©The Author(s) 2023.
World J Cardiol. Sep 26, 2023; 15(9): 415-426
Published online Sep 26, 2023. doi: 10.4330/wjc.v15.i9.415
Published online Sep 26, 2023. doi: 10.4330/wjc.v15.i9.415
Figure 1 Full transformation of the pre-existing magnetic resonance imaging environment into an interventional cardiac magnetic resonance imaging suite.
A: Pre-existing diagnostic magnetic resonance imaging (MRI) scanner room; B: Pre-existing diagnostic MRI control room; C: Transformed interventional cardiac magnetic resonance (iCMR) suite; D: Transformed iCMR control room. E: The non-MR compatible RF generator including cooling-pump positioned in the iCMR control room. EP, electrophysiological; iCMR, interventional cardiac MRI. Citation: Bijvoet GP, Holtackers RJ, Smink J, Lloyd T, van den Hombergh CLM, Debie LJBM, Wildberger JE, Vernooy K, Mihl C, Chaldoupi SM. Transforming a pre-existing MRI environment into an interventional cardiac MRI suite. J Cardiovasc Electrophysiol 2021; 32: 2090-2096 [PMID: 34164862 DOI: 10.1111/jce.15128]. Epub 2021 Jul 4. Copyright © 2021 The Authors. Journal of Cardiovascular Electrophysiology published by Wiley Periodicals LLC. (Reproduced with permission)[13].
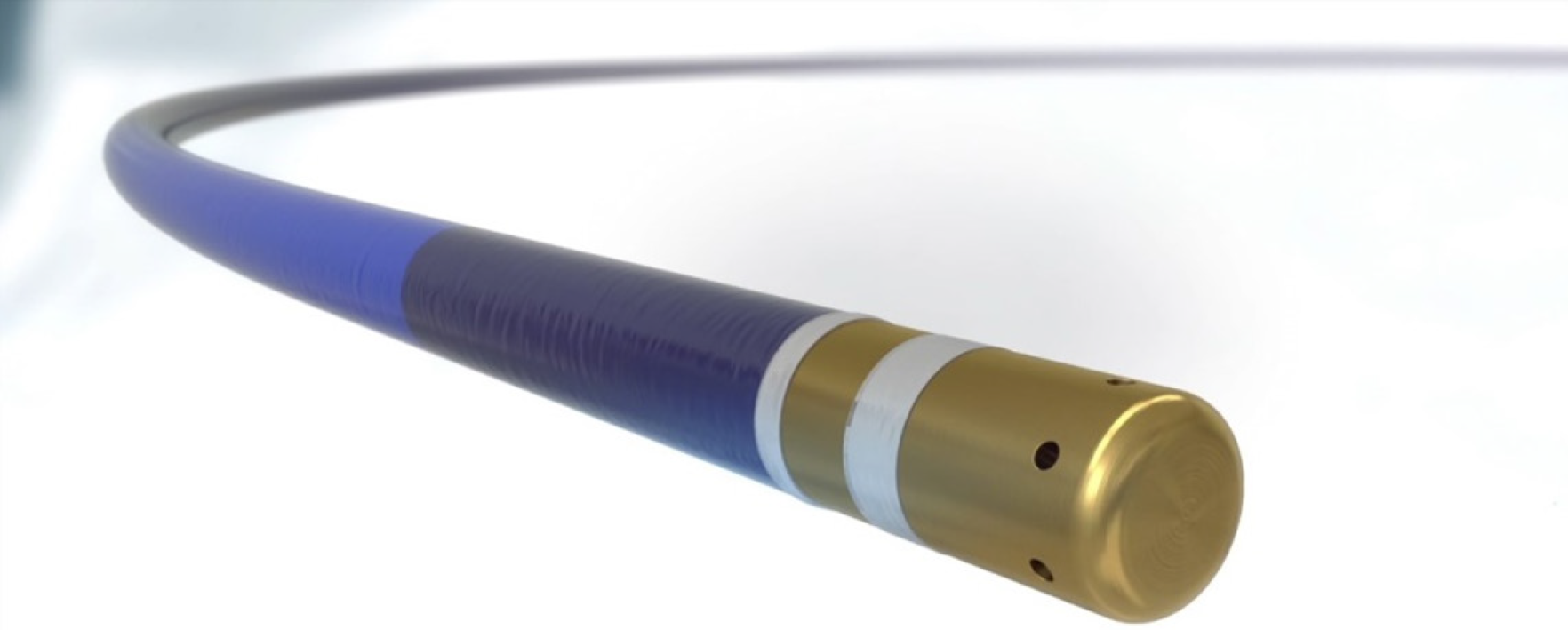
Figure 2 9 Fr.
bipole irrigated-tip ablation catheter with two magnetic resonance receive coils in the distal end for active magnetic resonance tracking. (Reproduced with permission from https://imricor.com).
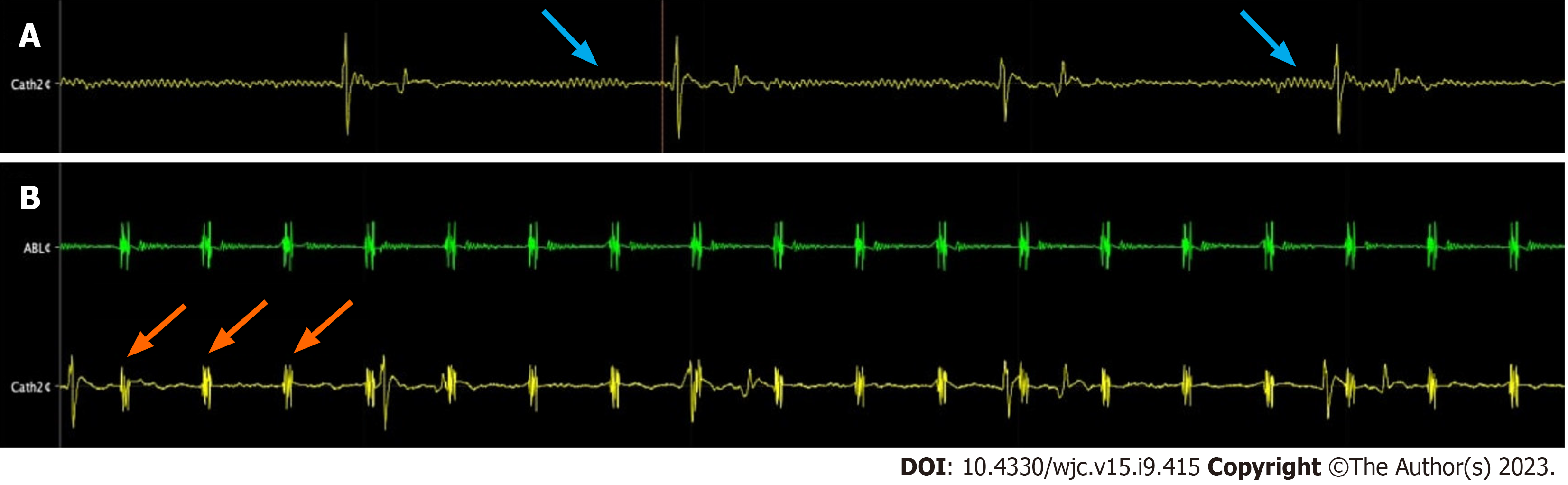
Figure 3 Distortion of the electrograms within the magnetic field.
A: Baseline noise of intra-cardiac electrograms recorded with the coronary sinus catheter (blue arrows indicate the maximally distorted signal); B: Gradient-induced artifacts that cause high frequency peaks during magnetic resonance scanning (orange arrows). ABLc: Ablation catheter; CATH2c: Coronary sinus catheter.
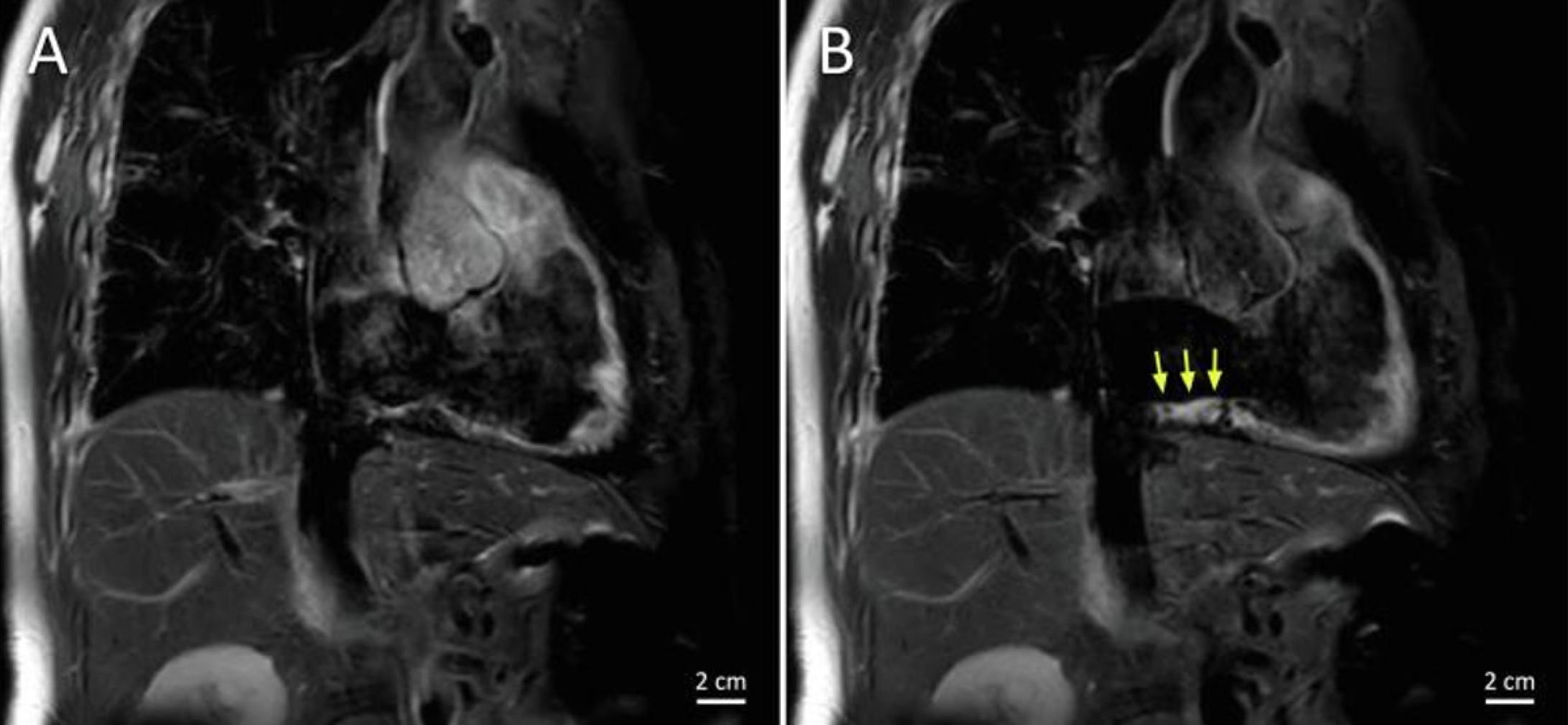
Figure 4 Imaging with T2 mapping detects inflamed edematous tissue.
A and B: T2-weighted magnetic resonance images of the cavotricuspid isthmus in the RAO view before (A) and after (B) ablation showing edema in the ablation lesions, indicated by the yellow arrows. Citation: Bijvoet GP, Holtackers RJ, Nies HMJM, Mihl C, Chaldoupi SM. The role of interventional cardiac magnetic resonance (iCMR) in a typical atrial flutter ablation: The shortest path may not always be the fastest. Int J Cardiol Heart Vasc 2022; 41: 101078. [PMID: 35800043 DOI: 10.1016/j.ijcha.2022.101078]. Copyright © 2022 The Authors. Published by Elsevier B.V. (Reproduced under the terms of the Creative Commons CC-BY license)[44].
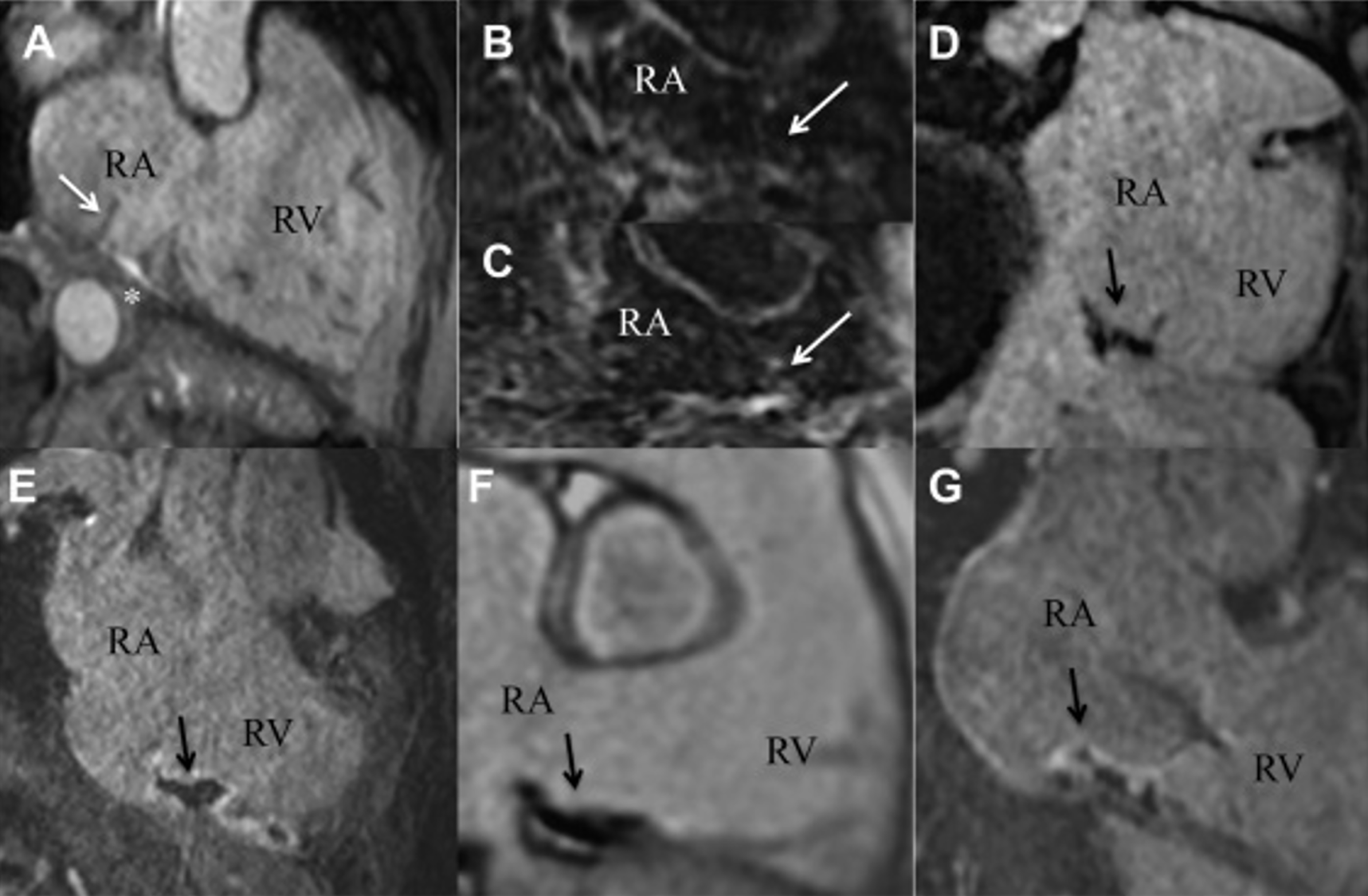
Figure 5 Acute lesion after radiofrequency ablation of the right cavotricuspid isthmus.
A: Balanced steady-state free precision sequence image of the cavotricuspid isthmus (CTI) immediately after ablation. White asterisk indicates pericardial effusion. White arrow indicates a prominent eustachian valve; B and C: T2-weighted images preablation (B) and postablation (C) showing signal intensity enhancement of the isthmus line (white arrows); D: Noncontrast enhanced T1-weighted image of the CTI depicts acute necrotic lesions as signal intensity loss (black arrow); E: Postcontrast early enhancement image shows hypoenhanced myocardium localized at the CTI, known as a microvascular obstruction as an acute ablation lesion sign; F: Phase-sensitive inversion recovery image depicts acute ablation lesion in terms of black, hypoenhanced myocardium; G: Postcontrast late gadolinium enhancement images led to partially enhanced radiofrequency ablation lesions (white edge) with black necrotic core (black arrow). Citation: Ulbrich S, Huo Y, Tomala J, Wagner M, Richter U, Pu L, Mayer J, Zedda A, Krafft AJ, Lindborg K, Piorkowski C, Gaspar T. Magnetic resonance imaging-guided conventional catheter ablation of isthmus-dependent atrial flutter using active catheter imaging. Heart Rhythm O2. 2022; 3: 553-559 [PMID: 36340492 DOI: 10.1016/j.hroo.2022.06.011]. Copyright © 2022 Heart Rhythm Society. Published by Elsevier Inc. (Reproduced under the terms of the Creative Commons CC-BY license)[40].
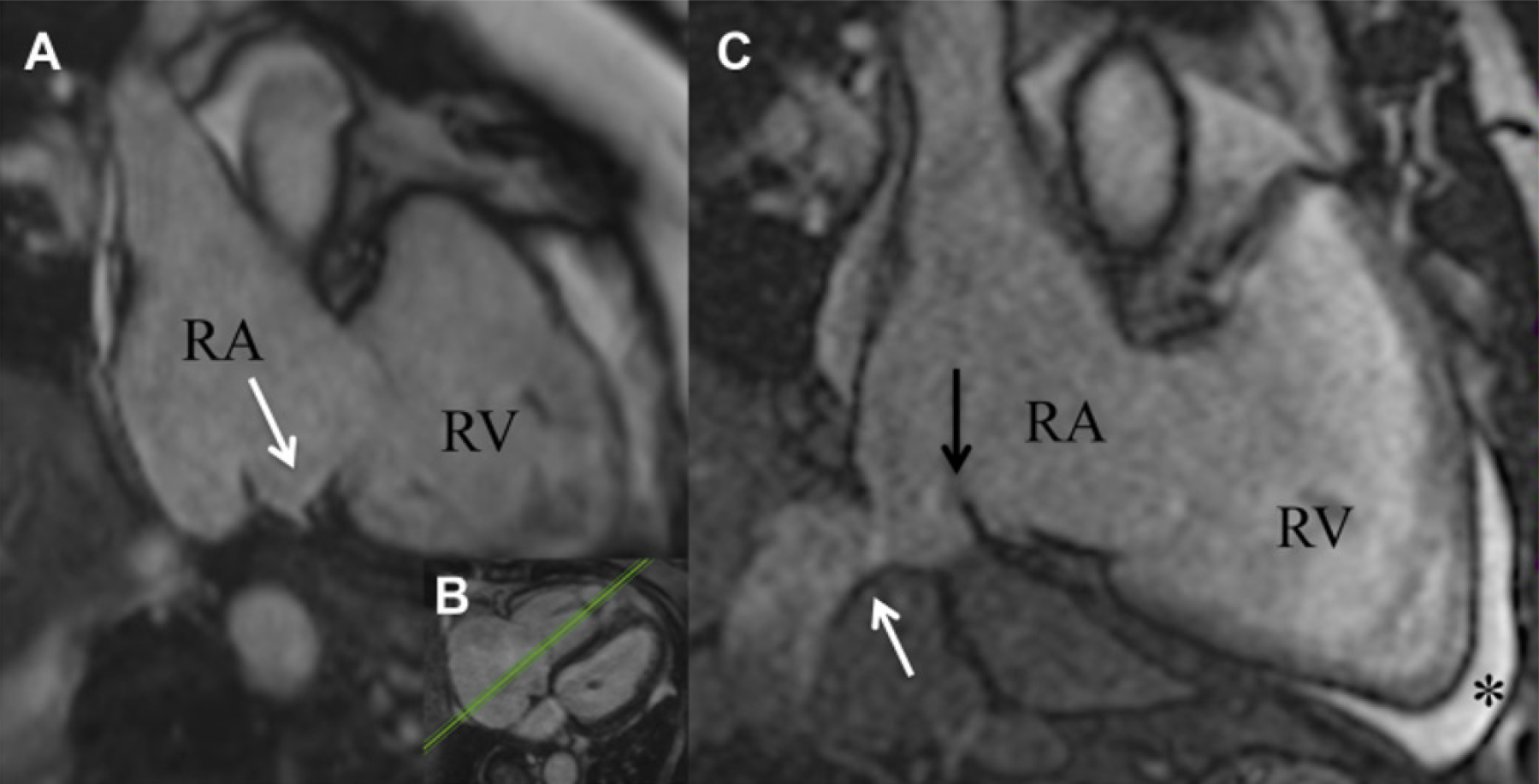
Figure 6 Isthmus pouches that are frequently present, a prominent Eustachian ridge and large pectinate muscles may impede catheter stability and navigation to target sites leading to poor tissue contact and low radio frequency energy delivery.
A and B: Septal pouch (white arrow) of the cavotricuspid isthmus in a balanced steady-state free precision sequence image [as visualized in the transversal plane (B)]; C: Kinking of the vena cava inferior junction in the right atrium (white arrow) and a eustachian valve (black arrow) was found. Anterior to the right ventricular apex, a pre-existing pericardial effusion was located (asterisk). Citation: Ulbrich S, Huo Y, Tomala J, Wagner M, Richter U, Pu L, Mayer J, Zedda A, Krafft AJ, Lindborg K, Piorkowski C, Gaspar T. Magnetic resonance imaging-guided conventional catheter ablation of isthmus-dependent atrial flutter using active catheter imaging. Heart Rhythm O2 2022; 3: 553-559 [PMID: 36340492 DOI: 10.1016/j.hroo.2022.06.011]. Copyright © 2022 Heart Rhythm Society. Published by Elsevier Inc. (Reproduced under the terms of the Creative Commons CC-BY license)[40].
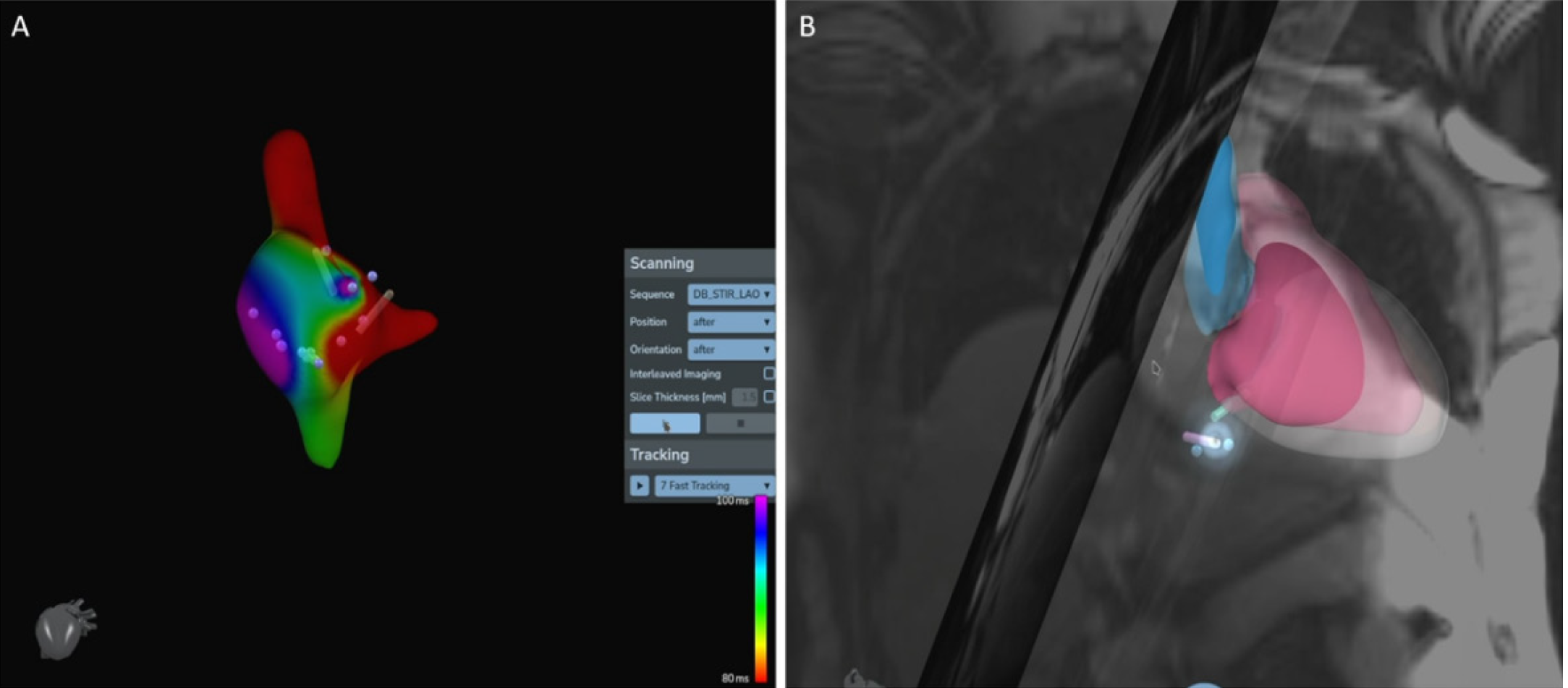
Figure 7 Electroanatomic mapping systems compatible for use inside a magnetic resonance scanner have been developed.
A: 3D electroanatomical activation mapping; B: Integration with real-time cardiac magnetic resonance imaging planes. (Reproduced with permission from https://imricor.com).
- Citation: Tampakis K, Pastromas S, Sykiotis A, Kampanarou S, Kourgiannidis G, Pyrpiri C, Bousoula M, Rozakis D, Andrikopoulos G. Real-time cardiovascular magnetic resonance-guided radiofrequency ablation: A comprehensive review. World J Cardiol 2023; 15(9): 415-426
- URL: https://www.wjgnet.com/1949-8462/full/v15/i9/415.htm
- DOI: https://dx.doi.org/10.4330/wjc.v15.i9.415