken S, Ruel M, Labinaz M, O'Brien ER. Natural history and management of aortocoronary saphenous vein graft aneurysms: a systematic review of published cases. Circulation. 2012;126:2248-2256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 113] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 18. | Chrissoheris MP, Donohue TJ, Young RS, Ghantous A. Coronary artery aneurysms. Cardiol Rev. 2008;16:116-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 40] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 19. | Kühl M, Varma C. A case of acute coronary thrombosis in diffuse coronary artery ectasia. J Invasive Cardiol. 2008;20:E23-E25. [PubMed] |
| 20. | Krüger D, Stierle U, Herrmann G, Simon R, Sheikhzadeh A. Exercise-induced myocardial ischemia in isolated coronary artery ectasias and aneurysms ("dilated coronopathy"). J Am Coll Cardiol. 1999;34:1461-1470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 170] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 21. | Warisawa T, Naganuma T, Tomizawa N, Fujino Y, Ishiguro H, Tahara S, Kurita N, Nojo T, Nakamura S. High prevalence of coronary artery events and non-coronary events in patients with coronary artery aneurysm in the observational group. Int J Cardiol Heart Vasc. 2016;10:29-31. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 22. | Doi T, Kataoka Y, Noguchi T, Shibata T, Nakashima T, Kawakami S, Nakao K, Fujino M, Nagai T, Kanaya T, Tahara Y, Asaumi Y, Tsuda E, Nakai M, Nishimura K, Anzai T, Kusano K, Shimokawa H, Goto Y, Yasuda S. Coronary Artery Ectasia Predicts Future Cardiac Events in Patients With Acute Myocardial Infarction. Arterioscler Thromb Vasc Biol. 2017;37:2350-2355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 111] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 23. | Alford WC Jr, Stoney WS, Burrus GR, Frist RA, Thomas CS Jr. Recognition and operative management of patients with arteriosclerotic coronary artery aneurysms. Ann Thorac Surg. 1976;22:317-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 47] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 24. | Robinson FC. Aneurysms of the coronary arteries. Am Heart J. 1985;109:129-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 82] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 25. | Zeb M, McKenzie DB, Scott PA, Talwar S. Treatment of coronary aneurysms with covered stents: a review with illustrated case. J Invasive Cardiol. 2012;24:465-469. [PubMed] |
| 26. | Kelley MP, Carver JR. Coronary artery aneurysms. J Invasive Cardiol. 2002;14:461-462. [PubMed] |
| 27. | Nichols L, Lagana S, Parwani A. Coronary artery aneurysm: a review and hypothesis regarding etiology. Arch Pathol Lab Med. 2008;132:823-828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 116] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 28. | Amano S, Hazama F, Hamashima Y. Pathology of Kawasaki disease: I. Pathology and morphogenesis of the vascular changes. Jpn Circ J. 1979;43:633-643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 120] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 29. | Dajani AS, Taubert KA, Gerber MA, Shulman ST, Ferrieri P, Freed M, Takahashi M, Bierman FZ, Karchmer AW, Wilson W. Diagnosis and therapy of Kawasaki disease in children. Circulation. 1993;87:1776-1780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 375] [Cited by in RCA: 330] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 30. | Carvalho T. COVID-19-induced Kawasaki disease. Lancet. 2020;395:1771-1778. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 679] [Cited by in RCA: 682] [Article Influence: 113.7] [Reference Citation Analysis (0)] |
| 31. | Sharma BK, Jain S, Suri S, Numano F. Diagnostic criteria for Takayasu arteritis. Int J Cardiol. 1996;54 Suppl:S141-S147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 232] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 32. | Panja M, Sarkar C, Kar AK, Kumar S, Mazumder B, Roy S, Sinha DP, Sarkar NC. Coronary artery lesions in Takayasu's arteritis--clinical and angiographic study. J Assoc Physicians India. 1998;46:678-681. [PubMed] |
| 33. | Hui-Yuen JS, Duong TT, Yeung RS. TNF-alpha is necessary for induction of coronary artery inflammation and aneurysm formation in an animal model of Kawasaki disease. J Immunol. 2006;176:6294-6301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 137] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 34. | Mata KM, Prudente PS, Rocha FS, Prado CM, Floriano EM, Elias J Jr, Rizzi E, Gerlach RF, Rossi MA, Ramos SG. Combining two potential causes of metalloproteinase secretion causes abdominal aortic aneurysms in rats: a new experimental model. Int J Exp Pathol. 2011;92:26-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 35. | Pahlavan PS, Niroomand F. Coronary artery aneurysm: a review. Clin Cardiol. 2006;29:439-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 153] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 36. | Ozaki K, Tanaka T. Molecular genetics of coronary artery disease. J Hum Genet. 2016;61:71-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 47] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 37. | Singh H, Singh C, Aggarwal N, Dugal JS, Kumar A, Luthra M. Mycotic aneurysm of left anterior descending artery after sirolimus-eluting stent implantation: a case report. Catheter Cardiovasc Interv. 2005;65:282-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 43] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 38. | Gadepalli R, Rayidi G, Pramod G, Srivastava SK, Venkata Balakrishna SN. A case of early development of giant coronary artery aneurysms after drug-eluting stents implantation: An unpredictable menace. Interv Med Appl Sci. 2017;9:47-50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 39. | Timmers L, Lim YC, Tan HC, Low AF. Coronary aneurysm without malapposition after bioresorbable vascular scaffold implantation. EuroIntervention. 2016;12:60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 40. | Lee WC, Chung WJ, Fang HY, Wu CJ. Coronary artery aneurysms formation within Everolimus-eluting stents and bioresorbable vascular scaffolds. Int J Cardiol. 2016;206:58-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 41. | Bell MR, Garratt KN, Bresnahan JF, Edwards WD, Holmes DR Jr. Relation of deep arterial resection and coronary artery aneurysms after directional coronary atherectomy. J Am Coll Cardiol. 1992;20:1474-1481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 60] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 42. | Regar E, Klauss V, Henneke KH, Werner F, Theisen K, Mudra H. Coronary aneurysm after bailout stent implantation: diagnosis of a false lumen with intravascular ultrasound. Cathet Cardiovasc Diagn. 1997;41:407-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 43. | Rath S, Har-Zahav Y, Battler A, Agranat O, Rotstein Z, Rabinowitz B, Neufeld HN. Fate of nonobstructive aneurysmatic coronary artery disease: angiographic and clinical follow-up report. Am Heart J. 1985;109:785-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 108] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 44. | Ebina T, Ishikawa Y, Uchida K, Suzuki S, Imoto K, Okuda J, Tsukahara K, Hibi K, Kosuge M, Sumita S, Mochida Y, Ishikawa T, Uchino K, Umemura S, Kimura K. A case of giant coronary artery aneurysm and literature review. J Cardiol. 2009;53:293-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 45. | Ebert PA, Peter RH, Gunnells JC, Sabiston DC Jr. Resecting and grafting of coronary artery aneurysm. Circulation. 1971;43:593-598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 59] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 46. | Van den Broek H, Segal BL. Coronary aneurysms in a young woman: angiographic documentation of the natural course. Chest. 1973;64:132-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 47. | Myler RK, Schechtmann NS, Rosenblum J, Collinsworth KA, Bashour TT, Ward K, Murphy MC, Stertzer SH. Multiple coronary artery aneurysms in an adult associated with extensive thrombus formation resulting in acute myocardial infarction: successful treatment with intracoronary urokinase, intravenous heparin, and oral anticoagulation. Cathet Cardiovasc Diagn. 1991;24:51-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 48. | Berkoff HA, Rowe GG. Atherosclerotic ulcerative disease and associated aneurysms of the coronary arteries. Am Heart J. 1975;90:153-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 48] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 49. | Matta A, Bouisset F, Lhermusier T, Campelo-Parada F, Elbaz M, Carrié D, Roncalli J. Coronary Artery Spasm: New Insights. J Interv Cardiol. 2020;2020:5894586. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 68] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 50. | Bove AA, Vlietstra RE. Spasm in ectatic coronary arteries. Mayo Clin Proc. 1985;60:822-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 51. | Daoud AS, Pankin D, Tulgan H, Florentin RA. Aneurysms of the coronary artery. Report of ten cases and review of literature. Am J Cardiol. 1963;11:228-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 248] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 52. | Scott DH. Aneurysm of the coronary arteries. Am Heart J. 1948;36:403-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 99] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 53. | Plachta A, Speer FD. Aneurysm of the left coronary artery; review of literature and report of three cases. AMA Arch Pathol. 1958;66:210-217. [PubMed] |
| 54. | Burns CA, Cowley MJ, Wechsler AS, Vetrovec GW. Coronary aneurysms: a case report and review. Cathet Cardiovasc Diagn. 1992;27:106-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 55. | Lachmann M, Will A, Linhard M, Ibrahim T. Progression of a coronary artery aneurysm with symptomatic compression of cardiac structures. Eur Heart J. 2018;39:3336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 56. | Ahmed T, Chahal D, Shkullaku M, Gupta A. Extensive coil embolization of a giant coronary artery aneurysm in an octogenarian: a case report. Eur Heart J Case Rep. 2020;4:1-5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 57. | Devabhaktuni S, Mercedes A, Diep J, Ahsan C. Coronary Artery Ectasia-A Review of Current Literature. Curr Cardiol Rev. 2016;12:318-323. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 86] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 58. | Baman TS, Cole JH, Devireddy CM, Sperling LS. Risk factors and outcomes in patients with coronary artery aneurysms. Am J Cardiol. 2004;93:1549-1551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 148] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 59. | Gülec S, Aras O, Atmaca Y, Akyürek O, Hanson NQ, Sayin T, Tsai MY, Akar N, Oral D. Deletion polymorphism of the angiotensin I converting enzyme gene is a potent risk factor for coronary artery ectasia. Heart. 2003;89:213-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 30] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 60. | Tengiz I, Ercan E, Aliyev E, Sekuri C, Duman C, Altuglu I. Elevated levels of matrix metalloprotein-3 in patients with coronary aneurysm: A case control study. Curr Control Trials Cardiovasc Med. 2004;5:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 61. | Hartnell GG, Parnell BM, Pridie RB. Coronary artery ectasia. Its prevalence and clinical significance in 4993 patients. Br Heart J. 1985;54:392-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 291] [Cited by in RCA: 350] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 62. | Boles U, Zhao Y, Rakhit R, Shiu MF, Papachristidis A, David S, Koganti S, Gilbert T, Henein MY. Patterns of coronary artery ectasia and short-term outcome in acute myocardial infarction. Scand Cardiovasc J. 2014;48:161-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 63. | Zhang Y, Huang QJ, Li XL, Guo YL, Zhu CG, Wang XW, Xu B, Gao RL, Li JJ. Prognostic Value of Coronary Artery Stenoses, Markis Class, and Ectasia Ratio in Patients with Coronary Artery Ectasia. Cardiology. 2015;131:251-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 64. | Friedman KG, Gauvreau K, Hamaoka-Okamoto A, Tang A, Berry E, Tremoulet AH, Mahavadi VS, Baker A, deFerranti SD, Fulton DR, Burns JC, Newburger JW. Coronary Artery Aneurysms in Kawasaki Disease: Risk Factors for Progressive Disease and Adverse Cardiac Events in the US Population. J Am Heart Assoc. 2016;5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 118] [Cited by in RCA: 200] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 65. | Matta A, Zouari F, Campelo-Parada F, Carrié D. A Giant Left Anterior Descending Artery (LAD) Coronary Artery Aneurysm Treated by Covered Stent Angioplasty: A Case Report. Am J Case Rep. 2020;21:e925820. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 66. | Saccà S, Pacchioni A, Nikas D. Coil embolization for distal left main aneurysm: a new approach to coronary artery aneurysm treatment. Catheter Cardiovasc Interv. 2012;79:1000-1003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 67. | Szalat A, Durst R, Cohen A, Lotan C. Use of polytetrafluoroethylene-covered stent for treatment of coronary artery aneurysm. Catheter Cardiovasc Interv. 2005;66:203-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 75] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 68. | Kilic ID, Fabris E, Serdoz R, Caiazzo G, Foin N, Abou-Sherif S, Di Mario C. Coronary covered stents. EuroIntervention. 2016;12:1288-1295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 55] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 69. | Schächinger V, Hamm CW, Münzel T, Haude M, Baldus S, Grube E, Bonzel T, Konorza T, Köster R, Arnold R, Haase J, Probst P, vom Dahl J, Neumann FJ, Mudra H, Hennen B, Thiele L, Zeiher AM; STENTS (STents IN Grafts) Investigators. A randomized trial of polytetrafluoroethylene-membrane-covered stents compared with conventional stents in aortocoronary saphenous vein grafts. J Am Coll Cardiol. 2003;42:1360-1369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 80] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 70. | Lattuca B, Schmutz L, Cornillet L, Ledermann B, Fernandez V, Messner P, Leclercq F, Cayla G. New polyurethane covered stent with low profile for treatment of a large aneurysm after Left Anterior Descending artery stenting: First experience. Int J Cardiol. 2015;201:208-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 71. | Bogana Shanmugam V, Psaltis PJ, T L Wong D, T Meredith I, Malaiapan Y, Ahmar W. Outcomes After Primary Percutaneous Coronary Intervention for ST-Elevation Myocardial Infarction Caused by Ectatic Infarct Related Arteries. Heart Lung Circ. 2017;26:1059-1068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 72. | Singh SK, Goyal T, Sethi R, Chandra S, Devenraj V, Rajput NK, Kaushal D, Tewarson V, Gupta S, Kumar S. Surgical treatment for coronary artery aneurysm: a single-centre experience. Interact Cardiovasc Thorac Surg. 2013;17:632-636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 73. | LaMotte LC, Mathur VS. Atherosclerotic coronary artery aneurysms: eight-year angiographic follow-up. Tex Heart Inst J. 2000;27:72-73. [PubMed] |
| 74. | van Stijn-Bringas Dimitriades D, Planken N, Kuipers I, Kuijpers T. CT Angiography or Cardiac MRI for Detection of Coronary Artery Aneurysms in Kawasaki Disease. Front Pediatr. 2021;9:630462. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 75. | Nieman K, Cademartiri F, Lemos PA, Raaijmakers R, Pattynama PM, de Feyter PJ. Reliable noninvasive coronary angiography with fast submillimeter multislice spiral computed tomography. Circulation. 2002;106:2051-2054. [PubMed] |
| 76. | Ropers D, Baum U, Pohle K, Anders K, Ulzheimer S, Ohnesorge B, Schlundt C, Bautz W, Daniel WG, Achenbach S. Detection of coronary artery stenoses with thin-slice multi-detector row spiral computed tomography and multiplanar reconstruction. Circulation. 2003;107:664-666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 705] [Cited by in RCA: 637] [Article Influence: 27.7] [Reference Citation Analysis (0)] |
| 77. | Tsujii N, Tsuda E, Kanzaki S, Kurosaki K. Measurements of Coronary Artery Aneurysms Due to Kawasaki Disease by Dual-Source Computed Tomography (DSCT). Pediatr Cardiol. 2016;37:442-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 78. | Duan Y, Wang X, Cheng Z, Wu D, Wu L. Application of prospective ECG-triggered dual-source CT coronary angiography for infants and children with coronary artery aneurysms due to Kawasaki disease. Br J Radiol. 2012;85:e1190-e1197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 79. | Forte E, Aiello M, Inglese M, Infante T, Soricelli A, Tedeschi C, Salvatore M, Cavaliere C. Coronary artery aneurysms detected by computed tomography coronary angiography. Eur Heart J Cardiovasc Imaging. 2017;18:1229-1235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: France
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cigrovski Berkovic M, Schoenhagen P S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Ma YJ