Published online Dec 26, 2019. doi: 10.4330/wjc.v11.i12.282
Peer-review started: March 28, 2019
First decision: June 6, 2019
Revised: June 25, 2019
Accepted: November 20, 2019
Article in press: November 20, 2019
Published online: December 26, 2019
Processing time: 268 Days and 9.7 Hours
Pericardial decompression syndrome (PDS) is an infrequent, life-threatening complication following pericardial drainage for cardiac tamponade physiology. PDS usually develops after initial clinical improvement following pericardiocentesis and is significantly underreported and may be overlooked in the clinical practice. Although the precise mechanisms resulting in PDS are not well understood, this seems to be highly associated with patients who have some underlying ventricular dysfunction. Physicians performing pericardial drainage should be mindful of the risk factors associated with the procedure including the rare potential for the development of PDS.
Core tip: Pericardial decompression syndrome (PDS) is an infrequent, life-threatening complication following an uncomplicated pericardial evacuation for cardiac tamponade physiology. Physicians should be familiar with the prevention strategies for PDS and offer vulnerable patients a very close clinical monitoring, especially those undergoing pericardial drainage for large malignant effusions for suspected tamponade.
- Citation: Prabhakar Y, Goyal A, Khalid N, Sharma N, Nayyar R, Spodick DH, Chhabra L. Pericardial decompression syndrome: A comprehensive review. World J Cardiol 2019; 11(12): 282-291
- URL: https://www.wjgnet.com/1949-8462/full/v11/i12/282.htm
- DOI: https://dx.doi.org/10.4330/wjc.v11.i12.282
Cardiac tamponade is an emergent clinical condition that occurs after a rapid and/or excessive accumulation of fluid in the pericardial space. It restricts appropriate filling of the cardiac chambers and impairs normal hemodynamics which ultimately causes hypotension and cardiac arrest[1-3]. Pericardial drainage either by pericardiocentesis or pericardiotomy is required to make the patients hemodynamically stable, however, it has been associated with many complications including a rare, underreported and potentially fatal complication known as pericardial decompression syndrome (PDS).
PDS was first described in 1983 by Vandyke et al[4]and the terminology was first proposed by Angouras et al[5] in 2010 and since then, it has been recognized in multiple clinical settings[6-9]. PDS is characterized by a paradoxical hemodynamic instability and/or pulmonary edema following an otherwise non-complicated pericardial drainage. Another terminology used to describe PDS is the post-pericardial drainage low cardiac output syndrome[10-12]. Epidemiological data is limited, however, the incidence of PDS from a few studies is estimated to be around < 5%, following surgical drainage[11]. The exact etiology of PDS remains unclear, but most patients usually have an underlying pathology involving myocardial or ventricular dysfunction. There have been various suggested pathophysiological mechanisms for this phenomenon in the literature.
In this paper, we provide a comprehensive case-based review of the PDS describing the etiology, pathophysiology, clinical presentation and prevention and treatment related strategies.
We searched MEDLINE/PubMed and google scholar literature database for original articles, reviews, editorials, abstracts and case reports published between 1983 and 2017. The search terms we used, alone or in combination, were “pericardial decompression syndrome”, “cardiac tamponade”, “pericardial effusion”, “pericardiostomy”, and “low cardiac output syndrome”. All articles were independently reviewed for their appropriateness for data analysis and inclusion for drafting this review. The articles were independently screened to avoid any duplication of reported cases or reports. Also, any books or book chapters were screened for the search term of pericardial decompression syndrome and cardiac tamponade. Subsequently, the data from all studies were carefully selected for inclusion which was found most relevant to the subject of this review. All articles included in the data assessment were English-language, full-text papers and/or abstracts.
In cardiac tamponade, the main abnormality is rapid or slow compression of the cardiac chambers resulting from an increased intrapericardial pressure. Once the pericardial contents reach the limit of the pericardial reserve volume (volume resulting in pericardial distension), the expansion rate increases significantly thus exceeding the pericardial stretch[1-3]. While the pericardium gradually stretches over time, when at any instant it is inextensible, it impairs the cardiac contractility as the heart has to compete with the increased pericardial contents for a fixed intrapericardial volume. As the cardiac chambers become sequentially smaller in size, the myocardial diastolic compliance is reduced leading to a limited cardiac inflow; and ultimately leading to equalization of the mean diastolic pericardial and chamber pressures. The rate of fluid accumulation relative to pericardial stretch is the key element to the effectiveness of compensatory mechanisms[1-3].
Rapidly developing pericardial effusion such as acute intrapericardial hemorrhage or cardiac rupture may lead to a quick development of tamponade physiology as there is a relatively stiff pericardium with limited stretch capacity and there is less time for adaptation before routine activation of the most of the compensatory mechanisms. On the contrary, in cases of a slow increase in pericardial effusion such as idiopathic or malignant effusions, effusion size of 2 L or even more can occur before critical tamponade physiology may ensue[1-3].
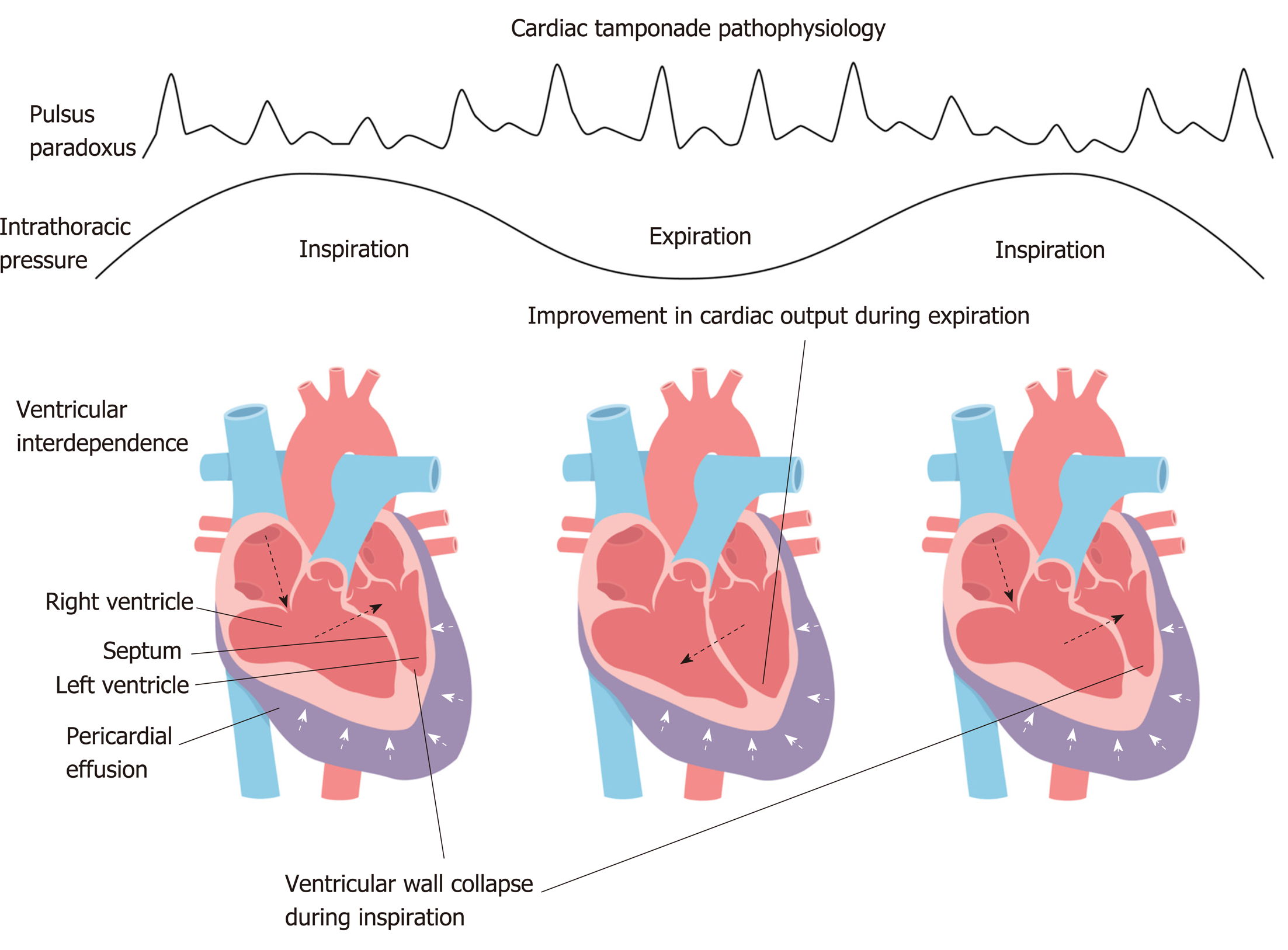
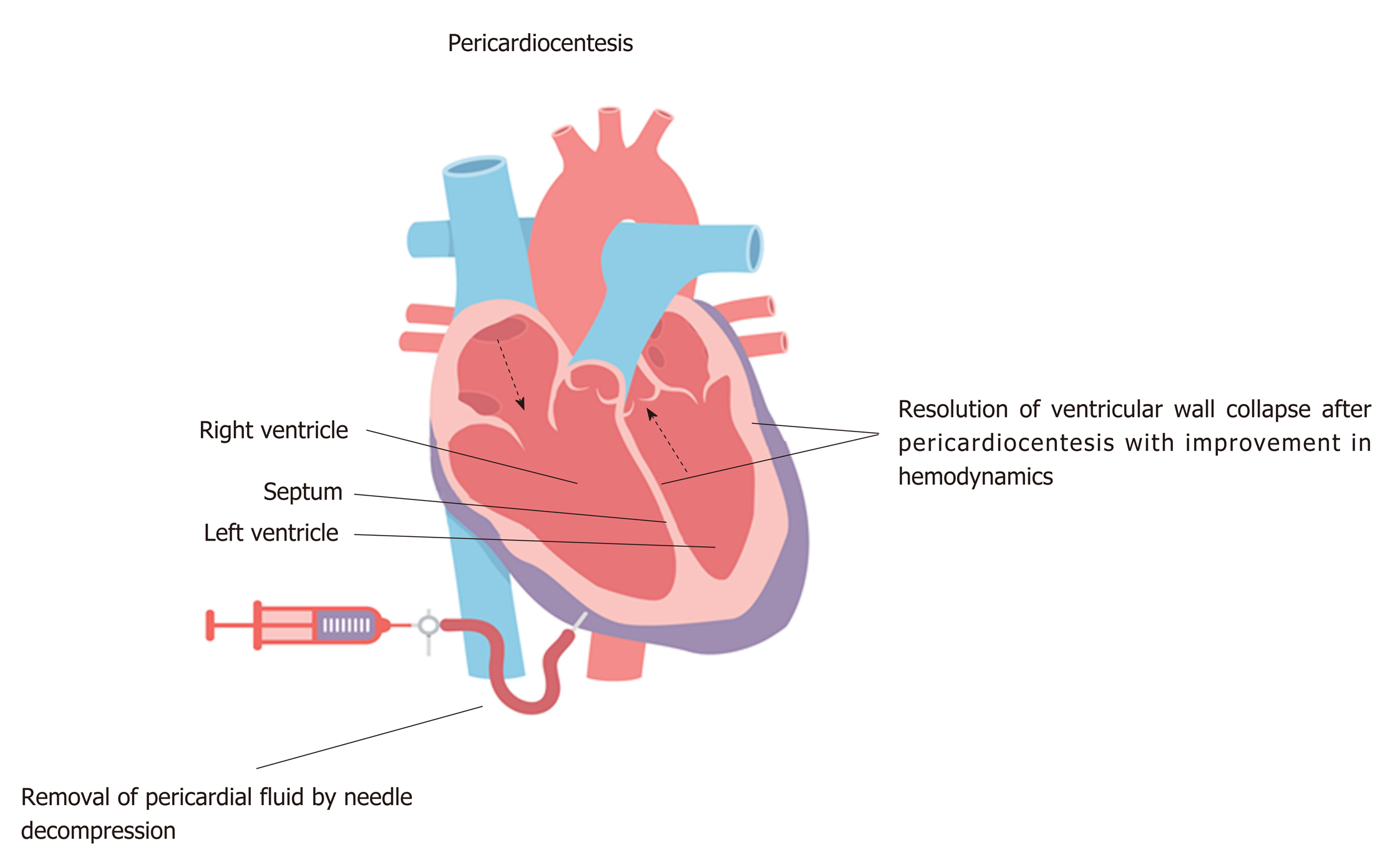
Rising pericardial pressure reduces and ultimately offsets the transmural pressure (intracardiac minus pericardial pressure), first for the right heart and ultimately for all chambers. Usually, during inspiration, the right heart filling increases at the expense of the left, so that its transmural pressure shows transient improvement which then reverses during expiration and this phenomenon is referred to as interventricular dependence in tamponade (Figure 1). When florid tamponade ensues, this mechanism cannot compensate for reduced stroke volumes, as these volumes are dependent on the elements which protect cardiac output and arterial pressures, mainly beta-adrenergic response causing increased heart rate, systemic peripheral resistance and ventricular ejection fraction. Emergent needle decompression of the pericardial fluid or pericardiocentesis is often required in tamponade as it helps in improvement of the transmural pressure, releases the interventricular dependence and thus ultimately restores normal hemodynamics (Figure 2). Rarely, there can be a paradoxical worsening of the hemodynamics after an otherwise successful and uncomplicated pericardial drainage (usually in long-standing large pericardial effusions) causing cardiac tamponade which can result in PDS and its pathophysiology has been discussed in further details below.
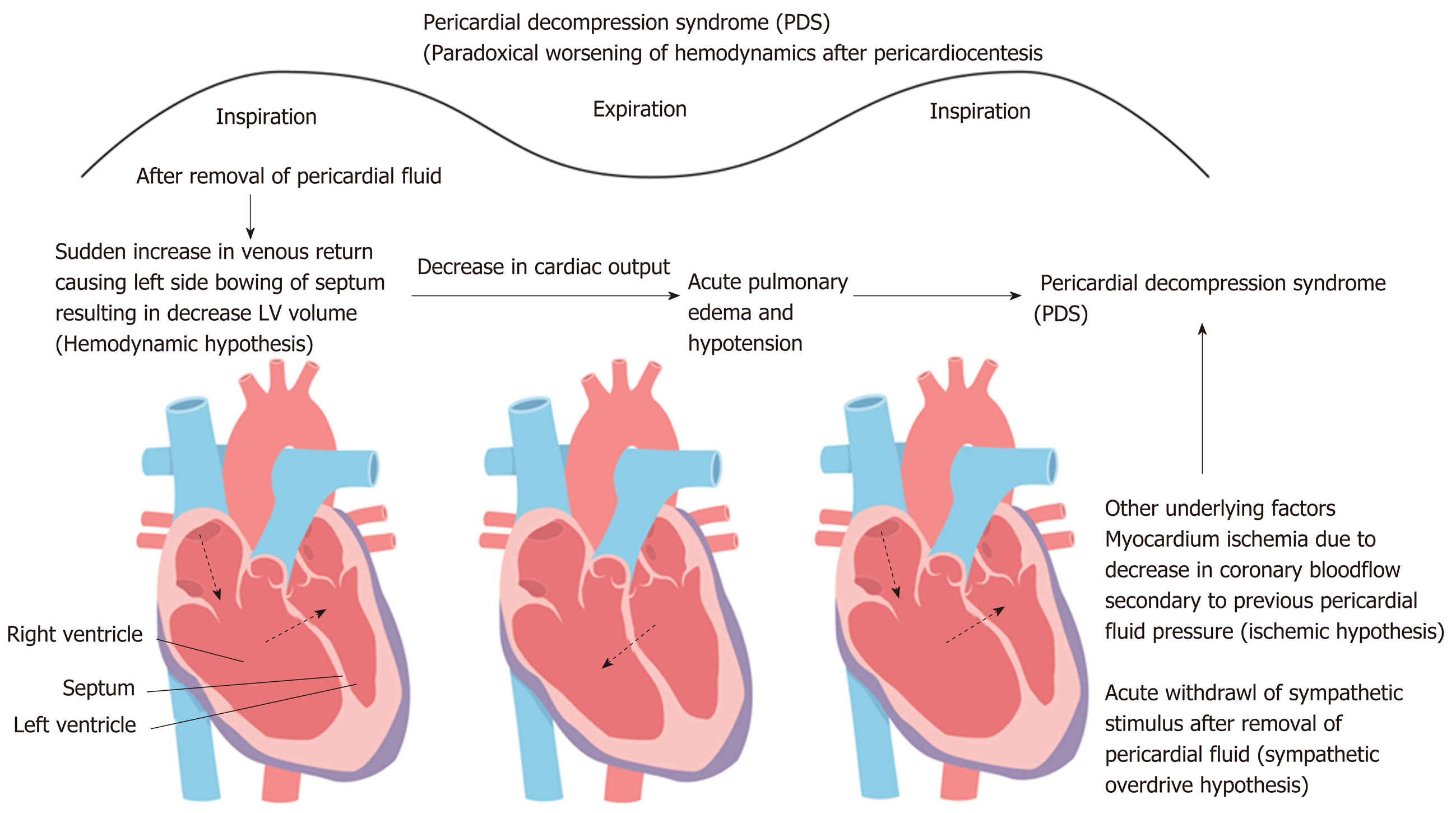
Various hypotheses have been reported to describe the clinical mechanism of PDS, however, its exact pathophysiology still remains unclear[12-34]. The proposed mechanism of PDS centers around three main hypotheses, namely: Hemodynamic, ischemic and autonomic hypothesis. These mechanisms provide greater insight into the possible pathophysiology of the PDS.
The simplest explanation of PDS is hemodynamic changes related to the interventricular interdependence. The hemodynamic hypothesis was first proposed in 1983 by Vandyke et al[4] when they first reported pulmonary edema in a patient who underwent uncomplicated pericardiocentesis for cardiac tamponade. Vandyke et al[4] hypothesized that pulmonary edema was precipitated by preload/afterload mismatch.
Following the rapid removal of the pericardial fluid originally compressing the right sided chambers during tamponade, now may lead to an increased venous return causing significant right ventricular expansion at the expense of the left chamber resulting in the reduced left ventricle volume/output and thus ensuing decompensated left heart failure and/or pulmonary edema. The rapid tamponade release is also followed by a net increase in the pulmonary venous return (left ventricular preload) while adaptive systemic vascular resistance (after-load) being still high (which is usually a compensatory phenomenon in tamponade to counteract hypotension response) may result in preload/afterload mismatch thus precipitating an acute onset heart failure (Figure 3)[10,11,14-16].
It is postulated that the coronary artery blood perfusion may be impaired due to compression caused by the pericardial fluid that may augment the risk of myocardial ischemia, leading to transient myocardial stunning that can persist after the removal of pericardial fluid thus causing transient left ventricular dysfunction.
Skalidis et al[21] demonstrated the first human-based report on how pericardial pressure can affect the coronary blood flow in humans, while previous reports had been based solely on animal studies. They studied a case of 52-years old patient with lung cancer who developed cardiac tamponade. The patient had successful pericardiocentesis, resulting in the removal of 850 mL of hemorrhagic fluid. The patient underwent a percutaneous balloon pericardiotomy 5 d later due to recurrence of pericardial effusion. During the pericardiotomy, the authors performed calculation of the amount of blood flow to the non-diseased left anterior descending coronary artery while pericardial pressure was gradually increased by infusing warmed normal saline at the rate of 30 mL/min. Coronary vasodilator reserve was computed using intracoronary adenosine. With increase in pericardial pressure, there was a gradual decline in the coronary blood flow, a gradual increase in the coronary vascular resistance, and an unaffected hyperemic response throughout. The maximal hyperemic flow was significantly less under the increased pericardial pressure than at normal pericardial pressure, which suggested an increased susceptibility to myocardial ischemia. In conclusion, the increased pericardial pressure during tamponade physiology can impair coronary perfusion leading to myocardial ischemia which can eventually cause left ventricular myocardial stunning that may persist even after pericardial drainage and can result in diastolic dysfunction thereby increasing the risk of PDS.
The imbalance in the autonomic system, specifically acute withdrawal of sympathetic stimulus after removal of pericardial fluid, may also be a precipitating factor for myocardial dysfunction and PDS. The myocardial dysfunction may occur by two ways due to this mechanism: One being the unmasking of underlying/pre-existing myocardial dysfunction and the second being the development of new myocardial dysfunction.
Wolfe and Edelman[14] reported that removal of sympathetic stimulus after pericardiocentesis might lead to unfolding of underlying left ventricular dysfunction that was not previously revealed due to an excessive catecholamine state, producing a markedly positive chronotropic and inotropic effect. Furthermore, Martins and colleagues showed that even though exogenous catecholamine administration improved coronary blood flow in patients with tamponade, filling pressures remained unchanged and there was only a modest increase in the cardiac index[22]. They proposed that since the sympathetic nervous system activation was already present, the elevated endogenous catecholamine levels did not provide any further potential benefit. The removal of the stimulus for an increased sympathetic state (that is, the relief of tamponade by pericardiocentesis) might well lead to the unmasking of left ventricular dysfunction that was previously compensated for by high endogenous catecholamine levels[17,18]. Thus, sympathetic overdrive mechanism might play an important role in the etiology of PDS because left ventricular systolic function abnormalities may occur after pericardiocentesis intervention as described.
Secondly, the patients may develop de novo transient systolic dysfunction due to overwhelming autonomic functional variations as a result of the stress from the cardiac tamponade and sudden hemodynamic alterations predisposed by the rapid evacuation of the pericardial space. This hypothesis may share some similar characteristics to the pathophysiology of patients with Takotsubo syndrome or stress-related cardiomyopathy[23].
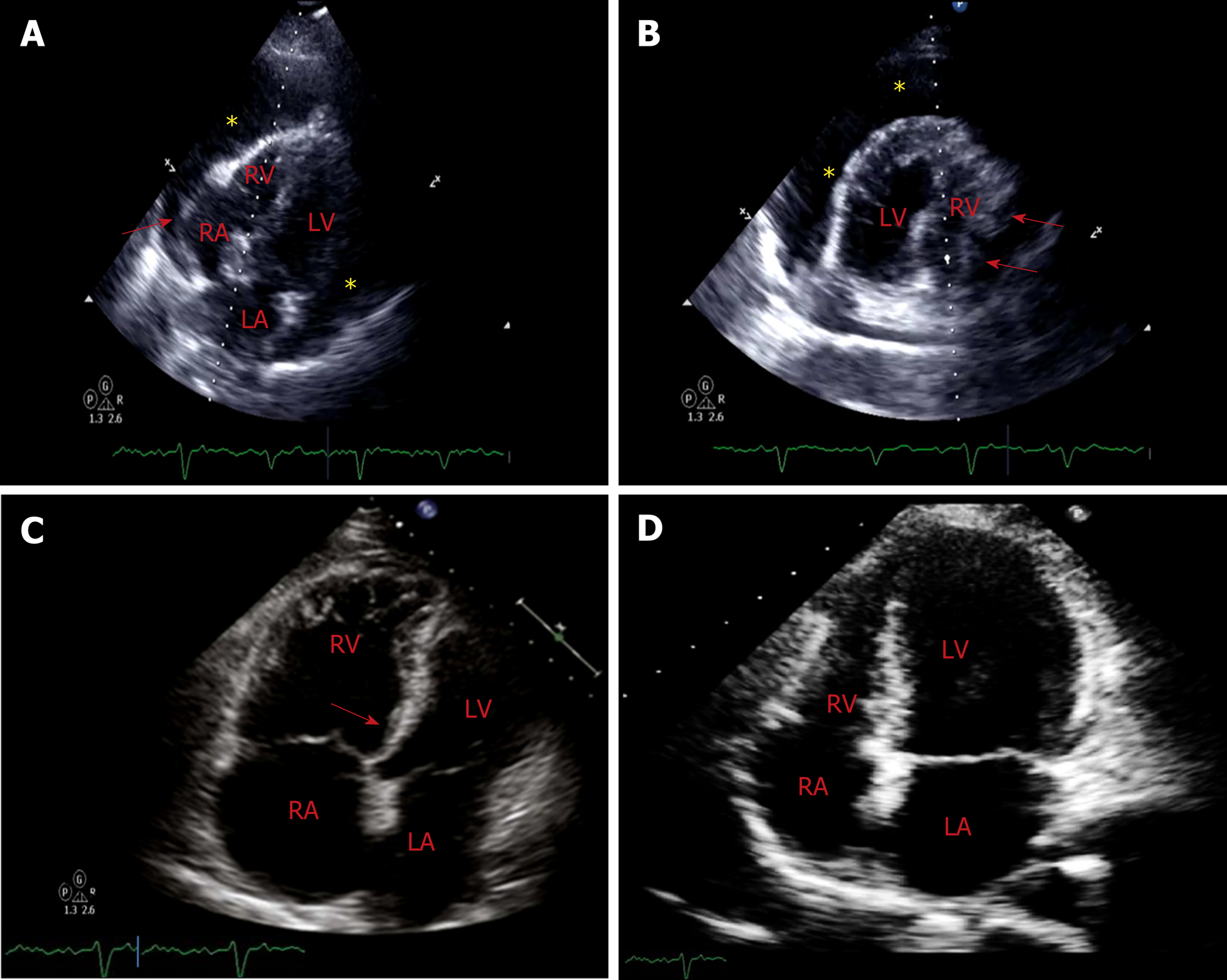
A 58-year-old woman with a history of Hodgkin lymphoma status post radiation therapy ten years ago, hypertension, diabetes mellitus and hypothyroidism presented to the emergency room with increasing dyspnea on exertion over 2 wk duration. Her medications included metformin 500 mg twice daily, aspirin 81 mg daily, levothyroxine 100 mcg daily, and metoprolol 25 mg twice a day. Initial vital signs demonstrated blood pressure of 96/60 mmHg, heart rate of 110 beats per minute (regular) and 96% oxygen saturation on room air. Her lung fields were clear, jugular venous pressure was elevated to the earlobe in an upright position, and the heart sounds were faint and distant. Peripheral pulses were weak bilaterally. 12-lead electrocardiogram showed low voltage and sinus tachycardia. Chest X-ray demonstrated cardiomegaly but otherwise was clear. Transthoracic echocardiogram demonstrated a left ventricular ejection fraction (LVEF) of 60%-65%, a large circumferential pericardial effusion with end diastolic right ventricular compression, and a swing sign (Figure 4A-B). Patient was taken to the cardiac catheterization laboratory for emergent pericardiocentesis. Ultrasound-guided pericardiocentesis resulted in rapid drainage of approximately 2200 mL of serous fluid with minimal improvement in hemodynamics. Patient was then taken to the cardiac catheterization laboratory holding area to be transported to the coronary care unit with the pericardial drain sutured in place. About 1 h later, the patient developed worsening dyspnea, hypotension (blood pressure of 72/40 mmHg), and labored breathing. Emergent chest radiograph showed diffuse bilateral pulmonary edema. She required intubation for hypoxic respiratory failure. Hemodynamic support was initiated with dobutamine and norepinephrine. Repeat emergent limited bedside echocardiogram demonstrated interval resolution of pericardial effusion, low-normal LVEF (50%), and mild to moderately dilated right ventricle with mild right ventricular (RV) hypokinesis and septal shift towards the left ventricle (Figure 4C). Patient was administered an intravenous saline bolus. Subsequently, the patient required hemodynamic support with intravenous vasopressors (norepinephrine) and inotropes (low-dose dopamine). Later, she was diuresed with intravenous lasix and vasopressor-inotropic support was gradually weaned off over the next 48 h. CT-chest angiography showed no evidence of pulmonary embolism with interval improvement in pulmonary edema. On day 3, patient’s hemodynamics improved without requirement of vasopressors and she was extubated. A repeat echocardiogram on day 5 demonstrated normalized ventricular function and trivial/minimal pericardial effusion (Figure 4D). She was discharged to home on day 6. We suspect that this patient developed pericardial decompression syndrome shortly after the pericardial drainage. Rapid pericardial fluid decompression may have resulted in paradoxical worsening of hemodynamics likely secondary to a combination of two factors, the first being a sudden increase in the venous return with still relatively higher systemic vascular resistance posing to a preload-afterload mismatch (hemodynamic hypothesis) and secondly likely due to sympathetic overdrive (as possibly evident from transient mild RV hypokinesis). These factors may have possibly led to the development of pulmonary edema, respiratory failure, and transient ventricular dysfunction. Supportive management resulted in spontaneous gradual improvement of her cardiopulmonary function.
Symptoms of pericardial decompression syndrome usually accompany with the paradoxical worsening of the patient's hemodynamics after a brief initial improvement in hemodynamics. The symptoms may be similar to those of acute heart failure exacerbation such as development of dyspnea, leg swelling, and increasing oxygen requirements, usually associated with rapid clinical deterioration including pulmonary edema and/or shock. Based on the papers by Pradhan et al[10] and Imazio[11], the onset of the syndrome ranged from immediate to usually 48 h following the pericardial fluid drainage for cardiac tamponade as an indication. According to an excellent analysis of 35 published cases from 1983 to 2013 by Pradhan et al[10], about 40% of patients had shock with left ventricular failure, 29% with pulmonary edema without shock, 20% with shock associated with biventricular failure and 11% with shock associated with RV failure and non-cardiogenic pulmonary edema. Diagnosis of PDS should only be established when other conditions predisposing to a shock-like state such as septic shock, cardiogenic shock resulting from MI and intraprocedural mechanical trauma (such as cardiac puncture, pneumothorax, diaphragmatic injury) have been ruled out. In relevant cases such as those presenting with isolated or significant RV dysfunction, exclusion of new-onset pulmonary embolism should probably be considered. Another important differential diagnosis is Takotsubo cardiomyopathy (TC) or stress-induced cardiomyopathy with cardiac tamponade, emotional stress and stress from significant hemodynamic derangements being the precipitating stressors for the development of TC[20,23]. In fact, transient ventricular (single or biventricular) dysfunction may be one of the driving mechanisms for the development of PDS as reported in some previous reports. The transient cardiac systolic dysfunction may be mechanistically very similar to TC. Most of the cases of primary TC are usually associated with characteristic staged ECG changes (which may include ST-elevations and T-wave inversions), rise in cardiac enzymes with most common presenting symptom being chest pain. In most of the reported cases of PDS (mimicking pathophysiology of TC) however, the patients usually have experienced dyspnea with no rise in cardiac enzymes and characteristic ECG changes only in minority[24,25].
The treatment of PDS is essentially supportive as the improvement of ventricular function is expected in survivors[7,10-12]. Patients undergoing pericardiocentesis or pericardiotomy require very close monitoring for the first 24 h, preferably in the intensive care unit[1,12,26]. In case of development of PDS, patients would require a very critical intensive monitoring, management with inotropic support, aggressive heart failure treatment with pressors and diuretics and as needed hemodynamic device support such as with an intra-aortic balloon pump.
Till date, there are no clear evidence-based guidelines or recommendations to specifically prevent PDS. A sensible strategy would be not drain large quantities of pericardial fluid in a single sitting especially in case of large pericardial effusions. The most reasonable approach would be to remove the amount of pericardial fluid just enough to result in the resolution of the cardiac tamponade physiology (which can be easily achieved by hemodynamic or echo-doppler monitoring) and then place a prolonged pericardial drainage to achieve a slow and gradual removal of additional pericardial fluid. Prolonged pericardial drainage may be removed when there is a daily fluid return below 30-50 mL[1,11]. The maximum amount of safely drainable pericardial fluid and rate of drainage has been previously suggested in some studies and guideline documents[1,27,28]. European Society of Cardiology 2004 guidelines generally recommend draining pericardial fluid in steps of less than 1 L at a time to avoid PDS based on case series of 3 patients with echocardiographic evidence of volume overload after pericardiocentesis[27,28]. Although judicious pericardial drainage may be potentially preventative against PDS, PDS may rarely develop even after small amount of pericardial drainage as previously documented in an isolated case report where patient developed PDS with pericardial fluid drainage of as little as 450 mL[29]. In general, the experts recommend stopping the initial drainage following the improvement of symptoms and hemodynamics followed by a slow gradual decompression through an indwelling pericardial catheter[4,27,30]. The slow gradual drainage may potentially allow a myocardial adaptation to the hemodynamic and filling pressure changes.
Cardiac tamponade is a critical clinical condition that results from a sudden and/or excessive accumulation of pericardial fluid. The treatment of cardiac tamponade is pericardiocentesis, preferably by a needle with the use of echocardiography. However, hemodynamically unstable patients warrant the use of pericardiocentesis without imaging following ruling out type A aortic dissection. Surgical drainage is required if the heart cannot be reached by a needle such as loculated effusion or predominant posterior location, clotted hemopericardium or ongoing intrapericardial bleeding where needle drainage is either ineffective or contraindicated[1].
Pericardiocentesis and pericardiostomy has its own procedure-related mechanical complications that include cardiac puncture, arrhythmias, pneumothorax, hemothorax, pneumopericardium, hepatic and diaphragmatic injury[27,35]. PDS is a rare complication that manifests as paradoxical worsening of hemodynamics following pericardial fluid drainage. The actual incidence of PDS is unknown among the general patient population with cardiac tamponade and may be related to its under-reporting and/or low general familiarity to the Cardiologists regarding PDS. Incidence has been estimated to be between 5% to 34% following pericardial drainage from malignant pericardial effusion from a handful of case studies and series[20,24]. The clinical presentation may be variable that may include pulmonary edema, shock and/or reversible ventricular impairment (RV, LV or biventricular dysfunction). Certain clinical variables such as history of malignancy, prior radiotherapy use, pericardial calcification, low ejection fraction, and connective tissue disorders have been known to increase the risk of PDS. Among these, most of the reported cases in literature who developed pericardial effusion leading to cardiac tamponade and PDS were related to malignant effusions. Thus, patients with history of malignancy and suspected malignant pericardial effusion may require more close monitoring for possible development of PDS. Halting the initial pericardial drainage following the improvement of symptoms and hemodynamics followed by gradual slow decompression by using pericardial catheter may be a favored approach in such patients[11]. Some authors also favor pericardiocentesis over pericardiotomy as pericardiotomy was associated with a higher mortality in patients who developed PDS. Although no precise reason known for this observation, it has been argued that surgical drainage may lead to a more rapid expansion of the right ventricle due to a rapid pericardial decompression[10,36].
Supportive therapy is the key for the treatment of PDS that includes intra-aortic balloon pump, inotropic support, and aggressive heart failure treatment as previously discussed. LV dysfunction if present, may usually demonstrate improvement within a few days, accompanied with a solid mid-term prognosis[37].
PDS is an uncommon complication of pericardial drainage and has a high mortality and morbidity. Physicians should be familiar with the prevention strategies for PDS and offer vulnerable patients a very close clinical monitoring, especially those undergoing pericardial drainage for large malignant effusions for suspected tamponade.
Further studies are needed to for better understanding of the pathophysiology and prevention strategies for PDS. Also, establishing a large multicenter registry database may provide further insights about the best choices for the drainage techniques and treatment strategies.
| 1. | Spodick DH. Acute cardiac tamponade. N Engl J Med. 2003;349:684-690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 533] [Cited by in RCA: 439] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 2. | Spodick DH. The normal and diseased pericardium: current concepts of pericardial physiology, diagnosis and treatment. J Am Coll Cardiol. 1983;1:240-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 140] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 3. | Chhabra L, Spodick DH, Aronow WS, Fleg JL, Rich MW. Pericardial disease in the elderly. Tresch and Aronow's Cardiovascular Disease in the Elderly. 5th ed. Aronow WS, Fleg JL, Rich MW. Boca Raton, FL: CRC Press; 2014; 644-668. |
| 4. | Vandyke WH, Cure J, Chakko CS, Gheorghiade M. Pulmonary edema after pericardiocentesis for cardiac tamponade. N Engl J Med. 1983;309:595-596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 71] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Angouras DC, Dosios T. Pericardial decompression syndrome: a term for a well-defined but rather underreported complication of pericardial drainage. Ann Thorac Surg. 2010;89:1702-3; author reply 1703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Lim AS, Paz-Pacheco E, Reyes M, Punzalan F. Pericardial decompression syndrome in a patient with hypothyroidism presenting as massive pericardial effusion: a case report and review of related literature. BMJ Case Rep. 2011;2011:bcr0420114117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Fozing T, Zouri N, Adam O, Oezbek C. Management of a patient with pericardial decompression syndrome and HOCM. BMJ Case Rep. 2016;2016:bcr2015211550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Ligero C, Leta R, Bayes-Genis A. Transient biventricular dysfunction following pericardiocentesis. Eur J Heart Fail. 2006;8:102-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 33] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Glasser F, Fein AM, Feinsilver SH, Cotton E, Niederman MS. Non-cardiogenic pulmonary edema after pericardial drainage for cardiac tamponade. Chest. 1988;94:869-870. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Pradhan R, Okabe T, Yoshida K, Angouras DC, DeCaro MV, Marhefka GD. Patient characteristics and predictors of mortality associated with pericardial decompression syndrome: a comprehensive analysis of published cases. Eur Heart J Acute Cardiovasc Care. 2015;4:113-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 38] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 11. | Imazio M. Pericardial decompression syndrome: a rare but potentially fatal complication of pericardial drainage to be recognized and prevented. Eur Heart J Acute Cardiovasc Care. 2015;4:121-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Sabzi F, Faraji R. Predictors of post pericardiotomy low cardiac output syndrome in patients with pericardial effusion. J Cardiovasc Thorac Res. 2015;7:18-23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 13. | Braverman AC, Sundaresan S. Cardiac tamponade and severe ventricular dysfunction. Ann Intern Med. 1994;120:442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Wolfe MW, Edelman ER. Transient systolic dysfunction after relief of cardiac tamponade. Ann Intern Med. 1993;119:42-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 49] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Hamaya Y, Dohi S, Ueda N, Akamatsu S. Severe circulatory collapse immediately after pericardiocentesis in a patient with chronic cardiac tamponade. Anesth Analg. 1993;77:1278-1281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Wechsler AS, Auerbach BJ, Graham TC, Sabiston DC. Distribution of intramyocardial blood flow during pericardial tamponade. Correlation with microscopic anatomy and intrinsic myocardial contractility. J Thorac Cardiovasc Surg. 1974;68:847-856. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 2] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 17. | Chamoun A, Cenz R, Mager A, Rahman A, Champion C, Ahmad M, Birnbaum Y. Acute left ventricular failure after large volume pericardiocentesis. Clin Cardiol. 2003;26:588-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | Weijers RW, Post JC. Transient left ventricular systolic dysfunction mimicking myocardial infarction after pericardiocentesis. Neth Heart J. 2013;21:364-366. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Palatianos GM, Thurer RJ, Pompeo MQ, Kaiser GA. Clinical experience with subxiphoid drainage of pericardial effusions. Ann Thorac Surg. 1989;48:381-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 41] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 20. | Versaci F, Donati R, Mezzanotte R, Chiariello L, Ammirati F. An unusual complication following pericardiocentesis: reversible left ventricular dysfunction. J Cardiovasc Med (Hagerstown). 2015;16 Suppl 2:S133-S135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 21. | Skalidis EI, Kochiadakis GE, Chrysostomakis SI, Igoumenidis NE, Manios EG, Vardas PE. Effect of pericardial pressure on human coronary circulation. Chest. 2000;117:910-912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 29] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 22. | Martins JB, Manuel WJ, Marcus ML, Kerber RE. Comparative effects of catecholamines in cardiac tamponade: experimental and clinical studies. Am J Cardiol. 1980;46:59-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 36] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Ayoub C, Chang M, Kritharides L. A case report of ventricular dysfunction post pericardiocentesis: stress cardiomyopathy or pericardial decompression syndrome? Cardiovasc Ultrasound. 2015;13:32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 24. | Pilgrim TM, Wyss TR. Takotsubo cardiomyopathy or transient left ventricular apical ballooning syndrome: A systematic review. Int J Cardiol. 2008;124:283-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 353] [Cited by in RCA: 365] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 25. | Wagner PL, McAleer E, Stillwell E, Bott M, Rusch VW, Schaffer W, Huang J. Pericardial effusions in the cancer population: prognostic factors after pericardial window and the impact of paradoxical hemodynamic instability. J Thorac Cardiovasc Surg. 2011;141:34-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 44] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 26. | Neelakandan B, Jayanthi N, Kanthimathi R. Subxiphoid drainage for pericardial tamponade. J Thorac Cardiovasc Surg. 1996;111:489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 27. | Maisch B, Seferović PM, Ristić AD, Erbel R, Rienmüller R, Adler Y, Tomkowski WZ, Thiene G, Yacoub MH; Task Force on the Diagnosis and Management of Pricardial Diseases of the European Society of Cardiology. Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology. Eur Heart J. 2004;25:587-610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 847] [Cited by in RCA: 776] [Article Influence: 35.3] [Reference Citation Analysis (11)] |
| 28. | Armstrong WF, Feigenbaum H, Dillon JC. Acute right ventricular dilation and echocardiographic volume overload following pericardiocentesis for relief of cardiac tamponade. Am Heart J. 1984;107:1266-1270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 28] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 29. | Dosios T, Theakos N, Angouras D, Asimacopoulos P. Risk factors affecting the survival of patients with pericardial effusion submitted to subxiphoid pericardiostomy. Chest. 2003;124:242-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 54] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 30. | Albeyoglu S, Aldag M, Ciloglu U, Kutlu H, Dagsali S. Biventricular transient systolic dysfunction after mitral valve replacement: Pericardial decompression syndrome. Int J Surg Case Rep. 2016;28:145-148. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 31. | Khalid N, Ahmad SA, Shlofmitz E, Chhabra L. Pathophysiology of Takotsubo Syndrome. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019; . [PubMed] |
| 32. | Chhabra L, Chaubey VK. Right Ventricle Involvement in Tako-Tsubo Cardiomyopathy. JACC Cardiovasc Imaging. 2016;9:632-633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 33. | Khalid N, Chhabra L, Ahmad SA, Sareen P, Spodick DH. Autonomic Dysfunction and Takotsubo Cardiomyopathy. Am J Med. 2015;128:e45-e46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 34. | Gowdar S, Syal S, Chhabra L. Probable protective role of diabetes mellitus in takotsubo cardiomyopathy: a review. Vessel Plus. 2017;1:129-136. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 35. | Charron P, Adler Y. 'Ten Commandments' of 2015 ESC Guidelines for diagnosis and management of pericardial diseases. Eur Heart J. 2015;36:2874. [PubMed] |
| 36. | Allen KB, Faber LP, Warren WH, Shaar CJ. Pericardial effusion: subxiphoid pericardiostomy versus percutaneous catheter drainage. Ann Thorac Surg. 1999;67:437-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 81] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 37. | Moreno Flores V, Pascual Figal DA, Caro Martínez C, Valdés-Chávarri M. Transient left ventricular dysfunction following pericardiocentesis. An unusual complication to bear in mind. Rev Esp Cardiol. 2009;62:1071-1072. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
Manuscript source: Invited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
P-Reviewer: Greenway SC S-Editor:Ma YJ L-Editor: A E-Editor: Zhang YL