Published online Mar 26, 2021. doi: 10.4330/wjc.v13.i3.46
Peer-review started: June 8, 2020
First decision: October 21, 2020
Revised: January 13, 2021
Accepted: March 8, 2021
Article in press: March 8, 2021
Published online: March 26, 2021
Processing time: 283 Days and 3.6 Hours
Implantable cardioverter defibrillators (ICDs) and cardiac resynchronisation therapy with defibrillators (CRT-D) reduce mortality in certain cardiac patient populations. However, inappropriate shocks pose a problem, having both adverse physical and psychological effects on the patient. The advances in device technology now allow remote monitoring (RM) of devices to replace clinic follow up appointments. This allows real time data to be analysed and actioned and this may improve patient care.
To determine if RM in patients with an ICD is associated with fewer inappropriate shocks and reduced time to medical assessment.
This was a single centre, retrospective observational study, involving 156 patients implanted with an ICD or CRT-D, followed up for 2 years post implant. Both appropriate and inappropriate shocks were recorded along with cause for inappropriate shocks and time to medical assessment.
RM was associated with fewer inappropriate shocks (13.6% clinic vs 3.9% RM; P = 0.030) and a reduced time to medical assessment (15.1 ± 6.8 vs 1.0 ± 0.0 d; P < 0.001).
RM in patients with an ICD is associated with improved patient outcomes.
Core Tip: Advances in device technology now allow remote monitoring of implantable cardioverter defibrillators to replace clinic follow up appointments. This allows real time data to be analysed and actioned. This study shows that remote monitoring of such devices is associated with fewer inappropriate shocks and reduced time to medical assessment in a remote and rural area. This represents better patient care and will reduce the morbidity caused by inappropriate shocks.
- Citation: Callum K, Graune C, Bowman E, Molden E, Leslie SJ. Remote monitoring of implantable defibrillators is associated with fewer inappropriate shocks and reduced time to medical assessment in a remote and rural area. World J Cardiol 2021; 13(3): 46-54
- URL: https://www.wjgnet.com/1949-8462/full/v13/i3/46.htm
- DOI: https://dx.doi.org/10.4330/wjc.v13.i3.46
Implantable cardioverter defibrillators (ICD) and cardiac resynchronisation therapy with defibrillation (CRT-D) are established treatments for a range of cardiac disorders and are proven to reduce mortality[1-4]. The continuing care for patients with ICDs and CRT-Ds involves regular follow up appointments to monitor the function of the device and the clinical status of the patient. A limitation of the conventional clinic follow up model is the lack of information between visits and immediately after therapy (e.g., shocks). Remote monitoring (RM) using a telephonic transmission of pacemaker information from the patients home fills this gap with clinical trials having demonstrated the usefulness[5,6] including its safety[7], economic benefits[8] and improved clinical outcome[9].
The delivery of a shock can result in adverse effects for the patient, including impaired quality of life, psychiatric disturbances and is associated with increased all cause mortality[10], which increases with each subsequent shock. Shocks can be appropriate (e.g., to treat potentially fatal rapid ventricular rhythms) or inappropriate (non-fatal tachyarrythmia or lead dysfunction). RM reduces inappropriate shocks[5,11,12] through the earlier detection of events preceding the delivery of inappropriate shocks. In addition, RM offers the ability to reduce the time from a clinical event (such as an appropriate or inappropriate shock) to a clinical decision being made [time to medical assessment (TMA)]. This is an especially pertinent issue in remote and rural areas where patients can live long distances from specialist care.
This study aimed to assess appropriate and inappropriate shocks in patients with and without RM and to measure differences in TMA in a real world, remote and rural population.
This was a single site, retrospective observational study in a hospital serving a remote and rural population of 320000 spread over a geographical area of 32500 km2 including several islands. Patients who were implanted with an ICD or CRT-D between January 1, 2010 and January 1, 2014 were included. All patients were followed up for 2 years post implant. There were no exclusion criteria. Device programming and the use of RM was decided on an individual basis at the discretion of the cardiac rhythm physiologists after discussion with the clinician and patient. All RM systems transmit a variety of parameters, (such as lead parameters, battery status, therapy delivery, arrhythmias, intracardiac electrograms (IEGM), heart rate and rhythm statistics and patient activity levels) from the patients’ device via a mobile network link of landline, to the manufacturer’s central repository. Clinicians responsible for the follow up of patients receive automated email notifications if pre-specified criteria are met (e.g., shock delivered). All transmitted data is stored on a dedicated, secure, password protected website. Follow up arrangements between groups were similar, and on a case by case basis at the discretion of the follow up clinician. All ad-hoc reviews prompted by events highlighted from home monitoring were also arranged at the discretion of the clinician.
Baseline characteristics were collected from patient medical records. Device related data was retrieved from both hard and electronic copies of the patient records and from each of the companies’ respective RM systems; Home Monitoring (Biotronik), CareLink (Medtronic) or Merlin (St Jude Medical).
TMA was calculated in days; beginning with event onset at the delivery of a shock and ending when a clinical decision was made. Clinical decision was defined as management of an event, medical intervention, physician decision, decision for follow up clinic, or hospitalisation.
An inappropriate shock was defined as the delivery of a shock not for true ventricular tachycardia or ventricular fibrillation. Shocks were classified on a shock by shock basis, rather than by episode. For example, 4 shocks all received for an episode of T wave over sensing would be counted as 4 shocks not 1. Analysis of the IEGM by cardiac physiologists was used to ascertain whether shocks were appropriate or inappropriate. Inappropriate shocks were classified in relation to their cause, for example, atrial fibrillation (AF) or flutter, supraventricular tachycardia (SVT), T wave over sensing, noise, or V lead displacement.
Patients were defined as “RM” if they had an ICD/RCT-D with RM function and “clinic” if they had a standard ICD/CRT-D with no RM function. Baseline characteristics from the “RM” vs “clinic” monitoring groups were compared using the Wilcoxon rank sum test for continuous variables, with the Chi squared test being used for categorical variables. Continuous variables were reported as mean with standard deviation. The Man Whitney U, chi squared test and the students t test were used to analyse the inappropriate shock and TMA as appropriate. All tests were performed at a P = 0.05 significance level. All data were processed and analysed using Microsoft Excel 2007 software and SPSS software version 18.0.
This was a service evaluation using routinely collected data and therefore formal ethical approval was not required. Local Caldecott approval was obtained to access patients’ records for this project.
Of 156 patients were identified, with 45 in the clinic group and 111 in the RM group. Baseline characteristics are shown in Table 1. There was no significant difference between the two groups except for the manufacturer of the implanted device. A total of 16 patients were lost to follow up (10.3%) (Table 2).
| Clinic, n (%) | RM, n (%) | |
| n | 45 | 111 |
| Age at implant (year) | 63.6 ± 13.0 | 64.2 ± 11.5 |
| Male | 30 (85.7) | 85 (82.5) |
| NYHA functional class | ||
| I | 12 (34.3) | 40 (38.8) |
| II | 18 (51.4) | 52 (50.5) |
| III | 5(14.3) | 11 (10.7) |
| Cardiac disease category | ||
| Coronary artery disease | 21 (60.0) | 54 (52.4) |
| Non ischaemic dilated cardiomyopathy | 4 (11.4) | 15 (14.6) |
| Primary electrical disease | 3 (8.6) | 5 (4.9) |
| Hypertrophic cardiomyopathy | 1 (2.9) | 6 (5.8) |
| Valvular heart disease | 1 (2.9) | 2 (1.9) |
| Hypertensive | 1 (2.9) | 3 (2.9) |
| Other cardiomyopathy | 1 (2.9) | 5 (4.9) |
| Undetermined | 2 (5.7) | 10 (9.7) |
| None | 1 (2.9) | 1 (1.0) |
| ECG history of | ||
| Sustained ventricular tachycardia | 7 (20.0) | 24 (23.3) |
| Ventricular fibrillation | 6 (17.1) | 19 (18.4) |
| Torsade de pointes | 1 (2.9) | 3 (2.9) |
| Indication for ICD | ||
| Primary | 20 (57.1) | 57 (55.3) |
| Secondary | 15 (42.9) | 46 (44.7) |
| Implanted device | ||
| Single chamber ICD | 13 (37.1) | 27 (26.2) |
| Dual chamber ICD | 19 (54.3) | 74 (71.8) |
| CRT-D | 5 (14.3) | 23 (22.3) |
| Type of implant | ||
| Original | 30 (85.7) | 83 (80.6) |
| Replacement | 5 (14.3) | 20 (19.4) |
| Drug therapy | ||
| Beta-blocker | 25 (71.4) | 69 (70.0) |
| Digoxin | 2 (5.7) | 12 (11.7) |
| Amiodarone | 4 (11.4) | 8 (7.8) |
| Manufacturer | ||
| Biotronik | 11 (31.4) | 44 (42.7) |
| Boston scientific/guidant | 8 (28.8) | 0 (0)1 |
| Medtronic | 5 (14.3) | 41 (39.8) |
| St Jude Medical | 11 (31.4) | 18 (17.5) |
| Clinic, n (%) | RM, n (%) | |
| n | 45 | 111 |
| Reason lost to follow up | ||
| Out of area | 3 (6.7) | 4 (3.6) |
| Death | 7(15.6) | 4 (3.6) |
| Number of patients receiving shocks (appropriate) | 3 (8.6) | 14 (13.6) |
| 1 shock | 3 (8.6) | 9 (8.7) |
| 2-9 shocks | 0 | 6 (5.8) |
| ≥ 10 | 0 | 0 |
| Number of patients receiving shocks (inappropriate) | 4 (11.4) | 4 (3.9) |
| 1 shock | 0 | 2 (1.9) |
| 2-9 shocks | 2 (5.7) | 2 (1.9) |
| ≥ 10 | 2 (5.7) | 0 |
| Causes inappropriate shocks (number of shocks) | ||
| AF/flutter | 18 (42.9) | 2 (20.0) |
| SVT | 14 (33.3) | 1 (10.0) |
| T wave over sense | 0 | 1 (10.0) |
| V lead displacement | 0 | 6 (60.0) |
| Noise | 10 (23.8) | 0 |
| TMA | ||
| Appropriate shocks | 11.7 ± 9.2 | 1.8 ± 0.6 |
| Inappropriate shocks | 15.1 ± 6.8 | 1.0 ± 0.0 |
Table 2 shows the incidence of appropriate and inappropriate shocks for both groups. There was no significant difference between groups for the number of patients receiving appropriate shocks [3 (8.6%) clinic patients vs 14 (13.6%) RM patients, P = 0.388]. However, there was a significant difference for the number of patients receiving inappropriate shocks [4 (11.4%) clinic patients vs 4 (3.9%) RM patients, P = 0.030]. The maximum number of shocks received by 1 patient was 14, this patient was in the clinic follow up group and shocks were due to incorrectly identified SVT.
The most common cause of inappropriate shocks was AF/flutter in the clinic group and ventricular lead displacement in the RM group (Table 2).
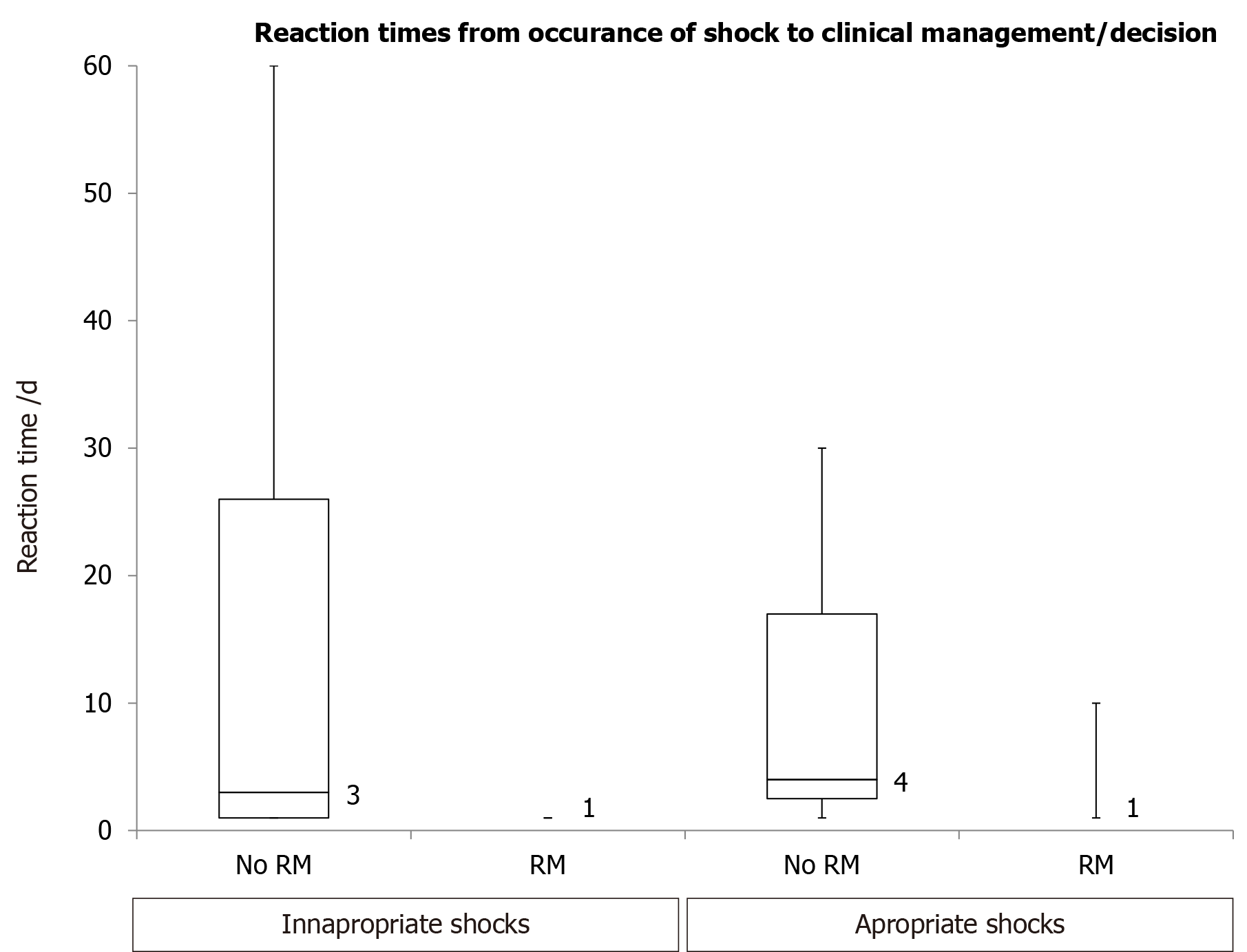
TMA was significantly higher in clinic vs RM group for inappropriate shocks (15.1 ± 6.8 vs 1.0 ± 0.0 d; P < 0.001) and appropriate shocks (11.7 ± 9.2 vs 1.8 ± 0.6 d; P < 0.001). (Figure 1) Reasons for a delayed TMA included patients unaware of shocks, ability to travel and delayed transfers from community hospitals.
This study has shown that RM is associated with a reduced TMA and a reduced number of inappropriate shocks in a patient population living in a remote and rural area.
Prompt identification and intervention of inappropriate shocks is essential to prevent subsequent inappropriate shocks. Although patients are typically aware of receiving a shock there are occasions when patients are not. This study was able to demonstrate an association between RM and a reduced TMA following the delivery of a shock (appropriate or inappropriate) compared to clinic follow up. A quicker TMA following an inappropriate shock may reduce the likelihood of further inappropriate shocks due to medical or programming interventions. Although programming or prescribing changes are not necessarily required after an appropriate shock, RM is associated with a reduced TMA by allowing remote assessment of the device and care to be provided to the patient at local hospitals, with specialist device support provided remotely. The ability of RM to reduce TMA has been demonstrated in larger clinical trials[13,14] and the home guide registry[15]. However, it is worth noting that these trials included all device alerts when calculating TMA rather than just shock as is the case here. The ability of RM to reduce TMA and to deliver the same level of care to all patients regardless of geographical location is advantageous.
The reduced number of inappropriate shocks in the RM group is consistent with data from the ECOST and EVATEL trials[11,12]. ICD shocks are known to have both a physical and psychological effect on the patient, including acute pain, anxiety and depression[13], as well as having an adverse effect on the myocardial function, leading to an increased risk of death[16,17]. With these known detrimental effects of shocks it is well recognised that there is a need to reduce the occurrence of inappropriate shocks, in order to increase the quality of life for patients with ICDs and CRT-Ds.
The incidence of inappropriate shocks (all follow up methods) from major clinical trials were compared to the findings in this study. In contemporary trials with clinic follow up inappropriate ICD therapies have been reported in up to 25%-35% of cases[18-20], with more recent trials reporting inappropriate shock rate of 10%-11.5%[3,21], also with clinic follow up. Our study showed an inappropriate shock rate in clinic follow up patients of 11.4%, which is not dissimilar; suggesting that the service patients receive here is comparable to hospitals worldwide. There are fewer trials with inappropriate shock data for patients followed up with RM, but in a recently reported cohort a rate of 3.9% per annum was reported[22], which is identical to the rate in this current study.
The safety of RM compared to clinic follow up has been confirmed by several large clinical trials, such as TRUST[7] and ECOST[11], both of which have evaluated major adverse events to prove the non-inferiority of RM compared to clinic follow up. However, these trials only included those patients with Biotronik’s Home Monitoring system. Although a similar trial by Al-Khatib et al[23] reported similar findings for Medtronic’s Carelink system. Our study included patients with 3 manufacturers (Biotronik, Medtronic, St Jude Medical and Boston scientific/Guidant) with no obvious differences between the four providers although numbers were small.
This was a retrospective single centre study and therefore there is a risk that these results are not generalizable. However, all device follow up in our area is provided at this one site and all device patients were included. Our centre is the only cardiac unit in our region and therefore it is likely that our patient population is representative. A further potential limitation is the study design which was an observational cohort study and not randomised. Nevertheless, the groups although of differing size were similar with regard to demographics and the results are consistent with previous studies. The implant period covered 4 years, with RM perhaps becoming more available/widely adopted in those patients implanted later on in the study and improved experience and medical therapy may have skewed results. The number of inappropriate shocks in both groups is small and this is a statistical limitation of the study. It is also recognised that this study does not include data regarding anti-tachycardia pacing delivered to patients, whilst this would provide additional therapy and arrhythmia information it was out with the scope of this review.
The lower incidence of inappropriate shocks in patients with RM compared to published data is of interest. The geographical location of the study centre in a dispersed population has led to an increase use of RM, perhaps more than other centres and the informal response in terms of staff and patients has been positive.
RM was associated with fewer inappropriate shocks and reduced TMA post shock (for appropriate and inappropriate shock). Inappropriate shocks are known to have detrimental effects on a patient’s quality of life and to increase mortality. For these reasons it is essential that reducing the incidence of inappropriate shocks is a high priority in the continuing care and follow up of patients. More widespread use of RM might lead to a decrease in inappropriate shocks.
Implantable cardioverter defibrillators (ICDs) and cardiac resynchronisation therapy with defibrillators (CRT-D) reduce mortality in certain cardiac patient populations. However, inappropriate shocks pose a problem, having both adverse physical and psychological effects on the patient. The advances in device technology now allow remote monitoring (RM) of devices to replace clinic follow up appointments. This allows real time data to be analysed and actioned and this may improve patient care.
This is because inappropriate shocks and delayed assessment can lead to morbidity and reduced quality of life for patients.
The primary objective was to determine if RM in patients with an ICD is associated with fewer inappropriate shocks and reduced time to medical assessment.
This was a single centre, retrospective observational study, involving 156 patients implanted with an ICD or CRT-D, followed up for 2 years post implant. Both appropriate and inappropriate shocks were recorded along with cause for inappropriate shocks and time to medical assessment.
RM was associated with fewer inappropriate shocks (13.6% clinic vs 3.9% RM; P = 0.030) and a reduced time to medical assessment (15.1 ± 6.8 vs 1.0 ± 0.0 d; P < 0.001).
RM in patients with an ICD is associated with both improved patient outcomes.
The role of RM in other areas should be investigated.
| 1. | Anderson JL, Hallstrom AP, Epstein AE, Pinski SL, Rosenberg Y, Nora MO, Chilson D, Cannom DS, Moore R. Design and results of the antiarrhythmics vs implantable defibrillators (AVID) registry. The AVID Investigators. Circulation. 1999;99:1692-1699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 77] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 2. | Buxton AE, Lee KL, Fisher JD, Josephson ME, Prystowsky EN, Hafley G. A randomized study of the prevention of sudden death in patients with coronary artery disease. Multicenter Unsustained Tachycardia Trial Investigators. N Engl J Med. 1999;341:1882-1890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1796] [Cited by in RCA: 1673] [Article Influence: 62.0] [Reference Citation Analysis (0)] |
| 3. | Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, Domanski M, Troutman C, Anderson J, Johnson G, McNulty SE, Clapp-Channing N, Davidson-Ray LD, Fraulo ES, Fishbein DP, Luceri RM, Ip JH; Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005;352:225-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4998] [Cited by in RCA: 4855] [Article Influence: 231.2] [Reference Citation Analysis (0)] |
| 4. | Kadish A, Dyer A, Daubert JP, Quigg R, Estes NA, Anderson KP, Calkins H, Hoch D, Goldberger J, Shalaby A, Sanders WE, Schaechter A, Levine JH; Defibrillators in Non-Ischemic Cardiomyopathy Treatment Evaluation (DEFINITE) Investigators. Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N Engl J Med. 2004;350:2151-2158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1548] [Cited by in RCA: 1474] [Article Influence: 67.0] [Reference Citation Analysis (0)] |
| 5. | Mabo P, Victor F, Bazin P, Ahres S, Babuty D, Da Costa A, Binet D, Daubert JC; COMPAS Trial Investigators. A randomized trial of long-term remote monitoring of pacemaker recipients (the COMPAS trial). Eur Heart J. 2012;33:1105-1111. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 245] [Cited by in RCA: 254] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 6. | Sack S, Wende CM, Nägele H, Katz A, Bauer WR, Barr CS, Malinowski K, Schwacke H, Leyva F, Proff J, Berdyshev S, Paul V. Potential value of automated daily screening of cardiac resynchronization therapy defibrillator diagnostics for prediction of major cardiovascular events: results from Home-CARE (Home Monitoring in Cardiac Resynchronization Therapy) study. Eur J Heart Fail. 2011;13:1019-1027. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 39] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Guédon-Moreau L, Lacroix D, Sadoul N, Clémenty J, Kouakam C, Hermida JS, Aliot E, Boursier M, Bizeau O, Kacet S; ECOST trial Investigators. A randomized study of remote follow-up of implantable cardioverter defibrillators: safety and efficacy report of the ECOST trial. Eur Heart J. 2013;34:605-614. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 197] [Cited by in RCA: 231] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 8. | Heidbuchel H, Hindricks G, Broadhurst P, Van Erven L, Fernandez-Lozano I, Rivero-Ayerza M, Malinowski K, Marek A, Romero Garrido RF, Löscher S, Beeton I, Garcia E, Cross S, Vijgen J, Koivisto UM, Peinado R, Smala A, Annemans L. EuroEco (European Health Economic Trial on Home Monitoring in ICD Patients): a provider perspective in five European countries on costs and net financial impact of follow-up with or without remote monitoring. Eur Heart J. 2015;36:158-169. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 82] [Cited by in RCA: 81] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 9. | Dyer C. East Kent trust failed to act on risks in maternity care raised by investigators. BMJ. 2020;369:m1445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Powell BD, Saxon LA, Boehmer JP, Day JD, Gilliam FR 3rd, Heidenreich PA, Jones PW, Rousseau MJ, Hayes DL. Survival after shock therapy in implantable cardioverter-defibrillator and cardiac resynchronization therapy-defibrillator recipients according to rhythm shocked. The ALTITUDE survival by rhythm study. J Am Coll Cardiol. 2013;62:1674-1679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 130] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 11. | Guédon-Moreau L, Kouakam C, Klug D, Marquié C, Brigadeau F, Boulé S, Blangy H, Lacroix D, Clémenty J, Sadoul N, Kacet S. Decreased delivery of inappropriate shocks achieved by remote monitoring of ICD: a substudy of the ECOST trial. J Cardiovasc Electrophysiol. 2014;25:763-770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 62] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 12. | Mabo P, Defaye P, Sadoul N. EVATEL: Remote follow up of patients implanted with an ICD: The prospective randomised EVATEL study. Heart Rhythm. 2012;9:S226-S227. |
| 13. | Dario C, Delise P, Gubian L, Saccavini C, Brandolino G, Mancin S. Large Controlled Observational Study on Remote Monitoring of Pacemakers and Implantable Cardiac Defibrillators: A Clinical, Economic and Organizational Evaluation. Interact J Med Res. 2016;5:e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | Crossley GH, Boyle A, Vitense H, Chang Y, Mead RH; CONNECT Investigators. The CONNECT (Clinical Evaluation of Remote Notification to Reduce Time to Clinical Decision) trial: the value of wireless remote monitoring with automatic clinician alerts. J Am Coll Cardiol. 2011;57:1181-1189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 370] [Cited by in RCA: 384] [Article Influence: 25.6] [Reference Citation Analysis (0)] |
| 15. | Ricci RP, Morichelli L, D'Onofrio A, Calò L, Vaccari D, Zanotto G, Curnis A, Buja G, Rovai N, Gargaro A. Effectiveness of remote monitoring of CIEDs in detection and treatment of clinical and device-related cardiovascular events in daily practice: the HomeGuide Registry. Europace. 2013;15:970-977. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 89] [Cited by in RCA: 104] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 16. | Poole JE, Johnson GW, Hellkamp AS, Anderson J, Callans DJ, Raitt MH, Reddy RK, Marchlinski FE, Yee R, Guarnieri T, Talajic M, Wilber DJ, Fishbein DP, Packer DL, Mark DB, Lee KL, Bardy GH. Prognostic importance of defibrillator shocks in patients with heart failure. N Engl J Med. 2008;359:1009-1017. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1224] [Cited by in RCA: 1160] [Article Influence: 64.4] [Reference Citation Analysis (0)] |
| 17. | Moss AJ, Schuger C, Beck CA, Brown MW, Cannom DS, Daubert JP, Estes NA 3rd, Greenberg H, Hall WJ, Huang DT, Kautzner J, Klein H, McNitt S, Olshansky B, Shoda M, Wilber D, Zareba W; MADIT-RIT Trial Investigators. Reduction in inappropriate therapy and mortality through ICD programming. N Engl J Med. 2012;367:2275-2283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1032] [Cited by in RCA: 1096] [Article Influence: 78.3] [Reference Citation Analysis (0)] |
| 18. | Moss AJ, Greenberg H, Case RB, Zareba W, Hall WJ, Brown MW, Daubert JP, McNitt S, Andrews ML, Elkin AD; Multicenter Automatic Defibrillator Implantation Trial-II (MADIT-II) Research Group. Long-term clinical course of patients after termination of ventricular tachyarrhythmia by an implanted defibrillator. Circulation. 2004;110:3760-3765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 474] [Cited by in RCA: 460] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 19. | Wilkoff BL, Hess M, Young J, Abraham WT. Differences in tachyarrhythmia detection and implantable cardioverter defibrillator therapy by primary or secondary prevention indication in cardiac resynchronization therapy patients. J Cardiovasc Electrophysiol. 2004;15:1002-1009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 230] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 20. | Wathen MS, DeGroot PJ, Sweeney MO, Stark AJ, Otterness MF, Adkisson WO, Canby RC, Khalighi K, Machado C, Rubenstein DS, Volosin KJ; PainFREE Rx II Investigators. Prospective randomized multicenter trial of empirical antitachycardia pacing vs shocks for spontaneous rapid ventricular tachycardia in patients with implantable cardioverter-defibrillators: Pacing Fast Ventricular Tachycardia Reduces Shock Therapies (PainFREE Rx II) trial results. Circulation. 2004;110:2591-2596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 584] [Cited by in RCA: 544] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 21. | Daubert JP, Zareba W, Cannom DS, McNitt S, Rosero SZ, Wang P, Schuger C, Steinberg JS, Higgins SL, Wilber DJ, Klein H, Andrews ML, Hall WJ, Moss AJ; MADIT II Investigators. Inappropriate implantable cardioverter-defibrillator shocks in MADIT II: frequency, mechanisms, predictors, and survival impact. J Am Coll Cardiol. 2008;51:1357-1365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 618] [Cited by in RCA: 621] [Article Influence: 34.5] [Reference Citation Analysis (0)] |
| 22. | Bergau L, Willems R, Sprenkeler DJ, Fischer TH, Flevari P, Hasenfuß G, Katsaras D, Kirova A, Lehnart SE, Lüthje L, Röver C, Seegers J, Sossalla S, Dunnink A, Sritharan R, Tuinenburg AE, Vandenberk B, Vos MA, Wijers SC, Friede T, Zabel M. Differential multivariable risk prediction of appropriate shock vs competing mortality - A prospective cohort study to estimate benefits from ICD therapy. Int J Cardiol. 2018;272:102-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 23. | Al-Khatib SM, Piccini JP, Knight D, Stewart M, Clapp-Channing N, Sanders GD. Remote monitoring of implantable cardioverter defibrillators versus quarterly device interrogations in clinic: results from a randomized pilot clinical trial. J Cardiovasc Electrophysiol. 2010;21:545-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 82] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Satoh H, Wetterling F, Zhang LZ S-Editor: Fan JR L-Editor: A P-Editor: Li JH