Published online Jul 26, 2020. doi: 10.4330/wjc.v12.i7.342
Peer-review started: January 30, 2020
First decision: March 24, 2020
Revised: May 10, 2020
Accepted: May 29, 2020
Article in press: May 29, 2020
Published online: July 26, 2020
Processing time: 176 Days and 10.7 Hours
Atrial fibrillation (AF) is the most common cardiac arrhythmia encountered in clinical practice. However, the outcomes associated with AF in hospitalized patients with liver cirrhosis are unknown.
To determine the outcomes of hospitalized patients with liver cirrhosis and AF.
In this study, we examined morbidity and mortality of patients with concomitant AF and liver cirrhosis from the National Inpatient Sample database, the largest publicly available inpatient healthcare database in the United States.
A total of 696937 patients with liver cirrhosis were included, 45745 of whom had concomitant AF (6.6%). Liver cirrhosis patients with AF had higher rates of in-hospital mortality (12.6% vs 10.3%, P < 0.001), clinical stroke (1.6% vs 1.1%, P < 0.001), and acute kidney injury (28.2% vs 25.1%, P < 0.001), and less gastrointestinal bleeding (4.4% vs 5.1%, P < 0.001) and blood transfusion (22.5% vs 23.8%, P < 0.001) compared with those who did not have the arrhythmia. In addition, they had a longer length of stay (8 ± 10 d vs 7 ± 8 d, P < 0.001) and higher hospitalization costs (20720 ± 33210 $ vs 16272 ± 24166 $, P < 0.001).
In subjects with liver cirrhosis, AF is associated with higher rates of inpatient mortality, stroke, and acute kidney injury compared to those who do not have the cardiac arrhythmia.
Core tip: Atrial fibrillation is an adverse prognostic indicator in patients with liver cirrhosis. It is associated with increased inpatient mortality and a higher risk of cerebrovascular attack and renal failure. Furthermore, it leads to a longer hospital stay and admission to an acute care or a rehabilitation facility in this patient population.
- Citation: Darrat YH, Smer A, Elayi CS, Morales GX, Alqahtani F, Alkhouli M, Catanzaro J, Shah J, Salih M. Mortality and morbidity in patients with atrial fibrillation and liver cirrhosis. World J Cardiol 2020; 12(7): 342-350
- URL: https://www.wjgnet.com/1949-8462/full/v12/i7/342.htm
- DOI: https://dx.doi.org/10.4330/wjc.v12.i7.342
Atrial fibrillation (AF) is the most common cardiac rhythm disorder in the general population. It is estimated that 3 million adults in the United States have been diagnosed with the arrhythmia and the prevalence is estimated to rise to 12.1 million in 2030[1]. However, the prevalence and outcomes of AF in patients with liver cirrhosis is not well described. There are only a few relatively small-scale studies that measured its impact in patients with liver cirrhosis, and these show discordant results[2-5]. Furthermore, the mortality rate associated with AF in patients with liver cirrhosis remains not well defined[5,6]. Therefore, conflicting data exist about the prevalence and prognosis of patients with both conditions.
The National Inpatient Sample (NIS) database is the largest publicly available inpatient healthcare database in the United States and provides an opportunity for such a comparison. It is representative of the United States population admitted to the hospital, and also reflects daily practice. Using this data set, we aimed to compare the differences in morbidity, mortality, length of stay (LOS), and trends in patients with liver cirrhosis with and without AF.
The NIS database was used to derive patient-relevant information between January 2003 and December 2014. It is an all-payer administrative claims-based database and contains information about patient discharges from approximately 1000 nonfederal hospitals in 45 states. It contains clinical and resource utilization information on 5 to 8 million discharges annually, with safeguards to protect the privacy of individual patients, physicians, and hospitals. These data are stratified to represent approximately 20% of United States in-patient hospitalizations across different hospitals and geographic regions (random sample). National estimates of the entire United States hospitalized population were calculated using the Agency for Healthcare Research and Quality sampling and weighting method.
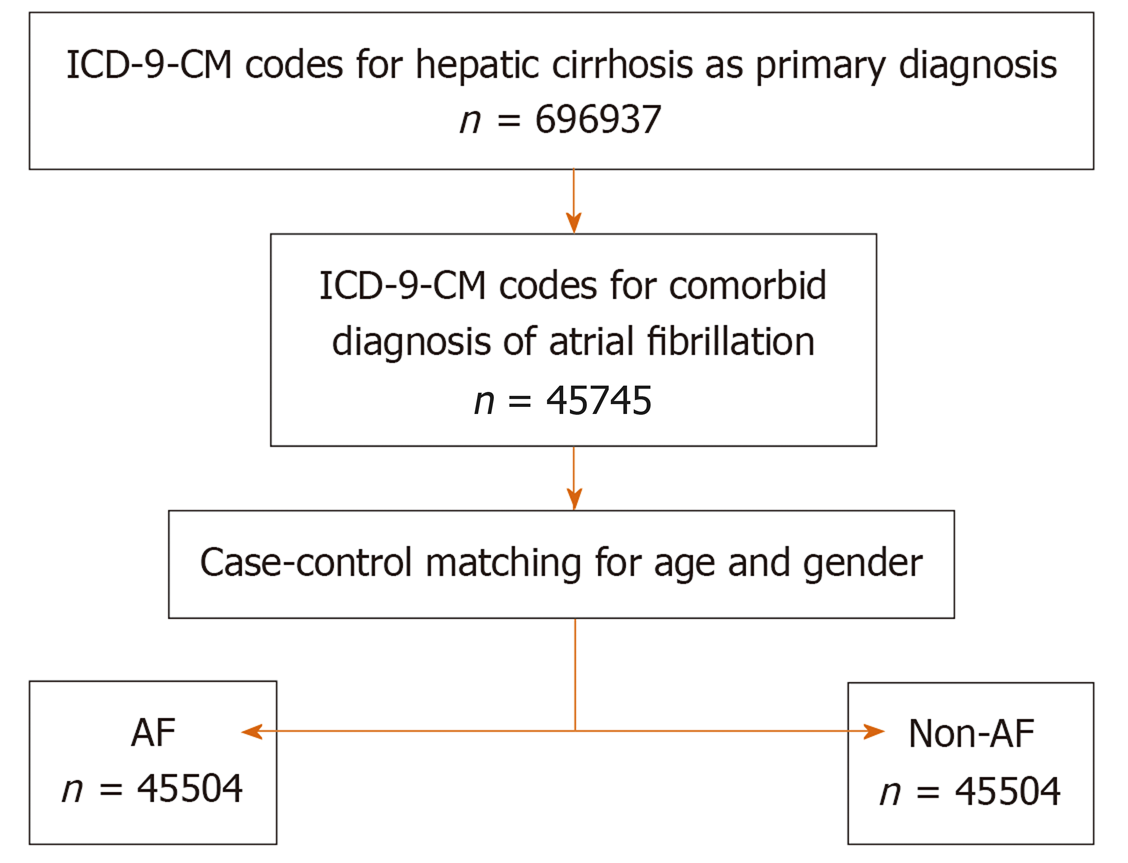
Patients with a discharge diagnosis of hepatic cirrhosis [International Classification of Diseases-Ninth Revision-Clinical Modification (ICD-9-CM) codes 571.2, 571.3, 571, and 572.4] and diagnosis of AF (ICD-9-CM codes 427.31 and 427.32) during the study period were identified. Advanced liver cirrhosis was determined by the presence of hepatic cirrhosis and one or more of the following: Portal hypertension, ascites, hepatic encephalopathy, and hepatorenal syndrome (ICD-9-CM codes 572.3, 789.59, 572.2, and 572.4, respectively). The study flowsheet is presented in Figure 1.
The trends of AF in patients with hepatic cirrhosis during the 12-year study period were assessed using the Cochran–Armitage test for trend. Baseline patient co-morbidities and hospital characteristics were described. In-hospital morbidity, in-hospital outcomes including disposition, and cost of care of AF were assessed. We aimed to perform a comparative analysis based on the presence of AF in patients with liver cirrhosis. We anticipated significant heterogeneity regarding demographic and comorbid characteristics. To account for potential confounding factors and reduce the effect of selection bias, a propensity score matching model was developed using logistic regression to derive two matched groups for comparative outcome analysis using a nearest neighbor 1:1 variable ratio, parallel, balanced propensity matching model using a caliper of 0.01. Propensity scores were derived from multiple clinical and demographic covariates including the Elixhauser comorbidity index (Supplementary Table 1).
The primary endpoint was in-hospital death. Secondary outcomes included cerebral vascular accidents, transient ischemic attack, acute kidney injury, blood transfusion, gastrointestinal bleeding, LOS, hospital charges, and discharge disposition.
Patient-relevant descriptive statistics are presented as frequencies with percentages for categorical variables and as the mean ± SD for continuous variables. Baseline characteristics were compared between the groups using a Pearson chi-square test for categorical variables and an independent- samples t-test for continuous variables. We performed multiple imputations to impute missing values for the race (missing in 13.2% of observations) using the fully conditional specification method (an iterative Markov Chain Monte Carlo algorithm) in SPSS Statistics 24 (IBM Corporation, Armonk, NY, United States). A Cochran-Armitage test was used to evaluate trends of AF in patients with cirrhosis. Matched categorical variables are presented as frequencies with percentages and were compared using the McNemar test. Matched continuous variables are presented as the mean ± SD and were compared using a paired-samples t-test. All statistical analyses were performed using SPSS Statistics 24 and R version 3.3.1 (Bell Laboratories, New Jersey, NJ, United States), and the statistical review of the study was performed by a biomedical statistician.
We identified 696937 patients with a primary diagnosis of hepatic cirrhosis, 45745 of whom had a concomitant diagnosis of AF (6.6%). Patients with AF were older and had more co-morbidities including hypertension, diabetes mellitus, coronary artery disease, chronic pulmonary disease, chronic kidney disease, and peripheral vascular disease. The baseline characteristics of patients with liver cirrhosis categorized by the presence of AF are presented in Table 1.
| Characteristic | Non-AF (n = 651192) | AF (n = 45745) | P value |
| Age (mean ± SD, yr) | 54 ± 11 | 65 ± 11 | < 0.001 |
| Female, n (%) | 171592 (28.3) | 9244 (20.2) | < 0.001 |
| Race, n (%) | < 0.001 | ||
| Caucasian | 343516 (65.8) | 30624 (76.2) | |
| African American | 57718 (11.1) | 3674 (9.1) | |
| Hispanic | 91439 (17.5) | 4130 (10.3) | |
| Medical comorbidity, n (%) | |||
| Hypertension | 215381 (35.7) | 23136 (50.7) | < 0.001 |
| Diabetes mellitus | 126047 (20.8) | 12282 (26.8) | < 0.001 |
| Prior sternotomy | 8602 (1.4) | 2926 (6.4) | < 0.001 |
| Chronic pulmonary disease | 106826 (17.6) | 14176 (31) | < 0.001 |
| Chronic renal failure | 62065 (10.3) | 9884 (21.6) | < 0.001 |
| Anemia | 186205 (30.8) | 13771 (30.1) | 0.004 |
| Chronic alcohol use | 418372 (69.1) | 29194 (63.8) | < 0.001 |
| Hypothyroidism | 35221 (5.8) | 4662 (10.2) | < 0.001 |
| Peripheral vascular disease | 16026 (2.6) | 3518 (7.7) | < 0.001 |
| Smoking | 159957 (26.4) | 8420 (18.4) | < 0.001 |
| Coronary artery disease | 31636 (5.2) | 6994 (15.3) | < 0.001 |
| Hospital characteristic, n (%) | |||
| Teaching hospital | 303751 (50.4) | 22069 (48.4) | < 0.001 |
| Rural area | 57619 (9.6) | 4378 (9.6) | 0.761 |
| Hospital bed-size | < 0.001 | ||
| Small | 72730 (12.1) | 5903 (13) | |
| Medium | 156654 (26) | 11616 (25.5) | |
| Large | 373165 (61.9) | 28057 (61.6) | |
| Primary payer, n (%) | < 0.001 | ||
| Medicare/Medicaid | 350547 (57.9) | 33371 (73) | |
| Private including HMO | 140515 (23.2) | 8278 (18.1) | |
| Self-pay | 72366 (12) | 2287 (5) | |
After accounting for covariates using propensity score matching to patients without AF (Table 2), we found that patients with AF had higher rates of in-hospital mortality (12.6% vs 10.3%, P < 0.001), clinical stroke (1.6% vs 1.1%, P < 0.001), and acute kidney injury (28.2% vs 25.1%, P < 0.001), and less gastrointestinal bleeding (4.4% vs 5.1%, P < 0.001) and blood transfusion (22.5% vs 23.8%, P < 0.001). The outcomes of propensity matched hepatic cirrhosis patients categorized by presence of AF are presented in Table 3.
| Characteristic | Non-AF (n = 45504) | AF (n = 45504) | P value |
| Age (mean ± SD, yr) | 65 ± 11 | 65 ± 11 | 0.827 |
| Female, n (%) | 9174 (20.2) | 9221 (20.3) | 0.703 |
| Race, n (%) | 0.561 | ||
| Caucasian | 34548 (75.9) | 34633 (76.1) | |
| African American | 4314 (9.5) | 4179 (9.2) | |
| Hispanic | 4644 (10.2) | 4692 (10.3) | |
| Medical comorbidity, n (%) | |||
| Hypertension | 23142 (50.9) | 22972 (50.5) | 0.251 |
| Diabetes mellitus | 12456 (27.4) | 12229 (26.9) | 0.091 |
| Prior sternotomy | 2610 (5.7) | 2843 (6.2) | 0.07 |
| Chronic pulmonary disease | 14165 (31.1) | 14051 (30.9) | 0.404 |
| Chronic renal failure | 9595 (21.1) | 9751 (21.4) | 0.192 |
| Anemia | 13623 (29.9) | 13690 (30.1) | 0.634 |
| Chronic alcohol use | 29054 (63.8) | 29060 (63.9) | 0.972 |
| Hypothyroidism | 4456 (9.8) | 4603 (10.1) | 0.103 |
| Peripheral vascular disease | 3420 (7.5) | 3463 (7.6) | 0.592 |
| Smoking | 8264 (18.2) | 8405 (18.5) | 0.222 |
| Coronary artery disease | 6893 (15.1) | 6898 (15.2) | 0.969 |
| Hospital characteristic, n (%) | |||
| Teaching hospital | 22061 (48.5) | 22129 (48.6) | 0.567 |
| Rural area | 41154 (90.4) | 41141 (90.4) | 0.893 |
| Hospital bed-size | 0.253 | ||
| Small | 6062 (13.3) | 5871 (12.9) | |
| Medium | 11469 (25.2) | 11569 (25.4) | |
| Large | 27973 (61.5) | 28064 (61.7) | |
| Primary payer, n (%) | 0.052 | ||
| Medicare/ Medicaid | 33277 (73.1) | 33138 (72.8) | |
| Private including HMO | 8389 (18.4) | 8270 (18.2) | |
| Self-pay | 2101 (4.6) | 2287 (5) | |
| Non-AF (n = 45504) | AF (n = 45504) | P value | |
| Clinical outcome, n (%) | |||
| In-hospital death | 4697 (10.3) | 5755 (12.6) | < 0.001 |
| Gastrointestinal bleeding | 2329 (5.1) | 1995 (4.4) | < 0.001 |
| Blood transfusion | 10841 (23.8) | 10219 (22.5) | < 0.001 |
| Transient ischemic attack | 124 (0.3) | 134 (0.3) | 0.575 |
| Clinical stroke | 496 (1.1) | 722 (1.6) | < 0.001 |
| Acute kidney injury | 11433 (25.1) | 12810 (28.2) | < 0.001 |
| Discharge status, n (%) | < 0.001 | ||
| Discharged home | 27646 (60.8) | 25705 (56.5) | |
| Discharged SNF/NH/IC | 12242 (26.9) | 13114 (28.8) | |
| Length of stay (mean ± SD, d) | 7 ± 8 | 8 ± 10 | < 0.001 |
| Hospital cost (mean ± SD, $) | 16272 ± 24166 | 20720 ± 33210 | < 0.001 |
We performed a regression analysis excluding stroke and acute kidney injury and found that predictors of in-hospital mortality in patients with liver cirrhosis and AF included older age (66-85 years, odds ratio [OR] = 2.014; above 86 years, OR = 2.449), congestive heart failure (CHF; OR = 1.587), and vascular disease (OR = 1.218). In AF patients with a CHA2DS2-VASc score of 2 or higher, there were more with clinical stroke (P < 0.001) and need for blood transfusion (P = 0.018).
Patients with AF had a longer LOS (8 ± 10 d vs 7 ± 8 d, P < 0.001) and higher hospitalization costs (20720 ± 33210 $ vs 16272 ± 24166 $, P < 0.001) compared to those without. They were also less likely to be discharged home and more likely to go to a rehabilitation or acute care facility. The prevalence of AF according to different age groups and gender for in-patients with liver cirrhosis compared to national estimates are presented in Table 4.
| Age (yr) | Gender | AF in liver cirrhosis (%) | AF national estimate (%) |
| < 45 | Male | 1.70 | 1.76 |
| Female | 0.90 | 0.88 | |
| 46-65 | Male | 5.90 | 5.91 |
| Female | 3.20 | 3.16 | |
| 66-85 | Male | 20.00 | 20.03 |
| Female | 16.00 | 15.99 | |
| > 86 | Male | 34.10 | 34.18 |
| Female | 33.50 | 33.60 |
The main finding of this study is that patients with hepatic cirrhosis and concomitant AF are at an increased risk of in-hospital mortality, stroke, and acute kidney injury compared to their counterparts without the arrhythmia. Furthermore, the LOS and cost are higher in this group of patients.
Liver cirrhosis is the eighth leading cause of death in the United States[7] and its prevalence is increasing due to non-alcoholic steatohepatitis[8]. The prevalence of AF in the general population varies based on age as well as the geographic location[9]. This is also true among patients with liver cirrhosis, with an estimated prevalence of AF varying geographically from 0.15% to 10.9%[2-4]. The reported prevalence seems even higher in patients presenting for liver transplant with significant model for end-stage liver disease scores at 42.1%[5]. However, the latest group is sicker and may not be well representative of the overall population. In our study, the prevalence of AF in patients with liver cirrhosis was 6.6%, which is very similar to that based on estimates in the general population according to age and gender as shown in Table 4. This indicates that liver cirrhosis per se is not associated with an increased risk of AF.
Furthermore, in a prospective study that included patients with liver cirrhosis followed for 24 mo, AF occurred in 6.2% and was found to be related to age[10]. Similarly, Gundling et al[3] demonstrated that AF occurred in 16.4% of a sample of patients with liver cirrhosis and correlated with advanced age and co-morbidities including atherosclerotic disease, hyperlipidemia, and diabetes mellitus. Likewise, in our study, patients with hepatic cirrhosis and associated AF had the known risk factors for developing atrial dysrhythmia, including age, hypertension, and diabetes mellitus.
In some previous studies, mortality was not found to be increased in liver cirrhosis patients with AF compared to controls[6,10]. However, the 30-d and 1-year survival rates were found to be lower in patients with a preoperative diagnosis of AF undergoing liver transplant[5]. Besides, a meta-analysis that included 385866 patients with liver cirrhosis showed that AF was associated with a significantly increased mortality risk in cirrhotic patients with the pooled odds ratio of 1.44 (95%CI: 1.36–1.53, I2 = 0%)[11]. Our study has almost double the number of subjects and has shown increased mortality, specifically in hospitalized patients. Furthermore, they were more likely to be admitted to a rehabilitation or an acute care facility, indicating that they tend to be sicker. As seen in other studies[12], we found that CHA2DS2-VASc of 2 or more was associated with a higher risk of stroke. The reasons that AF is linked to higher mortality and morbidity are likely higher rates of stroke and acute kidney injury (AKI). Also, long QT is commonly seen in advanced liver disease and is a strong predictor of increased death[13].
In our study, the risk of gastrointestinal bleeding and blood transfusion is higher in the non-AF group. This finding can be possibly explained using β-blockers in patients with AF, which can be protective in esophageal varices. However, this cannot be inferred from this study since medication use was not captured. The higher rate of AKI may also deter from prescribing anticoagulants and thereby this may lead to less hemorrhage. Also, the use of oral anticoagulants is associated with a higher risk of bleeding in liver cirrhosis due to the presence of thrombocytopenia or increased INR[14]. Therefore, anticoagulants are under-utilized in this population[15], which may explain the higher stroke rate but at the same time a lower bleeding risk.
This study comes with limitations inherent to retrospective analysis[16-19]. Mainly, the NIS database consists of time-limited administrative data that is related to a specific hospitalization. The possibility of incomplete or misclassified diagnoses and procedures, or omitted documentation might have existed. Specifically, important patient-level information could not be retrieved, such as how AF was documented, and the list of medications used (including β-blockers and anticoagulants). We may have also missed patients who were not correctly labeled as having AF or liver cirrhosis, likewise, they may have been misdiagnosed as having either condition. However, the NIS database is the largest administrative United States data set with admission and discharge level information. Therefore, NIS analysis provides the opportunity to compare and reveal patients’ characteristics, diagnoses, and outcomes with a strong statistical power. Even if there might be some coding errors or omissions, these should be minimized by the large number of patients analyzed.
In our investigation, we have included certain medical comorbidities (hypertension, diabetes mellitus, renal failure, chronic obstructive pulmonary disease, anemia, alcohol use, hypothyroidism, peripheral vascular disease, smoking, and coronary artery disease), but other variables that could be associated with measured outcomes were not available, additionally due to the lack of randomization. Therefore, there might have been unmeasured clinical variables related to the outcomes that were not considered. Furthermore, the database does not provide any data after hospital discharge; therefore, long-term outcomes beyond hospital discharge cannot be assessed. However, the data represents real-life inpatient practice and reflects actual hospital outcomes in patients with liver cirrhosis and AF that can guide clinical management as well as policy-making strategies.
AF is a predictor of increased in-hospital-mortality in patients with liver cirrhosis and is associated with a higher risk of stroke and AKI but interestingly less gastrointestinal bleeding and need for blood transfusion. Besides, patients with liver cirrhosis and AF have a longer length of stay and higher cost of hospitalization compared to those who do not have the arrhythmia. It is essential to recognize AF as an adverse prognostic indicator in this population to provide them with an appropriate management strategy and to reduce associated hospitalization costs.
Atrial fibrillation (AF) is the most common arrhythmia encountered in medical practice and is associated with adverse outcomes. However, the outcomes of AF in the special population of patients with liver cirrhosis have not been well studied and the results of several studies are conflicting.
Mortality rate and clinical outcomes of patients with concomitant AF and liver cirrhosis are an integral aspect of clinical decision and policymaking. Realizing the clinical impact of such disorders in a patient paves the path to design prospective studies.
We aimed to investigate if death is higher in patients with liver cirrhosis who have AF and to also assess outcomes during hospitalization. Understanding the outcomes will assist future research in designing prospective studies and randomized trials to improve morbidity and mortality.
In this study, we examined outcomes of patients with concomitant AF and liver cirrhosis from the National Inpatient Sample database, the largest publicly available inpatient healthcare resource in the United States. We investigated inpatient mortality rate as a primary outcome. Secondary outcomes included cerebral vascular accidents, transient ischemic attack, acute kidney injury, blood transfusion, gastrointestinal bleeding, length of stay, hospital charges, and discharge disposition.
Inpatient mortality was found to be higher in patients with concomitant AF and liver cirrhosis compared to patients without the arrhythmia. We also found that it was associated with higher rates of stroke and acute kidney injury, and prolonged hospitalization.
AF is an adverse prognostic indicator in inpatients with liver cirrhosis. It is associated with increased rates of death, stroke, and acute kidney injury but interestingly less gastrointestinal bleeding and need for blood transfusion. Also, it is associated with prolonged hospitalization and increased cost.
Future studies are needed to prospectively investigate the impact of the arrhythmia in liver cirrhosis.
| 1. | Colilla S, Crow A, Petkun W, Singer DE, Simon T, Liu X. Estimates of current and future incidence and prevalence of atrial fibrillation in the U.S. adult population. Am J Cardiol. 2013;112:1142-1147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 760] [Cited by in RCA: 1006] [Article Influence: 77.4] [Reference Citation Analysis (0)] |
| 2. | Zamirian M, Sarmadi T, Aghasadeghi K, Kazemi MB. Liver cirrhosis prevents atrial fibrillation: A reality or just an illusion? J Cardiovasc Dis Res. 2012;3:109-112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Gundling F, Schmidtler F, Zelihic E, Seidl H, Haller B, Ronel J, Löffler N, Schepp W. [Frequency of cardiac arrhythmia in patients with liver cirrhoses and evaluation of associated factors]. Z Gastroenterol. 2012;50:1149-1155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Bargehr J, Trejo-Gutierrez JF, Patel T, Rosser B, Aranda-Michel J, Yataco ML, Taner CB. Preexisting atrial fibrillation and cardiac complications after liver transplantation. Liver Transpl. 2015;21:314-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 5. | Vannucci A, Rathor R, Vachharajani N, Chapman W, Kangrga I. Atrial fibrillation in patients undergoing liver transplantation-a single-center experience. Transplant Proc. 2014;46:1432-1437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Lee H, Choi EK, Rhee TM, Lee SR, Lim WH, Kang SH, Han KD, Cha MJ, Oh S. Cirrhosis is a risk factor for atrial fibrillation: A nationwide, population-based study. Liver Int. 2017;37:1660-1667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 55] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 7. | Murray CJ, Atkinson C, Bhalla K, Birbeck G, Burstein R, Chou D, Dellavalle R, Danaei G, Ezzati M, Fahimi A, Flaxman D, Foreman, Gabriel S, Gakidou E, Kassebaum N, Khatibzadeh S, Lim S, Lipshultz SE, London S, Lopez, MacIntyre MF, Mokdad AH, Moran A, Moran AE, Mozaffarian D, Murphy T, Naghavi M, Pope C, Roberts T, Salomon J, Schwebel DC, Shahraz S, Sleet DA, Murray, Abraham J, Ali MK, Atkinson C, Bartels DH, Bhalla K, Birbeck G, Burstein R, Chen H, Criqui MH, Dahodwala, Jarlais, Ding EL, Dorsey ER, Ebel BE, Ezzati M, Fahami, Flaxman S, Flaxman AD, Gonzalez-Medina D, Grant B, Hagan H, Hoffman H, Kassebaum N, Khatibzadeh S, Leasher JL, Lin J, Lipshultz SE, Lozano R, Lu Y, Mallinger L, McDermott MM, Micha R, Miller TR, Mokdad AA, Mokdad AH, Mozaffarian D, Naghavi M, Narayan KM, Omer SB, Pelizzari PM, Phillips D, Ranganathan D, Rivara FP, Roberts T, Sampson U, Sanman E, Sapkota A, Schwebel DC, Sharaz S, Shivakoti R, Singh GM, Singh D, Tavakkoli M, Towbin JA, Wilkinson JD, Zabetian A, Murray, Abraham J, Ali MK, Alvardo M, Atkinson C, Baddour LM, Benjamin EJ, Bhalla K, Birbeck G, Bolliger I, Burstein R, Carnahan E, Chou D, Chugh SS, Cohen A, Colson KE, Cooper LT, Couser W, Criqui MH, Dabhadkar KC, Dellavalle RP, Jarlais, Dicker D, Dorsey ER, Duber H, Ebel BE, Engell RE, Ezzati M, Felson DT, Finucane MM, Flaxman S, Flaxman AD, Fleming T, Foreman, Forouzanfar MH, Freedman G, Freeman MK, Gakidou E, Gillum RF, Gonzalez-Medina D, Gosselin R, Gutierrez HR, Hagan H, Havmoeller R, Hoffman H, Jacobsen KH, James SL, Jasrasaria R, Jayarman S, Johns N, Kassebaum N, Khatibzadeh S, Lan Q, Leasher JL, Lim S, Lipshultz SE, London S, Lopez, Lozano R, Lu Y, Mallinger L, Meltzer M, Mensah GA, Michaud C, Miller TR, Mock C, Moffitt TE, Mokdad AA, Mokdad AH, Moran A, Naghavi M, Narayan KM, Nelson RG, Olives C, Omer SB, Ortblad K, Ostro B, Pelizzari PM, Phillips D, Raju M, Razavi H, Ritz B, Roberts T, Sacco RL, Salomon J, Sampson U, Schwebel DC, Shahraz S, Shibuya K, Silberberg D, Singh JA, Steenland K, Taylor JA, Thurston GD, Vavilala MS, Vos T, Wagner GR, Weinstock MA, Weisskopf MG, Wulf S, Murray; U. S. Burden of Disease Collaborators. The state of US health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310:591-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1691] [Cited by in RCA: 1886] [Article Influence: 145.1] [Reference Citation Analysis (1)] |
| 8. | Kabbany MN, Conjeevaram Selvakumar PK, Watt K, Lopez R, Akras Z, Zein N, Carey W, Alkhouri N. Prevalence of Nonalcoholic Steatohepatitis-Associated Cirrhosis in the United States: An Analysis of National Health and Nutrition Examination Survey Data. Am J Gastroenterol. 2017;112:581-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 184] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 9. | Darrat YH, Shah J, Elayi CS, Morales GX, Naditch-Brûlé L, Brette S, Taniou C, Kowey PR, Schwartz PJ. Regional Lack of Consistency in the Management of Atrial Fibrillation (from the RECORD-AF Trial). Am J Cardiol. 2017;119:47-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Mwalitsa JP, Maimone S, Filomia R, Alibrandi A, Saitta C, Caccamo G, Cacciola I, Spinella R, Oliva G, Lembo T, Vadalà D, Gambino G, Raimondo G, Squadrito G. Atrial fibrillation in patients with cirrhosis. Liver Int. 2016;36:395-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Chokesuwattanaskul R, Thongprayoon C, Bathini T, O'Corragain OA, Sharma K, Preechawat S, Wijarnpreecha K, Kröner PT, Ungprasert P, Cheungpasitporn W. Epidemiology of atrial fibrillation in patients with cirrhosis and clinical significance: a meta-analysis. Eur J Gastroenterol Hepatol. 2019;31:514-519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 12. | Cho MS, Lee CH, Kim J, Ahn JM, Han M, Nam GB, Choi KJ, Kim YH. Clinical Implications of Preoperative Nonvalvular Atrial Fibrillation with Respect to Postoperative Cardiovascular Outcomes in Patients Undergoing Non-Cardiac Surgery. Korean Circ J. 2020;50:148-159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Kim SM, George B, Alcivar-Franco D, Campbell CL, Charnigo R, Delisle B, Hundley J, Darrat Y, Morales G, Elayi SC, Bailey AL. QT prolongation is associated with increased mortality in end stage liver disease. World J Cardiol. 2017;9:347-354. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 14. | Niizuma H, Suzuki J, Yonemitsu T, Otsuki T. Spontaneous intracerebral hemorrhage and liver dysfunction. Stroke. 1988;19:852-856. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 38] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Kuo L, Chao TF, Liu CJ, Lin YJ, Chang SL, Lo LW, Hu YF, Tuan TC, Liao JN, Chung FP, Chen TJ, Lip GYH, Chen SA. Liver Cirrhosis in Patients With Atrial Fibrillation: Would Oral Anticoagulation Have a Net Clinical Benefit for Stroke Prevention? J Am Heart Assoc. 2017;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 81] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 16. | Ogunbayo GO, Charnigo R, Darrat Y, Shah J, Patel R, Suffredini J, Wilson W, Parrott K, Kusterer N, Biase LD, Natale A, Morales G, Elayi CS. Comparison of Complications of Catheter Ablation for Ventricular Arrhythmias in Adults With Versus Without Structural Heart Disease. Am J Cardiol. 2018;122:1345-1351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Elayi CS, Darrat Y, Suffredini JM, Misumida N, Shah J, Morales G, Wilson W, Bidwell K, Czarapata M, Parrott K, Di Biase L, Natale A, Ogunbayo GO. Sex differences in complications of catheter ablation for atrial fibrillation: results on 85,977 patients. J Interv Card Electrophysiol. 2018;53:333-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 18. | Ogunbayo GO, Charnigo R, Darrat Y, Morales G, Kotter J, Olorunfemi O, Elbadawi A, Sorrell VL, Smyth SS, Elayi CS. Incidence, predictors, and outcomes associated with pneumothorax during cardiac electronic device implantation: A 16-year review in over 3.7 million patients. Heart Rhythm. 2017;14:1764-1770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 19. | Romero J, Ogunbayo G, Elayi SC, Darrat Y, Rios SA, Diaz JC, Alviz I, Cerna L, Gabr M, Chernobelsky E, Mohanty S, Trivedi CG, Della Rocca DG, Natale A, Di Biase L. Safety of catheter ablation for atrial fibrillation in the octogenarian population. J Cardiovasc Electrophysiol. 2019;30:2686-2693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Invited manuscript
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fedeli U, Gulel O, Vidal-Perez R S-Editor: Ma YJ L-Editor: Wang TQ E-Editor: Wu YXJ