Published online Sep 27, 2016. doi: 10.4240/wjgs.v8.i9.656
Peer-review started: May 25, 2016
First decision: July 6, 2016
Revised: July 12, 2016
Accepted: July 29, 2016
Article in press: August 1, 2016
Published online: September 27, 2016
Processing time: 124 Days and 10.9 Hours
Eosinophilic gastroenteritis (EGE) is a rare condition characterized by eosinophilic infiltration of the gastrointestinal tract. Depending on the dominant layer of infiltration it is classified into three types namely, mucosal, muscularis and subserosal. The most uncommon variant is the subserosal type characterized by primarily subserosal disease, eosinophilic ascites and peripheral hypereosinophilia. The clinical features are non-specific with history of atopic predisposition and allergy. Endoscopic biopsy is frequently non-diagnostic due to an uninvolved gastrointestinal mucosa rendering its diagnosis a challenge. The mainstay of diagnosis is peripheral hypereosinophilia and eosinophil-rich ascitic fluid on diagnostic paracentesis. Oral steroid therapy is usually the first line of treatment with dramatic response. Due to a propensity for relapse, steroid-sparing therapy should be considered for relapses of EGE. We report a case of subserosal EGE with diagnostic clinical features and treatment response and review the current strategy in the management of eosinophilic ascites.
Core tip: Eosinophilic gastroenteritis (EGE) is a rare condition and the diagnosis of subserosal EGE is challenging due to its nonspecific symptoms and signs and frequently non-diagnostic biopsy on gastrointestinal endoscopy. This review describes a patient with typical findings of peripheral hypereosinophilia and eosinophilic ascites and outlines the current strategy in the diagnosis and treatment of subserosal EGE.
- Citation: Agrawal S, Vohra S, Rawat S, Kashyap V. Eosinophilic ascites: A diagnostic and therapeutic challenge. World J Gastrointest Surg 2016; 8(9): 656-659
- URL: https://www.wjgnet.com/1948-9366/full/v8/i9/656.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v8.i9.656
Eosinophilic gastroenteritis (EGE) is a rare and potentially fatal condition with clinico-pathologic characteristics of peripheral hypereosinophilia and eosinophilic infiltration of the gastrointestinal tract. It is classified into three pathologic types depending on the dominant gastrointestinal layer of eosinophilic infiltration[1]. The subserosal type characterized by primarily subserosal disease and eosinophilic ascites is the rarest presentation of EGE[2,3]. Biopsy of the mucosal layer obtained during upper gastrointestinal endoscopy frequently fails to diagnose subserosal EGE. The diagnosis of subserosal EGE is challenging because of its rarity, nonspecific clinical presentation and non-diagnostic endoscopy. This study presents the typical clinico-pathologic and radiologic findings in subserosal EGE and reviews the current diagnostic and therapeutic strategy in patients with abdominal pain, ascites and peripheral hypereosinophilia.
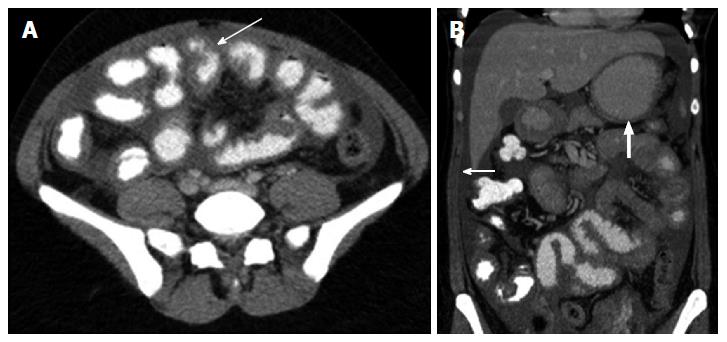
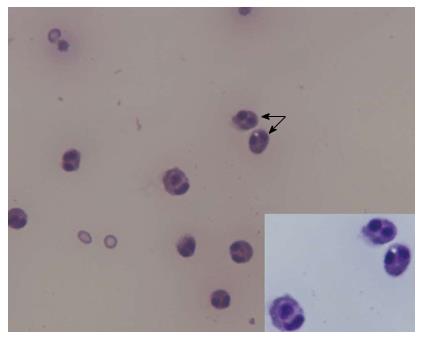
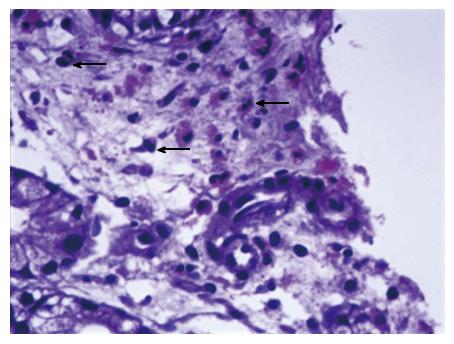
A 35-year-old female presented to the clinic with complaints of abdominal distension and an episode of self-limiting diarrhea three weeks ago. She admitted to the recent use of green tea and increased consumption of nuts in her diet. Past medical history was remarkable for recurrent allergic bronchitis. On examination there was no evidence of pallor, icterus or peripheral edema and abdominal examination revealed moderate distention with a doughy consistency. Abdominal ultrasonography demonstrated moderate ascites with no signs of portal hypertension, liver or renal disease. Contrast-enhanced abdominal computed tomography confirmed the presence of free peritoneal fluid, diffuse circumferential thickening of small bowel loops, distal stomach and esophagus (Figure 1). Laboratory examination revealed peripheral eosinophilic leukocytosis with 52% eosinophils (total leukocyte count 22900 cells/mm3) and no immature myeloid precursors. The C-reactive protein, erythrocyte sedimentation rate and IgE levels were within normal limits. Tumor marker CA-125 was normal. Skin prick test results for food allergens and stool examination for bacteria, ova and parasites were negative. Diagnostic paracentesis was moderately cellular with 100% eosinophils, negative for malignant cells and sterile (Figure 2). Upper endoscopy and colonoscopy demonstrated mild erythema of the gastric antrum with an unremarkable esophagus, duodenum, colon and terminal ileum. Histology revealed a mild inflammatory infiltrate in the lamina propria of the gastric antrum and duodenum comprising of lymphocytes, plasma cells and scattered eosinophils (Figure 3). Echocardiographic findings were normal. Bone marrow aspiration and biopsy showed hypercellularity with a marked increase in mature eosinophils without blasts. The findings confirmed a diagnosis of subserosal EGE.
The patient was treated with oral prednisone 25 mg daily with rapid symptomatic improvement and normalization of the hypereosinophilia within a week of initiation of steroid therapy. Four months after the weaning of steroids, follow-up abdominal computed tomography demonstrated complete resolution of the peritoneal fluid and bowel wall thickening. Two years after completion of therapy, the patient remains asymptomatic and free of ascites or hypereosinophilia.
EGE is a rare disease with an estimated prevalence of 28/100000 in United States[4]. Klein et al[1] classified EGE into three types based on the dominant layer of eosinophilic infiltration (1) predominant mucosal disease characterized by iron deficiency anemia, protein-losing enteropathy and malabsorption; (2) predominant muscle layer disease characterized by localized or diffuse thickening of the bowel wall with features of pyloric narrowing and obstructive symptoms; and (3) predominant subserosal disease characterized by eosinophil-rich ascites[1-5]. Mucosal EGE is the most common type (70%) followed by muscularis (20%) and subserosal (10%)[6,7]. EGE may also present with obstructive jaundice due to biliary tract involvement or extraintestinal manifestations such as eosinophilic cystitis, eosinophilic splenitis and hepatitis[7-9].
Talley et al[10] have defined three diagnostic criteria for EGE (1) presence of gastrointestinal symptoms; (2) biopsies of the gastrointestinal tract showing eosinophilic infiltration or characteristic radiologic findings with peripheral eosinophilia or eosinophil-rich ascites with; and (3) no evidence of parasitic or extraintestinal disease. Characteristic findings of EGE on abdominal computed tomography include thickening of bowel wall or fold, layering of the bowel wall, luminal narrowing without obstruction, intra- or extral-uminal granuloma, mesenteric lymphadenopathy with peripheral rim-like enhancement or necrosis and ascites[11]. The etiology of EGE is unclear however, an atopic predisposition is noted in patients with EGE with a history of allergy reported in 50% patients with EGE[10]. A genetic predisposition is suspected as 16% of patients with EGE have a family member with a similar condition[9]. The majority of the patients diagnosed with EGE are 20-50 years of age with no reported gender predisposition[3].
The differential diagnosis of eosinophilic ascites includes parasitic infection (Stronglyloides stercoralis, Toxocara canis), abdominal tuberculosis, rupture of hydatid cyst, chronic pancreatitis, vasculitis (Churg-Strauss syndrome), hypereosinophilic syndrome, malignancy and Crohn’s disease[12]. The diagnosis of subserosal EGE remains challenging because of its rarity and non-specific clinical features. The most common clinical features include abdominal pain (90.4%), nausea and vomiting (57.1%), diarrhea (52.3%) and abdominal distension (38.1%)[13]. It should be considered in the diagnostic evaluation of patients with abdominal pain, ascites and peripheral hypereosinophilia and a high index of suspicion should be maintained by the physician[3]. The mainstay of diagnosis of subserosal EGE is confirmation of eosinophil-rich ascitic fluid on diagnostic paracentesis and peripheral hypereosinophilia.
The overall prognosis of EGE is good with an excellent response to oral steroids comprising the first line of therapy[2]. Prednisone 20-40 mg daily in divided doses is highly effective with symptomatic remission in 80% patients within a week and normalization of eosinophil counts within two weeks of initiation of therapy[13]. Other medical therapy includes antihistaminic drugs, sodium cromoglycate, montelukast and ketotifen[2,12,14,15]. Ketotifen an antihistaminic drug and mast cell stabilizer has been used to successfully treat eosinophilic ascites as the sole therapeutic intervention. Casella et al[15] recommend ketotifen as the first-line approach to eosinophilic ascites because it is a relatively inexpensive and safe drug. Surgical intervention is rare and reserved for patients with obstructive complications[2,3]. The clinical course may be characterized by periods of remission and relapses usually when the steroid therapy is discontinued in up to 50% patients[14]. Steroid-sparing therapy with anti-histamines, mast cell inhibitors, leukotriene receptor antagonists, anti-interleukin drugs including ketotifen is useful in the treatment of relapses to avoid the side-effects of steroids[12,15]. In rare cases of failure to respond to steroid therapy, total parenteral nutrition or immunosuppressive agents including oral azathioprine or cyclophosphamide may be added to the steroid regimen in patients with diffuse mucosal disease[5].
A 35-year-old female presented with abdominal distension and diarrhea and was diagnosed with subserosal eosinophilic gastroenteritis (EGE). She responded to oral steroid therapy with complete resolution of the ascites and normalization of peripheral hypereosinophilia.
Subserosal EGE.
Ovarian cancer, abdominal tuberculosis, vasculitis, parasitic infection, congestive heart failure.
Peripheral hypereosinophilia and eosinophil-rich fluid on diagnostic paracentesis.
Abdominal computed tomography demonstrated moderate ascites with diffuse wall thickening of the small bowel.
Mucosal biopsy of the stomach and duodenum on upper endoscopy was non-diagnostic.
Oral steroid therapy.
A high index of suspicion of subserosal EGE in patients with abdominal pain, ascites and peripheral hypereosinophilia. Oral steroids adequate for initial therapy and ketotifen may be considered for relapse of EGE.
The manuscript deals with a case report and a review on an important condition and is well written.
| 1. | Klein NC, Hargrove RL, Sleisenger MH, Jeffries GH. Eosinophilic gastroenteritis. Medicine (Baltimore). 1970;49:299-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 434] [Cited by in RCA: 410] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 2. | Antonini F, Saltarelli P, Frieri G, Latella G. Education and Imaging: gastrointestinal: eosinophilic ascites. J Gastroenterol Hepatol. 2012;27:1759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (1)] |
| 3. | Jarry J, Peycru T, Shekher M. A rare cause of ascites. Gastroenterology. 2011;140:1149, 1364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Spergel JM, Book WM, Mays E, Song L, Shah SS, Talley NJ, Bonis PA. Variation in prevalence, diagnostic criteria, and initial management options for eosinophilic gastrointestinal diseases in the United States. J Pediatr Gastroenterol Nutr. 2011;52:300-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 227] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 5. | Triantafillidis JK, Parasi A, Cherakakis P, Sklavaina M. Eosinophilic gastroenteritis: Current aspects on etiology, pathogenesis, diagnosis and treatment. Ann Gastroenterol. 2007;15:106-115. |
| 6. | Simoniuk U, McManus C, Kiire C. Eosinophilic gastroenteritis--a diagnostic enigma. BMJ Case Rep. 2012;2012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Baig MA, Qadir A, Rasheed J. A review of eosinophilic gastroenteritis. J Natl Med Assoc. 2006;98:1616-1619. [PubMed] |
| 8. | Baek MS, Mok YM, Han WC, Kim YS. A patient with eosinophilic gastroenteritis presenting with acute pancreatitis and ascites. Gut Liver. 2014;8:224-227. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Elliott JA, McCormack O, Tchrakian N, Conlon N, Ryan CE, Lim KT, Ullah N, Mahmud N, Ravi N, McKiernan S. Eosinophilic ascites with marked peripheral eosinophilia: a diagnostic challenge. Eur J Gastroenterol Hepatol. 2014;26:478-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Talley NJ, Shorter RG, Phillips SF, Zinsmeister AR. Eosinophilic gastroenteritis: a clinicopathological study of patients with disease of the mucosa, muscle layer, and subserosal tissues. Gut. 1990;31:54-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 506] [Cited by in RCA: 525] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 11. | Zheng X, Cheng J, Pan K, Yang K, Wang H, Wu E. Eosinophilic enteritis: CT features. Abdom Imaging. 2008;33:191-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Salgueiro P, Magalhães R, Lago P. Cramping pain and eosinophilic ascites: what is the diagnosis? Gastroenterology. 2013;144:1353, 1577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Zhang L, Duan L, Ding S, Lu J, Jin Z, Cui R, McNutt M, Wang A. Eosinophilic gastroenteritis: clinical manifestations and morphological characteristics, a retrospective study of 42 patients. Scand J Gastroenterol. 2011;46:1074-1080. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 69] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 14. | Pineton de Chambrun G, Desreumaux P, Cortot A. Eosinophilic enteritis. Dig Dis. 2015;33:183-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 15. | Casella G, Villanacci V, Bassotti G. Eosinophilic ascites resolution with ketotifen. Mayo Clin Proc. 2011;86:1027. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: India
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Losanoff JE, Ooi LLPJ, Pani SP, Xavier-Elsas P S- Editor: Ji FF L- Editor: A E- Editor: Li D