Published online Nov 26, 2020. doi: 10.4330/wjc.v12.i11.571
Peer-review started: August 21, 2020
First decision: October 5, 2020
Revised: October 21, 2020
Accepted: October 30, 2020
Article in press: October 30, 2020
Published online: November 26, 2020
Processing time: 97 Days and 4.7 Hours
Complications of transcatheter aortic valve implantation (TAVI) procedures include bleeding, vascular complications, and strokes. These complications are often associated with the type of access used. The two types of access in TAVI procedures are primary and secondary. The main use of the primary access is for valve delivery, while secondary access is used for angiography and hemodynamic monitoring. While there are many options for primary access, those for secondary access are transfemoral and transradial.
To compare outcomes between transradial vs transfemoral secondary access (TFSA).
A systematic search was conducted using major databases (EMBASE, PubMed, Cochrane Central, Google Scholar), which resulted in 5 studies that met the criteria for study selection. Outcomes of interest were 30-d rates each of major/life-threatening bleeding, vascular complications, strokes, and mortality. All 5 studies were observational. Only adjusted or matched data were used when available in this meta-analysis.
A total of 5065 patients underwent TAVI, with 1453 patients (28.7%) having undergone transradial secondary access (TRSA) and 3612 patients (71.3%) TFSA. Irrespective of the site of primary access, the odds of having major or life-threatening bleeding were 60% lower in the TRSA group than the TFSA group (P < 0.00001). The odds of having major vascular complications were 52% lower in the TRSA group (P < 0.0001) with no difference in minor vascular complications between the 2 groups. Similarly, the odds of mortality in 30-d after the procedure were 41% lower (P = 0.006) and the odds of stroke were 54% lower (P = 0.001) in the TRSA group than the TFSA group.
The transradial secondary approach appears to be a safer alternative to the transfemoral secondary approach in TAVI procedures.
Core Tip: Transcatheter aortic valve implantation (TAVI) procedures can result in complications due to secondary access site. This meta-analysis looks into 5 observational studies that compared outcomes in TAVI related to secondary access. The outcomes included 30-d bleeding, vascular complications, strokes, and mortality. Meta-analysis showed decreased odds of outcomes when transradial secondary access was used over transfemoral.
- Citation: Radhakrishnan SL, Ho KKL. Transradial vs transfemoral secondary access outcomes in transcatheter aortic valve implantation: A systematic review and meta-analysis. World J Cardiol 2020; 12(11): 571-583
- URL: https://www.wjgnet.com/1949-8462/full/v12/i11/571.htm
- DOI: https://dx.doi.org/10.4330/wjc.v12.i11.571
The transcatheter aortic valve implantation (TAVI) procedure is a promising alternative to surgical aortic valve replacement in patients with aortic stenosis. As with any procedure, TAVI is not without complications. Bleeding, vascular complications, and strokes are some of the most common adverse events associated with TAVI. These complications are often associated with the type of access used in the procedure.
TAVI utilizes two vascular access sites—primary and secondary. The valve itself is delivered through the primary access site, while the secondary access site is used for the introduction of catheters for angiography, aiding in device placement, and obtaining invasive hemodynamic data[1]. Options for primary access include transfemoral, transaortic, transapical, and subclavian, among others, out of which transfemoral has been the most popular. The two main sites used for secondary access are the contralateral femoral artery and either radial artery. Historically, the transfemoral site was chosen as the preferred secondary access site. However, during recent years, the transradial site has shown promising results with lower complication rates. There are a handful of studies, mostly with relatively small sample sizes, directly comparing outcomes in transfemoral (TF) and transradial (TR) access sites[1-6]. These studies have suggested that the transradial site for secondary access has better outcomes than the transfemoral site for bleeding and vascular complications. The aim of this review is to pool data from available relevant studies to compare outcomes between TR and TF secondary accesses.
This study was registered on PROSPERO on May 7, 2020, and the meta-analysis was conducted using PRISMA guidelines. A comprehensive literature search was conducted through June 10, 2020 using PubMed, EMBASE, Google Scholar, and Cochrane databases. Search words included “transfemoral vs transradial secondary access in transcatheter aortic valve replacement” and “radial vs femoral secondary access in TAVI.” Literature search was conducted independently by two investigators (Radhakrishnan SL and Darmoch F—see acknowledgement) using the above search strategy. There was uniform agreement between both investigators on what studies to include and exclude, resulting in a kappa correlation of 1.
All observational or experimental trials which aimed at comparing data related to secondary access in patients who underwent TAVI were considered in this review, irrespective of primary access. We included studies if they reported data comparing outcomes between transradial and transfemoral secondary access. Studies considered had to include tables comparing demographics and other baseline characteristics and outcomes. The outcomes considered for the purpose of this review were 30-d all-cause mortality, 30-d stroke, 30-d bleeding complications, and 30-d vascular complications. Studies were included if they reported at least one of the four outcomes in the format desired (comparing TR vs TF).
Studies that did not meet inclusion criteria based on title were excluded. Studies that did not report data specifically related to secondary access in TAVI procedures in the format desired were also excluded. Letters to the editor, abstracts, and posters were excluded.
Statistical analysis was performed using Review Manager 5.3. Subgroup analysis was only done if data were reported in at least four studies to increase confidence in the findings. The test statistic calculated in this meta-analysis was the odds ratio. A random-effect model was chosen over a fixed-effect model since the underlying population in each study was thought to be different. Heterogeneity was determined by the I2 value to describe the percentage of variability due to heterogeneity rather than due to sampling bias. The higher the I2 value, the higher the heterogeneity. That is, an I2 of < 50% indicates more similarity between studies. A P value of 0.05 or less was considered to be significant for all test statistics. Funnel plots were created to assess for evidence of bias and to determine heterogeneity. Results are expressed as mean ± standard deviation, with 95% confidence intervals for odds ratio denoted by square brackets.
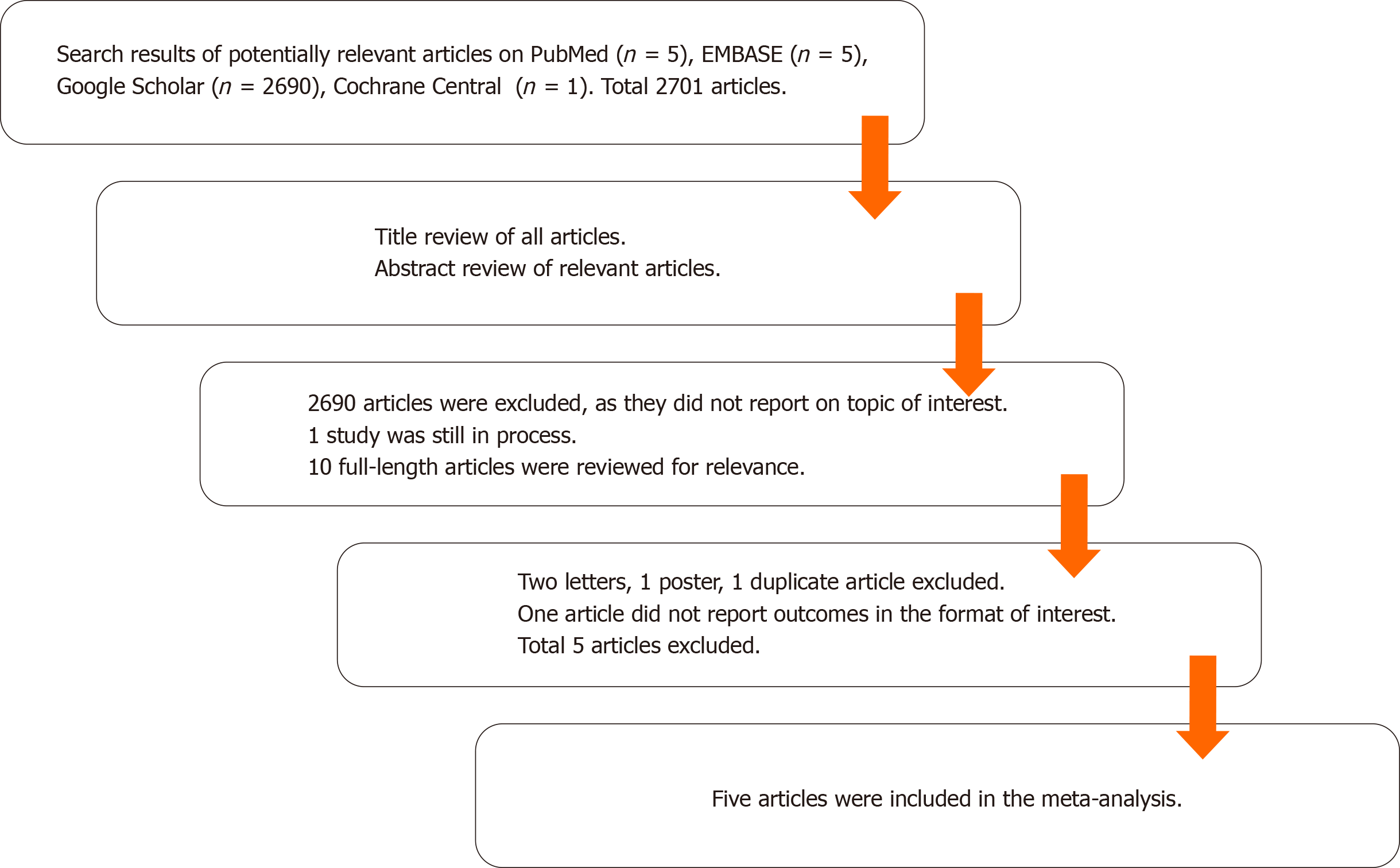
Using the search strategy described above resulted in 2701 articles (2690 from Google scholar, 5 from PubMed, 5 from Embase, and 1 from Cochrane Central). Of these, 2690 articles were excluded after title and/or abstract review, and 1 trial was still in process and unpublished. Each of the remaining 10 articles was reviewed in full. Of these, 2 letters, 1 poster, and 1 duplication were excluded. Although a study by Wynne et al[1] was an observational study which focused on the topic of interest, results reported were not dichotomized based on the type of secondary access and hence excluded from the meta-analysis. Five remaining studies were included in the meta-analysis[2-6]. Detailed results of the search strategy are outlined in Figure 1.
All 5 studies included were observational cohort studies. Definitions of bleeding and vascular events were based on Valve Academic Research Consortium-2 (VARC-2) criteria in 4 studies and the original VARC criteria in 1 study (Curran et al[3]). All studies provided outcomes comparing transradial secondary access (TRSA) with transfemoral secondary access (TFSA). The primary access was solely femoral in 2 studies (Fernandez-Lopez et al[6] and Curran et al[3]). Allende et al[4] and Jackson et al[5] reported data on all primary accesses (APA, i.e., femoral and non-femoral primary accesses) with distinction in comparative outcomes based on transfemoral primary access (TFPA) vs non-TFPA. In Junquera et al[2], the study included APA subjects. However, it did not separately provide comparative data on TFPA subjects. Due to the lack of uniformity in the type of primary access, most of the analyses in the study mainly focused on APA. The 2 studies that reported only TFPA outcomes were considered as APA for practical purposes. A separate analysis was also done for TFPA alone, thus excluding Junquera et al[2]. Relevant study characteristics are outlined in Table 1.
| Junquera et al[2] | Fernandez-Lopez et al[6] | Jackson et al[5] | Allende et al[4] | Curran et al[3] | |
| Study details | |||||
| Year of publication | 2020 | 2018 | 2018 | 2014 | 2014 |
| Country of origin | Multinational (Canada, Europe) | France | The United Kingdom | Canada | Italy |
| Number of centers | Multicenter | Single center | Single center | Single center | Single center |
| Study design | Retrospective and prospective cohort study | Retrospective and prospective cohort study | Retrospective cohort study | Retrospective cohort study | Retrospective cohort study |
| Study subjects | A total of 4949 patients who underwent TAVI between 2007 and 2018 in 10 tertiary centers were included. Selection of secondary access was up to the heart team. 3906 subjects had matched outcomes | Retrospective cohort of 194 patients underwent TFSA TAVI between Sept 2015 and Apr 2016. Prospective cohort of 217 pts underwent TRSA TAVI between April 2016 and May 2017 | All consecutive TAVI cases between May 2015 and June 2017 included. Default TRSA used for all non-TF TAVIs from Jan 2016. Prior to this, secondary access was selected based on clinical grounds | Consecutive patients who underwent TAVI from 2007 to 2014 enrolled. From May 2007-Jan 2013, TFSA was chosen. From Jan 2013 onwards, TRSA was chosen in TFPA TAVI and some non-TFPA TAVI | A total of 87 consecutive patients who underwent TFPA TAVI between June 2011 and March 2012 were included in the study. The first 46 TRSA candidates and 41 TFSA candidates were considered |
| Primary access | TF + non-TF | TF only | TF + non-TF | TF + non-TF | TF only |
| Total No. of study subjects (APA) with matched or adjusted data if available | 3906 (TRSA = 928, TFSA = 2978) | 411 (TRSA = 217, TFSA = 194) | 199 (TRSA = 135, TFSA = 64) | 462 (TRSA = 127, TFSA = 335) | 87 (TRSA = 46, TFSA = 41) |
| Total No. of study subjects (TFPA) with matched or adjusted data | NA | 411 (TRSA = 217, TFSA = 194) | 179 (TRSA = 115, TFSA = 64) | 221 (TRSA = 118, TFSA = 103) | 87 (TRSA = 46, TFSA = 41) |
| Definition of bleeding and vascular events | VARC-2 criteria | VARC-2 criteria | VARC-2 criteria | VARC-2 criteria | Original VARC criteria |
| Limitations of study | Nonrandomized study | (1) Non-randomized study; (2) Relatively small sample size; (3) TFSA technique was novel resulting in a learning curve | (1) Non-randomized study; (2) Relatively small sample size; (3) Unclear if there was a difference in the populations (risk adjustment not reported) | (1) Non-randomized study; (2) Relatively small sample size; (3) Low use of percutaneous closure devices (13%) for obtaining hemostasis in TFSA | (1) Non-randomized study; (2) Relatively small sample size; (3) TFSA technique was novel resulting in a learning curve |
| Was risk-adjustment done? | Both unadjusted and propensity score-matched data available | Adjusted for age, Euroscore, BMI, NYHA class, type, and size of valve | Not reported | Adjusted for gender and peripheral disease | Not reported |
| TAVI Procedure details | |||||
| Hemostasis of PA | TFPA—Percutaneous in 76.3%, surgical cutdown in 23.7% | TFPA—ProGlide device | TFPA—2 ProGlide devices | TFPA—surgical cutdown | NA |
| Hemostasis of TF secondary access | Manual compression (24%), ProGlide (39%), Angio-Seal (37%) | Angio-Seal or ProGlide | NA | Manual compression (87%), ProGlide (8%), Angio-Seal (5%) | NA |
| Post-closure angiography? | No angiography was performed systematically in TFPA |
Of the 5 studies, risk adjustment in some manner was reported in 3 of 5 studies. When available, matched/adjusted scores were used; however, if no adjustment or matching was reported, the study was still included in this review. Allende et al[4] adjusted data for differences in gender and peripheral disease. Fernandez-Lopez et al[6] reported that results were adjusted for age, Euroscore, body mass index, New York Heart Association (NYHA) functional class, type and size of valve. Junquera et al[2] reported both overall unadjusted data and propensity score-matched data. Jackson et al[5] and Curran et al[3] did not report having performed specific risk adjustment or matching.
In Junquera et al[2], both unadjusted as well as propensity score-matched data were reported. For the purpose of this study, only propensity score-matched data was included.
A total of 5065 patients underwent TAVI inclusive of APA, with 1453 patients (28.7%) having TRSA and 3612 patients (71.3%) having TFSA. A secondary analysis was conducted in patients that underwent TAVI with TFPA. Four out of 5 studies qualified for the TFPA sub-group analysis. The total population of this cohort was 898 patients, out of which 496 patients (55.2%) underwent TRSA and 402 (44.8%) patients underwent TFSA.
Baseline demographics in each study are compared in Table 2. The mean age of the study population was 81.1 ± 7.2 in the TFSA group and 81.3 ± 7.1 in the TRSA group. Forty six percent (46%) were males in the TFSA group and 53% in the TRSA group. Atrial fibrillation was present in 26% of subjects in the TFSA group and 28% in the TRSA group. The mean STS-PROM score was 6.4 in the TFSA group and 6.0 in the TRSA group.
| Junquera et al[2] | Fernandez-Lopez et al[6] | Jackson et al[5] | Allende et al[4] | Curran et al[3] | ||||||
| TFSA (n = 2978) | TRSA (n = 928) | TFSA (n = 194) | TRSA (n = 217) | TFSA (n = 64) | TRSA (n = 135) | TFSA (n = 335) | TRSA (n = 127) | TFSA (n = 41) | TRSA (n = 46) | |
| Baseline characteristics of patients | ||||||||||
| Age | 81 ± 4 | 81 ± 8 | 83 ± 7 | 82 ± 6 | 82 ± 6 | 82 ± 7 | 79 ± 8 | 80 ± 9 | 80 ± 10 | 80 ± 5 |
| %Male | 52.60% | 53.20% | 44.80% | 53.50% | 57.00% | 43.00% | 45.00% | 61.00% | 31.70% | 52.20% |
| Baseline comorbidities | ||||||||||
| Diabetes | 26.90% | 27.00% | 31.40% | 24.40% | 20.00% | 20.00% | 35.00% | 31.00% | 30.00% | 26.10% |
| HTN | - | - | 56.70% | 55.30% | - | - | 88.00% | 84.00% | 92.50% | 80.40% |
| CAD | 51.20% | 50.30% | - | - | 53.00% | 52.60% | 67.00% | 63.00% | - | - |
| Previous CABG | 19.80% | 19.60% | 4.10% | 6.00% | 20.00% | 19.30% | 39.00% | 33.00% | 17.10% | 17.40% |
| AFib | 33.50% | 34.70% | 27.80% | 33.60% | 25.00% | 25.00% | 17.00% | 20.00% | - | - |
| PVD | 16.30% | 19.20% | 13.40% | 14.30% | 18.00% | 26.70% | 40.00% | 24.00% | - | - |
| Prior CVA | - | - | 10.30% | 10.60% | 17.00% | 16.30% | 19.00% | 16.00% | - | - |
| eGFR < 60 mL/min/1.73 m2 | 67.60% | 69.40% | - | - | - | - | 57.00% | 51.00% | - | - |
| COPD/Pul disease | 21.30% | 20.90% | 11.90% | 13.40% | 25.00% | 25.90% | 29.00% | 25.00% | 20.00% | 13.00% |
| STS-PROM score | 4.5 | 4.7 | 5.0 ± 3.0 | 4.8 ± 3.6 | - | - | 7.1 ± 4.5 | 7.2 ± 5.0 | 9.0 ± 7.8 | 7.2 ± 7.5 |
| Valve type | ||||||||||
| Balloon-expandable | 60.00% | 63.50% | NA | NA | NA | NA | 96.00% | 88.00% | NA | NA |
| Self-expandable | 40.00% | 36.50% | NA | NA | NA | NA | 3.00% | 10.00% | NA | NA |
| 1° Access | ||||||||||
| TFPA | 88.50% | 89.90% | 100% | 100% | 100% | 85.20% | 30.80% | 93.00% | 100% | 100% |
| Non-TFPA | 11.50% | 10.10% | 0 | 0 | 0 | 14.80% | 69.20% | 7.00% | 0 | 0 |
| Transapical | 9.10% | 3.70% | 58.20% | 6.00% | ||||||
| Transaortic | 1.90% | 8.80% | 10.70% | 1.00% | ||||||
| Subclavian | 1.50% | 2.20% | 0.30% | 0 | ||||||
| Transcarotid | 4.06% | 0 | 0 | 0 | ||||||
| Transcaval | 0.12% | 0 | 0 | 0 | ||||||
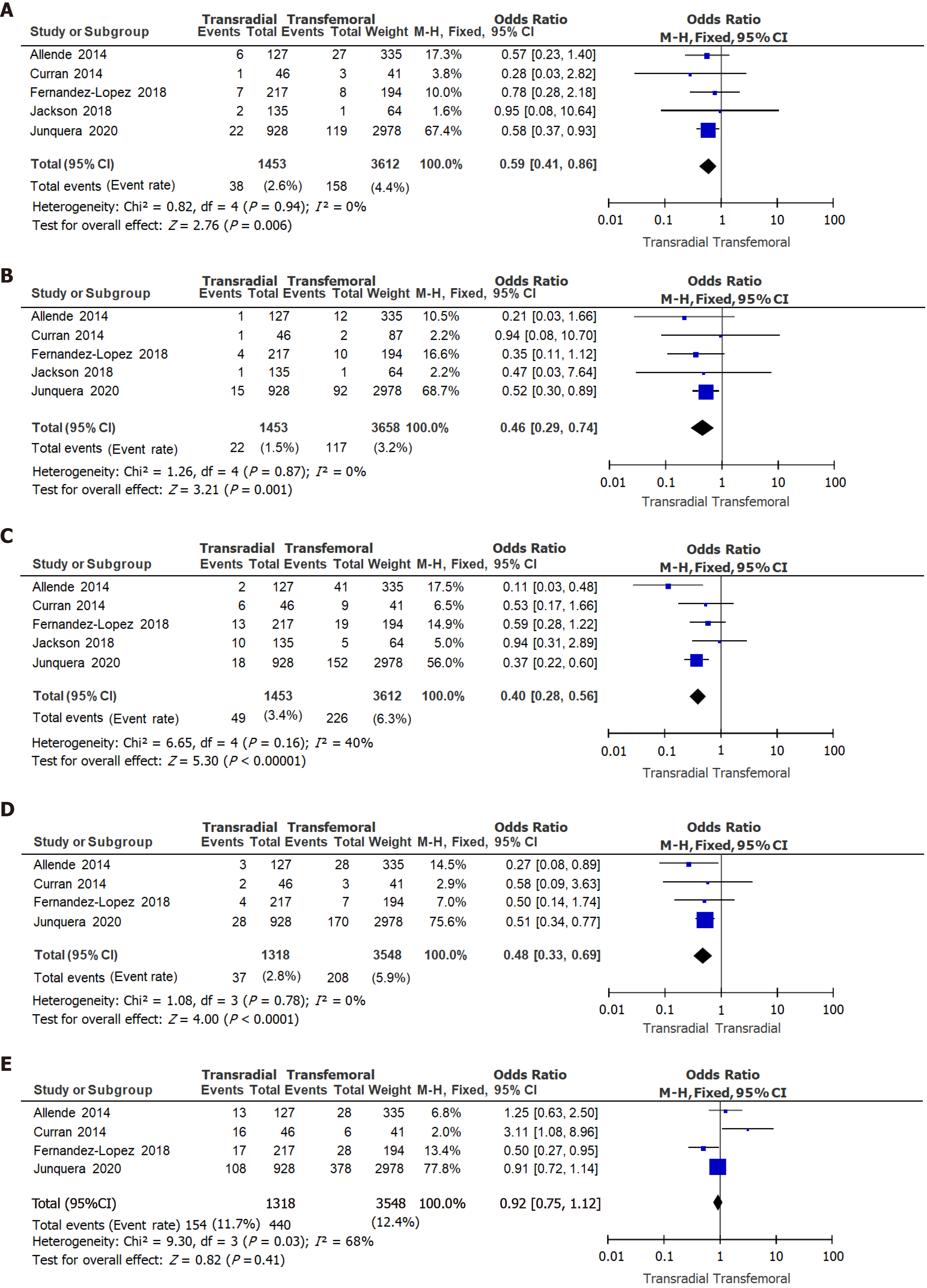
All-cause mortality: When APA-TAVI procedures were considered, the 30-d all-cause mortality rate was 2.6% in the TRSA group and 4.4% in the TFSA group, odds ratio (OR) 0.59 [0.41, 0.86] (P = 0.006, Figure 2A).
Stroke: The 30-d stroke rate was 1.5% in the TRSA group and 3.2% in the TFSA group, OR 0.45 [0.29, 0.74] (P = 0.001, Figure 2B).
Bleeding complications: The incidence of major and life-threatening bleeding complications by 30 d post-TAVI was 3.4% in TRSA patients and 6.3% in TFSA, OR 0.40 [0.28, 0.56] (P < 0.00001, Figure 2C).
Vascular complications: Major vascular complications by 30 d post-TAVI were seen in 2.8% of TRSA patients and 5.9% in TFSA, OR 0.48 [0.33, 0.69] (P < 0.0001, Figure 2D). The incidence of 30-d minor vascular complications was 11.7% in TRSA patients and 12.4% in TFSA, OR 0.92 [0.75, 1.12] (P = 0.41, Figure 2E).
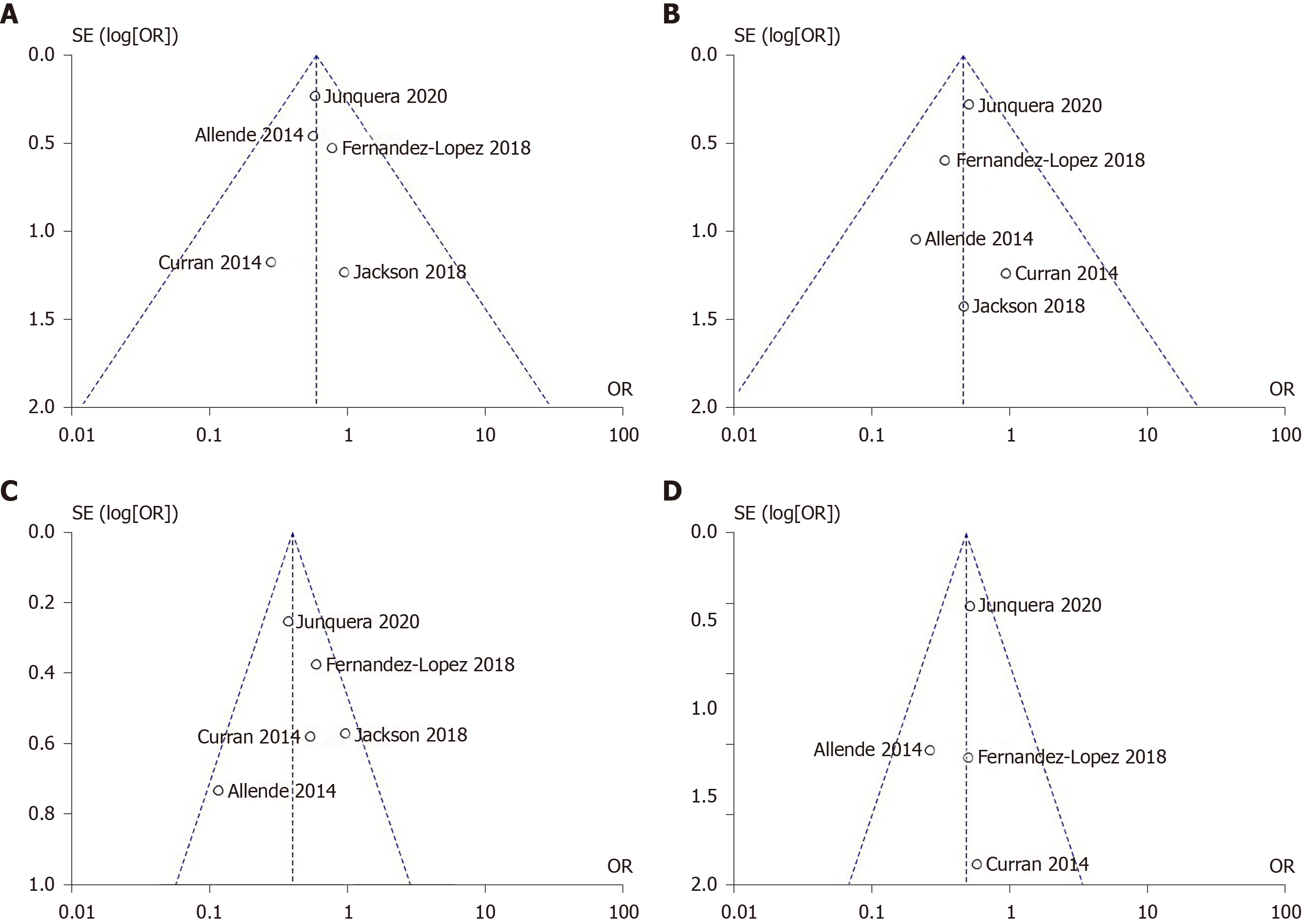
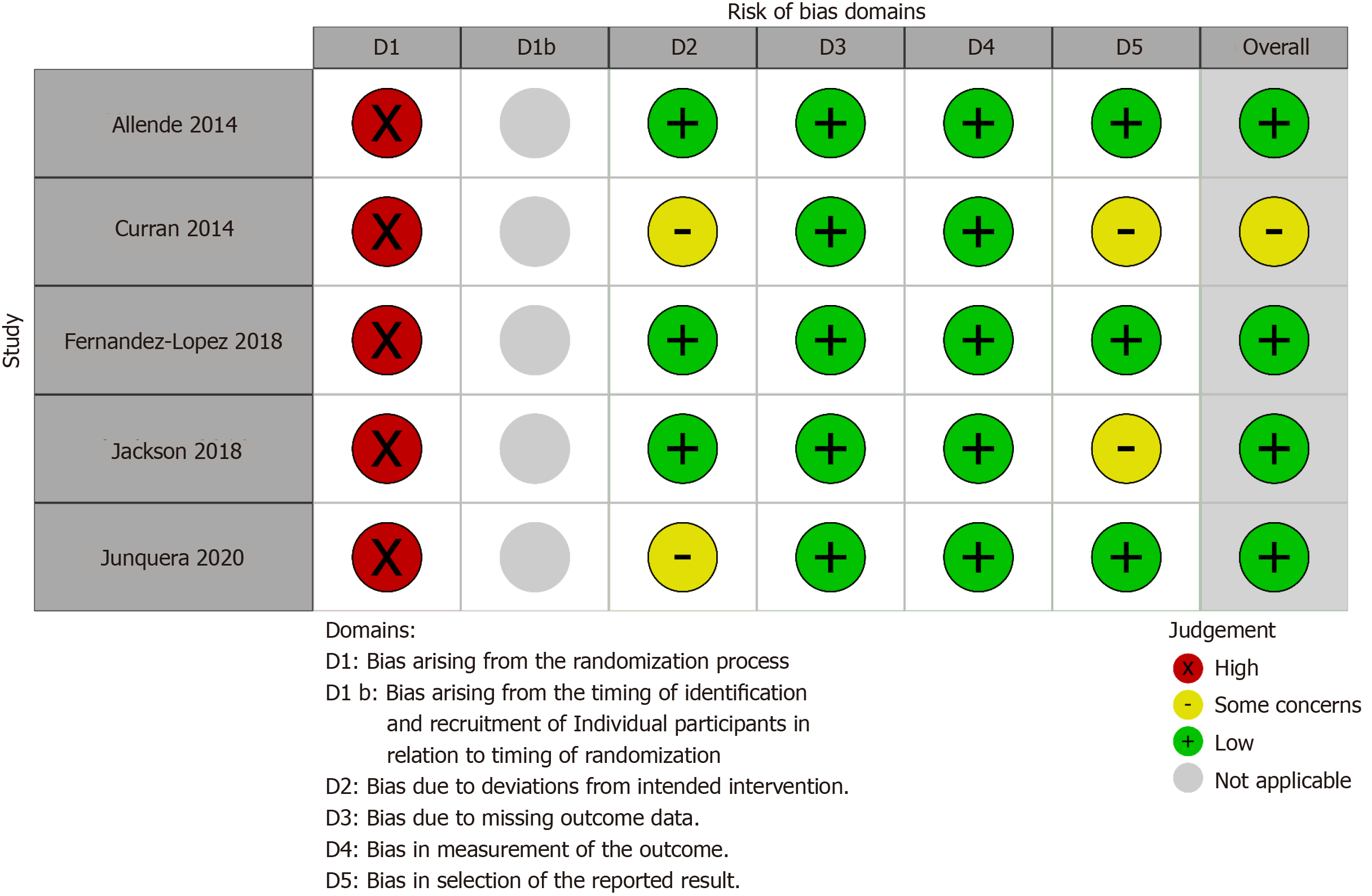
Figure 3 shows funnel plots for the main outcomes. The plots were symmetric, and all studies lie within the triangular region, close to the mean, without outliers. This indicates minimal heterogeneity in this review. Figure 4 shows traffic light plots of the domain-level judgements for each individual result to assess risk of bias.
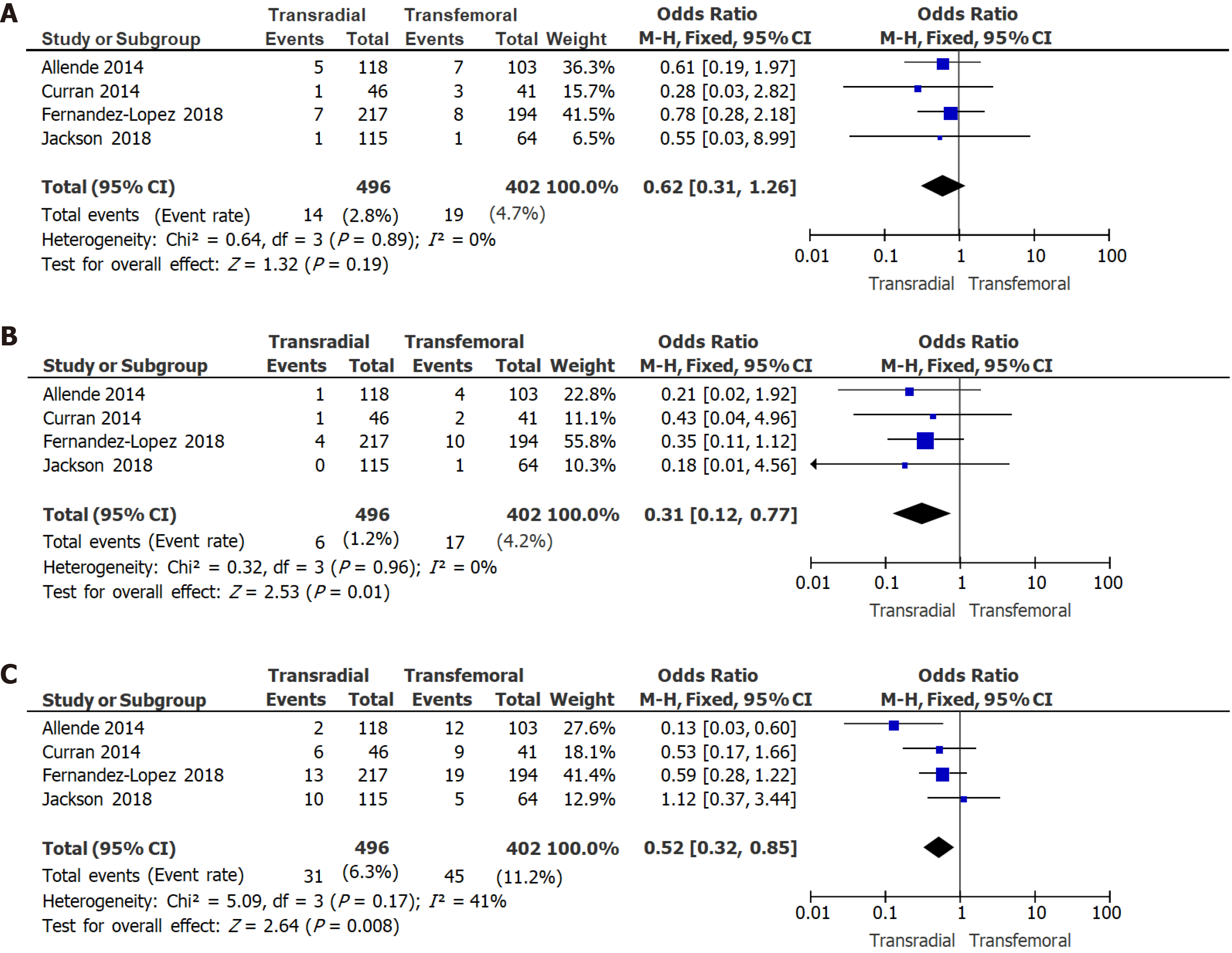
All-cause mortality: The 30-d all-cause mortality rate was 2.8% in the TRSA group and 4.7% in the TFSA group, OR 0.62 [0.31, 1.26] (P = 0.19, Figure 5A).
Stroke: The 30-d stroke rate was 1.2% in the TRSA group and 4.2% in the TFSA group, OR 0.31 [0.12, 0.77] (P = 0.01, Figure 5B).
Bleeding complications: In patients who had TFPA during their TAVI, major/Life-threatening bleeding complications were seen by 30 d in 6.3% of TRSA patients and 11.2% in TFSA, OR 0.52 [0.32, 0.85] (P = 0.008, Figure 5C).
Vascular complications: This was not analyzed for the TFPA group, as only 3 out of 5 studies reported on this outcome in the TFPA group.
In this meta-analysis, we found that patients who underwent TRSA had significantly lower odds than those with TFSA of developing 30-d mortality, stroke, bleeding, and major vascular complications. When APA site procedures were considered, the odds of mortality up to 30 d after the procedure were found to be 41% lower, and the odds of 30-d stroke 54% lower in the TRSA group than the TFSA group. Similarly, the odds of having major or life-threatening bleeding were 60% lower in the TRSA group than the TFSA group. The odds of having major vascular complications were 52% lower in the TRSA group. Our findings are consistent with previously published data[1-10], which have also reported that TRSA has lower odds of complications.
When TFPA alone was considered, there was no significant difference in 30-d mortality between the TRSA and TFSA groups as opposed to the APA group which showed a significant decrease in mortality in the TRSA group. The absolute mortality rates and odds ratio in the APA and TFPA cohorts were, however, comparable. This discrepancy in statistical significance can be attributed to the smaller sample size in the TFPA group. There were significantly lower odds of having a stroke or major/life-threatening bleeding in the TRSA group compared with the TFSA group in the TFPA cohort.
The transradial access has some advantages over transfemoral access. For one, the transradial site is more easily compressible in case of bleeding complications[11-13]. It also avoids the need to puncture both femoral arteries[3]. These advantages could lead to improved rates of vascular complications when compared with femoral secondary access. The disadvantage of radial access is that it does not allow the use of other interventional devices[11,13]. Some other challenges include difficulty navigating in case of anatomical variations and the possibility of developing radial artery occlusion with larger catheter diameters.
This review has several limitations. One major limitation of this meta-analysis is that all studies included were non-randomized. No randomized studies on this topic have been published yet. Hence there is high risk for selection bias. Risk adjustment or propensity score-matching was done in some studies. Two studies did not report on risk adjustment or matching in their study, hence there is a possibility of differences in their study populations. Moreover, unmeasured confounders cannot be accounted for. To improve confidence in the results, subgroup analysis was done only if data were reported in at least four studies. On another note, there was no uniformity in the type of primary access among studies. Few studies reported outcomes in the TFPA subgroup. This was a small fraction of the overall study population and results were mostly similar to APA results. Lastly, the presence of a learning curve should be considered, with the assumption that complication rates improve with experience. Due to the novelty of the procedure when initially adapted in some of these studies, one could assume that complications were more likely to occur in the early phase of implementing this procedure. In experienced operators, complication rates would likely be lower. This could skew the study results accordingly, especially if radial secondary access was adopted later in institutional experience.
In patients undergoing transcatheter aortic valve implantation (TAVI), irrespective of primary access, those who underwent TRSA had lower complication rates than those who underwent TFSA. In the absence of contraindications, a transradial approach for secondary access seems preferable in TAVI procedures. Confirmation by randomized controlled studies of TAVI procedures stratified by primary access site would be useful to adjust for primary access while comparing secondary access-related outcomes.
Complications of transcatheter aortic valve implantation (TAVI) procedures include bleeding, vascular complications, and strokes. These complications are often associated with the type of access used. Access can be primary or secondary. Few studies have been published on the effect of secondary access on outcomes.
The objective of this meta-analysis is to investigate if transradial secondary access (TRSA) has fewer complications than transfemoral or vice versa, with the hope of reducing complications in TAVI procedures related to access.
This systematic review aims to compare outcomes between transradial vs transfemoral secondary access (TFSA).
A systematic search was conducted using major databases (EMBASE, PubMed, Cochrane Central, Google Scholar), which resulted in 5 studies that met criteria for study selection. Outcomes of interest were 30-d rates each of major/life-threatening bleeding, vascular complications, strokes, and mortality. All 5 studies were observational. Adjusted or matched data were used if reported.
A total of 5065 patients underwent TAVI, with 1453 patients (28.7%) having undergone TRSA and 3612 patients (71.3%) TFSA. Irrespective of the site of primary access, the odds of having major or life-threatening bleeding were 60% lower in the TRSA group than the TFSA group (P < 0.00001). The odds of having major vascular complications were 52% lower in the TRSA group (P < 0.0001) with no difference in minor vascular complications between the 2 groups. Similarly, the odds of mortality in 30d after the procedure were 41% lower (P = 0.006) and the odds of stroke were 54% lower (P = 0.001) in the TRSA group than the TFSA group.
TRSA appears to be a safer alternative to the TFSA in TAVI procedures.
Our findings need to be confirmed in randomized clinical trials, which should minimize selection bias and both measured and unmeasured confounding.
The authors are grateful for the assistance of Darmoch F, MD, in conducting the literature search.
| 1. | Wynne DG, Rampat R, Trivedi U, de Belder A, Hill A, Hutchinson N, Hildick-Smith D. Transradial Secondary Arterial Access for Transcatheter Aortic Valve Implantation: Experience and Limitations. Heart Lung Circ. 2015;24:682-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Junquera L, Urena M, Latib A, Muñoz-Garcia A, Nombela-Franco L, Faurie B, Veiga-Fernandez G, Alperi A, Serra V, Regueiro A, Fischer Q, Himbert D, Mangieri A, Colombo A, Muñoz-García E, Vera-Urquiza R, Jiménez-Quevedo P, de la Torre JM, Pascual I, Garcia Del Blanco B, Sabaté M, Mohammadi S, Freitas-Ferraz AB, Guimarães L, Couture T, Côté M, Rodés-Cabau J. Comparison of Transfemoral Versus Transradial Secondary Access in Transcatheter Aortic Valve Replacement. Circ Cardiovasc Interv. 2020;13:e008609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 41] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 3. | Curran H, Chieffo A, Buchanan GL, Bernelli C, Montorfano M, Maisano F, Latib A, Maccagni D, Carlino M, Figini F, Cioni M, La Canna G, Covello RD, Franco A, Gerli C, Alfieri O, Colombo A. A comparison of the femoral and radial crossover techniques for vascular access management in transcatheter aortic valve implantation: the Milan experience. Catheter Cardiovasc Interv. 2014;83:156-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 4. | Allende R, Urena M, Cordoba JG, Ribeiro HB, Amat-Santos I, DeLarochellière R, Paradis JM, Doyle D, Mohammadi S, Côté M, Abdul-Jawad O, Del Trigo M, Ortas MR, Laflamme L, Laflamme J, DeLarochellière H, Dumont E, Rodés-Cabau J. Impact of the use of transradial versus transfemoral approach as secondary access in transcatheter aortic valve implantation procedures. Am J Cardiol. 2014;114:1729-1734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 53] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 5. | Jackson MWP, Muir DF, de Belder MA, Palmer S, Owens WA, Goodwin A, Hayat U, Williams PD. Transradial Secondary Access to Guide Valve Implantation and Manage Peripheral Vascular Complications During Transcatheter Aortic Valve Implantation. Heart Lung Circ. 2019;28:637-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 6. | Fernandez-Lopez L, Chevalier B, Lefèvre T, Spaziano M, Unterseeh T, Champagne S, Benamer H, Sanguineti F, Garot P, Hovasse T. Implementation of the transradial approach as an alternative vascular access for transcatheter aortic valve replacement guidance: Experience from a high-volume center. Catheter Cardiovasc Interv. 2019;93:1367-1373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Cortese B, Rigattieri S, Aranzulla TC, Russo F, Latib A, Burzotta F, Agostoni P, Ielasi A, Tarantino F, Sticchi A, Di Palma G, de Benedictis M, Trani C, Boccaletti R, Miccoli R, Valsecchi O, Colombo A. Transradial vs transfemoral ancillary approach in complex structural, coronary, and peripheral interventions. Results from the multicenter ancillary registry: A study of the Italian Radial Club. Catheter Cardiovasc Interv. 2018;91:97-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Jhand A, Apala DR, Dhawan R, Katta N, Aronow HD, Daniels MJ, Porter TR, Altin E, Goldsweig AM. Meta-analysis Comparing Transradial Versus Transfemoral Secondary Access in Transcatheter Aortic Valve Implantation. Am J Cardiol. 2020;131:74-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 9. | Félix-Oliveira A, Campante Teles R, Mesquita Gabriel H, de Araújo Gonçalves P, de Sousa Almeida M. The Spotlight Is on Secondary Access for TAVR: Radial Versus Femoral Revisited. JACC Cardiovasc Interv. 2020;13:655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Bazarbashi N, Gad MM, Saad AM, Mick SL, Reed GW, Puri R, Svensson L, Navia JL, Tuzcu EM, Krishnaswamy A, Kapadia S. Reply: The Spotlight Is on Secondary Access for TAVR: Radial Versus Femoral Revisited. JACC Cardiovasc Interv. 2020;13:655-656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Sallam M, Al-Hadi H, Rathinasekar S, Chandy S. Comparative study of the radial and femoral artery approaches for diagnostic coronary angiography. Sultan Qaboos Univ Med J. 2009;9:272-278. [PubMed] |
| 12. | Buchanan GL, Chieffo A, Montorfano M, Maccagni D, Maisano F, Latib A, Covello RD, Grimaldi A, Alfieri O, Colombo A. A "modified crossover technique" for vascular access management in high-risk patients undergoing transfemoral transcatheter aortic valve implantation. Catheter Cardiovasc Interv. 2013;81:579-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 13. | Ranasinghe MP, Peter K, McFadyen JD. Thromboembolic and Bleeding Complications in Transcatheter Aortic Valve Implantation: Insights on Mechanisms, Prophylaxis and Therapy. J Clin Med. 2019;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Barik R, Tung TH, Vermeersch P S-Editor: Gao CC L-Editor: A P-Editor: Li JH