Published online Aug 27, 2015. doi: 10.4240/wjgs.v7.i8.174
Peer-review started: November 11, 2014
First decision: December 26, 2014
Revised: June 5, 2015
Accepted: June 18, 2015
Article in press: June 19, 2015
Published online: August 27, 2015
Peritoneal encapsulation (PE) is a rare congenital malformation, characterized by a thin accessory peritoneal membrane which covers all or part of the small bowel, forming an accessory peritoneal sac. Most cases are asymptomatic and diagnosed incidentally during surgery and/or autopsy. Clinical presentation with intestinal obstruction is extremely rare and we report a case. A 25-year-old male, referred to emergency department with diffuse abdominal pain, crampy, with 8 h evolution, associated with nausea, vomiting and constipation in the last 48 h. The abdominal examination revealed an asymmetric and fixed distension, with hard consistency on palpation of lower abdominal quadrants. The abdominal radiography reveals a small bowel distension and fluid levels. Submitted to laparoscopic surgery that recourse to conversion because there is a total peritoneal encapsulation of the small bowel. After opening the peritoneal sac, we find a rotation of mesentery, at its root, conditioning twisting of small bowel and consequently occlusion. Uneventful postoperative with discharged at the 6th day. The PE is a very rare congenital anomaly characterized by abnormal bowel back into the abdominal cavity in the early stages of development. Your knowledge becomes important because, although rare, it might be diagnosis in patients with intestinal obstruction, in the absence of other etiologic factors.
Core tip: Peritoneal encapsulation is a rare congenital malformation, characterized by a thin accessory peritoneal membrane which covers all or part of the small bowel, forming an accessory peritoneal sac. Most cases are asymptomatic and diagnosed incidentally during surgery and/or autopsy. Clinical presentation with intestinal obstruction is extremely rare and we report a case.
- Citation: Teixeira D, Costa V, Costa P, Alpoim C, Correia P. Congenital peritoneal encapsulation. World J Gastrointest Surg 2015; 7(8): 174-177
- URL: https://www.wjgnet.com/1948-9366/full/v7/i8/174.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v7.i8.174
Peritoneal encapsulation (PE) is a rare congenital malformation, characterized by an accessory peritoneal membrane covering partially or totally the small bowel. Most cases are asymptomatic and diagnosed incidentally during surgery and/or autopsy[1-4].
PE, abdominal cocoon (AC) and sclerosing encapsulated peritonitis (SEP) are rare entities causing small bowel encapsulation. PE is an embryological malformation, while AC is idiopathic and SEP is predominantly associated with peritoneal dialysis[3]. However, on current literature these entities are predominantly represented by clinical cases.
Clinical presentation with intestinal obstruction is extremely rare[1-4].
A 25-year-old male with past history of gastritis, that has no medication or surgical history, referred to Emergency Department presenting diffuse and crampy abdominal pain, within 8 h, associated with nausea, vomiting and constipation for the last 48 h.
At admission, he was hemodynamically stable, apyretic and slightly dehydrated. The abdominal examination reveals a fixed and asymmetrical distension, with superficial and deep pain on palpation, especially in lower quadrants, with hard consistency and signs of peritoneal irritation.
The analytical study hasn’t significant changes and the simple abdominal radiograph documented distention of small bowel loops with air-fluid levels. Submitted to laparoscopic surgery that recourse to conversion after establishing pneumoperitoneum.
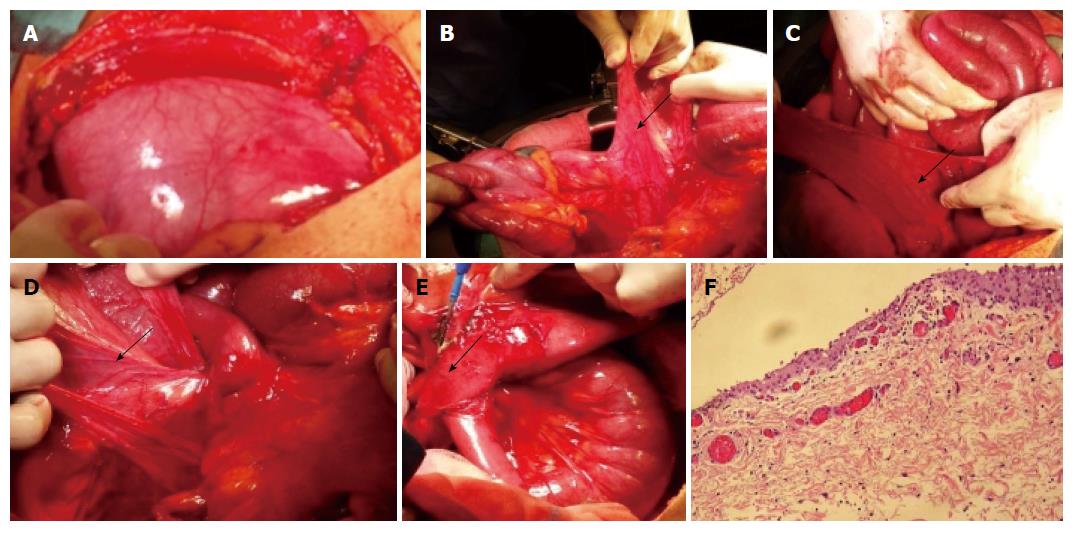
When abdominal wall was opened, there was a thin membrane covering the small bowel with hypoplasia of the great omental (Figure 1A). The obstruction was caused by the posterior aspect of right edge’s sac. The band, which obstructed the small bowel, was traced to the superior mesenteric artery, near its origin, and passed downwards until a few inches proximal to the ileocaecal valve, where it lays just above the sacral promontory (Figure 1B-D). At this point, it trapped the ileum against the sacral promontory causing obstruction. The band was divided to release the obstruction. The band contained a vessel which splits into two branches above the terminal ileum (Figure 1E). One passed downwards and backwards, deep into the pelvis, towards the upper part of the rectum. The other passed across the ileum, to end up in the sigmoid colon. The accessory peritoneal sac was excised.
Histological examination of specimen demonstrated fibrovascular tissue covered by mesothelium of peritoneal origin (Figure 1F).
Postoperative period held without complications and patient has been discharged at the 6th postoperative day.
PE is a rare congenital malformation, characterized by an accessory peritoneal membrane covering partially or totally the small bowel. It was first described in 1868 by Cleland. There’re less than 20 reports described in literature, the most diagnosed accidentally[1]. However, the actual incidence of PE becomes a challenge due to difficulty in distinguishing between this entity and the AC/SEP.
The boundaries of the peritoneal sac are laterally the ascending and descending colon, superiorly the transverse colon and inferiorly the near surface of parietal peritoneum. The membrane covers entire small bowel, since Treitz angle to ileocolic junction. The great omental, if present, covers the bag but is separated from it in full[1-4].
Embryologically, PE appears to be explained by abnormal return of small bowel to the abdominal cavity during the 12th week of pregnancy. Concomitantly the yolk sac’s coat migrates together with intestine, rather than remaining in umbilical pedicle[1].
Most cases are asymptomatic and diagnosed incidentally during surgery and/or autopsy. The case we described exemplifies clinical presentation with intestinal obstruction, which is extremely rare[1-4].
With respect to the physical examination, a patient with intestinal obstruction caused by peritoneal encapsulation presents some clinical signs: asymmetrical and fixed abdominal distension, peristalsis without variation and differences in consistency on abdominal palpation[1,5].
The preoperative diagnosis may be impossible because abdominal radiography is often normal or only reveal distended loops of small bowel, as presented in our case, such as computed tomography scan[1]. During abdominal contrast injection, the AC is characterized as a serpentiniform layout of small bowel, with a set of U-shaped loops, and slowed transit. Abdominal CT scan may reveal a central cluster of small bowel loops, with a dense coat, and signs of obstruction; intestinal wall thickening; ascites and fluid collections[1,3,5]. Differential diagnoses of PE are SEP and AC.
SEP was first described in 1907[6] being an acquired entity, in which the small bowel is covered by a whitish-gray dense collagen membrane. Is usually associated with chronic peritoneal dialysis therapy with beta-blockers, recurrent peritonitis, peritoneum or venous ventricular-peritoneal shunts, sarcoidosis, tuberculosis, Mediterranean fever, protein S deficiency, after liver transplantation, Lupus Erythematosus and fibrogenic foreign material.
The AC was first described by Foo et al[7] in 1978. It typically occurs in adolescent females in tropical or subtro pical countries. The etiology is unknown, although several theories have been presented, such as the retrograde menstruation with over-viral infection peritonitis and retrograde cell-mediated immune response promoted by gynaecological infection. It is likely that AC may be result of subclinical peritonitis. The small bowel is encapsulated by a fibrocollagenous membrane similar to SEP.
It may be associated with other anomalies such as embryological hypoplasia of great omental, as exemplified by our case, as well as malformations of mesenteric vessels[5].
The therapeutic approach in cases of intestinal obstruction, caused by PE, consists on urgent surgery, with excision of the membrane and lysis of adhesions between loops. Normally, enterectomy is not necessary, except in cases of non-reversible ischemia[3,4].
In our case, there was a twisting of peritoneal membrane, on its emergency root, conditioned by an adherence that, after lysis, provided reversibility on the caliber of small bowel loops, without ischemia. Unlike cases of SEP related to peritoneal dialysis, which earns surgical mortality beyond 60%-80%, the PE has a high survival rate, with low recurrence[5]. Histologically the membrane is composed of fibrovascular tissue covered by mesothelium from peritoneal origin. The postoperative course usually runs uneventfully, with no reported cases of recurrence[2-4].
The PE is an extremely rare congenital anomaly characterized by abnormal bowel back into the abdominal cavity in the early stages of development. Your knowledge becomes important because although rare, it might be diagnosis in patients with intestinal obstruction, in absence of other etiologic factors, such as the authors describe in this clinical case.
Peritoneal encapsulation (PE) is a rare congenital malformation, characterized by an accessory peritoneal membrane covering partially or totally the small bowel.
Most cases are asymptomatic and diagnosed incidentally during surgery and/or autopsy. Asymmetrical and fixed abdominal distension, peristalsis without variation and differences in consistency on abdominal palpation are the main clinical signs.
Differential diagnoses of PE are sclerosing encapsulated peritonitis and abdominal cocoon.
The preoperative diagnosis may be impossible because abdominal radiography is often normal or only reveal distended loops of small bowel, as presented in our case, such as computed tomography scan.
The small bowel is encapsulated by a fibrocollagenous membrane from peritoneal origin.
The therapeutic approach in cases of intestinal obstruction, caused by the PE, consists on urgent surgery with excision of the membrane and lysis of adhesions between loops. Normally, enterectomy is not necessary, except in cases of non-reversible ischemia.
The postoperative course usually runs uneventfully, with no reported cases of recurrence.
This paper is reporting an interesting congenital anomaly.
| 1. | Naraynsingh V, Maharaj D, Singh M, Ramdass MJ. Peritoneal encapsulation: a preoperative diagnosis is possible. Postgrad Med J. 2001;77:725-726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Sherigar JM, McFall B, Wali J. Peritoneal encapsulation: presenting as small bowel obstruction in an elderly woman. Ulster Med J. 2007;76:42-44. [PubMed] |
| 3. | Chew MH, Sophian Hadi I, Chan G, Ong HS, Wong WK. A problem encapsulated: the rare peritoneal encapsulation syndrome. Singapore Med J. 2006;47:808-810. [PubMed] |
| 4. | Al-Taan OS, Evans MD, Shami JA. An asymptomatic case of peritoneal encapsulation: case report and review of the literature. Cases J. 2010;3:13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Rajagopal AS, Rajagopal R. Conundrum of the cocoon: report of a case and review of the literature. Dis Colon Rectum. 2003;46:1141-1143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Naidoo K, Mewa Kinoo S, Singh B. Small Bowel Injury in Peritoneal Encapsulation following Penetrating Abdominal Trauma. Case Rep Surg. 2013;2013:379464. [PubMed] |
| 7. | Foo KT, Ng KC, Rauff A, Foong WC, Sinniah R. Unusual small intestinal obstruction in adolescent girls: the abdominal cocoon. Br J Surg. 1978;65:427-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 208] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Contini S, Golffier C, Parker W S- Editor: Ji FF L- Editor: A E- Editor: Jiao XK